Abstract
The authors’ study evaluates the complications associated with the treatment of clavicle fractures in adolescents. During the study period, 153 clavicle fractures occurred in patients between the ages of 14 and 17 years who were treated at the authors’ center, of which 23 (15.0%) were treated surgically. Compared to the fractures treated nonoperatively, the surgical fractures had greater shortening (mean, 2.0 vs 0.9 cm; P<.001) and were more likely to be comminuted (65.2% vs 23.1%; P<.001). Complications occurred in 21.7% of fractures treated surgically. One delayed union occurred in the nonoperative cohort, but no other complications or patients who required clavicular osteotomy for malunion. Pediatric fellowship-trained orthopedic surgeons treated 78 displaced fractures, resulting in 8 (10.3%) surgeries. Nonpediatric orthopedic specialists treated 46 displaced fractures, 15 (32.6%) of which were treated operatively (P=.0035).
Figure.

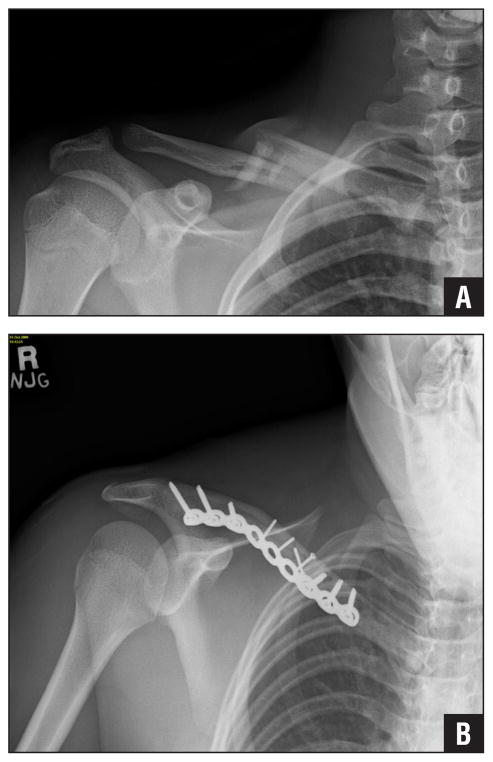
A 15-year-old boy sustained a comminuted clavicle fracture from playing football. Preoperative radiograph showing significant clavicle shortening and a vertical fragment.
Clavicle fractures account for approximately 15% of all fractures in children.1–5 Midshaft clavicle fractures are the most common, representing 70% to 90% of fractures.1,6–9 Due to the excellent healing potential in children, even significantly displaced adolescent clavicle fractures have traditionally been treated nonoperatively.1,3,10 However, recent studies in adults have reported higher rates of nonunion and impaired biomechanics following nonoperative management of displaced and shortened fractures.4,8,11–14 The changing approach to clavicle fracture treatment in adults has raised new questions regarding treatment in the adolescent population. The purpose of this study was to compare fracture characteristics and short-term complications for adolescent midclavicular fractures treated operatively compared with those treated nonoperatively.
Materials and Methods
This study was a single-institution, retrospective review of all clavicle fractures sustained by adolescents aged 14 to 17 years from January 2005 to January 2013. Institutional Review Board approval was obtained for all aspects of the study. Inclusion criteria were midshaft clavicle fractures in adolescents. Medial or distal shaft fractures, pathologic fractures, and fractures with inadequate radiographs were excluded. Patients who had sustained fractures to both clavicles in separate, unrelated injuries were included, and each fracture was considered a distinct case in this study. Medical records were reviewed to gather information on patient demographics, injury mechanism and severity, treatment method, follow-up length, and complications. A complication was defined in this study as any subsequent adverse event (eg, refractures or delayed bone healing that necessitated further treatment). Radiographic images at the time of injury were reviewed to determine fracture pattern and displacement and to assess for the amount of shortening. Injury mechanism was assessed as high, medium, or low energy:
Low energy: falls, running or playground injuries
Medium energy: sports, bicycle, wrestling, and skateboard injuries
High energy: football, hockey, skiing/snowboarding, all-terrain vehicle, motocross, and motor vehicle collision injuries In the nonoperative group, patients were treated in a sling, in a figure-8 splint, or with immobilization. In the operative group, surgical fixation was performed with plate or intramedullary nail fixation. Patients were followed until radiographic union.
Statistical comparison of injury severity, fracture characteristics, and treatment method with patient demographics were analyzed using the chi-square test and the 2-tailed Fisher’s exact test. P values were reported to show the probability of having a significant association. The significance level was determined to be a P value less than .05. Descriptive statistics were reported as numbers for all variables of interest (percentage, mean, range).
Results
Between 2005 and 2013, a total of 149 patients between ages 14 and 17 years were treated for 153 midshaft clavicle fractures (Table 1). Of those, 113 fractures were caused by a high-energy mechanism (Table 2), most commonly involving football (n=41) and motocross (n=23). A majority of these occurred in males (n=103, 91.2%). Associated injuries were seen in 21 patients and included rib fractures, spine fractures, proximal and distal extremity fractures, facial fractures, and closed-head injuries. No open or impending open fractures were reported. Twenty-three (15.0%; 19 boys, 4 girls) fractures underwent surgical treatment using either plate (n=19) or intramedullary nail (n=4) fixation (Table 3). Mean age was 15.5 years (range, 14 to 17 years) in the surgical group and 15.4 years in the nonsurgical group (P=.717). Eighteen fractures were caused by a high-energy mechanism, most commonly from football (n=7).
Table 1.
Injury Severity Distribution
| Injury Severity | No. of Patients |
|---|---|
| Low | 13 |
| Medium | 27 |
| High | 113 |
| Total | 153 |
Table 2.
High-Energy Mechanism Causes of Clavicle Fracture
| Cause | No. of Patients |
|---|---|
| All-terrain vehicle | 8 |
| Football | 41 |
| Hockey | 17 |
| Motocross | 23 |
| Motor vehicle collision | 11 |
| Skateboard, ski, sled, or snowboard | 13 |
| Total | 113 |
Table 3.
Surgery Group
| Age, y/Gender | Mechanism (Energya) | Clavicle Shortening, cm | Comminution | Implant Used | Refracture | Additional Surgery |
|---|---|---|---|---|---|---|
| 17/M | Sledding (3) | 2.5 | Yes | Plate | No | |
| 17/M | Football (3) | 2.3 | No | Plate | No | |
| 16/F | Hockey (3) | 2.5 | Yes | Plate | No | |
| 16/M | Track (2) | 2.3 | Yes | Plate | No | |
| 16/F | ATV (3) | 1.6 | No | Nail | No | Revision ORIF w/plate |
| 16/M | Football (3) | 2.9 | Yes | Nail | No | |
| 16/M | MVC (3) | 1.8 | Yes | Plate | No | Implant removal |
| 16/M | Hockey (3) | 1.9 | No | Plate | No | |
| 16/M | Motocross (3) | 1.7 | Yes | Plate | No | |
| 16/M | MVC (3) | 2.0 | No | Plate | No | |
| 16/M | Motocross (3) | 2.6 | No | Nail | Yes | |
| 16/M | Skiing (3) | 1.7 | Yes | Plate | No | Implant removal |
| 15/M | Football (3) | 2.1 | Yes | Plate | No | |
| 15/F | Soccer (2) | 1.6 | Yes | Plate | No | |
| 15/M | Skiing (3) | 1.6 | Yes | Plate | No | |
| 15/M | Gym (2) | 2.4 | Yes | Plate | No | |
| 15/M | Football (3) | 3.4 | Yes | Plate | No | |
| 15/M | Football (3) | 1.6 | Yes | Nail | No | |
| 15/M | Hockey (3) | 0.6 | No | Plate | No | |
| 14/M | Football (3) | 0.9 | No | Plate | No | |
| 14/M | BMX (2) | 1.8 | Yes | Plate | Yes | Revision ORIF w/plate |
| 14/M | Football (3) | 2.7 | Yes | Plate | No | |
| 14/F | Soccer (2) | 2.5 | No | Plate | No |
Abbreviations: ATV, all-terrain vehicle; BMX, bicycle motocross; MVC, motor vehicle collision; ORIF, open reduction and internal fixation.
Energy: 1=low, 2=medium, 3=high.
The surgically treated fractures were all displaced, with a mean shortening of 2.0 cm (range, 0.6–3.4 cm). Of the 130 non-operatively treated fractures, 89 (68.5%) were displaced, and mean shortening was 0.9 cm (range, 0–3.0 cm; P<.001), including 13 fractures (10%) with more than 2 cm of shortening. Comminution was more common in the surgical group than in the nonsurgical group (65.2% vs 23.1%, respectively; P<.001). Five (21.7%) surgical patients experienced complications, including refracture (n=2), implant removal for prominence (n=2), and nonunion with implant failure (n=1). One complication was associated with intramedullary nailing, whereas the other 4 complications occurred in clavicles treated with plate fixation. No infections or cutaneous nerve problems were observed in the operative group. Of the 130 adolescents who had nonoperative treatment, none sustained a refracture or malunion that required surgical intervention.
In the current study, 124 displaced fractures received orthopedic consults. Pediatric fellowship-trained orthopedic surgeons treated 78 displaced fractures with mean clavicle shortening of 1.1 cm, resulting in 8 (10.3%) surgeries. Of these 8 fractures, 7 had a vertical fragment (Figure 1). The 8 patients had a mean age of 15.0 years, with a mean clavicle shortening of 1.9 cm. Nonpediatric orthopedic specialists treated 46 displaced fractures with mean clavicle shortening of 1.3 cm (P=.19), of which 15 (32.6%) were treated operatively (P=.0035). Compared with the former group, this group had a mean age of 15.7 years (P=.09), with a mean clavicle shortening of 2.1 cm (P=.44).
Figure 1.
A 15-year-old boy sustained a comminuted clavicle fracture from playing football. Pre-operative radiograph showing significant clavicle shortening and a vertical fragment (A). Postoperative radiograph showing fixation with a pelvic reconstruction plate (B).
Discussion
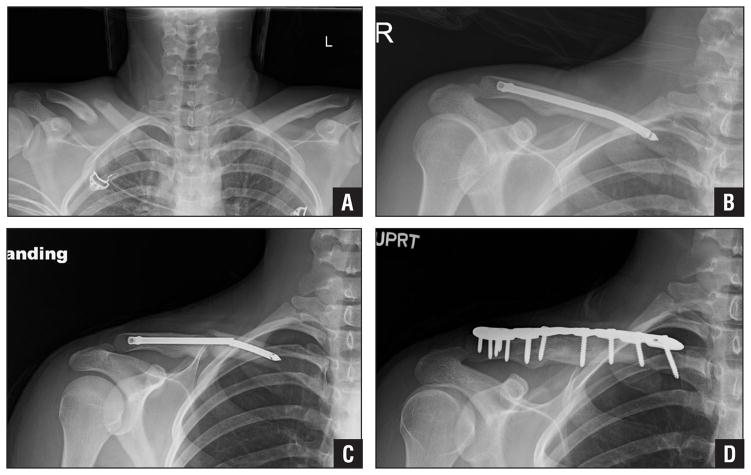
Recent studies in adults have supported the surgical management of displaced clavicle fractures, showing high rates of nonunion and functional deficits compared with the uninjured side, particularly for fractures with more than 2 cm of shortening.4,9,11,12,15–17 As a result, clavicle fractures in adolescents are more frequently treated with surgery.10 However, the literature describing surgical fixation of clavicle fractures in children and adolescents is limited.1,2 The current series reported a high complication rate (22%) for surgical fixation of clavicle fractures, with 2 refractures, 2 implant removals, and 1 implant failure. Both cases of refracture occurred approximately 10 months after the original injury due to the same mechanism—1 from motocross and the other from bicycle motocross. One patient was subsequently treated with immobilization, and the other underwent repeat surgical fixation. The nonunion occurred in a 16-year-old girl who sustained multiple traumas from an all-terrain vehicle accident and underwent intramedullary nail fixation. At 7-months follow-up, radiographic images showed that the intramedullary nail had broken and the fracture had not healed. All workups for infection were negative, and the patient underwent revision surgery with plating and autologous bone graft, which resulted in union (Figure 2). Overall, 4 (17.4%) patients required an additional surgery.
Figure 2.
A 16-year-old female sustained after an all-terrain vehicle accident. Preoperative radiograph showing a displaced midclavicular fracture with 1.6 cm of shortening (A). Radiograph showing intramedullary nail fixation postoperatively (B). Radiograph 7 months after initial surgery showing nonunion with failed implant (C). Radiograph showing healed clavicle 1 year after revision plating (D).
Kubiak and Slongo1 reviewed a series of 15 patients with a mean age of 13.1 years (range, 9.3–15.6 years) who underwent surgical fixation of clavicle fractures. Although all patients had satisfactory outcomes and minimal complications, all of those who had wire or nail fixation (n=13) eventually underwent a second surgery for implant removal.1 Mehlman et al18 reported on a series of 24 patients with a mean age of 12 years 8 months (range, 7–16) who underwent surgical fixation for displaced midshaft clavicle fractures. All fractures healed with only minor complications, although all patients elected for a second surgery for implant removal.18
Vander Have et al2 retrospectively compared the surgical and nonsurgical treatment of clavicle fractures in adolescents. Three (17.6%) of 17 surgical patients underwent elective hardware removal. Conversely, in the nonoperative patients, the authors found a high rate of symptomatic malunions, with 80% of those patients undergoing a corrective osteotomy for indications such as painful bony prominence and weakness with overhead activities.2 In contrast, for the current series of fractures, no patients treated nonoperatively sustained a malunion that required delayed surgical fixation or corrective osteotomy. There was 1 (4.3%) nonunion in 23 operative fractures, which is more consistent with earlier studies in adults.9,17 Although, on average, there was more shortening and comminution in the operative group, 13 (10%) fractures in the nonoperative group had shortening greater than 2.0 cm and 30 (23%) fractures were comminuted. Thus, due to a lack of definitive outcomes data, fractures with similar radiographic appearances may be treated operatively or nonoperatively based on surgeon and family decision making.
The rate of implant removal in the authors’ operative cohort also differed from the existing literature, indicating wide practice variability.1,2,18 Some surgeons prefer to remove the implant in all patients after clavicle fracture union, whereas others plan for additional surgery only if the patient complains of symptomatic hardware. In either case, adolescent patients undergoing surgical fixation for clavicle fracture must be warned of the possibility of return to the operating room to remove the implant.
Physician preference continues to play an important role in the decision to operate. Carry et al10 conducted a survey of members of the Pediatric Orthopaedic Society of North America (POSNA) to determine treatment preferences. Although most POSNA members preferred nonoperative treatment for all fracture patterns across all age groups and genders, there was no clear consensus for patients aged 16 to 19 years. Caird5 recommended that the decision should be based on the overall clinical picture and sport or activity level of the patient. At the authors’ center, it appears that operative management is favored by their adult trauma surgeons (32.6% of fractures) rather than by their pediatric orthopedic team (10.3%), despite the lack of significant difference in clavicle shortening in patients seen by the 2 groups (1.3 vs 1.1 cm, respectively; P=.19). Adult surgeons operated on nearly all fractures with more than 1.5 cm of shortening. The majority of patients who received surgical treatment by the authors’ pediatric orthopedic surgeons had a vertical fragment or severe comminution. The overall surgical group had a mean fracture shortening of 2.0 cm, consistent with the relative indication for surgery utilized by most surgeons, although some fractures with 100% displaced but minimal radiographic shortening also underwent operative treatment.2,3,5,12 Thus, further data are needed to determine how much shortening results in impaired shoulder function and at what degree of skeletal maturity remodeling becomes insufficient to restore acceptable shoulder function.
The main limitations of the current study include its retrospective design, the lack of patient-reported outcomes, and its follow-up only until fracture union. Nevertheless, this series showed a low rate of reoperation and complications in the nonoperative group compared with the operative group. Given the rate of complications in surgically treated fractures, significant functional benefit must be demonstrated to support operative management of displaced clavicle fractures in adolescents. Recent data in nonoperative adolescent clavicle fractures suggest subtle functional deficits on motion analysis testing, although no comparison studies to operative clavicle fractures have been done.19 This may provide valuable information regarding the long-term functional results of nonoperative treatment vs operative treatment of displaced, shortened clavicle fractures.
Conclusion
The authors’ series showed satisfactory results in patients undergoing operative and nonoperative treatment of displaced clavicle fractures. Patients and families should be counseled about the treatment outcomes and the likelihood for reoperation due to prominent implants, refractures, or nonunion following operative treatment. Patients who participate in activities with high-energy mechanisms of injury should be warned about returning to activity too early due to the possibility of refracture. Most patients treated surgically by pediatric orthopedic surgeons had a vertical fragment with comminution. Non-pediatric orthopedic specialists operated on a higher percentage of displaced clavicle fractures in adolescents, showing that a wide practice variation remains for the management of midshaft clavicle fractures in this age group.
Footnotes
The authors have no relevant financial relationships to disclose.
References
- 1.Kubiak R, Slongo T. Operative treatment of clavicle fractures in children: a review of 21 years. J Pediatr Orthop. 2002;22(6):736–739. [PubMed] [Google Scholar]
- 2.Vander Have KL, Perdue AM, Caird MS, Farley FA. Operative versus nonoperative treatment of midshaft clavicle fractures in adolescents. J Pediatr Orthop. 2010;30(4):307–312. doi: 10.1097/BPO.0b013e3181db3227. [DOI] [PubMed] [Google Scholar]
- 3.Silva SR, Fox J, Speers M, et al. Reliability of measurements of clavicle shaft fracture shortening in adolescents. J Pediatr Orthop. 2013;33(3):e19–e22. doi: 10.1097/BPO.0b013e318287f73f. [DOI] [PubMed] [Google Scholar]
- 4.Ledger M, Leeks N, Ackland T, Wang A. Short malunions of the clavicle: an anatomic and functional study. J Shoulder Elbow Surg. 2005;14(4):349–354. doi: 10.1016/j.jse.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 5.Caird MS. Clavicle shaft fractures: are children little adults? J Pediatr Orthop. 2012;32(suppl 1):S1–S4. doi: 10.1097/BPO.0b013e31825870ad. [DOI] [PubMed] [Google Scholar]
- 6.Hillen RJ, Burger BJ, Poll RG, van Dijk CN, Veeger DH. The effect of experimental shortening of the clavicle on shoulder kinematics. Clin Biomech (Bristol, Avon) 2012;27(8):777–781. doi: 10.1016/j.clinbiomech.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 7.Frye BM, Rye S, McDonough EB, Bal GK. Operative treatment of adolescent clavicle fractures with an intramedullary clavicle pin. J Pediatr Orthop. 2012;32(4):334–339. doi: 10.1097/BPO.0b013e31825611da. [DOI] [PubMed] [Google Scholar]
- 8.Canadian Orthopaedic Trauma Society. Non-operative treatment compared with plate fixation of displaced midshaft clavicular fractures: a multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89(1):1–10. doi: 10.2106/JBJS.F.00020. [DOI] [PubMed] [Google Scholar]
- 9.Rowe CR. An atlas of anatomy and treatment of midclavicular fractures. Clin Orthop Relat Res. 1968;(58):29–42. [PubMed] [Google Scholar]
- 10.Carry PM, Koonce R, Pan Z, Polousky JD. A survey of physician opinion: adolescent mid-shaft clavicle fracture treatment preferences among POSNA members. J Pediatr Orthop. 2011;31(1):44–49. doi: 10.1097/BPO.0b013e3181ff67ce. [DOI] [PubMed] [Google Scholar]
- 11.McKee MD, Pedersen EM, Jones C, et al. Deficits following nonoperative treatment of displaced midshaft clavicular fractures. J Bone Joint Surg Am. 2006;88(1):35–40. doi: 10.2106/JBJS.D.02795. [DOI] [PubMed] [Google Scholar]
- 12.Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br. 1997;79(4):537–539. doi: 10.1302/0301-620x.79b4.7529. [DOI] [PubMed] [Google Scholar]
- 13.Duan X, Zhong G, Cen S, Huang F, Xiang Z. Plating versus intramedullary pin or conservative treatment for midshaft fracture of clavicle: a meta-analysis of randomized controlled trials. J Shoulder Elbow Surg. 2011;20(6):1008–1015. doi: 10.1016/j.jse.2011.01.018. [DOI] [PubMed] [Google Scholar]
- 14.Pandya NK, Namdari S, Hosalkar HS. Displaced clavicle fractures in adolescents: facts, controversies, and current trends. J Am Acad Orthop Surg. 2012;20(8):498–505. doi: 10.5435/JAAOS-20-08-498. [DOI] [PubMed] [Google Scholar]
- 15.Post M. Current concepts in the treatment of fractures of the clavicle. Clin Orthop Relat Res. 1989;(245):89–101. [PubMed] [Google Scholar]
- 16.Neer CS. Nonunion of the clavicle. JAMA. 1960;172:1006–1011. doi: 10.1001/jama.1960.03020100014003. [DOI] [PubMed] [Google Scholar]
- 17.Wilkes JA, Hoffer MM. Clavicle fractures in head-injured children. J Orthop Trauma. 1987;1(1):55–58. doi: 10.1097/00005131-198701010-00008. [DOI] [PubMed] [Google Scholar]
- 18.Mehlman CT, Yihua G, Bochang C, Zhigang W. Operative treatment of completely displaced clavicle shaft fractures in children. J Pediatr Orthop. 2009;29(8):851–855. doi: 10.1097/BPO.0b013e3181c29c9c. [DOI] [PubMed] [Google Scholar]
- 19.Schulz J, Moor M, Roocroft J, Bastrom TP, Pennock AT. Functional and radiographic outcomes of nonoperative treatment of displaced adolescent clavicle fractures. J Bone Joint Surg Am. 2013;95(13):1159–1165. doi: 10.2106/JBJS.L.01390. [DOI] [PubMed] [Google Scholar]