Abstract
A 49-year-old Japanese man had multiple huge masses (max. size 60 mm diameter) in his liver. These tumors were pathologically diagnosed by tumor biopsy as epithelioid hemangioendotheliomas of the liver. In this case, multiple liver tumors existed in both lobes. Also this patient did not agree to receive surgical resection including liver transplantation. Chemotherapy with sorafenib at a dose of 400 mg/body twice a day was started. About 6 months later, CT findings revealed that these tumors were shrinking slightly; 33 months later, the tumors obviously showed a partial response in accordance with the Response Evaluation Criteria in Solid Tumors (RECIST). Also 60 months later, the partial response continued with sorafenib monotherapy.
Key Words: Epithelioid hemangioendothelioma, Sorafenib, Malignant liver tumor
Case Report
A 49-year-old man was admitted to the local hospital complaining of upper abdominal pain. Contrast-enhanced CT imaging revealed multiple hypoenhanced tumors (max. size 60 mm diameter) mainly in peripheral areas of the liver (fig. 1a, fig. 2a). The patient was referred to our hospital for a more detailed diagnosis and treatment.
Fig. 1.
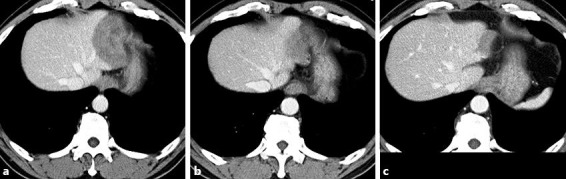
Enhanced abdominal CT findings. a At baseline. Huge hypoenhanced tumors showed mainly in peripheral areas of the liver (segments 2 and 3). b About 3 years later. The liver tumors have gradually decreased in size. c About 5 years later. The liver tumors have shrunk considerably.
Fig. 2.

Enhanced abdominal CT findings. a At baseline. Hypoenhanced tumors showed in segment 5 of the liver. b About 3 years later. The liver tumors have gradually decreased in size. c About 5 years later. The liver tumors have almost disappeared.
Laboratory data including tumor markers were almost within normal range. Needle biopsy specimens from the tumors revealed that the liver parenchyma was replaced by a fibrotic tissue containing moderate dysplastic polygonal tumor cells within spindle- or round-shaped nuclei (fig. 3a). Immunohistochemical examinations revealed that the tumor cells showed positive staining for CD31 (fig. 3b). We finally diagnosed epithelioid hemangioendothelioma (EHE) of the liver. According to previously reported cases, this tumor is a low-grade malignancy; surgical resection or liver transplantation should be considered the first treatment if EHE is confined to the liver. In our case, multiple liver tumors existed in both lobes. Also this patient did not agree to receive surgical resection including liver transplan-tation.
Fig. 3.
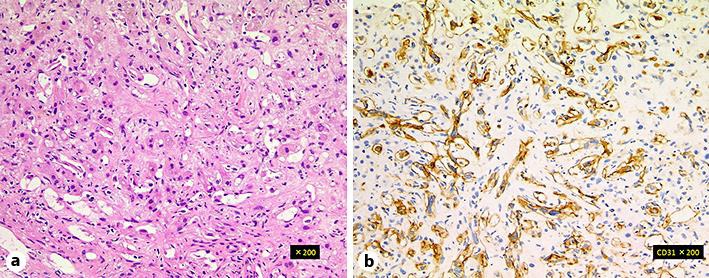
a, b Microscopic examination of biopsy specimens. The liver parenchyma was replaced by a fibrotic tissue containing moderate dysplastic polygonal tumor cells within spindle- or round-shaped nuclei. An immunohistochemical analysis revealed the cells to be positive for CD31.
Chemotherapy with sorafenib at a dose of 400 mg/body twice a day was started. Major toxicity of grade 3 or 4 (Common Terminology Criteria for Adverse Events) did not occur; only grade 1 or 2 hand foot syndrome appeared. The patient was continuously taking sora-fenib at 400–800 mg/day according to the grade of the hand foot syndrome. About 6 months later, CT findings revealed that the tumors were shrinking slightly; 33 months later, the tumors obviously showed a partial response in accordance with the Response Evaluation Criteria in Solid Tumors (RECIST) (fig. 1b, fig. 2b). Also 60 months later, they were shrinking significantly (fig. 1c, fig. 2c). Currently, the patient is still taking sorafenib, and the partial response is still continuing.
Discussion
Hepatic EHE is a rare mesenchymatous tumor with an epithelial aspect developed from endothelial cells. From 1984 to 2006, 434 cases of EHE were reported, with only 252 cases of primary liver disease [1]. EHE displays a low-to-intermediate grade of malignancy between liver hemangioma and angiosarcoma [2]. Symptoms of EHE are nonspecific, and tumor marker levels are usually normal. Radiological findings associated with these tumors facilitate an accurate diagnosis. On nonenhanced CT images, all nodules are hypoattenuating as compared with normal liver parenchyma, and contrast-enhanced CT images sometimes display discontinuous peripheral rim enhancement. Multiple tumor nodules frequently coalesce and form larger confluent masses, with a propensity to involve the peripheral regions of the liver and to extend to the liver margin [3]. A definitive diagnosis of hepatic EHE requires histological confirmation. Histologically, the tumors are composed of fibrous myxoid stroma with a relatively hypocellular center. The tumor periphery shows increased cellularity with active proliferation of epithelioid round cells and spindle-shaped cells in variable proportions. Immunostaining for endothelial markers such as factor VIII, CD31, and CD34 is essential for diagnosis [4].
Treatment of localized EHE requires surgery with partial or total hepatectomy. Liver transplantation is another therapeutic option. In metastatic or unresectable EHE patients, various regimens of chemotherapy have been tried, without any evidence for a first-line treatment due to the low incidence of EHE.
Sorafenib is one of the theoretic options for unresectable EHE. It is an inhibitor of the tyrosine kinase associated with this signaling pathway. In addition, sorafenib strongly inhibits several tyrosine kinases associated with molecules involved in the angiogenic process, such as VEGFR-2 and −3 and platelet-derived growth factor subunit B. According to a large reliable prospective phase II study (n = 15), sorafenib provided long-lasting (>6 months) tumor growth arrest in >33% of the patients with unresectable EHE. However, partial responses were very rare (in 2 of the 15 patients), and the time to progression was 6 months [5]. Cioffi et al. [6] reported a retrospective study of 42 additional patients with metastatic EHE; 34 of those patients received systemic treatment, including conventional doxorubicin-containing regimens, other chemotherapy regimens, and angiogenesis-targeting drugs or tyrosine ki nase inhibitors, but there was no objective response. The median progression-free survival was 4.8 months, and the median overall survival was 41.0 months. Our case, therefore, presented with a very rare condition, displaying tumor shrinkage with sorafenib monotherapy for hepatic EHE over a period of 5 years.
Statement of Ethics
The authors have no ethical conflicts to disclose.
Disclosure Statement
The authors declare that there are no conflicts of interest.
References
- 1.Mehrabi A, Kashfi A, Fonouni H, Schemmer P, Schmied BM, Hallscheidt P, et al. Primary malignant hepatic epithelioid hemangioendothelioma: a comprehensive review of the literature with emphasis on the surgical therapy. Cancer. 2006;107:2108–2121. doi: 10.1002/cncr.22225. [DOI] [PubMed] [Google Scholar]
- 2.Weiss SW, Enzinger FM. Epithelioid hemangioendothelioma: a vascular tumor often mistaken for a carcinoma. Cancer. 1982;50:970–981. doi: 10.1002/1097-0142(19820901)50:5<970::aid-cncr2820500527>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 3.Bruegel M, Muenzel D, Waldt S, Specht K, Rummeny EJ. Hepatic epithelioid hemangioendothelioma: findings at CT and MRI including preliminary observations at diffusion-weighted echo-planar imaging. Abdom Imaging. 2011;36:415–424. doi: 10.1007/s00261-010-9641-5. [DOI] [PubMed] [Google Scholar]
- 4.Makholouf HR, Ishak KG, Goodman ZD. Epithelioid hemangioendothelioma of the liver: a clinicopathologic study of 137 cases. Cancer. 1999;85:562–582. doi: 10.1002/(sici)1097-0142(19990201)85:3<562::aid-cncr7>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 5.Chevreau C, Le Cesne A, Ray-Coquard I, Italiano A, Cioffi A, Isambert N, et al. Sorafenib in patients with progressive epithelioid hemangioendothelioma: a phase 2 study by the French Sarcoma Group (GSF/GETO) Cancer. 2013;119:2639–2644. doi: 10.1002/cncr.28109. [DOI] [PubMed] [Google Scholar]
- 6.Cioffi A, Italiano A, Penel N, et al. Metastatic epithelioid hemangioendothelioma (EHE): role of systemic therapy and survival (abstract) J Clin Oncol. 2011;29(suppl):10079. [Google Scholar]


