Abstract
We present a case of cryptococcal meningoencephalitis producing narrowing of both middle cerebral arteries on MRI/MRA, described in a 56-year-old man with a history of Wegener’s granulomatosis. Diagnosis was based on the presence of cryptococcal antigen in serum and CSF. Imaging performed seven months after initial presentation demonstrated thickened enhancing leptomeninges with focal inflammatory masses in the Sylvian fissures. To our knowledge, this striking appearance has not been previously demonstrated simultaneously on MRI/MRA.
Abbreviations: MRI, magnetic resonance imaging; CSF, cerebrospinal fluid; MRA, magnetic resonance angiogram; MCA, middle cerebral artery; DWI, diffusion-weighted imaging; MIP, maximal intensity projection
Case report
A 56-year-old man receiving prednisone for Wegener’s granulomatosis presented with fever, confusion, and progressive weakness. Wegener’s granulomatosis had been previously diagnosed with a temporal artery biopsy, which demonstrated neutrophilic infiltration of the vessel wall consistent with a necrotizing vasculitis. Serum studies and CSF (titer 1:4096) were positive for Cryptococcus neoformans with a normal opening pressure. Cytology and flow cytometry were negative for B cells, plasma cells, or malignant cells. The patient was treated with ambisone and flucytosine initially. He also had cavitating lesions in the lung, spleen, and liver consistent with disseminated cryptococcal infection.
For the next six to seven months, the patient was re-admitted to the hospital repeatedly due to intermittent recurring headaches. Serial MRIs demonstrated progressive development of new lesions in the basal ganglia, ventriculitis, and worsening leptomeningitis with associated cerebritis. The patient was weaned off prednisone. His persistent symptoms were thought to be due to immune reconstitution syndrome, given the combination of worsening imaging features and elevated lumbar-puncture opening pressure, in the setting of reduced CSF cryptococcal antigen and negative CSF cultures. He subsequently changed to fluconazole for treatment of his cryptococcal meningoencephalitis.
MRI with contrast (Fig. 1) obtained approximately seven months after first presentation demonstrated a nodular mass with meningeal enhancement and parenchymal edema adjacent to the right MCA trifurcation, and a slightly more medial mass adjacent to the left MCA. There was high-grade vessel narrowing seen on MRA (Fig. 2) in both vessels at the precise location of the enhancement. Moderate irregularity of the left proximal A1 segment, which was also involved with inflammatory disease, was also noted on the MRA. Abnormal enhancement of the ependyma and choroid plexi was present. No infarct was seen on DWI.
Figure 1.
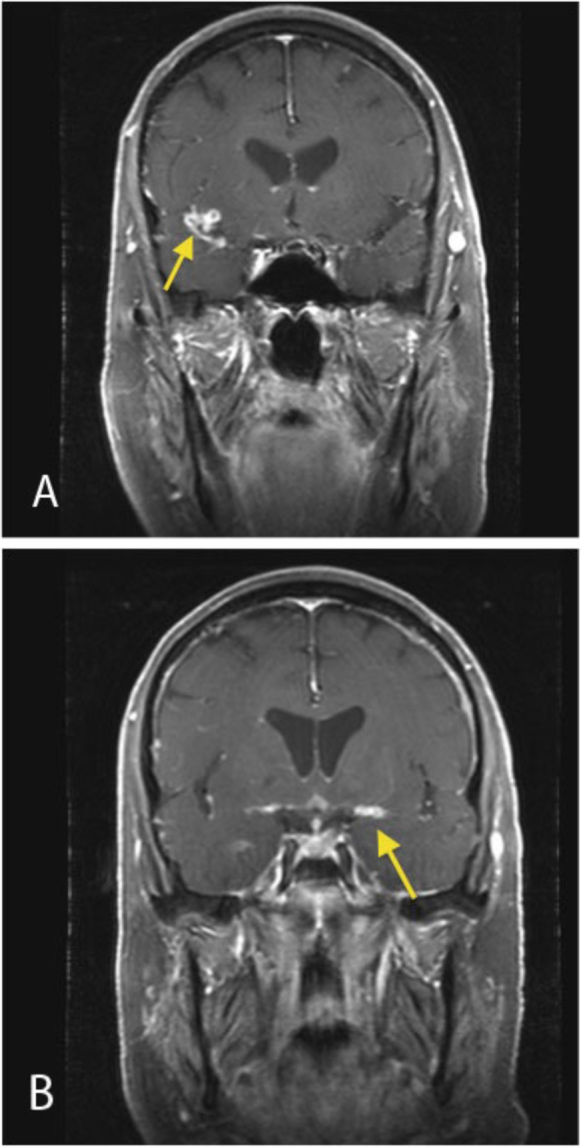
Coronal contrast-enhanced T1-weighted MRI (A, right side; B, left side) demonstrates nodular leptomeningeal enhancement in the Sylvian fissures in the location of the M1 segments of the middle cerebral arteries (arrows). Diffuse pachymeningeal enhancement is also demonstrated.
Figure 2.
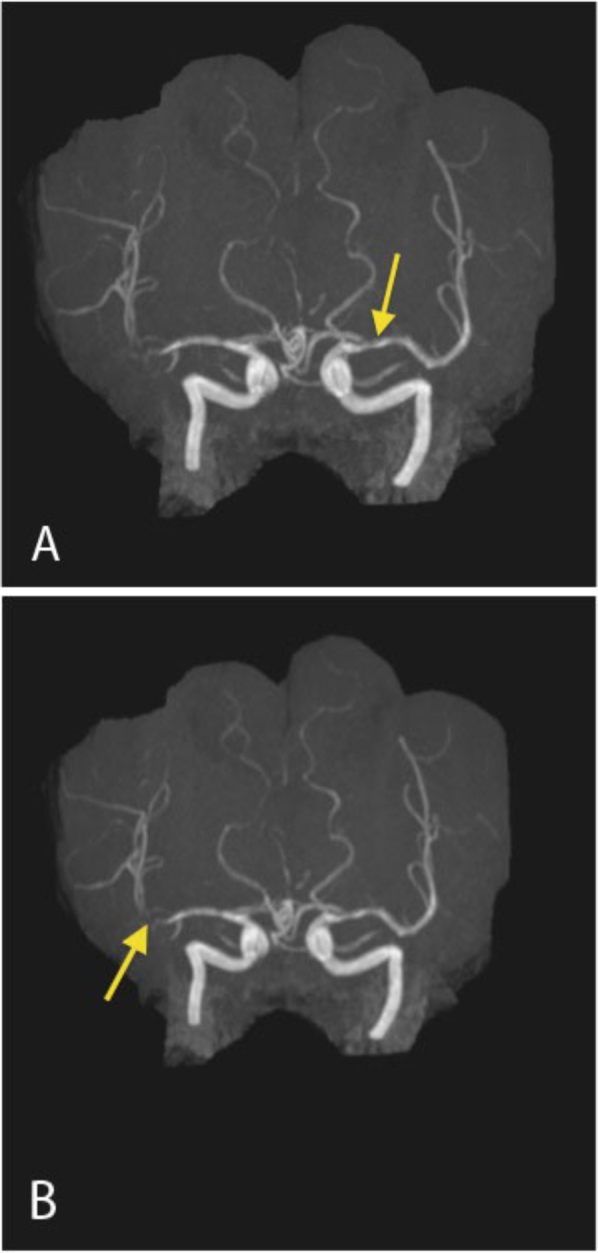
MRA time of flight (3D MIP) demonstrates (A) mild narrowing of the left middle cerebral artery and (B) marked narrowing of the right middle cerebral artery trifurcation. These areas of narrowing coincide with the areas of nodular leptomeningeal enhancement on the contrast MRI.
Biopsy of the right temporal lobe, performed approximately one month after the images shown were obtained, demonstrated active and chronic inflammation and numerous yeast forms, although no growth on culture media was observed. The final diagnosis was Cryptococcus neoformans infection.
The latest MRI, performed ten months after initial presentation (not shown), demonstrated stable subependymal nodules and a decrease in the extent of leptomeningeal enhancement, particularly in the Sylvian fissures. Grossly similar, persistent, unchanged high-grade vessel narrowing was seen on the repeated standard sequences (T2 and postcontrast T1), although repeat MRA was not performed.
Discussion
MRI and CT findings previously described in CNS cryptococcosis range from no abnormality to meningeal enhancement, ventriculomegaly, and meningoencephalitis in the form of pseudocysts in the basal ganglia, thalami, midbrain, cerebellum, and the periventricular regions (1). These pseudocysts may demonstrate diffusion restriction (2). Granulomatous lesions have also been described. The differential diagnoses include neoplasm, granulomatous disease, brain abscess, and arteriovenous malformation.
Arterial stenosis secondary to exudates and inflammation has been documented in the literature, most often in the setting of angioinvasive aspergillus and atypical meningitis (cryptococcal and tuberculosis). Clinical symptoms in those with arterial stenosis are often indistinguishable from those without stenosis (3), suggesting adequate preservation of flow. These intracranial arterial stenoses have also been noted to persist over a longer period of time than other complications in atypical meningitis (3). This was evident in our case, where the imaging features of stenosis were evident despite a time interval of over three months. Studies have shown that the stenoses of major intracranial cerebral arteries can be slowly progressive, or can be reversible (3).
Exudates involving the basal cisterns and Sylvian fissures in the setting of chronic cryptococcal meningoencephalitis have been documented as a cause of cerebral infarction, particularly lacunar infarcts (4). Cerebral infarction can occur both in the acute stage and latter stages of treatment (5). The mechanisms are thought to be either related to vasculitis with inflammation, spasms, constriction, and subsequent thrombosis or necrotizing panarteritis with secondary thrombosis and occlusion. However, infarcts in major vascular territories are rare (5). Involvement distal to the M1 segments of the middle cerebral arteries is rare (5). Other uncommon locations include the cortical branches of the middle cerebral artery, the supraclinoid portion of the ICA, and the vertebrobasilar system (6).
Although our case distinctively illustrates distal large-vessel narrowing on MRI/MRA at a single time point, serial MRA may serve as a useful tool to monitor those with progressive intracranial arterial stenoses, as this subset of patients may have a poorer prognosis.
In conclusion, we present a case of cryptococcal meningitis associated with vascular narrowing and multifocal enhancement. Although vascular narrowing is not commonly associated with cryptococcal infection, we conclude that this may occur, either as a result of direct vascular invasion or more likely secondary to associated inflammation.
Footnotes
Published: October 20, 2011
References
- 1.Tien RD, Chu PK, Hesselink JR, Duberg A, Wiley C. Intracranial cryptococcosis in immunocompromised patients: CT and MR findings in 29 cases. AJNR Am J Neuroradiol. 1991;12:283–289. [PubMed] [PMC free article] [PubMed] [Google Scholar]
- 2.Caldemeyer Central Nervous System Cryptococcosis: Parenchymal Calcification and Large Gelatinous Pseudocysts. AJNR Am J Neuroradiol. 1997;18:107–109. [PubMed] [PMC free article] [PubMed] [Google Scholar]
- 3.Lu CH. Clinical Relevance of Intracranial Arterial Stenoses in Tuberculous and Cryptococcal Meningitis. Infection. 2007;35:359–363. doi: 10.1007/s15010-007-6263-0. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Leiguarda R, Berthier M, Starkstein S, Maques M, Lylyk P. Ischemic infarction in 25 children with tuberculous meningitis. Stroke. 1988;19:202–204. doi: 10.1161/01.str.19.2.200. [PubMed] [DOI] [PubMed] [Google Scholar]
- 5.Lan SH. Cerebral infarction in chronic meningitis: a comparison of tuberculous meningitis and cryptococcal meningitis. Q J Med. 2001;94:247–253. doi: 10.1093/qjmed/94.5.247. [PubMed] [DOI] [PubMed] [Google Scholar]
- 6.Bhargava S, Gupta AK, Tandon PN. Tuberculous meningitis: a CT scan study. Br J Radiol. 1982;55:189–196. doi: 10.1259/0007-1285-55-651-189. [PubMed] [DOI] [PubMed] [Google Scholar]


