Abstract
This report describes the ability of computed tomography angiography (CTA) imaging of the heart to visualize an acquired shunt between the left ventricular outflow tract (LVOT) and the right atrium (RA) (Gerbode defect). Previously, transesophageal echocardiography (TEE) has been the mainstay of diagnosis. To the best of our knowledge, the use of cardiac CTA imaging to visualize and diagnose this disorder has not been previously reported. Cardiac CTA allows for more detailed visualization of cardiac anatomy and can supplement or supplant TEE as the diagnostic test of choice for evaluation of patients with this rare defect.
Abbreviations: MRI, magnetic resonance imaging; CTA, computed tomography angiography; TEE, transesophageal echocardiography
Case report
A 56-year-old male presented to our institution with shortness of breath, heart palpitations, left-sided chest discomfort, chills, nausea, and vomiting. He had a prior medical history of rheumatic fever, subacute bacterial endocarditis, and a successful aortic valve replacement 17 years ago. His physical exam revealed normal respirations, sinus tachycardia, no audible murmurs, and normal pedal pulses without peripheral edema.
A transesophageal echocardiogram (TEE) revealed severe mitral regurgitation, a dilated ascending aortic root with a perivalvular leak, and a normally functioning prosthetic aortic valve. Coronary angiography showed moderate stenosis of the left anterior descending coronary artery. Subsequently, the patient underwent complex mitral-valve repair with reconstruction of the artificial chordae, a sliding plasty of posterior mitral-valve leaflet, and an annuloplasty using a 28-mm Cosgrove ring. He also had aortic root replacement with reimplantation of the coronaries, using a 27-mm freestyle aortic prosthesis. The ascending aortic aneurysm was also repaired without any complications, and the patient was discharged seven days after admission.
The patient returned to the hospital five months later with complaints of palpitation and chest pain a few days after an accidental electrical shock at work. He was diagnosed with atrial flutter and successfully cardioverted to sinus rhythm. According to the patient, TEE was performed at an outside hospital, and he raised the possibility of an intracardiac “shunt.” However, the patient did not have specific details/diagnosis of the underlying defect or records of the echocardiogram. To define the surgically altered cardiac anatomy and to evaluate for a possible intracardiac defect, a cardiac CTA imaging study was requested.
CTA of the chest was performed using a 64-slice CT scanner (Philips Brilliance-64) (Fig. 1). A bolus-tracking technique was used, with the region of interest placed in the aortic arch. The threshold for contrast triggering was set at 120 HU. 100ml of ioversol (Optiray-350, Mallinckrodt, Inc) was administered intravenously at a rate of 5 ml/sec, followed by 40ml of a saline chaser. Scan parameters were as follows: collimation, 64 × 0.625mm; voltage, 120 kVp; current, 800 mAs. ECG gating was used, and multiphase retrospective reconstruction was performed for image interpretation.
Figure 1.
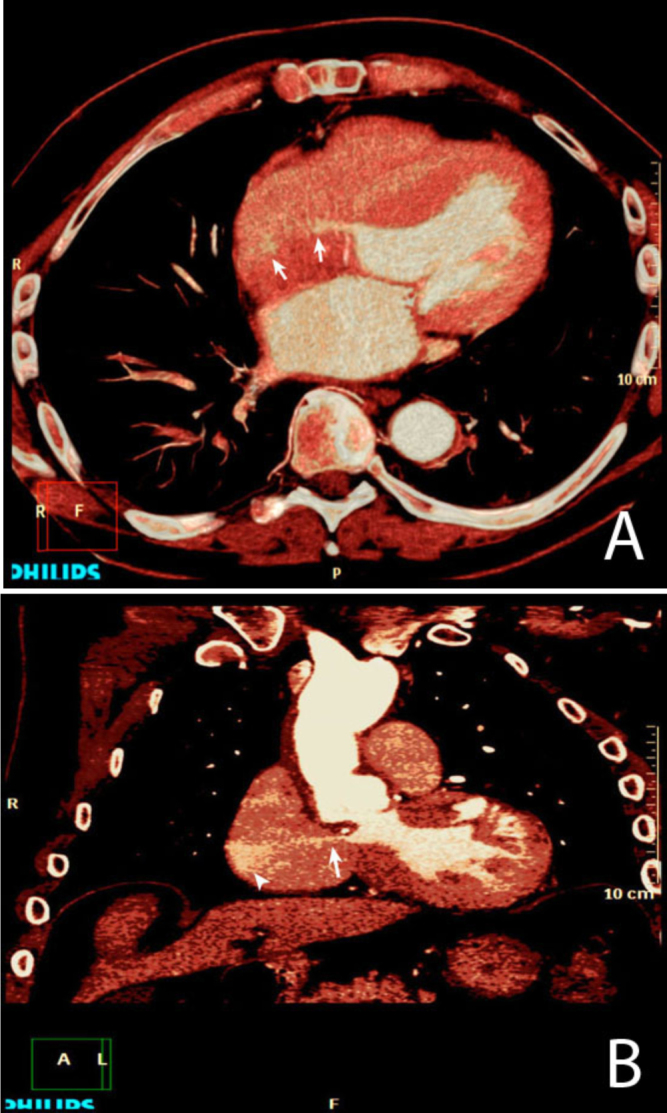
Axial (A) and coronal maximum-intensity projection MIP (B) images from a CTA of the chest demonstrate a blush of contrast (arrows) from the left ventricular outflow tract (LVOT) into the unopacified right atrium. The jet of contrast (arrow) from the LVOT extends to the right atrial free wall (arrowhead) as depicted in B.
The CTA demonstrated a postsurgical appearance compatible with the prior ascending thoracic aortic aneurysm repair and aortic and mitral valve replacement. However, an irregular, small outpouching of contrast material was noted from the noncoronary sinus of Valsalva, which was presumably related to the aortic surgery. A left-ventricular-to-right-atrial septal defect was also noted, which was felt to be a postoperative complication from the recent aortic surgery.
TEE images were obtained from an outside hospital after the diagnosis of shunt was made using CTA. On color Doppler imaging, these TEE images showed a high-velocity jet originating from the aortic root, apparently from the right sinus. There was a fairly prominent jet seen from that location moving into the right atrium, although the actual opening itself appeared to be small and well-defined. The right atrium itself did not appear to be enlarged (Figs. 2A, 2B).
Figure 2.
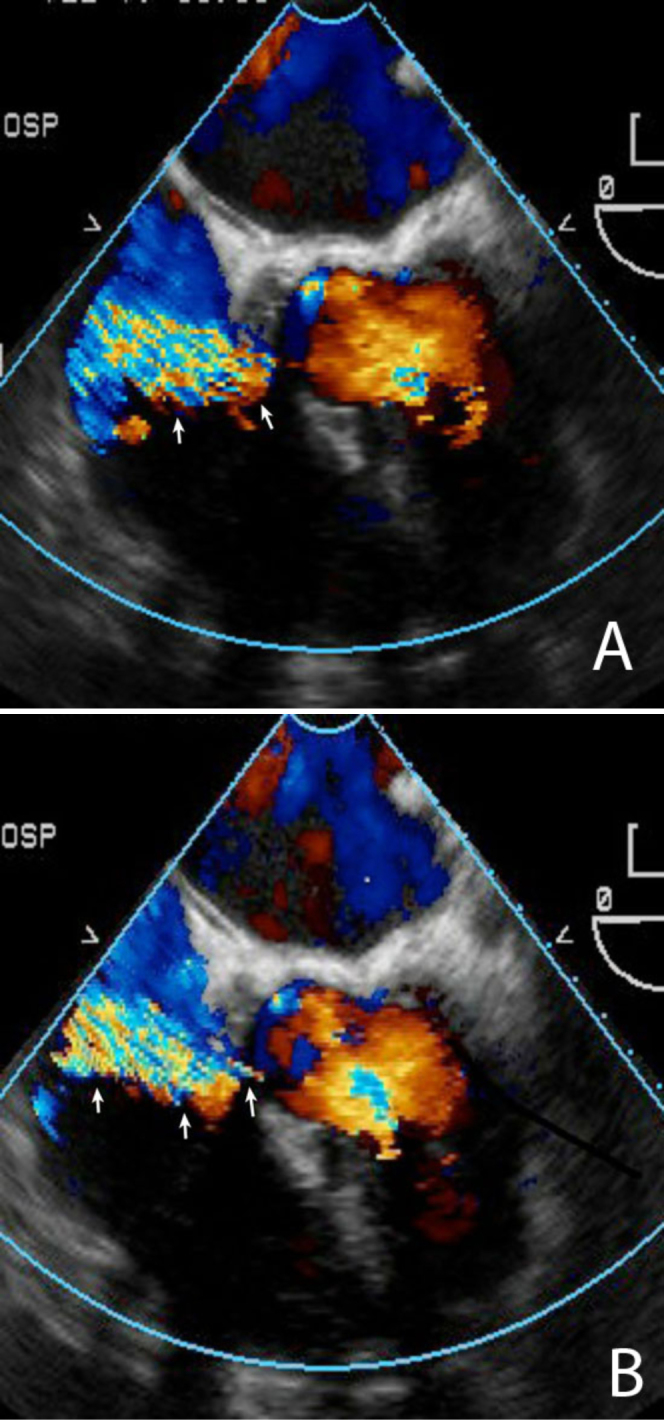
Transthoracic echocardiographic examination with apical four-chamber view shows a jet (arrows) originating from aortic root to the right atrium (RA). The RA does not appear to be enlarged.
Because the patient had minimal symptoms, this defect was managed with observation. There was no right heart dilatation or dysfunction, and the defect was associated with a small restrictive shunt.
Discussion
Left-ventricular-to-right-atrial (LV – RA) communications are rare intracardiac defects resulting from ventricular septal perforation due to congenital or acquired causes. These defects are collectively known as Gerbode defects. Both congenital and acquired forms result from a defect in the membranous interventricular septum.
The congenital form accounts for less than 1% of congenital heart disease, is often associated with an atrial septal defect, and was originally described by Frank Gerbode in a five-case series (1).
Acquired cases have been reported less frequently, mostly resulting from infective endocarditis in patients with ventricular septal defect (2, 3). They have also been reported to arise occasionally as the result of trauma (4), acute myocardial infarction (5), and aortic valve replacement (6).
The responsible defect in the membranous interventricular septum can be above or below the tricuspid valve (7). Because the tricuspid annulus has a more apical location than the mitral annulus, the septal leaflet of the tricuspid valve normally rests 5 mm to 10 mm more apically than the anterior leaflet of the mitral valve. This anatomical arrangement allows the septal leaflet to divide the membranous ventricular septum into two portions: a supravalvular (or atrioventricular) portion, and an infravalvular (or interventricular) portion. A defect in the supravalvular portion results in a direct LV-RA communication. A similar defect in the infravalvular portion represents a perimembranous ventricular septal defect and would normally result in a communication between the LV and the RV. The prominent physical finding of an LV-RA shunt is a loud and harsh pansystolic murmur, often associated with a thrill along the left sternal border. Nevertheless, a diagnosis is usually not possible on the basis of physical examination alone.
As previously reported, TEE has been the mainstay of diagnosis (8, 9). Most published articles have described typical cardiac catheterization features of this defect, with cardiac MR imaging reportedly offering better visualization of the defect and helping to quantify the amount of blood shunting across the defect (10).
To the best of our knowledge, our case is the first documented report of LVOT-to-RA communication demonstrated with cardiac CTA. We feel that cardiac CTA allows for better visualization and more detailed evaluation of cardiac anatomy and that it can supplement and possibly supplant TEE as the test of choice for diagnosis of this rare defect.
It may never be possible to ascertain the exact mechanism of septal perforation in this case. However, it is likely that the defect was caused by surgical trauma, because there was no such defect seen on the echocardiogram performed before aortic valve replacement and mitral valve repair. This unusual complication after aortic valve replacement is a rare condition and should be kept in mind in patients who present with progressive dyspnea after operation.
Footnotes
Published: July 20, 2011
References
- 1.Gerbode F, Hultgren H, Melrose D, Osborn J. Syndrome of left ventricular-right atrial shunt; successful surgical repair of defect in five cases, with observation of bradycardia on closure. Ann Surg. 1958;148:433–446. doi: 10.1097/00000658-195809000-00012. PubMed) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wasserman SM, Fann JI, Atwood JE, Burdon TA, Fadel BM. Acquired left ventricular-right atrial communication: Gerbode-type defect. Echocardiography. 2002;19:67–72. doi: 10.1046/j.1540-8175.2002.00067.x. PubMed) [DOI] [PubMed] [Google Scholar]
- 3.Velebit V, Schoneberger A, Ciaroni S, Bloch A, Maurice J, Christenson JT, Simonet F, Schmuziger M. “Acquired” left ventricular-to-right atrial shunt (Gerbode defect) after bacterial endocarditis. Tex Heart Inst J. 1995;22:100–102. PubMed) [PMC free article] [PubMed] [Google Scholar]
- 4.Olsovsky MR, Topaz O, DiSciascio G, Vetrovec GW. Acute traumatic ventricular septal rupture. Am Heart J. 1996;131:1039–1041. doi: 10.1016/s0002-8703(96)90193-3. PubMed) [DOI] [PubMed] [Google Scholar]
- 5.Newman JN, Jr, Rozanski L, Kreulen T. Acquired left ventricular to right atrial intracardiac shunt after myocardial infarction: A case report and review of the literature. J Am Soc Echocardiogr. 1996;9:716–720. doi: 10.1016/s0894-7317(96)90070-x. PubMed) [DOI] [PubMed] [Google Scholar]
- 6.Katz ES, Tunick PA, Kronzon I. To-and-fro left ventricular-to-right atrial shunting after valve replacement shown by transesophageal echocardiography. Am Heart J. 1991;121:211–214. doi: 10.1016/0002-8703(91)90983-o. PubMed) [DOI] [PubMed] [Google Scholar]
- 7.Riemenschneider TA, Moss AJ. Left ventricular-right atrial communication. Am J Cardiol. 1967;19:710–718. doi: 10.1016/0002-9149(67)90476-6. PubMed) [DOI] [PubMed] [Google Scholar]
- 8.Eroglu S, Sade E, Bozbas H, Pirat B, Yildirir A, Muderrisoglu H. Echocardiographic diagnosis of left ventricular-right atrial communication (Gerbode-type defect) in an adult with chronic renal failure: a case report. Eur J Echocardiog. Jan 11 2007 doi: 10.1016/j.euje.2006.11.010. PubMed) [DOI] [PubMed] [Google Scholar]
- 9.Erdol C, Gokce M, Celik S, Baykan M, Orem C, Bayram A. Twodimensional color Doppler echocardiographic imaging of a Gerbode defect: a case report. Echocardiography. May 2000;17(4):335–336. doi: 10.1111/j.1540-8175.2000.tb01145.x. PubMed) [DOI] [PubMed] [Google Scholar]
- 10.Cheema OM, Patel AA, Chang SM, Shah DJ. Gerbode ventricular septal defect diagnosed at cardiac MR imaging: case report. Radiology. 2009 Jul;252(1):50–52. doi: 10.1148/radiol.2521082186. PubMed) [DOI] [PubMed] [Google Scholar]


