Abstract
Action Learning Collaboratives (ALCs), whereby teams apply quality improvement (QI) tools and methods, have successfully improved patient care delivery and outcomes. We adapted and tested the ALC model as a community-based obesity prevention intervention focused on physical activity and healthy eating.
Methods
The intervention used QI tools (e.g., progress monitoring) and team-based activities and was implemented in three communities through 9 monthly meetings. To assess process and outcomes, we used a longitudinal repeated-measures and mixed-methods triangulation approach with a quasi-experimental design including objective measures at three time points.
Results
Most of the 97 participants were female (85.4%), White (93.8%), and non-Hispanic/Latino (95.9%). Average age was 52 years; 28.0% had annual household income of $20,000 or less; mean body mass index was 35. Through mixed-effects models, we found some physical activity outcomes improved. Other outcomes did not significantly change. Although participants favorably viewed the QI tools, components of the QI process such as sharing goals and data on progress in teams and during meetings were limited. Participants’ requests for more education or activities around physical activity and healthy eating, rather than progress monitoring and data sharing required for QI activities challenged ALC model implementation.
Conclusions
An ALC model for community-based obesity prevention may be more effective when applied to pre-existing teams in community-based organizations.
Keywords: Physical Activity, Obesity, Community, Intervention, Learning Collaborative, Quality Improvement
Introduction
Programs for applying evidence-based interventions to improve cardiovascular health and fitness at the community level continue to evolve as more rigor is demanded regarding outcomes (Khan et al., 2009). Recent reviews suggest that programs that focus on self-monitoring of food intake, exercise, and weight might achieve better outcomes (Burke, Swigart, Turk, Derro, & Ewing, 2009; Burke, Wang, & Sevick, 2011; Pearson, 2012). In addition, social support (Hart, Einav, Weingarten, & Stein, 1990; Wing & Jeffery, 1999) and goal setting (Pearson, 2012), along with specific plans to reach goals (Benyamini et al., 2013), appear to improve outcomes related to weight, food intake and exercise.
One potential model for systematically supporting planning, goal-setting, self-monitoring, tracking outcomes, and social support in community settings is the Action Learning Collaborative (ALC). ALCs, which have been successfully applied in health care and other organizational settings to improve health outcomes (Malenka et al., 2005; O’Connor et al., 1996), involve team-based learning using quality improvement (QI) tools and methods to “bring about organizational or systemic change” (Bazos et al., 2013). Modeled on the Institute for Healthcare Improvement’s Breakthrough Series Collaborative (Institute for Healthcare Improvement, 2003), teams use an experiential and iterative process to set goals, develop a plan to achieve goals, learn QI tools for data collection to monitor progress, and share results with other team members to set new goals or revise goals. ALCs have been used mostly in healthcare settings, but are starting to be used in community-based organizations and for public health topics (Bazos et al., 2013; Mozaffarian et al., 2010).
Given the success of the ALC model in improving outcomes and evidence that aspects of the ALC model (e.g., goal-setting, monitoring, tracking outcomes, team-based activities) support individual improvement in physical activity and/or healthy eating (Benyamini et al., 2013; Burke et al., 2009; Burke et al., 2011; Hart et al., 1990; Pearson, 2012; Wing & Jeffery, 1999), we sought to adapt and test the ALC model for community members in a community-based intervention. This paper examines the applicability of an ALC model as an intervention to promote physical activity and healthy eating in community-based settings.
Background
The Prevention Research Center (PRC) at Dartmouth focuses on improving cardiovascular health of residents in New Hampshire and Vermont in three communities (one rural location, one town, one city). Leaders of the three communities’ health coalitions agreed to participate as the vision of the PRC aligned well with the mission and vision of their respective coalitions, all of which had been in existence for at least five years prior to the initiation of the PRC. Initially, the primary mechanism to develop, test and revise intervention approaches related to improving heart health was at the community leadership and organization levels through ALCs, including a worksite intervention to improve vending options, a walkability assessment resulting in recommendations to city planners, and creation of a wallet blood pressure card for patients (Bazos et al., 2013). Given the success of the ALC model at these community organization levels, we sought to adapt and test the ALC model for community members in a community-based intervention focused on individual improvement in physical activity and/or healthy eating. Our model, called InSHAPE® Together (IST), focused on physical activity and nutrition for vulnerable populations in the three participating communities, including individuals who have low incomes or education, live in rural or under-resourced areas, and were not meeting recommended levels of physical activity as defined by the 2008 Physical Activity Guidelines for Americans (U.S. Department of Health and Human Services, 2008). In collaboration with community partners, we modified components of the ALC model, including QI concepts and tools, to be relevant for community settings and community members, and focused the intervention on teams in an effort to increase social support for participating individuals.
Methods
We used a longitudinal repeated-measures and mixed-methods triangulation approach (Schifferdecker & Reed, 2009) with a quasi-experimental design to assess process and outcomes. The research protocol was reviewed and approved by Dartmouth College’s Committee for the Protection of Human Subjects. Participants completed informed consent procedures and parents of minors provided consent while minors provided assent prior to participation. A full description of the IST intervention, study communities and study design are described in more detail elsewhere (Bazos et al., 2013). However, we provide a brief summary below.
Intervention
The study was conducted from July 2012 through April 2013 in three community sites (one rural location, one town, one city). The intervention involved nine monthly ALC meetings (each lasting 90 minutes) with community participants (n=96) led by local project coordinators and physical activity and nutrition experts. Participants had the option to attend team-based activities in between ALC meetings. The IST curriculum was designed with the local community health coalition leaders, coordinators and physical activity and nutrition experts, all who lived and worked in their community settings, to adapt the ALC model. The IST curriculum included the following: teaching about the QI process and tools, team formation and learning, content and experiential learning around physical activity and healthy eating, individual goal setting, and team support and monitoring of goals. Across the three communities, ALC meetings followed the same overall framework but were adapted locally to account for the different contexts and the goals and learning needs of participants. Examples of adaptations included taking advantage of facilities available in the local area (e.g., parks, walking paths, farmer’s market, etc.) or planning activities in sessions based on questions asked by participants (e.g., demonstrating use of an exercise band). Participants were also offered an activity log to track daily minutes of moderate and vigorous activity, as well as a food intake log based on current dietary guidelines from the United States Department of Agriculture (United States Department of Agriculture, 2014) as tools to support monitoring of goals. In addition, participants received a wearable portable activity monitor (KAM©)(KershWellness) at the start of the project with instructions and technical support on proper wearing, interpretation of data and reports, and device use for goal-setting and tracking.
Participants
Participants were eligible to participate if they were at least 12 years old, not pregnant, were inactive or low-activity by government standards (U.S. Department of Health and Human Services, 2008) for engagement in physical activities (i.e., exercised less than 3 times per week), and had medical clearance to participate. Recruitment occurred through advertisements in local newspapers, neighborhood watch meetings, faith-based and community action groups, and general distribution of fliers around community venues.
Measures
Measures included process and outcome measures. Outcome measures were obtained through three measurement sessions: pretest (prior to first ALC), Posttest 1 (Month 4), and Posttest 2 (Month 9). A cash incentive per session ($25 at pretest and Posttest 1; $30 at Posttest 2) was offered to those who attended. At each session, trained administrators obtained height and weight measurements, conducted a 6-minute walk test, and monitored a participant survey (paper-and-pencil survey) of activity levels, fruit and vegetable consumption, sense of community, and demographics (age, gender, race, ethnicity, marital status, education level, annual household income). Process measures were obtained through end-of-project focus groups in each community and end-of-project survey questions added to the Posttest 2 survey. Details on measures and data collection are provided below.
Height and weight
We calculated body mass index (BMI) from height and weight measurements. Trained administrators obtained height and weight measures using the PhenX Toolkit version July 29, 2011 Version 4.5 adult protocol for standing height (protocol ID 020703) with the modification that we used a wall chart instead of a stadiometer and measured weight (protocol ID 021501) with the modification that wearing clothes was permitted (Hamilton et al., 2011).
Six-minute walk test
We used a 6-minute walk test to assess cardiorespiratory fitness, a performance-based measure of exercise capacity. The six-minute walk test protocol was adapted from the procedures recommended by the American Thoracic Society (Crapo et al., 2002; Enright, 2003). We asked participants to walk a measured distance as far as they were able in 6 minutes. In this test, participants walk as many 100-foot laps (e.g., as marked by cones in a hallway) as they are able. The number of total feet walked calculated from the sum of the number of full laps plus the number of feet walked in the final, partial lap is treated as the outcome measure. This low-risk test has been used successfully in sedentary individuals with chronic disorders and is well tolerated in populations with high sedentary behavior (Crapo et al., 2002; Enright, 2003).
Survey
We gave participants a self-administered paper-and-pencil survey at each of the three measurement sessions. Survey questions, based largely on well-known and validated measures, included the following items: physical activity (vigorous, moderate, walking) and sedentary behavior (9 items; number of days per week or hours per day) (Craig et al., 2003; Eaton et al., 2012; Hoelscher, Day, Kelder, & Ward, 2003). We asked about self-confidence (3 items; 5-point scale), barriers to physical activity (15 items; 5-point scale) (Forsyth A, Schmitz K, & Oakes M, 2003; Forsyth, Oakes, & Schmitz, 2009), and social support for exercise (5 items; 5-point scale) (Sallis, Grossman, Pinski, Patterson, & Nader, 1987). Regarding eating habits, we asked about fruit and vegetable intake, fruit juice, and other sugary drink intake from the past day based on current dietary guidelines from the United States Department of Agriculture (United States Department of Agriculture, 2014) and from previously validated studies (5 items; 5-point scale) (Hoelscher et al., 2003; Lytle et al., 1993). We also asked about average hours of screen time (television or movies, video games, Internet) in an average day (1 item; 7-point scale) (Eaton et al., 2012) and sense of community (11 items; 5-point scale)(Chavis D, 2008). For multi-item assessments, such as barriers to physical activity that contained 15 items, we created summary scores to use in the multivariate analysis described below.
End-of-project focus groups
Three focus groups (one per community) were conducted with six to eight ALC participants per group to gather impressions about the effectiveness of IST curricular elements and barriers and enablers to any improvements. Participants were selected at random from a list of interested individuals and focus groups were held in each community to facilitate participation. All focus groups were conducted within a one-month period towards the end of the intervention by one facilitator who was not involved with the interventions. Conversations were recorded and transcribed, and those attending were offered a $30 gift card.
End-of-project survey questions
Participants were asked to rate specific program elements of IST (e.g. use of daily logs, KAM team participation and function) with the following response categories on the Posttest 2 survey: did not do, not at all, moderately, extremely. These responses were postcoded with a range of 0 to 3, where the response category of “did not do” was coded as a 0 and “extremely” was coded as a 3.
Analysis
Quantitative Data (Biometrics, 6-Minute Walk Test, surveys)
Data were entered into Excel and then imported into SPSS (IBM Corp., 2011) for cleaning and verification. Cleaned data were imported from SPSS to SAS (SAS Institute, 2011). To compare means of participant characteristics we used SPSS (IBM Corp., 2011) to calculate ANOVAs. To examine outcomes, we used mixed-effects models using SAS (SAS Institute, 2011) to account for the correlation between the three time points. We assumed that data were missing at random. We controlled for ALC group, age, gender, education, and household income. Both 4-month and 9-month assessments were considered as posttest measurements in the analysis where we assumed that the effect of the intervention remains stable from 4-month to 9-month. The mixed-model approach takes into account when any of the two posttest measurements was missing and generates unbiased estimates as long as the missing occurred at random. We also checked for interactions with BMI by doing two interaction models: with baseline BMI (with a cutoff at obese) and BMI trajectory (increased from pretest to Posttest 1 or not). We used a Bonferroni correction to adjust for comparisons. End-of-project survey data were entered into Excel and then imported into SPSS (IBM Corp., 2011) for cleaning and descriptive summaries.
Qualitative Data
Narratives from focus group transcripts and open-ended survey responses were collated and examined using a grounded theory technique (Glaser B & Strauss A, 1967), in which themes are drawn from the text during frequent comparative analysis of the data. When relevant, qualitative data were triangulated with survey responses to compare results for further exploration of the results.
Results
Sample
The primary sample characteristics and descriptive statistics are reported in Table 1. At pretest, 97 people consented to participate in the study and completed the pretest assessment. Most of the 97 participants were female (85.4%), White (93.8%), and non-Hispanic/Latino (95.9%). Participant average age was 52 years (range 12–86). Mean pretest adult BMI was 35, and 28.0% had annual household income of $20,000 or less. At Posttest 1, 70 (72%) enrolled participants completed the assessment and at Posttest 2, 61 (63%) enrolled participants completed the assessment. We used ANOVA to compare means between those who completed Posttest 1 and Posttest 2 assessments and those who did not on age, gender, race, ethnicity, marital status, education, and annual household income. There were significant differences for only one characteristic: age. Those who completed Posttest 1 and Posttest 2 assessments were significantly older compared to those who did not: mean age 53.8 years versus 45.9 years, F(1,94)=4.5, p=0.036, and 54.5 years versus 46.7 years, F(1,94)=5.1, p=0.027, respectively).
Table 1.
Characteristics of participants in the InSHAPE® Together program
| Characteristic | Pretest (N=97 unless otherwise noted) |
Posttest 1 (N=70 unless otherwise noted) |
Posttest 2 (N=61 unless otherwise noted) |
|||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Age (N = 96 at pretest; N=69 at Posttest 1) | ||||||
| Age (M ± SD) | 51.6±16.8 | 53.8±15.1 | 54.5±14.8 | |||
| Gender (N=96 at pretest; N=69 at Posttest 1; N=60 at Posttest 2) | ||||||
| Female | 82 | 84.5 | 58 | 84.1 | 51 | 83.6 |
| Race | ||||||
| White | 91 | 93.8 | 67 | 95.7 | 58 | 95.1 |
| Ethnicity | ||||||
| Non-Latino | 93 | 93.9 | 68 | 97.1 | 59 | 96.7 |
| Marital status | ||||||
| Married | 49 | 50.5 | 33 | 47.1 | 28 | 45.9 |
| Widowed | 7 | 7.2 | 7 | 10.0 | 7 | 11.5 |
| Living with significant other | 8 | 8.2 | 6 | 8.6 | 4 | 6.6 |
| Single (never married) | 18 | 18.6 | 12 | 17.1 | 11 | 18.0 |
| Divorced/separated | 14 | 14.4 | 11 | 15.7 | 10 | 16.4 |
| Civil union/domestic partner | 1 | 1.0 | 1 | 1.4 | 1 | 1.6 |
| Education | ||||||
| Less than high school | 7 | 7.2 | 4 | 5.7 | 4 | 6.6 |
| Graduated from high school or GED | 23 | 23.7 | 19 | 27.1 | 16 | 26.2 |
| Some college or technical school | 25 | 25.8 | 17 | 24.3 | 12 | 19.7 |
| Graduated from college | 30 | 30.9 | 22 | 31.4 | 22 | 36.1 |
| Postgraduate school or degree | 12 | 12.4 | 8 | 11.4 | 7 | 11.5 |
| Annual household income (N=93 at pre-test; N=66 at post-test 1; N=58 at post-test 2) | ||||||
| $20,000 or less | 26 | 26.8 | 24 | 34.3 | 21 | 34.4 |
| $20,001 to $40,000 | 17 | 17.5 | 12 | 17.1 | 11 | 18.0 |
| $40,001 to $60,000 | 17 | 17.5 | 11 | 15.7 | 11 | 18.0 |
| $60,001 to $80,000 | 8 | 8.2 | 4 | 5.7 | 3 | 4.9 |
| $80,001 to $100,000 | 4 | 4.1 | 2 | 2.9 | 2 | 3.3 |
| $100,000 or more | 5 | 5.2 | 5 | 7.1 | 5 | 8.2 |
| Don’t know/not sure | 16 | 16.5 | 8 | 11.4 | 5 | 8.2 |
Note: percentages are based upon the sample size noted at the top of each time period; some characteristics do not add to 100% due to missing data.
Twenty individuals from our main sample participated in one of the three focus groups that were conducted (one in each community). Participant average age was 58 years, 90% were female and 35% reported an annual household income of $20,000 or less. A majority (65%) were employed at the time of the groups, and almost half of them had a college or post-graduate degree. Most of them were part of small households, of three or fewer members, and all were White.
Intervention Dropouts
Over the course of the program, project coordinators from each community site notified us when a participant either decided to withdraw or was unreachable after missing two consecutive ALC meetings. In both cases, the participant was considered a dropout. We tried to contact each of the 29 dropouts (up to three times by phone and up to three times by e-mail, if available) to conduct a dropout interview. We were able to reach 17 (58.6%) of the dropouts. The primary reason given for dropping out was not having enough time (N=10). Two people talked about not feeling well, which prevented them from attending early sessions, which then led to their dropping out of the intervention entirely. Given that the primary reason for intervention dropout was not directly associated with our measured outcomes, we categorized our missing data from the measurement sessions as missing at random.
Outcome Measures
Descriptive results of each metric are reported in Table 2. Compared to the pretest fitness measures, physical activity and barriers to physical activity significantly improved at Posttests 1 and 2 (Table 3). For example, after participating in the intervention, participants increased their distance walked in 6 minutes by an average of 99.6 feet, and on surveys reported an increase in the number of days of vigorous and moderate activity by almost a day (0.7 day). After the Bonferroni correction, number of days per week walked at least 10 minutes and number of days engaged in intense physical activity for at least 20 minutes remained statistically significant.
Table 2.
Body mass index and health behavior outcomes from InSHAPE® Together program – Descriptive results
| Pretest (N=97 unless otherwise noted) (M±SD) |
Posttest 1 (N=70 unless otherwise noted) (M±SD) |
Posttest 2 (N=61 unless otherwise noted) (M±SD) |
|
|---|---|---|---|
| Outcomes | |||
| Body mass index | 34.2±9.5 | 33.3±9.5 | 32.4±9.2 |
| Physical activity | |||
| Distance walked in 6 minutes (N=69 at Posttest 1) | 1414.5±299.9 | 1508.6±326.0 | 1519.0±329.0 |
| # days vigorous activity past week (N=96 at pretest 1; N=69 at Posttest 1; N=60 at Posttest 2) | 1.4±1.6 | 2.0±2.0 | 2.3±2.1 |
| # days moderate activity past week (N=93 at pretest 1; N=68 at Posttest 1; N=60 at Posttest 2) | 2.5±2.2 | 3.2±2.5 | 3.4±2.3 |
| # days walked at least 10 minutes per week (N=96 at pretest 1; N=68 at Posttest 1; N=59 at Posttest 2) | 3.9±2.5 | 4.8±2.2 | 5.0±2.4 |
| # days intense physical activity for at least 20 minutes (N=93 at pretest 1; N=69 at Posttest 1; N=60 at Posttest 2) | 1.4±1.8 | 2.4±2.3 | 2.6±2.3 |
| # days intense physical activity for at least 60 minutes (N=88 at pretest 1; N=66 at Posttest 1; N=58 at Posttest 2) | 0.5±1.2 | 1.0±1.8 | 1.3±2.1 |
| Social support for exercise (N=68 at Posttest 1) | 17.6±4.6 | 17.3±4.8 | 17.6±4.0 |
| Self-confidence for vigorous activity (N=69 at Posttest 1) | 7.7±2.7 | 8.3±2.5 | 8.4±2.9 |
| Barriers to physical activity scale (N=68 at Posttest 1) | 44.8±10.0 | 42.0±11.1 | 40.3±10.5 |
| Sedentary activity | |||
| Hours of screen time in an average day (N=95 at pretest 1; N=69 at Posttest 1) | 4.4±1.5 | 4.0±1.6 | 4.0±1.5 |
| Fruit and vegetable consumption | |||
| Frequency of meals in the past day that were at least half fruits & vegetables (N=69 at Posttest 1) | 2.8±1.2 | 3.0±1.2 | 3.0±1.2 |
| Frequency of eating vegetables the day before (N=69 at Posttest 1) | 2.8±1.2 | 3.2±1.3 | 3.1±1.2 |
| Frequency of eating fruit the day before (N=96 at pretest 1; N=69 at Posttest 1) | 2.6±1.1 | 2.7±1.4 | 2.8±1.3 |
| Sense of community scale (N=68 at Posttest 1) | 39.6±6.6 | 38.3±6.1 | 39.3±7.0 |
Table 3.
Body mass index and health behavior outcomes from InSHAPE® Together program – mixed effects model
| Outcomes | Number of observations used1 | Estimate2 | p-value3 |
|---|---|---|---|
| Body mass index | 214 | −0.756 | 0.526 |
| Physical activity | |||
| Distance walked in 6 minutes | 214 | 99.634 | 0.013 |
| # days vigorous activity past week | 211 | 0.682 | 0.008 |
| # days moderate activity past week | 207 | 0.728 | 0.024 |
| # days walked at least 10 minutes per week | 209 | 1.012 | 0.003 |
| # days intense physical activity for at least 20 minutes | 208 | 1.113 | 0.0002 |
| # days intense physical activity for at least 60 minutes | 198 | 0.582 | 0.017 |
| Social support for exercise | 212 | −0.340 | 0.590 |
| Self-confidence for vigorous activity | 213 | 0.620 | 0.099 |
| Barriers to physical activity scale | 213 | −3.349 | 0.017 |
| Sedentary activity | |||
| Hours of screen time in an average day | 211 | −0.388 | 0.058 |
| Fruit and vegetable consumption | |||
| Frequency of meals in the past day that were at least half fruits & vegetables | 212 | 0.154 | 0.349 |
| Frequency of eating vegetables the day before | 213 | 0.257 | 0.123 |
| Frequency of eating fruit the day before | 212 | 0.171 | 0.329 |
| Sense of community scale | 212 | −0.977 | 0.276 |
The number of observations used includes all of the available data points from the three measurement sessions (pretest, Posttest 1, Posttest 2).
Estimates from each individual mixed effects model are shown. Each model controlled for: ALC group, age, gender, education, and household income.
We used a Bonferroni correction to adjust for the 15 comparisons, which put the p-value threshold at 0.003.
Outcomes in other areas, including BMI, eating habits, and social support were mixed. The interaction models using the baseline BMI (dichotomized into <=30 and >30 [obese]) and the BMI trajectory (BMI increased or not) did not show significant differences in BMI over time. Eating habits improved for fruit and vegetable consumption, and amount of screen time (a measure of sedentary behavior) decreased in an average weekday. However, neither of these changes were statistically significant. Similarly, social support for exercise, self-confidence for vigorous activity, and sense of community did not significantly change over time.
Process Measures
After triangulating data from the focus groups (n=20 participants) and end-of-project survey questions, results suggested that participants engaged in and appreciated a number of aspects of the ALC model. Focus group participants described successes in terms of making connections with other participants, gaining knowledge and motivation, using QI methods, having access to experts in nutrition and physical activity, and achieving personal successes (e.g., avoiding holiday weight gain, learning how to shop at the grocery store, losing weight). Similar findings were revealed in the final posttest survey, where most participants reported that they set goals for themselves at least sometimes (91.8%), tracked whether they were reaching their goals at least sometimes (86.2%), and reported that ALC meetings, setting goals, planning steps to achieve their goals, and tracking progress towards their goals with the KAM activity monitor were moderately to extremely useful (see Figure 1). The means and standard deviations of the categories shown in Figure 1 were as follows: monthly ALC meetings (M 2.4 ± SD 0.7); making goals (2.2 ± 0.8); planning steps to achieve your goals (2.1 ± 0.8); keeping track of progress towards your goals with your KAM (1.9 ± 0.8); keeping track of progress towards your goals with paper logs (1.4 ± 1.0). In thinking about the overall IST program, participants rated program staff (93.4%) and other IST participants (82.0%) as being moderately to extremely supportive and these sentiments were repeated in focus group participants’ reports as well.
Figure 1.
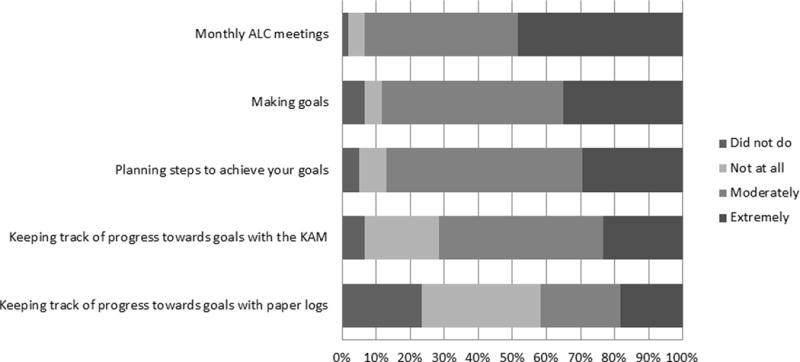
Respondent Reports of Usefulness of Different Elements of InSHAPE® Together
At the same time, some components of the ALC model were not fully realized. Although a majority of the participants (57%) became part of a team, focus group results indicated that most of the teams were not actively meeting or communicating between ALC meetings. A number of focus group participants indicated that they were not part of a team because of conflicting schedules or distance from each other and that the time and structure for team formation in ALC meetings was inadequate. Similarly although 71% of survey respondents indicated that the KAM was at least moderately useful for tracking progress towards their goals (Figure 1), focus group participants expressed mixed experiences, including technical or practical problems (e.g., proper wearing position too uncomfortable with bending or other work, accidently washing the device) that interfered with consistent use. Focus group results also suggested that while ALC meetings were packed with activities and information, participants preferred to focus on topics about physical activity and healthy eating rather than about improvement-oriented tools and activities. They also desired increased accountability, more frequent meetings, and teams formed around specific characteristics (e.g., work schedule, address, ability, activity interests).
Discussion
This community-based program yielded mixed results for the use of an ALC model to promote improvements in physical activity and healthy eating in community settings. The model as adapted here included key components shown to be successful for weight loss, most notably goal setting, planning steps, data monitoring and social support, and resulted in some positive changes in physical activity levels over a 9-month period. In addition, barriers to physical activity decreased and positive though not statistically significant improvements in fruit and vegetable consumption were reported. In addition, participants provided positive feedback on a number of the program components.
At the same time, a number of participants did not complete the entire program and some components of the ALC model were not fully realized, which may explain the mixed results. In the traditional ALC model, the lever for change is at the team rather than individual level. While participants in our study enrolled to address personal activity and healthy eating goals, the expectation for team participation was made at the outset though few individuals knew each other when joining. Despite efforts taken in early sessions to find common interests and form teams, only a few active teams formed at each site, compromising the sharing of team-level processes and improvements that are a focus of the QI approach in ALCs. In addition, over the course of the program, technical assistance for nutrition and physical activity appeared to support and assist individual improvement efforts more than team efforts during and between ALC meetings. Lack of active teams may have limited the degree to which peer learning and dynamics could enhance accountability and social support for making behavior change.
Another challenge in translating the ALC model to health improvements in community settings occurred with the use of data for setting goals and monitoring progress. The community teams responsible for running the ALC meetings discussed challenges with the following aspects related to data: 1) supporting participants with numeracy challenges (e.g., understanding KAM data); 2) assisting participants in creating relevant and basic QI tracking methods; 3) needing to respond to the desire and requests by participants to focus a majority of the ALC meetings on education or activities around exercise and healthy eating rather than reviewing goals, sharing data and setting new goals; and 4) creating an atmosphere in which participants felt comfortable sharing personal data.
Limitations
Our analysis was limited to those who attended the three measurement sessions. Recruitment at each location was labor-intensive. As a pilot study, we did not have adequate resources to overcome this challenge. Future studies should include a wait-list control group for comparison. We used a proxy measure of sedentary behavior because our primary measure to capture it, although based on a standardized instrument (the International Physical Activity Questionnaire) (Craig et al., 2003), had too many out-of-bounds responses. It is possible that participants decreased their sedentary behavior beyond what we could approximate. This study was only conducted in three communities, which limits generalizability. Dropout in our study also limits generalizability; over one-third of the original participants did not complete Posttest 2 assessments. Although we did not see significant differences between those who completed Posttest 1 and Posttest 2 assessments and those who did not on gender, race, ethnicity, marital status, education, or annual household income, another possible limitation of our study was that participants who completed Posttest 1 and Posttest 2 assessments were significantly older compared to those who did not. In both cases this age difference was less than a decade (eight years). If such a difference is clinically relevant to the point that those who participated would have declined in their levels of physical activity due to age, it is possible that our findings underestimate the potential impact of this intervention. Alternatively, future studies could examine the possibility that this intervention may be more helpful to older compared to younger adults. Finally, it is possible that perceived lack of time to participate in the intervention could reflect a similar perception or inability to have time for physical activity, which was a directly measured outcome. We also hope to carefully measure likelihood of this latter possibility in future studies to better understand the extent to which it may or may not have affected our results.
Recommendations
Our community-based ALC model yielded some results to support changes in physical activity and healthy eating. However two important components of the ALC model proved difficult to implement in a community setting: team formation and personal data collection and tracking. Given these findings and review of other community-based programs, we recommend the following changes to the adapted ALC model for future implementation and testing:
Recruit preformed teams or dedicate more time to team formation based on factors that may support success, such as similar work schedules, age and interests, wellness goals, or proximity (e.g., work/live in same neighborhood)
Establish clearer expectations and support for team meetings between ALC sessions. Support may include time to schedule meetings during ALC sessions, having program staff attend to provide additional coaching in tracking and reporting of personal data, and offering incentives for teams to meet.
Consider more frequent meetings or longer meetings to provide adequate time for QI components (i.e., sharing of data) while still offering specific content about healthy eating and physical activity.
Use time in early meetings to help participants choose or design preferred tracking systems, including option to use the type of activity monitor (e.g., pedometer, FitBit, paper-based log) that best matches personal preferences, activity goals and numeracy skills to ensure a good fit.
In conclusion, an ALC model may work best at the level of organizations and organizational change to design and promote higher level community-based efforts, such as creating policy and environmental conditions supportive to increasing physical activity and healthier eating. Communities should consider resources and the level at which they wish to address a health issue when considering implementing an Action Learning Collaborative.
Acknowledgments
This work was supported by the Centers for Disease Control and Prevention #U48DP001935 and #U48DP005018 and the Department of Health and Human Services Public Health Training Center Grant #UB6HP20157. The authors wish to thank our community leader partners Rudy Fedrizzi, Jaime Hoebeke, Laural Ruggles, Anna Thomas and Yvonne Goldsberry, whose participation and support made this study possible, and the community-based implementation and research teams who partnered with us to implement and measure the project. Thank you to Inger Imset for coordinating the training and measurement sessions. We are especially grateful to the community participants who partnered with us in this research.
References
- Bazos DA, Schifferdecker KE, Fedrizzi R, Hoebeke J, Ruggles L, Goldsberry Y. Action-Learning Collaboratives as a Platform for Community-Based Participatory Research to Advance Obesity Prevention. Journal of Health Care for the Poor and Underserved. 2013;24(2):61–79. doi: 10.1353/hpu.2013.0104. [DOI] [PubMed] [Google Scholar]
- Benyamini Y, Geron R, Steinberg DM, Medini N, Valinsky L, Endevelt R. A Structured Intentions and Action-Planning Intervention Improves Weight Loss Outcomes in a Group Weight Loss Program. American Journal of Health Promotion. 2013;28(2):119–127. doi: 10.4278/Ajhp.120727-Quan-365. [DOI] [PubMed] [Google Scholar]
- Burke LE, Swigart V, Turk MW, Derro N, Ewing LJ. Experiences of Self-Monitoring: Successes and Struggles During Treatment for Weight Loss. Qualitative Health Research. 2009;19(6):815–828. doi: 10.1177/1049732309335395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke LE, Wang J, Sevick MA. Self-Monitoring in Weight Loss: A Systematic Review of the Literature. Journal of the American Dietetic Association. 2011;111(1):92–102. doi: 10.1016/J.Jada.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavis D, L K, Acosta J. The Sense of Community (SCI) Revised: The Reliability and Validity of the SCI-2. Paper presented at the Paper presented at: 2nd International Community Psychology Conference; Lisboa, Portugal. 2008. [Google Scholar]
- Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Oja P. International physical activity questionnaire: 12-country reliability and validity. Medicine and Science in Sports and Exercise. 2003;35(8):1381–1395. doi: 10.1249/01.Mss.0000078924.61453.Fb. [DOI] [PubMed] [Google Scholar]
- Crapo RO, Casaburi R, Coates AL, Enright PL, MacIntyre NR, McKay RT, Comm A. ATS statement: Guidelines for the six-minute walk test. American Journal of Respiratory and Critical Care Medicine. 2002;166(1):111–117. doi: 10.1164/Rccm.166/1/111. [DOI] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Flint KH, Hawkins J, Wechsler H. Youth risk behavior surveillance - United States, 2011. MMWR Surveill Summ. 2012;61(4):1–162. [PubMed] [Google Scholar]
- Enright PL. The six-minute walk test. Respir Care. 2003;48(8):783–785. [PubMed] [Google Scholar]
- Forsyth A, Schmitz K, Oakes M. Twin Cities Walking Survey. 2003 doi: 10.1123/jpah.6.1.119. Retrieved 3/5/14 from http://activelivingresearch.org/node/10619. [DOI] [PubMed]
- Forsyth A, Oakes JM, Schmitz KH. Test-Retest Reliability of the Twin Cities Walking Survey. Journal of Physical Activity & Health. 2009;6(1):119–131. doi: 10.1123/jpah.6.1.119. [DOI] [PubMed] [Google Scholar]
- Glaser B, Strauss A. Discovery of Grounded Theory Strategies for Qualitative Research. Chicago: Aldine Pub. Co.; 1967. [Google Scholar]
- Hamilton CM, Strader LC, Pratt JG, Maiese D, Hendershot T, Kwok RK, Haines J. The PhenX Toolkit: Get the Most From Your Measures. American Journal of Epidemiology. 2011;174(3):253–260. doi: 10.1093/Aje/Kwr193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart J, Einav C, Weingarten MA, Stein M. The Importance of Family Support in a Behavior-Modification Weight-Loss Program. Journal of the American Dietetic Association. 1990;90(9):1270–1271. [PubMed] [Google Scholar]
- Hoelscher DM, Day RS, Kelder SH, Ward JL. Reproducibility and validity of the secondary level School-Based Nutrition Monitoring student questionnaire. Journal of the American Dietetic Association. 2003;103(2):186–194. doi: 10.1053/Jada.2003.50031. [DOI] [PubMed] [Google Scholar]
- IBM Corp. SPSS Statistics (Version 20.0.0) Armonk, NY: IBM Corp.; 2011. [Google Scholar]
- Institute for Healthcare Improvement. The Breakthrough Series: IHI’s Collaborative Model for Achieving Breakthrough Improvement. Boston: Institute for Healthcare Improvement; 2003. (IHI Innovation Series white paper). [Google Scholar]
- KershWellness. KAM: Accelerate your life. Retrieved 3/11/14, from http://www.kershkam.com/us/product/?f=1&ClientTZ=240.
- Khan LK, Sobush K, Keener D, Goodman K, Lowry A, Kakietek J, Zaro S. Recommended community strategies and measurements to prevent obesity in the United States. MMWR Recommendations and Reports. 2009;58(RR-7):1–26. [PubMed] [Google Scholar]
- Lytle LA, Nichaman MZ, Obarzanek E, Glovsky E, Montgomery D, Nicklas T, Feldman H. Validation of 24-Hour Recalls Assisted by Food Records in 3rd-Grade Children. Journal of the American Dietetic Association. 1993;93(12):1431–1436. doi: 10.1016/0002-8223(93)92247-U. [DOI] [PubMed] [Google Scholar]
- Malenka DJ, Leavitt BJ, Hearne MJ, Robb JF, Baribeau YR, Ryan TJ, O’Connor GT. Comparing long-term survival of patients with multivessel coronary disease after CABG or PCI: analysis of BARI-like patients in northern New England. Circulation. 2005;112(9 Suppl):I371–376. doi: 10.1161/CIRCULATIONAHA.104.526392. [DOI] [PubMed] [Google Scholar]
- Mozaffarian RS, Wiecha JL, Roth BA, Nelson TF, Lee RM, Gortmaker SL. Impact of an Organizational Intervention Designed to Improve Snack and Beverage Quality in YMCA After-School Programs. American Journal of Public Health. 2010;100(5):925–932. doi: 10.2105/Ajph.2008.158907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor GT, Plume SK, Olmstead EM, Morton JR, Maloney CT, Nugent WC, Kasper JF. A regional intervention to improve the hospital mortality associated with coronary artery bypass graft surgery. The Northern New England Cardiovascular Disease Study Group. JAMA. 1996;275(11):841–846. [PubMed] [Google Scholar]
- Pearson ES. Goal setting as a health behavior change strategy in overweight and obese adults: A systematic literature review examining intervention components. Patient Education and Counseling. 2012;87(1):32–42. doi: 10.1016/J.Pec.2011.07.018. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The Development of Scales to Measure Social Support for Diet and Exercise Behaviors. Preventive Medicine. 1987;16(6):825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- SAS Institute, I. SAS (Version 9.3) Cary, NC: SAS Institute, Inc.; 2011. [Google Scholar]
- Schifferdecker KE, Reed VA. Using mixed methods research in medical education: basic guidelines for researchers. Med Educ. 2009;43(7):637–644. doi: 10.1111/j.1365-2923.2009.03386.x. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. 2008 (U0036). Retrieved from http://www.health.gov/PAGuidelines/pdf/paguide.pdf.
- United States Department of Agriculture. ChooseMyPlate.gov. 2014 Retrieved 3/5/14, from http://www.choosemyplate.gov/index.html.
- Wing RR, Jeffery RW. Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. J Consult Clin Psychol. 1999;67(1):132–138. doi: 10.1037//0022-006x.67.1.132. [DOI] [PubMed] [Google Scholar]


