Abstract
A 67-year-old female presented to the emergency department with epigastric and left-upper-quadrant abdominal pain. The patient reported history of multiple episodes of abdominal pain similar in nature over the last 2 years. Computed tomography (CT) and magnetic resonance imaging (MRI) of the abdomen demonstrated acute pancreatitis along with the presence of pancreatic tissue around the descending portion of the duodenum (a characteristic feature of annular pancreas). The findings on different imaging modalities are described.
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging; MRCP, magnetic resonance cholangiopancreatography
Introduction
Annular pancreas is a rare congenital anomaly characterized by a ring of pancreatic tissue encircling the duodenum, most commonly the descending part of the duodenum. It may manifest during the early neonatal period with duodenal obstruction, but may also remain asymptomatic until adulthood with various presentations including pancreatitis.
Case report
A 67-year-old female with past medical history of chronic obstructive pulmonary disease and hypertension presented with epigastric and left-upper-quadrant abdominal pain. She had multiple previous episodes of similar abdominal pain resulting in hospital admission; this was diagnosed as pancreatitis and thought to be secondary to gallstones, for which she had a laparoscopic cholecystectomy the previous year. Physical exam revealed a nondistended and soft abdomen with significant tenderness in the epigastrium. Bowel sounds were normal.
Laboratory results were significant for markedly elevated serum amylase and lipase levels: 782 (normal 31-124 U/L) and 4,167 (normal 0-59 U/L), respectively.
The intravenous contrast-enhanced CT scan on admission showed peripancreatic inflammation most prominent around the head and neck, together with hypoattenuation and enlargement of the head consistent with acute pancreatitis (Figure 1, Figure 2). Another CT scan was performed two days later per multiphasic pancreatic protocol, with initial noncontrast arterial and portal venous phases followed by contrast-enhanced phase with addition of oral contrast. It clearly showed the duodenum surrounded by tissue that was isodense to the pancreas. The common duct (CD) was seen just posteromedial to the duodenum (Fig. 3). Coronal reformatted CT images showed pancreatic tissue along the lateral aspect of descending duodenum (Fig. 4). The pancreatic head again showed changes of pancreatitis. MRI of the abdomen at the level of pancreas showed pancreatic tissue surrounding the duodenum (Fig. 5). Magnetic resonance cholangiopancreatography (MRCP) did not reveal any CD stones.
Figure 1.

67-year-old female presented with epigastric and left-upper-quadrant abdominal pain. Contrast-enhanced axial CT image shows inflammatory/edematous changes (arrows) surrounding the head and neck of the pancreas.
Figure 2.
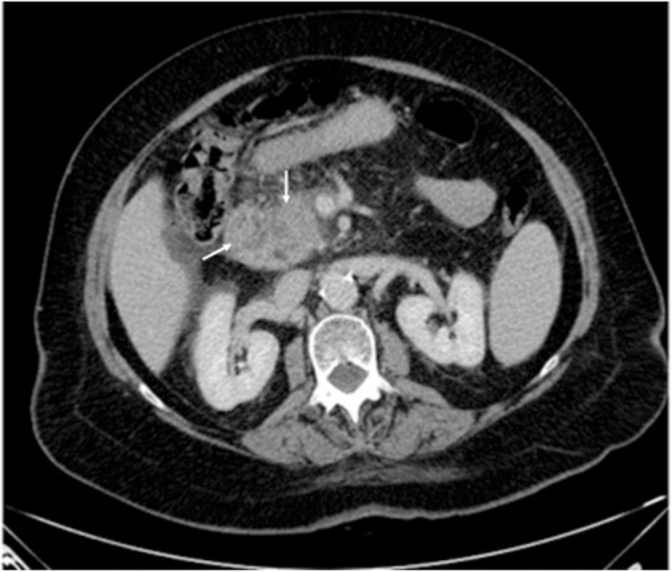
67-year-old female with epigastric and left-upper-quadrant abdominal pain. Contrast-enhanced axial CT image shows peripancreatic inflammatory changes (arrows) along with hypoattenuation and enlargement of the pancreatic head.
Figure 3.
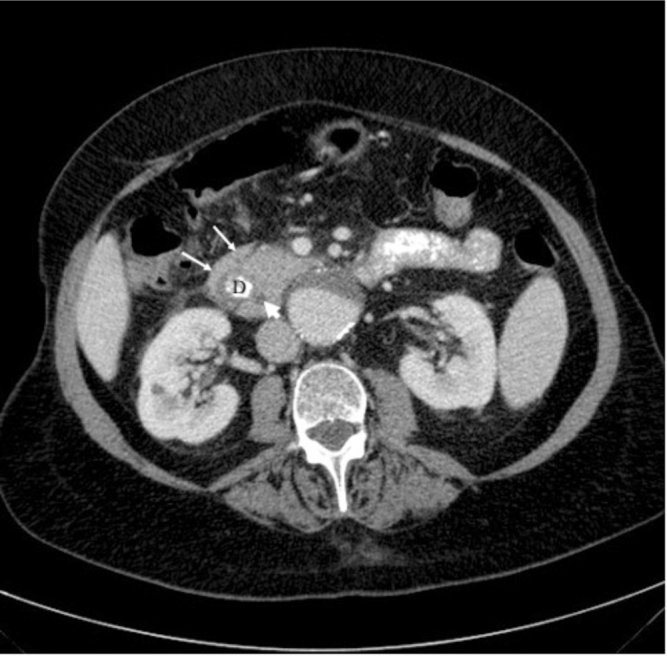
67-year-old female with epigastric and left-upper-quadrant abdominal pain. Axial CT image with both oral and intravenous contrast shows duodenum (D) surrounded by tissue isodense to pancreas (arrows). Also visible is the common duct (arrowhead) just posteromedial to the duodenum.
Figure 4.

67-year-old female with epigastric and left-upper-quadrant abdominal pain. Coronal CT reformatted image shows pancreatic tissue (arrow) along the lateral aspect of the descending duodenum. Acute inflammatory changes are again visible in pancreatic head.
Figure 5.

67-year-old female with epigastric and left-upper-quadrant abdominal pain. MRI abdomen T1-weighted 3 D VIBE axial image at the level of pancreas shows pancreatic tissue (arrows) surrounding the duodenum (D). Also visible is the common bile duct (arrowhead).
A review of the previous imaging record revealed that no comment was made about the presence of annular pancreas on the patient’s prior studies. One year ago, a CT scan of abdomen was reported to show a poorly defined hypodense region within the neck of the pancreas, with a possibility of pancreatitis or early pseudocyst formation along with some calcified gallstone. Although the initial CT scan was performed with enteric contrast, the annular pancreas may not have been well visualized, as enteric contrast material was not present in the duodenum at the time of scanning, most likely secondary to the delay between contrast intake and scanning time. Additionally, the presence of extensive inflammatory changes in this region may have made visualization of the annular pancreas difficult. Ultrasound examination also demonstrated poor visualization of the pancreas, likely due to known pancreatitis. We did not find any comment in the operative notes from the patient’s laproscopic cholecystectomy regarding the presence of annular pancreas as well.
The patient was treated conservatively with intravenous hydration, and pain management under the supervision of the gastroenterology service.
Discussion
Annular pancreas is an uncommon developmental malformation characterized by a ring of pancreatic tissue encircling the duodenum, most commonly the descending part of the duodenum (Fig. 6) (1). Among congenital pancreatic aberrations, it is the second most common after pancreatic divisum (2). The prevalence varies between 5-15/100,000 adults on a cadaveric case series, to 1 in 250 on an endoscopic retrograde cholangiopancreatography (ERCP) study (3, 4, 5). The prevalence ratio between infants and adults is approximately 0.008% versus 0.005 %, respectively (3, 4, 5, 6).
Figure 6.
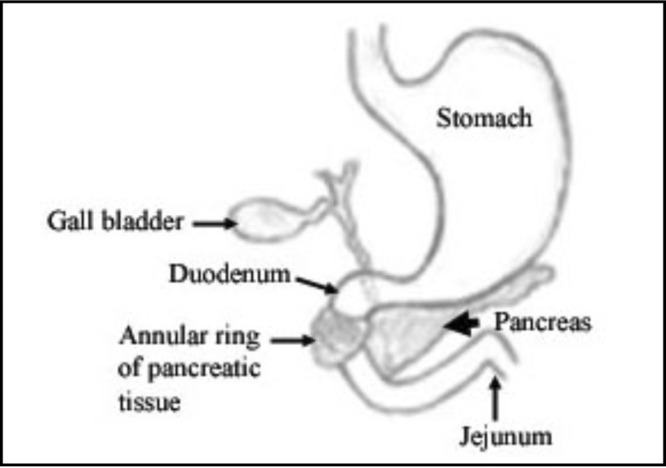
Schematic diagram illustrating the annular pancreas and its relationship to duodenum and surrounding structures.
This congenital anomaly is seen twice as commonly in males than in females. Well-recognized associations are described in the literature with other developmental anomalies/syndromes such as Down’s syndrome, duodenal atresia, congenital heart disease, imperforate anus, tracheoesophageal defects, and Hirsch sprung disease (1, 2). In more than half of the cases, annular pancreas does not manifest clinically and can be a purely incidental finding (3). However, when it is symptomatic, it may manifest in early infancy as duodenal obstruction, or it may appear later in life when it usually presents with abdominal pain, postprandial fullness, and vomiting, or even peptic/duodenal ulceration secondary to static duodenal contents. Reflux of duodenal contents in the pancreatic ducts due to continuous peristaltic waves in the proximal duodenum can result in acute, chronic, or acute-on-chronic pancreatitis (7, 8, 9, 10).
Pancreatic development starts in the fifth week in utero with the appearance of pancreatic buds, two ventral and one dorsal. The ventral buds then fuse together. The developing duodenum stimulates this fused ventral bud to rotate posteriorly and then to unite to the dorsal bud. Interruption in this step may result in entrapment of the descending part of the duodenum by the developing pancreatic tissue, resulting in a ring of pancreas encircling the duodenum (3). Different theories have been presented about the origin of annular pancreas, but it is clear that it is derived from the ventral bud of the developing pancreas (11). Specifically, the left lobe of the ventral bud is considered to be the origin (1).
Annular pancreas is a radiologic diagnosis. Several imaging modalities can aid in establishing the diagnosis. An upper gastrointestinal (GI) series most often shows concentric, smooth narrowing along the second portion of the duodenum. CT scan demonstrates not only the annular pancreatic tissue encircling the duodenum but possibly also dilated duodenum proximal to this stenosis. The value of enteric contrast is particularly great in this case, as it helps to clearly identify the anatomy in this region by delineating the course of the duodenum. MRCP classically shows the pancreatic tissue/duct entrapping the second portion of duodenum (2). Although the initial CT scan of the abdomen in our patient was done with the enteric contrast, the fact that the contrast had passed beyond the duodenum at the time of scanning made the visibility of annular pancreas difficult.
Although a complete ring of pancreatic tissue encircling the duodenum suggests annular pancreas, its absence does not exclude the diagnosis. In fact, Sandrasegaran et al found that more than 37% of patients in their study group had an incomplete annulus of pancreatic tissue around the second portion of duodenum in a jaw-like configuration (3).
In summary, annular pancreas is an uncommon congenital anomaly, but it should be considered in patients with repeated bouts of pancreatitis when the common etiologies like gallstones and alcoholism have been ruled out. In adults, it usually presents in the third to fourth decades. Our case demonstrates a late presentation of annular pancreas due to recurrent pancreatitis in the seventh decade.
Footnotes
Published: September 22, 2011
References
- 1.Chevillotte G, Sahel J, Raillat A, Sarles H. Annular pancreas. Report of one case associated with acute pancreatitis and diagnosed by endoscopic retrograde pancreatography. Dig Dis Sci. 1984 Jan;29(1):75–77. doi: 10.1007/BF01296865. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Jadvar H, Mindelzun RE. Annular pancreas in adults: imaging features in seven patients. Abdom Imaging. 1999 Mar-Apr;24(2):174–177. doi: 10.1007/s002619900470. [PubMed] [DOI] [PubMed] [Google Scholar]
- 3.Sandrasegaran K, Patel A, Fogel EL, Zyromski NJ, Pitt HA. Annular pancreas in adults. AJR Am J Roentgenol. 2009 Aug;193(2):455–460. doi: 10.2214/AJR.08.1596. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Ravitch MM, Woods AC., Jr. Annular pancreas. Ann Surg. 1950 Dec;132(6):1116–1127. doi: 10.1097/00000658-195012000-00011. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baggott BB, Long WB. Annular pancreas as a cause of extrahepatic biliary obstruction. Am J Gastroenterol. 1991 Feb;86(2):224–226. [PubMed] [PubMed] [Google Scholar]
- 6.Lainakis N, Antypas S, Panagidis A, Alexandrou I, Kambouri K, Kyriazis C, Dolatzas T. Annular pancreas in two consecutive siblings: an extremely rare case. Eur J Pediatr Surg. 2005 Oct;15(5):364–368. doi: 10.1055/s-2005-865838. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Silvis RS. Annular pancreas. Ann Surg. 1952 Feb;135(2):278–283. doi: 10.1097/00000658-195202000-00015. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alexander HC. Annular pancreas in the adult. Am J Surg. 1970 Jun;119(6):702–704. doi: 10.1016/0002-9610(70)90243-6. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.Whelan TJ, Jr., Hamilton GB. Annular pancreas. Ann Surg. 1957 Aug;146(2):252–262. doi: 10.1097/00000658-195708000-00015. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Macphee IW. Annular pancreas. Br J Surg. 1953 Mar;40(163):510–511. doi: 10.1002/bjs.18004016322. [PubMed] [DOI] [PubMed] [Google Scholar]
- 11.Dowsett JF, Rode J, Russell RC. Annular pancreas: a clinical, endoscopic, and immunohistochemical study. Gut. 1989 Jan;30(1):130–135. doi: 10.1136/gut.30.1.130. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]


