Abstract
Background:
Among preterm infants, the peripherally inserted central catheter (PICC) is the standard line for central venous access; however, its placement exposes them to hypothermia and pain. Ultrasound (US)-guided central line insertion may be less morbid than standard PICC line.
Aims:
To determine the ease, success rate, and morbidity associated with US-guided central line insertion in the internal jugular vein (IJV) by comparing it to the standard PICC line placement.
Materials and Methods:
This is a single-center nonrandomized prospective study evaluating preterm infants between October 2013 and June 2014. Patients were allocated into two groups: The standard group (control group) who underwent blind PICC line insertion and the intervention group who underwent a percutaneous US-guided central line insertion in the IJV. The epicutaneo-cava-catheter was used in both groups.
Results:
Fifty neonates were enrolled on study. A statistically difference in favor of US-IJV insertion was noted concerning the rate of successful first attempt (P < 0.001), insertion (P = 0.001), and procedure duration (P < 0.001) and number of trials (P < 0.001) compared to PICC. No difference in complications (P = 1.000) was noted.
Conclusion:
US guided catheterization of the IJV technique is faster than PICC line insertion with higher rates of successful first attempt and insertion, less procedure duration and fewer number of trials compared to PICC line insertion. There were no differences in complications.
Keywords: Central line, internal jugular vein, peripherally inserted central catheter, preterm neonates, ultrasound
Introduction
Very-low birth weight preterm neonates need a long duration of venous access to insure total parenteral nutrition (TPN) and administration of additional intravenous fluids and medications.[1,2] Many techniques are frequently performed to get central venous access lines in Neonatal Intensive Care Unit, such as peripherally inserted central catheters (PICCs), umbilical venous catheters, and central venous catheters.[1]
In recent years, several studies have encouraged the use of ultrasonography as a safe and efficient technique to assist in the venous detection and central line insertion.[3,4,5,6] The potential benefit of ultrasound (US)-guided PICC placement has been evaluated in several pediatric studies,[7,8] and there is a learning curve to overcome to improve skills in insertion.[4,9] In children and infants, the efficacy of US-guided central line insertion in internal jugular vein (IJV) is still debated,[10,11] and therefore not widely used for preterm infants. We compare the standard PICC insertion in preterm neonates to US-IJV access by evaluating the ease of use, success, and morbidity rate.
Materials and Methods
We conducted a single-center prospective nonrandomized quasi-experimental study of preterm infants who underwent an elective or emergent central line insertion between October 2013 and June 2014. Hospital's Institutional Review Board approved the study. An informed parental consent was signed for study entry. Inclusion criteria included preterm infants requiring TPN, antibiotic therapy for at least 7 days, and infants with inadequate peripheral venous access. Exclusion criteria included refusal to sign consent or patients with previously placed central lines.
The catheter used for all the patients were epicutaneo-cava-catheter (ECC), silicone tube material kit, 24G, VYGON® (Aachen, Germany). All procedures were performed under sterile precautions such as hand washing, use of sterile gloves and gowns, face mask, hair cover, and protective eyewear. To maintain an equal number of participants among both groups, patients were allocated to the control or intervention group alternating in the order in which participants were recruited in the study beginning with the control group.
The control group included neonates who underwent a PICC line placement. The method of insertion was performed as previously described by Pettit.[7] Patients in the intervention group underwent US-IJV. This procedure was carried out as follows: The patient's skin was sterilized with chlorhexidine gluconate. Vascular cannulation was performed by the winged needle present with the ECC. The target vessel was located via the US dynamic (real-time) method. At the point of needle insertion, the ECC was placed through the needle without guide wire placement. Once the catheter was inserted, a gentle aspiration was performed to show blood flow through the 3 ml syringe that was connected to the ECC. The catheter was then secured and fixed with simple steri-strips and covered by the transparent dressing. Both techniques were performed by two institutional neonatologists where one performed all PICC line placements while the other performed US-IJV.
The transducer selection and the axis of visualization are important to consider in the use of US for ECC. We used a linear 6–13 MHz transducer Sonosite M-turbo (manufacturer's recommendations). The transverse view shows the vessel under the transducer and the adjacent structures. The tip of the needle is visualized and inserted at a 45° angle. The longitudinal view helps to track the needle progression toward the IJV. Postprocedural chest radiography was done for both groups to confirm placement and evaluate for complications.
The primary outcome measured was a success at first attempt that was defined as the ability to catheterize the vein after its puncture. Secondary outcomes measured included: (1) Catheter malpositioning; (2) peri- or post-operative complication's incidence defined as occurrence of any of the following complications: Hematoma formation, carotid artery puncture, or development of a pneumothorax; (3) duration of catheterization in minutes defined as time needed from the puncture of the vein to external fixation of the catheter; (4) number of attempts until successful insertion. Additional patient information collected included sex, TPN administration, gestational age, and birth weight.
Sample size calculation. To increase the success of the first attempt by 50% as reported by de Carvalho Onofre et al.,[12] 21 neonates would be needed for every group to produce a study power of 85%.
Statistical analysis
Analysis was performed using SPSS version 22 (SPSS IBM, New York, USA). Characteristics of patients and outcome measures are described as numbers (%) or median (interquartile range) for nominal and continuous variables, respectively. For each outcome, we compared study arms. The null hypothesis was defined as no difference between the groups. Fisher's exact test was used to compare nominal variables. Continuous variables were compared using Mann–Whitney U-test. The value of P < 0.05 was considered statistically significant.
Results
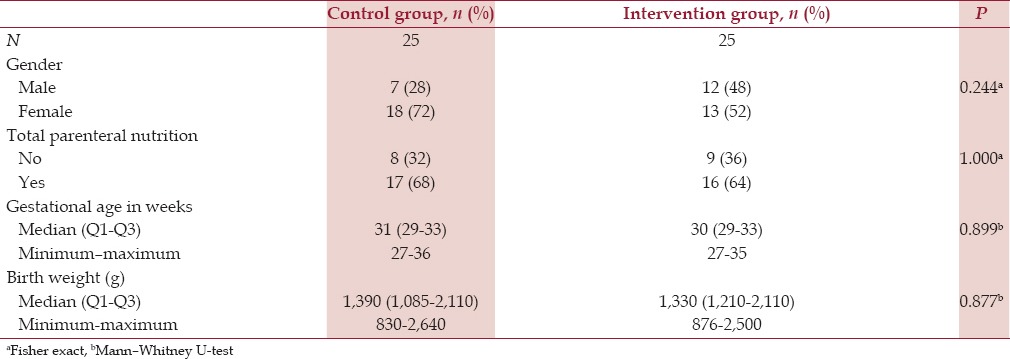
A total of 58 newborns were enrolled on study. Eight had failed central line insertions with the allocated method and were thus excluded. Five of the excluded cases were from the control group, remaining from the intervention group. The study sample consisted of fifty neonates allocated equally between groups. The groups showed no statistically significant difference at the level of gender, TPN need, age of gestation, and birth weight [Table 1]. Most of the newborns were female and required TPN. The median gestational age for the control group and interventional group was 31 and 30 weeks, respectively.
Table 1.
Baseline characteristics of the recruited neonates
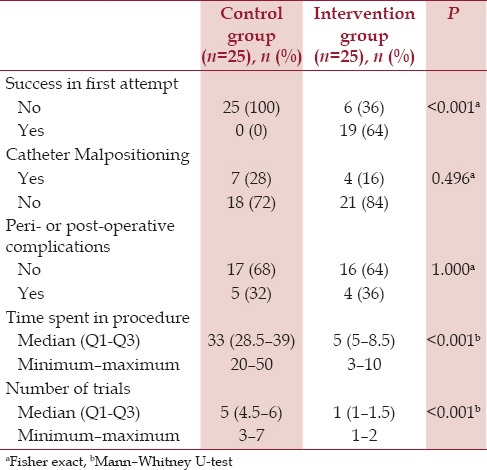
Comparison of our cohort is described in Table 2. A statistically difference in favor of US-IJV insertion was noted concerning the rate of successful first attempt (P < 0.001), insertion (P = 0.001), and procedure duration (P < 0.001) and number of trials (P < 0.001) compared to PICC. There were no differences in complications (P = 1.000). A hematoma at the site of puncture was the most common complication. No patients developed pneumothorax as a complication.
Table 2.
Results of central line placement using ultrasound-guided and umbilical technique compared to standard placement
Discussion
The advantages of the US-IJV access over anatomical landmarks in infants and children are reported in many studies,[13,14,15,16] but refuted by Sigaut et al., which found that US had no effect on the rate of failure of IJV access and the rate of puncture of the carotid artery.[11] In our study, population of preterm neonates, US was very useful during IJV access as it improved first puncture success rates. In addition, insertion of the ECC via US-guided technique is more successful and faster than PICC with no added increase risk of morbidity.
The number of attempts used during a PICC line or even the number of sites changed to have a successful insertion of a central line for the newborn reported in the literature[1] was comparable to our control group (seven attempts). As for the intervention group, the number of attempts was more than one attempt in the first five cases and was reduced to practice to one in almost all cases. This suggests that a short learning curve is enough without any specific training in interventional radiology.
Transverse and longitudinal views are used in the US-guided vascular access. In transverse view, the IJV is showed as a circle and adjacent vessels are visualized at the same time. In longitudinal view, the IJV is displayed as a long tube, it allows visualization of an entire vessel of interest, and improves the visibility of the needle tip during vessel puncture.[17,18] We believe that these two approaches are complementary, especially in preterm newborns to decrease complications.
In preterm neonates, the exposure to repeated painful procedures may lead to stress, delaying in weight gain and recovery, greater metabolic expenditure, and worsening their clinical conditions.[19,20] Probably as a follow on of our data, a more expanded study is necessary to evaluate the pain between the two groups as we might find a slight benefit in US technique since approximately one puncture is needed to complete the insertion of the central line.
Premature babies are prone to hypothermia, mainly when opening the portholes of the incubator for more than 30 min. The median time needed to insert a PICC line in our series was 33 min. Before developing hypothermia (under 36°C), we would stop the procedure until the neonate's temperature increased. However, the minimum temperature reached in the US-IJV group was 35.8°C, having a maximum time of insertion of 10 min. These findings suggest that US-guided technique prevents other commonly seen complications.
To the best of our knowledge, this is the first prospective study assessing the use of US-IJV in preterm patients. The study's strengths include a sufficient sample size, a comprehensive list of outcome measures, and well-trained personnel. Several limitations include nonrandomization of the patients. Blinding was not possible. Duration of catheterization did not include setup of US.
Conclusion
US-guided central line insertion in neonates is safe, fast, and reliable. It requires fewer trials of puncture and less procedure time without exposing premature babies to increased risk of complications. In the future, a prospective study will be conducted to evaluate the pain during the procedure and the central line-associated bloodstream infection's risk between these groups.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Thank you to professor Pascal Boileau, MD, PHD, head of NICU, department of perinatal medicine, CHI Poissy Saint-Germain, University of Versailles Saint Quentin, France for his critical review of the manuscript.
Thank you to professor Khalid Yunis, head of NICU, Normal Newborn Nursery, Department of Pediatrics and Adolescent Medicine, AUBMC, Lebanon for his critical review of the manuscript.
Thank you to Dr. Dany Assaf Curi, department of pediatrics, Saint Georges University Hospital, University of Balamand, Beirut, Lebanon for his critical review of the manuscript.
References
- 1.Janes M, Kalyn A, Pinelli J, Paes B. A randomized trial comparing peripherally inserted central venous catheters and peripheral intravenous catheters in infants with very low birth weight. J Pediatr Surg. 2000;35:1040–4. doi: 10.1053/jpsu.2000.7767. [DOI] [PubMed] [Google Scholar]
- 2.Niermeyer S, Kattwinkel J, Van Reempts P, Nadkarni V, Phillips B, Zideman D, et al. International guidelines for neonatal resuscitation: An excerpt from the guidelines 2000 for cardiopulmonary resuscitation and emergency cardiovascular care: International consensus on science. Contributors and reviewers for the neonatal resuscitation guidelines. Pediatrics. 2000;106:E29. doi: 10.1542/peds.106.3.e29. [DOI] [PubMed] [Google Scholar]
- 3.Rothschild JM. Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Rockville, MD: Agency for Healthcare Research and Quality; 2001. Ultrasound guidance of central vein catheterization. [Google Scholar]
- 4.Detaille T, Pirotte T, Veyckemans F. Vascular access in the neonate. Best Pract Res Clin Anaesthesiol. 2010;24:403–18. doi: 10.1016/j.bpa.2010.02.017. [DOI] [PubMed] [Google Scholar]
- 5.Stokowski G, Steele D, Wilson D. The use of ultrasound to improve practice and reduce complication rates in peripherally inserted central catheter insertions: Final report of investigation. J Infus Nurs. 2009;32:145–55. doi: 10.1097/NAN.0b013e3181a1a98f. [DOI] [PubMed] [Google Scholar]
- 6.Kumar A, Chuan A. Ultrasound guided vascular access: Efficacy and safety. Best Pract Res Clin Anaesthesiol. 2009;23:299–311. doi: 10.1016/j.bpa.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 7.Pettit J. Technological advances for PICC placement and management. Adv Neonatal Care. 2007;7:122–31. doi: 10.1097/01.anc.0000278210.18639.fd. [DOI] [PubMed] [Google Scholar]
- 8.Donaldson JS, Morello FP, Junewick JJ, O’Donovan JC, Lim-Dunham J. Peripherally inserted central venous catheters: US-guided vascular access in pediatric patients. Radiology. 1995;197:542–4. doi: 10.1148/radiology.197.2.7480709. [DOI] [PubMed] [Google Scholar]
- 9.Nicholson J. Development of an ultrasound-guided PICC insertion service. Br J Nurs. 2010;19:S9–17. doi: 10.12968/bjon.2010.19.Sup3.48212. [DOI] [PubMed] [Google Scholar]
- 10.Verghese ST, McGill WA, Patel RI, Sell JE, Midgley FM, Ruttimann UE. Comparison of three techniques for internal jugular vein cannulation in infants. Paediatr Anaesth. 2000;10:505–11. doi: 10.1046/j.1460-9592.2000.00554.x. [DOI] [PubMed] [Google Scholar]
- 11.Sigaut S, Skhiri A, Stany I, Golmar J, Nivoche Y, Constant I, et al. Ultrasound guided internal jugular vein access in children and infant: A meta-analysis of published studies. Paediatr Anaesth. 2009;19:1199–206. doi: 10.1111/j.1460-9592.2009.03171.x. [DOI] [PubMed] [Google Scholar]
- 12.de Carvalho Onofre PS, da Luz Gonçalves Pedreira M, Peterlini MA. Placement of peripherally inserted central catheters in children guided by ultrasound: A prospective randomized, and controlled trial. Pediatr Crit Care Med. 2012;13:e282–7. doi: 10.1097/PCC.0b013e318245597c. [DOI] [PubMed] [Google Scholar]
- 13.Leyvi G, Taylor DG, Reith E, Wasnick JD. Utility of ultrasound-guided central venous cannulation in pediatric surgical patients: A clinical series. Paediatr Anaesth. 2005;15:953–8. doi: 10.1111/j.1460-9592.2005.01609.x. [DOI] [PubMed] [Google Scholar]
- 14.Hosokawa K, Shime N, Kato Y, Hashimoto S. A randomized trial of ultrasound image-based skin surface marking versus real-time ultrasound-guided internal jugular vein catheterization in infants. Anesthesiology. 2007;107:720–4. doi: 10.1097/01.anes.0000287024.19704.96. [DOI] [PubMed] [Google Scholar]
- 15.Machotta A, Kerner S, Höhne C, Kerner T. Ultrasound-guided central venous cannulation in a very small preterm neonate. Paediatr Anaesth. 2005;15:325–7. doi: 10.1111/j.1460-9592.2005.01432.x. [DOI] [PubMed] [Google Scholar]
- 16.Arul GS, Livingstone H, Bromley P, Bennett J. Ultrasound-guided percutaneous insertion of 2.7 Fr tunnelled Broviac lines in neonates and small infants. Pediatr Surg Int. 2010;26:815–8. doi: 10.1007/s00383-010-2616-3. [DOI] [PubMed] [Google Scholar]
- 17.Stone MB, Moon C, Sutijono D, Blaivas M. Needle tip visualization during ultrasound-guided vascular access: Short-axis vs long-axis approach. Am J Emerg Med. 2010;28:343–7. doi: 10.1016/j.ajem.2008.11.022. [DOI] [PubMed] [Google Scholar]
- 18.Blaivas M, Brannam L, Fernandez E. Short-axis versus long-axis approaches for teaching ultrasound-guided vascular access on a new inanimate model. Acad Emerg Med. 2003;10:1307–11. doi: 10.1111/j.1553-2712.2003.tb00002.x. [DOI] [PubMed] [Google Scholar]
- 19.Crawford M, Soukup SM, Woods SS, Deisch P. Peripherally inserted central catheter program. Nurs Clin North Am. 2000;35:349–60. [PubMed] [Google Scholar]
- 20.Ahn Y. The relationship between behavioral states and pain responses to various NICU procedures in premature infants. J Trop Pediatr. 2006;52:201–5. doi: 10.1093/tropej/fmi099. [DOI] [PubMed] [Google Scholar]


