Abstract
Idiopathic hypoparathyroidism can rarely present with extensive spondyloarthropathic changes that closely resemble ankylosing spondylitis, diffuse idiopathic skeletal hyperostosis, or fluorosis. Clinical presentation of the patient, typical laboratory parameters, and radiological findings aid in their differential diagnosis. Extensive spondyloarthropathy with normal sacroiliac joints in patients with neuromuscular symptoms like tetany, paresthesia, and hypocalcemia should raise the possibility of this entity.
Abbreviations: MRI, magnetic resonance imaging; US, ultrasound
Introduction
Idiopathic hypoparathyroidism is an uncommon endocrinopathy caused by insufficient secretion of parathormone (PTH). It is characterized by hypocalcemia, hyperphosphatemia, and low levels of PTH. It occurs in young females with a familial history. Usual radiological findings include generalized osteosclerosis, calvarial thickening, basal ganglia calcification, and hypoplastic dentition. Spondyloarthopathy mimicking ankylosing spondylitis is a rare skeletal manifestation. We report a case of long-standing hypoparathyroidism with this rare presentation.
Case report
A 48-year-old female presented with recurrent episodes of carpopedal spasm, starting at the age of 22. At that time, she was found to have hypocalcemia and was managed with calcium supplements, though she was irregular with calcium intake. She complained of neck and back stiffness for the past 8 years. She had a recent fall in the bathroom and sustained an intertrochanteric fracture of the right femur. She was treated with an internal fixator and was referred to our hospital for further investigation and treatment.
Physical examination of the woman revealed Chovstek’s sign, with neck and back stiffness. After a workup for metabolic bone disease, biochemical serum parameters revealed low calcium (7.3mg/100ml), high phosphate (6.2mg/100ml), very low PTH (<1.0 pg/ml), and normal magnesium (1.86mg/100ml). In view of the possibility of spondyloarthropathy, HLA B 27 was performed; it was negative.
After a skeletal survey, anteroposterior (AP) radiography of the pelvis showed ossification of iliolumbar ligaments at the lateral margin of the acetabulum and capsular calcification around the hip joints. Enthesopathic changes were seen at the muscular insertions of lesser trochanter and greater trochanter, ischial tuberosities, and iliac crests, with normal sacroiliac joints (Fig. 1). AP radiography of the thoracolumbar spine revealed extensive ossification of the interspinous and supraspinous ligaments, and a syndesmophyte formation (Fig. 2). Lateral radiography of the cervical spine showed ossification of the anterior longitudinal ligament and enthesopathic changes at the posterior elements (Fig. 3). AP radiography of the forearm bones demonstrated ossification of the interosseous membrane (Fig. 4). There was a generalized mild increase in the bone density. Computed tomography (CT) of sacroiliac joints was performed to rule out sacroilitis. It showed normal sacroiliac joints with ossification of iliolumbar ligaments, enthesopathic changes, and osteophytes at the superior and inferior margins of the sacroiliac joint (Figure 5, Figure 6). A plain CT scan of brain showed bilateral symmetric basal-ganglia calcification (Fig. 7).
Figure 1.
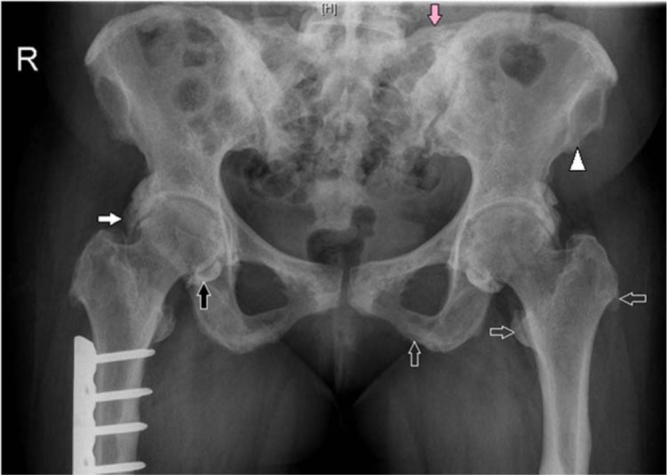
48-year old woman with idiopathic hypoparathyroidism. Anteroposterior (AP) radiograph of the pelvis shows mineralization of iliolumbar ligament (pink arrow), broad ossification at the lateral margin of acetabulum (white arrow), osseous proliferation and irregular bony excrescences above the acetabulum (arrowhead), and lesser and greater trochanters and ischial tuberosities (open arrows). Note the capsular calcification of the hip joint (black arrow) and internal fixator for the right femoral shaft fracture.
Figure 2.
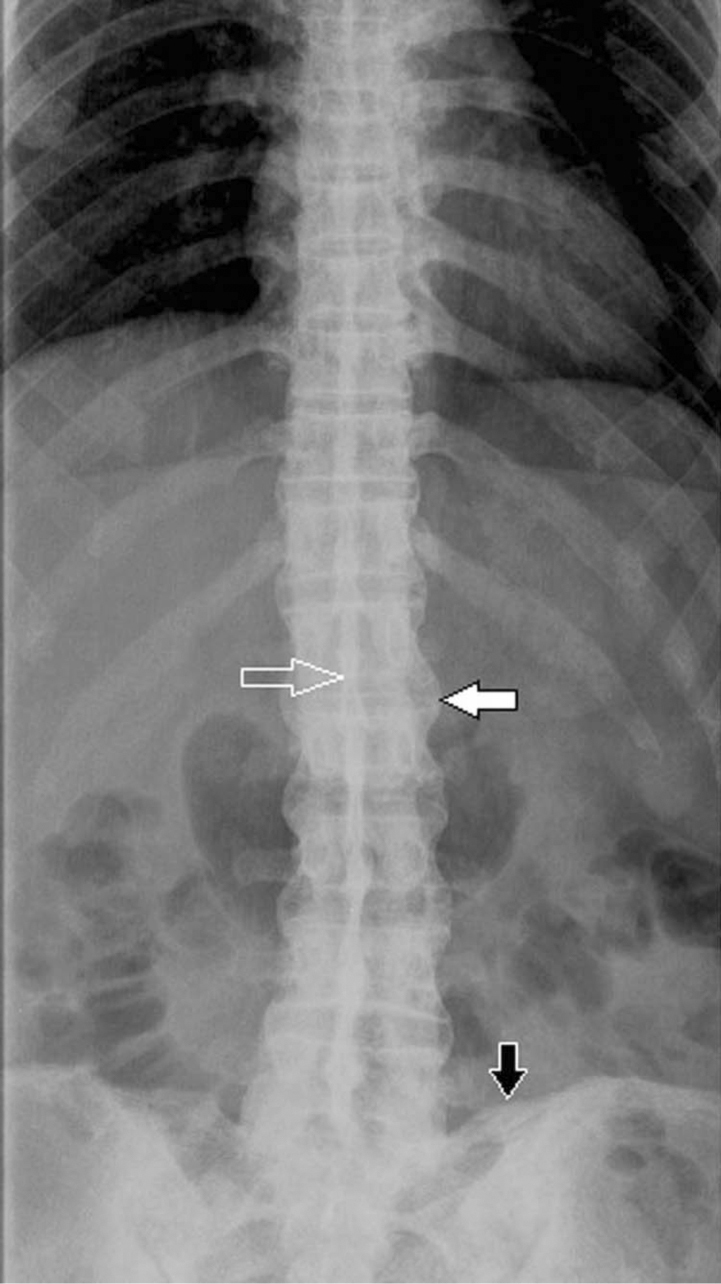
48-year old woman with idiopathic hypoparathyroidism. AP radiograph of the thoracolumbar spine shows ossification of interspinous ligament (open arrow) and syndesmophytes (white arrow). Note the ossification of iliolumbar ligament (black arrow).
Figure 3.
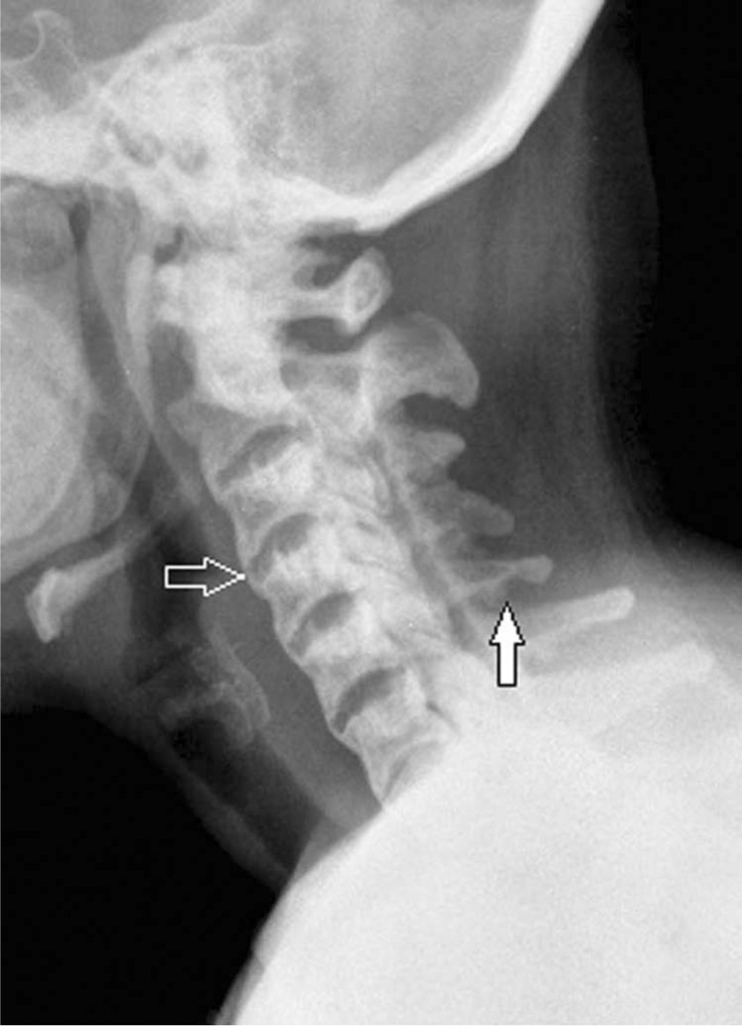
48-year old woman with idiopathic hypoparathyroidism. Lateral radiograph of the cervical spine shows ossification of the anterior longitudinal ligament (open arrow) and irregular bony excrescences at the inferior margin of the spinous process (white arrow). Note a mild diffuse increase in the bone density.
Figure 4.

48-year old woman with idiopathic hypoparathyroidism. AP radiograph of the forearm bones depicts ossification of the interosseous membrane (white arrow).
Figure 5.
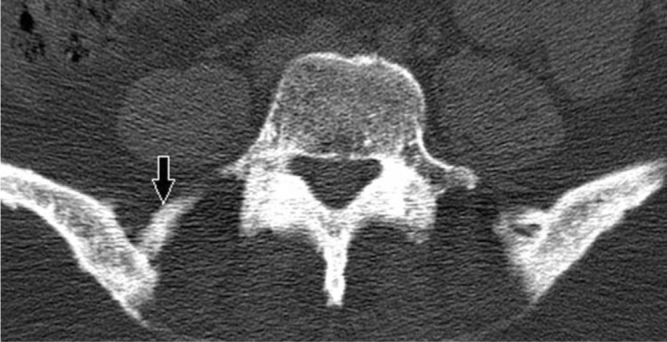
48-year old woman with idiopathic hypoparathyroidism. Axial CT of sacroiliac joint displays enthesopathic changes and the ossification of the iliolumbar ligament (black arrow).
Figure 6.
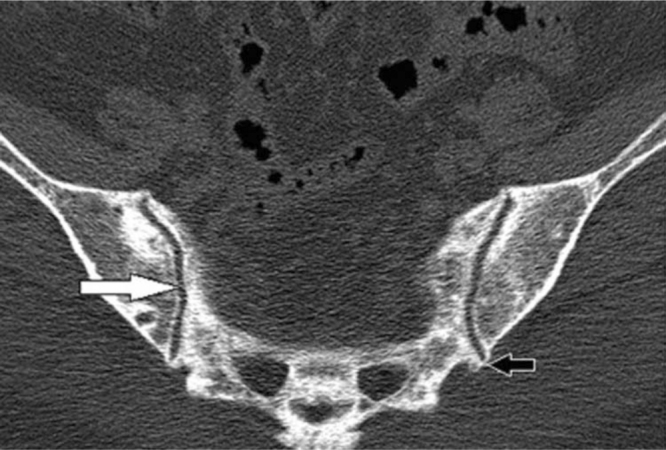
48-year old woman with idiopathic hypoparathyroidism. Axial CT of sacroiliac joints shows a normal sacroiliac joint (white arrow) with bridging calcification at the inferior margin of the joint (black arrow).
Figure 7.

48-year old woman with idiopathic hypoparathyroidism. Axial plain CT section of brain shows bilateral symmetrical basal-ganglia calcifications (white arrows).
Discussion
Hypoparathyroidism is an endocrine abnormality characterized by hypocalcemia and hyperphosphatemia with low PTH. In the majority of the cases, it is a complication of parathyroid surgery or a defective PTH receptor on the end organ as seen in pseudohypoparathyroidism. In rare cases, it can be idiopathic, which is thought to be autoimmune-related (1, 2). It clinically presents with neuromuscular signs and symptoms like tetany, carpopedal spasm, and paresthesia. Laboratory studies reveal hypocalcemia and hyperphosphatemia with low PTH in the serum. General radiological findings include generalized osteosclerosis, basal ganglia calcification, calvarial thickening, soft-tissue calcifications, and hypoplastic dentition (2).
Spondyloarthropathy is usually associated with long-standing hypoparathyroidsm (3, 4) as seen in our case. Spondyloarthropathy is often clinically occult, but patients may have radiological spondyloarthropathy in as high as 30% to 40% cases (5). Radiologically, spinal abnormalities include extensive bridging osteophytes and ossification of spinal ligaments, predominantly anterior and posterior longitudinal, interspinous, and supraspinous ligaments; these closely resemble ankylosing spondylitis and diffuse idiopathic skeletal hyperostosis (DISH) (1, 6, 7). Extraspinal abnormalities can be seen involving the pelvis and appendicular skeleton. The pelvis reveals ossification of sacrospinous, sacrotuberous, and iliolumbar ligaments, and ossification at the lateral margin of the acetabulum. Enthesopathic changes appear at various sites such as the lesser and greater trochanter, the iliac crest, and along the ischial tuberosities (1, 7, 8, 9). Sacroilitis is usually absent; however, Goswami R et al reported three cases of sacroilitis out of 40 cases (5). Clinically and radiologically, this condition closely simulates ankylosing spondylitis (6) and DISH (7, 8). The appendicular skeleton shows enthesopathic changes at various sites and interosseous membrane ossifications, which again can mimic fluorosis (1).
The clinical profile, biochemical parameters, and radiological features that aid in differential diagnosis also have a great bearing on patient management (5). In addition to back pain and stiffness, neuromuscular symptoms like muscle cramps, tetany, and carpopedal spasm are characteristic of idiopathic hypoparathyroidism and spondyloarthropathy but are absent in ankylosing spondylitis and DISH (5). Laboratory investigations reveal hypocalcemia with low PTH. HLA B27, ANA (antinuclear antibody), and C-reactive protein are typically within normal limits (5).
Spondyloarthopathy occurring in hypoparathyrodism usually spares the sacroiliac joint; this differentiates it from ankylosing spondylitis (5). Patients with DISH have no history of tetany or muscle cramps, and their biochemical parameters are within normal limits (1). Spondyloarthopathy with a long-standing history of vague neuromuscular symptoms in the setting of hypocalcemia and low PTH should raise the possibility of this entity.
Footnotes
Published: October 02, 2011
References
- 1.Resnick D., Kransdorf M.J. Bone and joint imaging. Elsevier; Philadelphia: 2005. [Google Scholar]
- 2.Youngwirth L., Benavidez J., Sippel R., Chen H. Parathyroid hormone deficiency after total thyroidectomy: incidence and time. J. Surg. Res. 2010;163(1):69–71. doi: 10.1016/j.jss.2010.03.059. [PubMed] Epub 2010. [DOI] [PubMed] [Google Scholar]
- 3.Takuwa Y., Matsumoto T., Kurokawa T. Calcium metabolism in paravertebral ligamentous ossification. Acta Endocrinol., (Copenh.) 1985;109(3):428–432. doi: 10.1530/acta.0.1090428. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Chaykin L.B., Frame B., Spondylitis J.W. a clue to hypoparathyroidism. Ann. Intern. Med. 1969;70(5):995–1000. doi: 10.7326/0003-4819-70-5-995. [PubMed] [DOI] [PubMed] [Google Scholar]
- 5.Goswami R., Ray D., Sharma R. Presence of spondyloarthropathy and its clinical profile in patients with hypoparathyroidism. Clin. Endocrinol., (Oxf.) 2008;68(2):258–263. doi: 10.1111/j.1365-2265.2007.03032.x. [PubMed] Epub 2007. [DOI] [PubMed] [Google Scholar]
- 6.Korkmaz C., Yasar S., Binboga A. Hypoparathyroidism simulating ankylosing spondylitis. Joint Bone Spine. 2005;72(1):89–91. doi: 10.1016/j.jbspin.2004.08.004. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Unverdi Selman, Ozturk M.D. Idiopathic hypoparathyroidism mimicking diffuse idiopathic skeletal hyperostosis. Journal of Clinical Rheumatology. 2009;15(7):361–362. doi: 10.1097/RHU.0b013e3181bb9865. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Haller J., Resnick D., Miller C.W. Diffuse idiopathic skeletal hyperostosis: diagnostic significance of radiographic abnormalities of the pelvis. Radiology. 1989;172(3):835–839. doi: 10.1148/radiology.172.3.2788894. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.Okazaki T., Takuwa Y., Yamamoto M. Ossification of the paravertebral ligaments: a frequent complication of hypoparathyroidism. Metabolism. 1984;33:710–713. doi: 10.1016/0026-0495(84)90209-9. [PubMed] [DOI] [PubMed] [Google Scholar]


