Abstract
Fistula formation between bowel and total hip arthroplasty or revision arthroplasty hardware is rare. We present a case of a 78-year-old woman with protrusio of left hip arthroplasty and acetabular reconstruction hardware that caused direct perforation of the sigmoid colon and fistula formation between the sigmoid colon and the left hip joint. The patient underwent several joint debridements, sigmoid colectomy, and removal of all orthopedic hardware; she ultimately died after two prolonged hospitalizations.
Abbreviations: CT, computed tomography
Introduction
Fistula formation between bowel and total hip arthroplasty or revision arthroplasty hardware is rare (1, 2, 3, 4). Predisposing conditions are the same as those associated with fistulization to the native hip joint, including Crohn’s disease, diverticulitis, steroid use, and pelvic radiation for malignancy (1, 2, 3, 5, 6, 7, 8, 9, 10). Moreover, coloarticular fistula formation can also be a complication of pelvic migration of hip arthroplasty, arthrodesis, or acetabular reconstruction hardware (4, 11, 12, 13, 14, 15). Coloarticular fistulas are associated with high morbidity, and can be fatal due to sepsis. We describe a case of a woman with medial migration of left acetabular reconstruction hardware that caused direct perforation of the sigmoid colon and led to fistula formation between the sigmoid colon and left hip joint, and periarticular soft tissues.
Case report
A 78-year-old woman with a revised left total hip arthroplasty presented to the emergency department with abdominal pain and hypotension seven months after placement of an antiprotrusio cage. Her initial left total hip arthroplasty was in 1998 for osteoarthritis. Ten years later, she developed progressive left hip pain and protrusio of the acetabular component due to central bone weakening. This was treated with a revision of the left total hip arthroplasty, acetabuloplasty with medial acetabular bone grafting, and placement of a unipolar hemiarthroplasty. Ten months following this revision, the patient developed left hip pain, and radiographs showed progressive superomedial migration of the unipolar head. An antiprotrusio cage was placed (Fig. 1).
Figure 1.
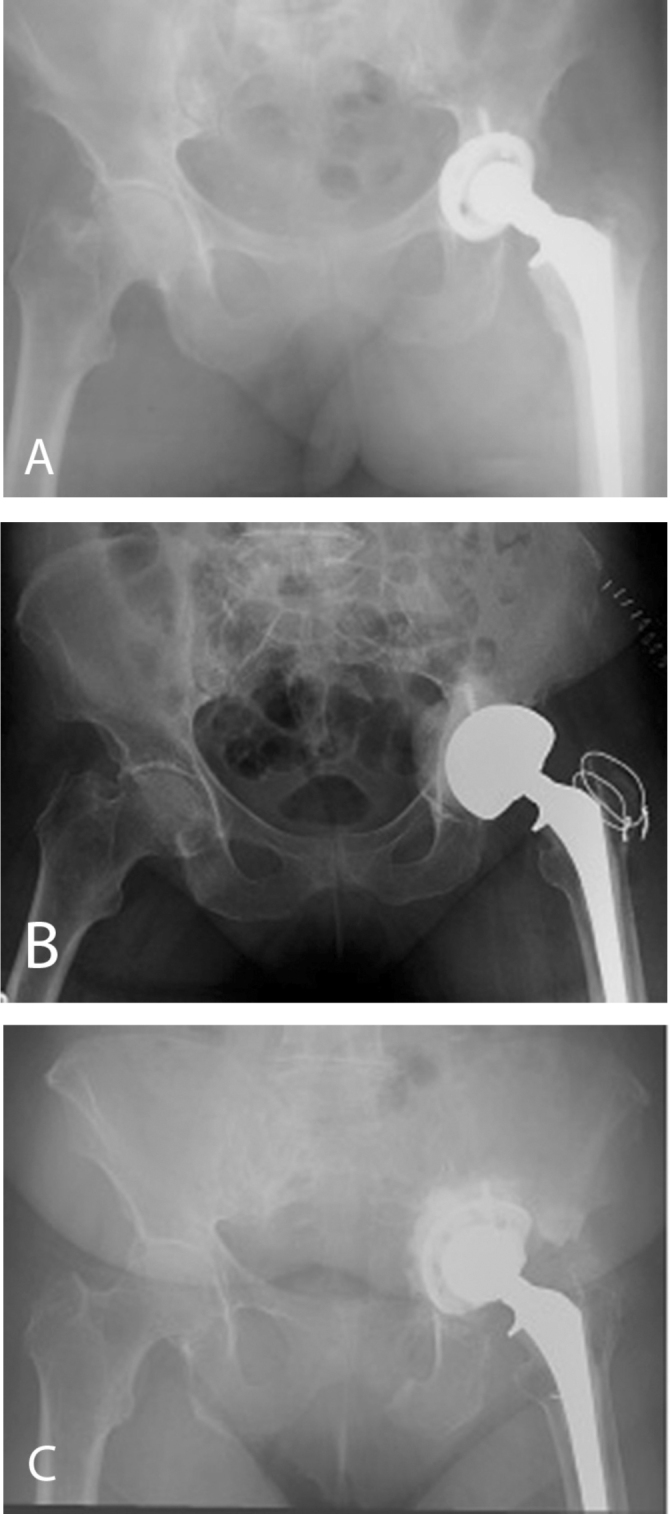
Frontal radiographs of the pelvis after (A) initial total hip arthroplasty in 1998, (B) revision bipolar arthroplasty and acetabular graft in 2008, and (C) acetabular reconstruction and placement of antiprotrusio cage in 2009 showing progressive medial migration of the left acetabular and femoral hardware and left pubic rami insufficiency fractures.
She had a medical history significant for cervical squamous-cell carcinoma (stage IB; limited to the cervix) treated with total hysterectomy in 1993, lymphoma treated with chemotherapy, and splenectomy. She had not received pelvic irradiation and was not on immunosuppressive medications (including steroids).
The patient presented to the emergency department with abdominal pain and was found to be hypotensive and to have a leukocytosis and pyuria. Notably, she did not have symptoms of increased left hip pain, and there was no edema or erythema surrounding the left hip on the initial physical examination.
On presentation, the CT scan of the abdomen and pelvis showed small bowel dilatation, and severe left hip protrusio with medial migration of the acetabular hardware. A portion of the hardware was seen to penetrate the wall of the sigmoid colon, and a large amount of fluid and gas was seen surrounding the left hip and greater trochanter (Fig. 2). Findings were suspicious for sigmoid colon perforation and fistula to the left hip joint and periarticular soft tissues. CT-guided aspiration of the fluid collection lateral to the left greater trochanter demonstrated fecal material, and a culture subsequently grew Escherichia coli, Streptococcus viridans, and Clostridium perfringens.
Figure 2.
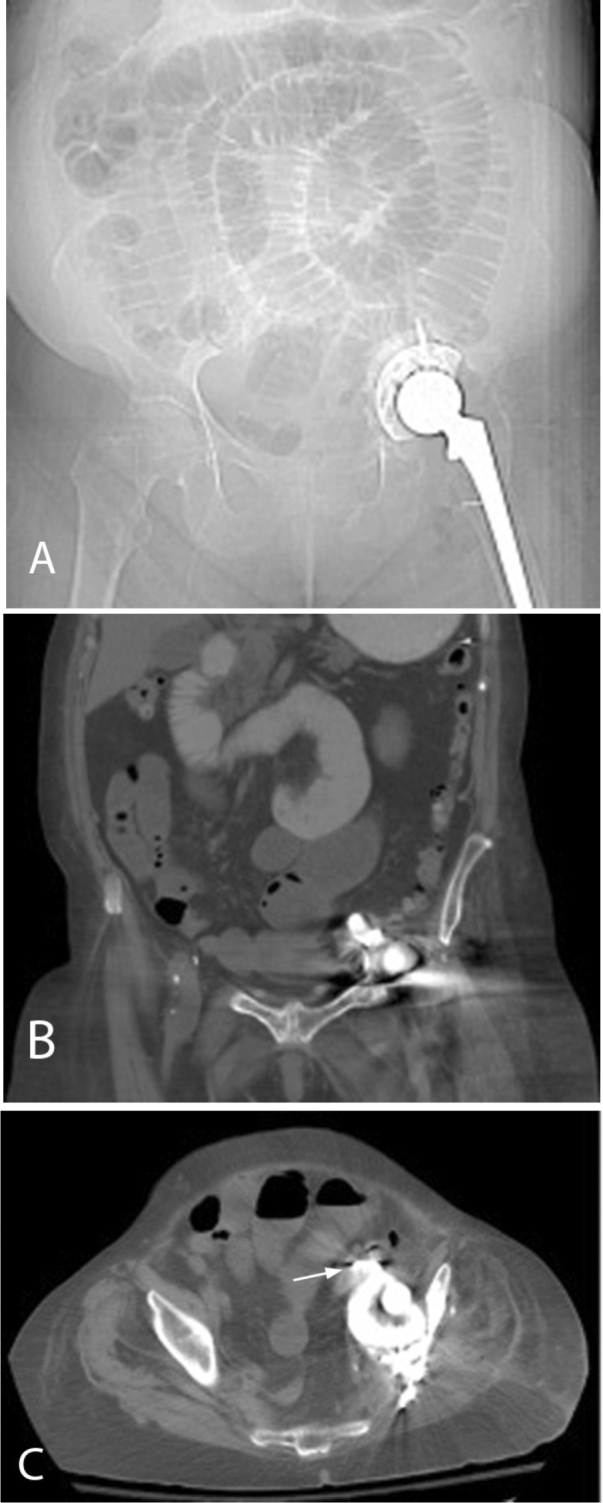
CT examination of the abdomen and pelvis on admission. (A) CT scout image demonstrates multiple dilated loops of small bowel from ileus and severe protrusio of the acetabular and femoral hardware. (B) Coronal and (C) axial CT images of the pelvis show complete discontinuity of the medial acetabular wall, and a hook-shaped flange of the acetabular cage traversing the sigmoid colon wall (arrow).
Surgery revealed a 1-cm titanium flange of the acetabular cage perforating the sigmoid colon (Fig. 3) and proximal small bowel dilatation likely due to ileus. There were no findings of diverticulitis, and the bowel was normally positioned. Sigmoidectomy, Hartmann procedure, end-sigmoid colostomy, and omental coverage of the hardware were performed.
Figure 3.
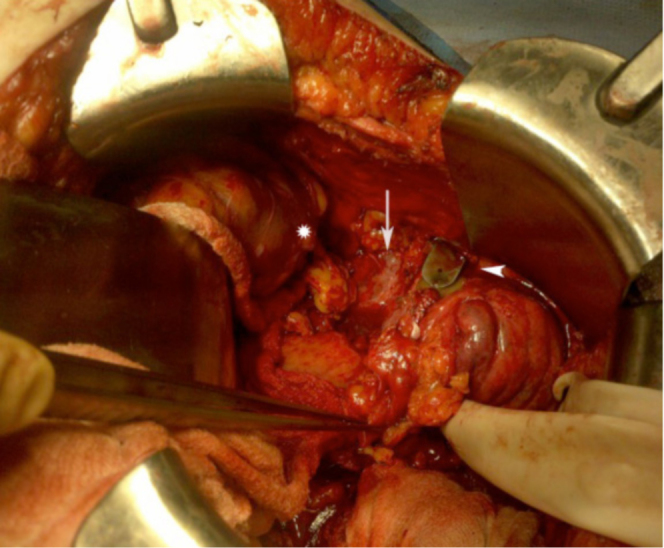
Intraoperative photograph demonstrates the proximity of the penetrating flange of the acetabular cup (arrowhead) to the left external iliac artery (arrow). Note the stapled proximal sigmoid colon (asterisk).
A lateral incision was made over the left hip revealing large pockets of brown fluid in the subcutaneous tissues and involving the vastus lateralis muscle and left hip. Debridement was performed. Cultures from the left hip similarly grew Escherichia coli, Streptococcus viridans, and Clostridium perfringens. Removal of the hardware initially was not attempted due to the high risk of injury to the adjacent left iliac vessels, sciatic nerve, and colon.
Seven left hip joint irrigations/debridements, hip disarticulation, femoral hardware removal, partial acetabular hardware removal, and emergent femoral-femoral arterial bypass for left-lower-extremity ischemia were performed over the initial two-month hospitalization. The first hospitalization was complicated by septicemia that was controlled during a two-week course in the intensive care unit. The patient was readmitted two weeks following initial discharge with gastrointestinal bleeding, infected left pelvic hematoma, and osteomyelitis of the proximal left femur. Decompression of the hematoma and serial irrigation and debridements of the left hip and removal of remaining acetabulum hardware (cemented cup, cage, four screws) were performed. The second hospital course was complicated by an exacerbation of congestive heart failure and aspiration. Three months after initial presentation, the patient became hypotensive and died during her second hospitalization.
Discussion
Fistula formation between the colon and hip joint can be a devastating complication of total hip arthroplasty, associated with a high morbidity and mortality (2, 3, 4, 10, 11, 12, 13, 14). In our patient, multiple prior surgeries were likely the main cause of the coloarticular fistula. However, it is possible that the patient’s immune status played a role, as the patient was susceptible to infection, particularly by encapsulated organisms, due to a previous splenectomy. Unlike the patient in the previous case report by Johnson and Doig (1), our patient had no active diverticular disease; unlike the patient in the case report by Levin et al. (2), our patient had not received previous pelvic radiation.
Similar to our case, there have been at least three previous reports of enteric fistulas communicating with the hip joint after revision total hip arthroplasties. However, our case is, to our knowledge, the first reported case of coloarticular fistula formation following acetabular reconstruction in the absence of other inciting factors such as diverticular disease, steroid treatment, or vascular compromise. We also believe that this is the first case to demonstrate bowel perforation from the acetabular hardware, both on imaging and in the operating suite.
Ridley et al. (14) reported colocutaneous fistula formation in a patient with rheumatoid arthritis on steroids that developed medial migration of the acetabular component of a revision hip arthroplasty. Arnold and Shives (11) reported protrusio of a revision total hip arthroplasty and fistula between the hip joint and sigmoid colon thought to be from inadequate reconstruction of the acetabulum in addition to factors such as previous vascular injury and subsequent tissue necrosis. None of these cases demonstrated direct perforation of bowel by acetabular hardware on imaging or in the operating room, although fistula formation in these cases was likely assumed to be due to previous bowel perforation.
Naito et al. (15) reported a case of small bowel perforation and peritonitis due to migration of an acetabular screw 13 years after a total hip arthroplasty. Perforation of the small bowel was seen in the operating room; however, in contrast to our case, this was an arthroplasty rather than a revision arthroplasty, there were no findings of coloarticular fistula, and the patient recovered well after a small bowel resection.
Moreover, the patient in our report presented with abdominal pain and sepsis rather than symptoms referable to the hip. Past reports of patients with coloarticular fistulas have nearly all presented with hip pain (2, 5, 9, 11, 12, 13, 14). The physical examination and initial lab tests in our patient suggested a gastrointestinal or urinary tract abnormality rather than hip joint infection. Findings of hardware impingement on the sigmoid colon, and fluid and air collections surrounding the hip on the initial abdomen and pelvis CT, prompted the CT-guided trochanteric aspiration, and both studies were important in determining the diagnosis and directing treatment.
This case demonstrates the importance of evaluating the position of hip arthroplasty and acetabuloplasty components on imaging in patients presenting with signs of infection. Although rare, the possibility of direct bowel injury and/or coloarticular fistula formation should be considered, and these patients may not present with hip pain.
Footnotes
Published: August xx, 2011
References
- 1.Johnson MB, Doig SG. Fistula between the hip and a diverticular abscess after revision total hip replacement. The Australian and New Zealand journal of surgery. 2000 Jan;70(1):80–82. doi: 10.1046/j.1440-1622.2000.01755.x. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Levin JS, Rodriguez AA, Luong K. Fistula between the hip and the sigmoid colon after total hip arthroplasty. A case report. The Journal of bone and joint surgery. 1997 Aug;79(8):1240–1242. doi: 10.2106/00004623-199708000-00018. [PubMed] [DOI] [PubMed] [Google Scholar]
- 3.Thompson NW, Swinson BD, Wilson DS, Gardiner K, Beverland DE. Hip arthroplasty complicated by coloarticular sinus formation–a case report. Acta orthopaedica Scandinavica. 2002 Oct;73(5):601–603. doi: 10.1080/000164702321022938. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Bach CM, Steingruber IE, Ogon M, Maurer H, Nogler M, Wimmer C. Intrapelvic complications after total hip arthroplasty failure. American journal of surgery. 2002 Jan;183(1):75–79. doi: 10.1016/s0002-9610(01)00845-5. [PubMed] [DOI] [PubMed] [Google Scholar]
- 5.Tortolani PJ, Kaufman HS, Nahabedian MY, Frassica FJ. Pericapsular fistula of the hip after radiation therapy and resection of a rectal carcinoma. A case report. The Journal of bone and joint surgery. 1999 Nov;81(11):1596–1599. doi: 10.2106/00004623-199911000-00012. [PubMed] [DOI] [PubMed] [Google Scholar]
- 6.Haleem S, Clifton R, Quraishi NA, Hallett JP. ‘Pointing’ in the wrong direction–a case of diverticulitis presenting at the hip. Hip Int. 2008 Jan-Mar;18(1):58–60. doi: 10.1177/112070000801800111. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Messieh M, Turner R, Bunch F, Camer S. Hip sepsis from retroperitoneal rupture of diverticular disease. Orthopaedic review. 1993 May;22(5):597–599. [PubMed] [PubMed] [Google Scholar]
- 8.Passick J, Hirsh DM. Recurrent infection of a total hip arthroplasty associated with radiation-induced ulcerative colitis. A case report. The Journal of arthroplasty. 1989;4(1):87–90. doi: 10.1016/s0883-5403(89)80057-9. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.Peravali R, Purohit N, Dutta S, Mohsen Y. Septic arthritis of the hip: a rare complication of fistulizing Crohn's disease. Colorectal Dis. 2009 Mar;11(3):323–324. doi: 10.1111/j.1463-1318.2008.01610.x. [PubMed] [DOI] [PubMed] [Google Scholar]
- 10.Shreeve DR, Ormerod LP, Dunbar EM. Crohn's disease with fistulae involving joints. Journal of the Royal Society of Medicine. 1982 Dec;75(12):946–948. doi: 10.1177/014107688207501205. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arnold DM, Shives TC. Enterocutaneous fistula complicating total hip arthroplasty. A case report. Clinical orthopaedics and related research. 1992 May;278:108–110. [PubMed] [PubMed] [Google Scholar]
- 12.Bach CM, Nogler M, Wimmer C, Stoeckel B, Ogon M. Fistula between a total hip arthroplasty and the rectum: a case report. Clinical orthopaedics and related research. 2001 Jul;388:143–146. doi: 10.1097/00003086-200107000-00021. [PubMed] [DOI] [PubMed] [Google Scholar]
- 13.Kumar JM, Jowett RL. Fistula between the hip and the caecum. J Bone Joint Surg Br. 1984 Aug;66(4):603. doi: 10.1302/0301-620X.66B4.6746699. [PubMed] [DOI] [PubMed] [Google Scholar]
- 14.Ridley MG, Price TR, Grahame R, Jourdan M, Watson M. Colocutaneous fistula as late complication of total hip replacement in rheumatoid arthritis. Journal of the Royal Society of Medicine. 1985 Nov;78(11):951–952. doi: 10.1177/014107688507801117. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Naito Y, Hasegawa M, Sudo A, Uchida A. Late small intestine perforation after cementless total hip arthroplasty. Hip Int. 2009 Oct-Dec;19(4):399. doi: 10.1177/112070000901900418. [PubMed] 341. [DOI] [PubMed] [Google Scholar]


