Abstract
Background and purpose
Knee pain after total knee arthroplasty (TKA) is not uncommon. Patellar retention in TKA is one cause of postoperative knee pain, and may lead to secondary addition of a patellar component. Patellar resurfacing in TKA is controversial. Its use ranges from 2% to 90% worldwide. In this randomized study, we compared the outcome after patellar resurfacing and after no resurfacing.
Patients and methods
We performed a prospective, randomized study of 74 patients with primary osteoarthritis who underwent a Triathlon CR TKA. The patients were randomized to either patellar resurfacing or no resurfacing. They filled out the VAS pain score and KOOS questionnaires preoperatively, and VAS pain, KOOS, and patient satisfaction 3, 12, and 72 months postoperatively. Physical performance tests were performed preoperatively and 3 months postoperatively.
Results
We found similar scores for VAS pain, patient satisfaction, and KOOS 5 subscales at 3, 12, and 72 months postoperatively in the 2 groups. Physical performance tests 3 months postoperatively were also similar in the 2 groups. No secondary resurfacing was performed in the group with no resurfacing during the first 72 months
Interpretation
Patellar resurfacing in primary Triathlon CR TKA is of no advantage regarding pain, physical performance, KOOS 5 subscales, or patient satisfaction compared to no resurfacing. None of the patients were reoperated with secondary addition of a patellar component within 6 years. According to these results, routine patellar resurfacing in primary Triathlon TKA appears to be unnecessary.
Anterior knee pain has been reported in 6–25% of patients after primary total knee arthroplasty (TKA) with patellar retention (Boyd et al. 1993, Waters and Bentley 2003, Li et al. 2011). Patellar resurfacing in primary TKA is still controversial, and there is a great difference between countries. In North America, more than 90% of surgeons resurface the patella (Abdel et al. 2014). In Australia, 60% patellar resurfacing was performed in primary TKA in 2014 (AOANJRR 2015). In Scandinavia, patellar resurfacing is performed in about 80% of cases in Denmark, while in Norway and Sweden only about 2% of TKAs had patellar resurfacing in 2014 (DKR 2015, Register 2015, SKAR 2015). In Sweden, patellar resurfacing was common in the 1980s when more than two-thirds of primary TKA patients underwent resurfacing. The number steadily decreased, and in 2014 the proportion of patellar resurfacing in primary TKA was only 2.2%, including all diagnoses—even RA (SKAR 2015).
Some surgeons resurface the patella routinely, others not at all, and a third group prefers selective resurfacing. Those who prefer resurfacing on a routine basis argue that the patients have less anterior knee pain, better knee function, and more satisfaction with the operative result; in addition, these patients avoid a possible secondary operation for addition of a patellar component (Mayman et al. 2003, Waters and Bentley 2003, Nizard et al. 2005, Pakos et al. 2005, Parvizi et al. 2005, Berti et al. 2006). Those who do not resurface the patella take into account peroperative and postoperative complications (e.g. fracture, infection, wear, or loosening), longer operation time, and higher cost of material—as well as similar operation outcomes (Grace and Sim 1988, Ortiguera and Berry 2002, Burnett et al. 2009, Lygre et al. 2010, Breeman et al. 2011). The third group of surgeons who recommend resurfacing only in selected cases—especially in patients with RA, patello-femoral symptoms, and obesity—believe that these factors increase the risk of patellar pain postoperatively (Fern et al. 1992, Burnett and Bourne 2004).
In a randomized study of 74 TKAs, we evaluated the effect of patellar resurfacing in Triathlon cruciate retaining knee (CR) TKA using patient-reported outcomes (VAS pain, KOOS, satisfaction), early performance tests, and reoperation as endpoints.
Patients and methods
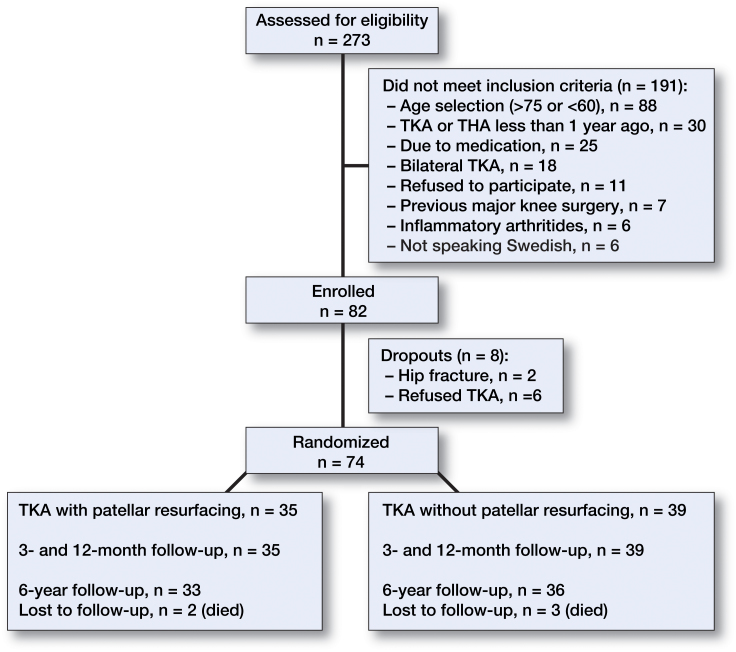
This study involved 74 patients aged between 60 and 75 years with primary osteoarthritis (Table 1 and Figure 1). The exclusion criteria were bilateral TKA, posttraumatic OA (e.g. fractures), previous high tibial osteotomy, rheumatoid arthritis, other forms of arthritis, severe heart failure, neurological disease, diseases that influence physical function, having undergone TKA or THA during the previous 12 months, patellar thickness of less than 22 mm (peroperative measurement), dementia, or being unable to speak Swedish. Patients who used antidepressants, neuroleptics, anticonvulsive drugs, or steroids were also excluded.
Table 1.
Patient characteristics
| Resurfacing group (n = 35) | No-resurfacing group (n = 39) | |
|---|---|---|
| Mean age (SD), years | 68 (4) | 69 (4) |
| Sex: F/M | 21/14 | 24/15 |
| Mean BMI (SD) | 30 (4) | 30 (4) |
| Anesthesia: spinal/general | 30/5 | 32/7 |
Figure 1.
Flow chart of patient selection.
Preoperatively, the patients filled out the KOOS questionnaire (0–100, where 0 means a major problem and 100 means no problem) (Roos et al. 1998) and a visual analog scale (VAS) for pain (0–100 mm, where 0 means no pain and 100 means intolerable pain). A physiotherapist, who was blind regarding the type of surgery, performed the physical performance tests: 20-meter walk test (the time required and number of steps for patients to walk 20 m), chair stand test (the time required for 5 repetitions of rising from a chair and sitting down), knee bending test (the number of single-side knee bendings in 30 s), and knee extension strength (extension power in kg) preoperatively and 3 months postoperatively (Andrews et al. 1996, Martin et al. 2006, Bremander et al. 2007, Villadsen et al. 2012). 3, 12, and 72 months postoperatively, the patients filled out the KOOS questionnaire, VAS pain, and patient satisfaction (very satisfied, satisfied, uncertain, dissatisfied) (Robertsson et al. 2000) (Table 2). 72 months postoperatively, the patient files regarding complications and reoperation were checked in our local complications registry database and also in the SKAR.
Table 2.
Scores used at different time periods
| Preop. | 3 months | 12 months | 6 years | |
|---|---|---|---|---|
| KOOS | + | + | + | + |
| VAS pain | + | + | + | + |
| Patient satisfaction | – | + | + | + |
| Performance tests | + | + | – | – |
The patients were operated on at Trelleborg Hospital between February 2008 and December 2009, by 5 senior orthopedic surgeons subspecialized in arthroplasty surgery. Spinal anesthesia was used as standard in 62 of the 74 patients (Table 1). All the patients had a tourniquet, a standard straight central skin incision, medial parapatellar arthrotomy, and patellar eversion. Preparation of the femur and tibia was done according to the instructions of the manufacturer. If the patellar thickness was less than 22 mm, the patient was excluded. Thereafter, a randomization envelope was opened for allocation of the patient (closed numbered envelopes had been prepared in blocks of 40). When the patient was randomized to patellar resurfacing, preparation of the patella was done according to the Triathlon CR knee system. Tibial, femoral, and patellar components were cemented at the same time. The physiotherapists and patients were kept uninformed about the results of randomization.
The patients in this study were included in 2 other studies, 1 regarding the effect of neuromuscular exercise and surgery on exercise-induced analgesia and pain sensitivity in patients with hip and knee osteoarthritis (Kosek et al. 2013), and the other regarding effects of neuromuscular training on patient-reported outcomes and physical function, also in the same patient groups (Ageberg et al. 2013)
Statistics
The primary endpoint of the study was the VAS pain measurement. A group difference in magnitude of 10–30 mm was considered clinically relevant (Lee et al. 2003, Tashjian et al. 2009). With 56 patients, a group difference in VAS of 15 mm can be detected with 5% statistical significance and 80% power using a 2-sided Student’s t-test. The patient number was increased by 20% to account for patients declining participation, which gave a total patient number of 68. The SD of the endpoint was estimated using a sample from the Swedish Knee Arthroplasty Register of 24,000 patients who had knee surgery and responded to a questionnaire in 2003.We therefore included 74 patients in this study. Fisher’s exact test was used for binomial variable analysis. Any p-value of <0.05 was considered statistically significant. Stata version 12.0 was used for data analysis.
Ethics
The study was performed in compliance with the Helsinki Declaration, and all patients had given their informed consent by signing a written consent form. The study was approved by the ethics committee of the Faculty of Medicine, Lund University (entry no. LU 812006).
Results
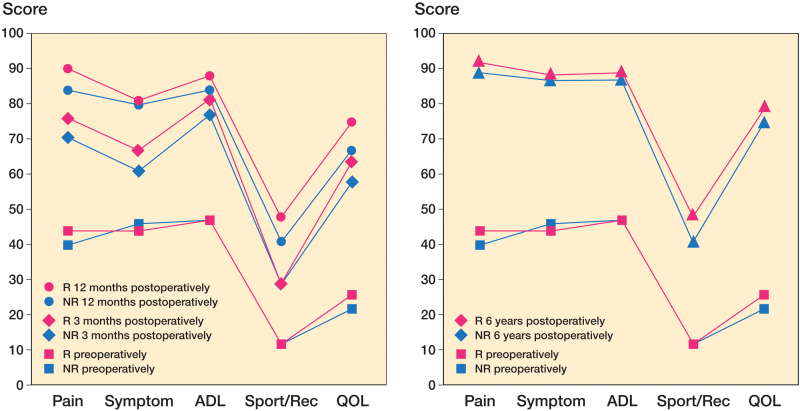
We found statistically significant improvements in VAS pain and KOOS 5 subscales (pain, symptom, ADL, sport/recreation, and quality of daily living (QOL)) in both groups at 3, 12, and 72 months postoperatively, which were similar in both groups (Figure 2, and Tables 3 and 4). We found no statistically significant differences in patient satisfaction at 3, 12, and 72 months postoperatively between the patellar resurfacing group and the no-resurfacing group (Table 3). We found no statistically significant differences in physical performance tests between the 2 groups at 3 months postoperatively. The mean chair stand test results in seconds were 12 in both groups and the mean results of the 20-meter walk test in seconds were 17 in both groups. The mean number of steps was 30 in the patellar resurfacing group, as opposed to 32 in the no-resurfacing group, the number of knee bendings in 30 seconds was 13 in both groups, and knee extension strength was 17 kg in both groups. None of the patients in the no-resurfacing group were reoperated with secondary patellar component addition within the first 72 months.
Figure 2.
KOOS subscales (with 0 meaning worst and 100 meaning best) preoperatively and 3 and 12 months postoperatively (left panel) and properatively and 6 years postoperatively (right panel). R: resurfacing: NR: no resurfacing.
Table 3.
Results. Values are mean (SD) or number of patients
| Missing observation | ||||||
|---|---|---|---|---|---|---|
| R (n = 35) | NR (n = 39) | R | NR | p-value | Difference (95% CI) | |
| VAS pain | ||||||
| preoperatively | 58 (17) | 55 (17) | 0 | 0 | 0.4 | 3 (−10 to 4.9) |
| 3 months postoperatively | 24 (17) | 26 (19) | 0 | 0 | 0.6 | −2 (−9.8 to 4.8) |
| 12 months postoperatively | 15 (19) | 14 (15) | 2 | 3 | 0.6 | 1 (−9.1 to 6.4) |
| 6 years postoperatively | 11 (14) | 10 (15) | 2 | 3 | 0.7 | 1(−6.1 to 8.4) |
| Chair stand test, s | ||||||
| preoperatively | 17 (6) | 16 (7) | 0 | 0 | 0.4 | 1 (−2.0 to 5.2) |
| 3 months postoperatively | 12 (3) | 12 (3) | 2 | 2 | 0.9 | 0 (−1.5 to1.4) |
| 20-m walk test | ||||||
| preoperatively, time, s | 21 (8) | 20 (4) | 0 | 0 | 0.4 | 1 (−1.5 to 3.9) |
| preoperatively, steps | 34 (9) | 33 (5) | 0 | 0 | 0.8 | 1 (−2.9 to 5.5) |
| 3 months postoperatively, time, s | 17 (4) | 17 (2) | 3 | 1 | 0.5 | 0 (−1.0 to 1.9) |
| 3 months postoperatively, steps | 30 (4) | 32 (3) | 3 | 1 | 0.5 | −2 (−1.9 to 1.2) |
| No. of knee bendings in 30 s | ||||||
| preoperatively | 13 (8) | 14 (7) | 4 | 5 | 0.5 | −1 (−5.2 to 2.4) |
| 3 months postoperatively | 13 (7) | 13 (8) | 4 | 3 | 0.9 | 0 (−3.9 to 4.1) |
| Knee extension strength, kg | ||||||
| preoperatively | 18 (6) | 19 (6) | 2 | 1 | 0.5 | −1 (−4.1 to 1.8) |
| 3 months postoperatively | 17 (5) | 17 (6) | 2 | 2 | 0.8 | 0 (−3.2 to 2.6) |
| Very satisfied or satisfied, n | ||||||
| 3 months postoperatively | 33/35 | 38/39 | 0 | 0 | 0.6 | |
| 12 months postoperatively | 34/35 | 37/38 | 0 | 1 | 0.7 | |
| 6 years postoperatively | 31/33 | 34/36 | 2 | 3 | 0.5 | |
R: resurfacing; NR: no resurfacing.
Table 4.
Results of KOOS 5 subscales (with 0 meaning worst and 100 meaning best). Values are mean (SD)
| Missing observation | ||||||
|---|---|---|---|---|---|---|
| R (n = 35) | NR (n = 39) | R | NR | p-value | Difference (95% CI) | |
| Preoperatively | ||||||
| Pain | 40 (14) | 44 (11) | 0 | 0 | 0.3 | −4 (−9.4 to 2.5) |
| Symptoms | 46 (17) | 44 (13) | 0 | 0 | 0.7 | 2 (−5.7 to 8.3) |
| ADL | 47 (17) | 47 (12) | 0 | 0 | 0.9 | 0 (−6.3 to 6.8) |
| Sport/Rec | 12 (12) | 12 (13) | 0 | 0 | 0.9 | 0 (−6.3 to 5.6) |
| QOL | 22 (13) | 26 (12) | 0 | 0 | 0.3 | −4 (−8.9 to 2.5) |
| 3 months postoperatively | ||||||
| Pain | 71 (15) | 76 (14) | 0 | 0 | 0.2 | −5 (−13 to 2.8) |
| Symptoms | 61 (14 | 67 (15 | 0 | 0 | 0.1 | −6 (−13 to 1.5) |
| ADL | 77 (14) | 81 (13) | 0 | 0 | 0.3 | −4 (−9.7 to 2.8) |
| Sport/Rec | 29 (24) | 29 (23) | 0 | 0 | 0.9 | 0 (−12 to 11) |
| QOL | 58 (17) | 64 (20) | 0 | 0 | 0.2 | −6 (−16 to 2.3) |
| 12 months postoperatively | ||||||
| Pain | 84 (16) | 90 (11) | 2 | 1 | 0.6 | −6 (−12 to 0.4) |
| Symptoms | 80 (16) | 81 (15) | 2 | 1 | 0.7 | −1 (−8.9 to 6.3) |
| ADL | 84 (16) | 88 (13) | 2 | 1 | 0.3 | −4 (−11 to 3.1) |
| Sport/Rec | 41 (26) | 48 (28) | 2 | 1 | 0.3 | −7 (−18 to 9.5) |
| QOL | 67 (24) | 75 (21) | 2 | 1 | 0.2 | −8 (−19 to 3.9) |
| 6 years postoperatively | ||||||
| Pain | 89 (11) | 92 (11) | 2 | 3 | 0.4 | −3 (−8.1 to 3.3) |
| Symptoms | 87 (11) | 88 (13) | 2 | 3 | 0.8 | –1 (−6.8 to 5.1) |
| ADL | 87 (17) | 89 (13) | 2 | 3 | 0.6 | −2 (−9.6 to 5.2) |
| Sport/Rec | 41 (25) | 48 (27) | 2 | 3 | 0.3 | −7 (−19 to 6.5) |
| QOL | 75 (20) | 79 (22) | 2 | 3 | 0.5 | −4 (−13 to 6.6) |
R: resurfacing; NR: no resurfacing; QOL: quality of daily living.
Discussion
In this study, patellar resurfacing in TKA had effects on postoperative VAS pain, patient satisfaction, and KOOS at 3, 12, and 72 months that were similar to those of TKA with no resurfacing. The results of physical performance tests at 3 months postoperatively were similar in both groups. There was no secondary patellar addition surgery during the first 72 months in the no-resurfacing group.
One strength of this randomized study was that VAS pain, satisfaction, and KOOS were patient-reported instruments. Another strength was that a physiotherapist who was blind regarding the assignment of patients to groups conducted the performance tests. We included only patients with primary osteoarthritis who were aged between 60 and 75 years, which is a common age for TKA in Sweden (SKAR 2015). It might have been an advantage to include all ages, and patients with other diagnosis. However, the inclusion/exclusion criteria were established in order to make the patients homogenous; for example, activity levels vary with age. The number of surgeons performing the operations may also be regarded as a strength for generalization of the results. The patient-reported outcomes and incidences of surgical complications were almost equal, according to the local registry database for the county of Skåne.
One limitation of the present study may have been the low number of patients. 74 patients may not be a sufficient number to show a small difference between the groups, as both resurfacing and no resurfacing are effective methods for reducing pain and improving knee function with a high degree of satisfaction. At the same time, our power analysis indicated that 74 patients would be a sufficient number to show a statistically significant difference between the groups concerning pain, which is one of the most important outcomes in knee arthroplasty surgery. Our primary endpoint was VAS pain score. A more relevant pain might be anterior knee pain. To our knowledge, there is no well-documented method available for measurement of this type of pain after knee replacement. It would also have been an advantage if we had also had postoperative performance tests at 12 months. However, at that time VAS pain scores and KOOS subscale scores were similar between the groups, so the results of performance tests would probably also have been similar.
In Sweden, patellar resurfacing in primary TKA has steadily decreased since the 1980s, from more than 70% to about 2% (SKAR 2015). One explanation would be improvement in the design of the patello-femoral joint in modern prostheses, which means that even for non-resurfaced patellas, the prosthesis offers better patello-femoral articulation. Also, the surgical technique—especially the positioning of the femoral and tibial components—has received more attention. Both of these factors may have had a role in the results we obtained, as no patellar additions were performed within 6 years. However, after more than 4 decades there is still no consensus between different countries and different surgeons on how to deal with the patella in TKA. We did not take into account the degree of OA of the patella, which is actually the praxis according to the surgeons who always replace patellas. We wanted to compare this attitude to the alternative one, which is not replacing the patella irrespective of the degree of patellar OA.
Several meta-analyses of RCT studies have not shown any statistically significant differences between resurfacing and no-resurfacing groups regarding anterior knee pain, knee function, and satisfaction, but a higher incidence of reoperations in no-resurfacing groups (He et al. 2011, Li et al. 2011, Pavlou et al. 2011, Pilling et al. 2012). On the other hand, there have also been several meta-analyses favoring patellar resurfacing in TKA (Forster 2004, Nizard et al. 2005, Pakos et al. 2005, Parvizi et al. 2005). One reason for more reoperations in the no-resurfacing groups might be postoperative knee pain—which can be explained by patello-femoral dysfunction, and the surgeon has one more operation to offer which cannot be offered to the group that already has a resurfaced patella. However, there are many possible reasons for knee pain other than an unresurfaced patella, such as scar discomfort, numbness, neuromas, bursitis, tendinitis, patellar instability, patellar fracture, or muscle weakness. In an observational Norwegian registry study, Lygre et al. (2010) found that resurfacing of the patella has no better effect on pain or knee function after TKA. On the other hand, in one of the largest RCT studies involving 514 patients, Waters and Bentley (2003) recommended patellar resurfacing in TKA because of less anterior knee pain. They found anterior knee pain in 25% of cases with no resurfacing as compared to 5% in resurfacing group. Finally, Parvizi et al. (2012) found that secondary resurfacing was not always a rewarding procedure, as 8 of 39 patients who underwent secondary resurfacing failed because of anterior knee pain. No patients in the no-resurfacing group in our study needed secondary patellar component addition. The number of satisfied patients was very high in both groups. Many of the TKA designs in the reference studies mentioned above are no longer in use, which makes comparison with the current prosthesis not fully relevant—because of continuous improvement of the patello-femoral articulation since that time.
An important advantage in the present study was the use of KOOS at different periods of the follow-up. It is well known that there is a disparity between patients’ and surgeons’ opinions of the result postoperatively (Lieberman et al. 1996, Gioe et al. 2009, Khanna et al. 2011). In the majority of previous RCT studies, no PROMs—such as KOOS—were used, which contrasts with our study. We believe that it is justified to express the result according to patient-reported outcomes rather than the doctor’s opinion.
One idea of this study was a very early check of the 2 knee arthroplasty groups, where both questionnaires and performance tests were used to help identify possible differences. Early and medium-term outcome were also assessed, to obtain a reasonably complete view of the time-related outcome. In both groups, compared to preoperative data we found lower VAS pain scores and improvements in all KOOS subscales, while physical performance test results were relatively similar to the preoperative values—which may have been due to the fact that 3 months is a short time to evaluate outcome after TKA (Nilsdotter et al. 2009). It is interesting that, for both groups, the degree of patient satisfaction was high and rather equal at 3, 12, and 72 months, while VAS pain was becoming less with longer observation time. Although patellar resurfacing is an additional trauma to the knee, at 3 months postoperatively it did not cause poorer performance than no resurfacing. For example, values for knee extension strength and number of knee bendings in 30 seconds were roughly equal to the preoperative values.
In summary, there is still remarkable controversy between countries and between surgeons regarding how to deal with the patella in TKA. Thus, there is a need for more RCT studies with modern prostheses and with follow-up using instruments for patient-reported outcome. In this study, we could not find any advantage of patellar resurfacing—either from short-term follow-up or from medium-term follow-up—regarding knee pain, KOOS, knee function, and patient satisfaction. None of the patients in the no-resurfacing group were reoperated with patellar component addition. Based on these findings, we believe that routine patellar resurfacing in primary Triathlon CR TKA is unnecessary.
We thank Professor Lars Lidgren, Department of Orthopedics, Clinical Sciences, Lund University, for valuable advice and encouragement, and Professor Jonas Ranstam, RC Syd, Clinical Sciences, Lund University, for advice on statistics. We are grateful to Ulrik Hansson, Gunnar Flivik, and Uldis Kesteris for recruitment and operation of patients, and Pia Schoug, physiotherapist, for pre- and postoperative evaluation of performance tests and collection of material. We thank all the medical staff of the Orthopedics Department at Trelleborg Hospital for excellent cooperation.
Financial support was received from Region Skåne, the Erik and Angelica Sparre Foundation, and the Medical Faculty of Lund University.
AA collected and analyzed the data, and prepared the manuscript. AA, AL, and MS recruited patients, performed the surgery, and followed up the patients. All the authors designed the study and helped in writing the manuscript.
No competing interests declared.
References
- Abdel M P, Parratte S, Budhiparama N C.. The patella in total knee arthroplasty: to resurface or not is the question. Curr Rev Musculoskelet Med 2014; 7 (2): 117–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ageberg E, Nilsdotter A, Kosek E, Roos E M.. Effects of neuromuscular training (NEMEX-TJR) on patient-reported outcomes and physical function in severe primary hip or knee osteoarthritis: a controlled before-and-after study. BMC Musculoskelet Disord 2013; 14: 232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews A W, Thomas M W, Bohannon R W.. Normative values for isometric muscle force measurements obtained with hand-held dynamometers. Phys Ther 1996; 76 (3): 248–59. [DOI] [PubMed] [Google Scholar]
- AOANJRR The Australian Orthopaedic Association National Joint Replacement Rigestry. 2015. [Google Scholar]
- Berti L, Benedetti M G, Ensini A, Catani F, Giannini S.. Clinical and biomechanical assessment of patella resurfacing in total knee arthroplasty. Clin Biomech (Bristol, Avon) 2006; 21 (6): 610–6. [DOI] [PubMed] [Google Scholar]
- Boyd A D Jr., Ewald F C, Thomas W H, Poss R, Sledge C B.. Long-term complications after total knee arthroplasty with or without resurfacing of the patella. J Bone Joint Surg (Am) 1993; 75 (5): 674–81. [DOI] [PubMed] [Google Scholar]
- Breeman S, Campbell M, Dakin H, Fiddian N, Fitzpatrick R, Grant A, et al. Patellar resurfacing in total knee replacement: five-year clinical and economic results of a large randomized controlled trial. J Bone Joint Surg (Am) 2011; 93 (16): 1473–81. [DOI] [PubMed] [Google Scholar]
- Bremander A B, Dahl L L, Roos E M.. Validity and reliability of functional performance tests in meniscectomized patients with or without knee osteoarthritis. Scand J Med Sci Sports 2007; 17 (2): 120–7. [DOI] [PubMed] [Google Scholar]
- Burnett R S, Bourne R B.. Indications for patellar resurfacing in total knee arthroplasty. Instr Course Lect 2004; 53: 167–86. [PubMed] [Google Scholar]
- Burnett R S, Boone J L, Rosenzweig S D, Steger-May K, Barrack R L.. Patellar resurfacing compared with nonresurfacing in total knee arthroplasty. A concise follow-up of a randomized trial. J Bone Joint Surg (Am) 2009; 91 (11): 2562–7. [DOI] [PubMed] [Google Scholar]
- DKR Danish Knee Arthroplasty Register. 2015. [Google Scholar]
- Fern E D, Winson I G, Getty C J.. Anterior knee pain in rheumatoid patients after total knee replacement. Possible selection criteria for patellar resurfacing. J Bone Joint Surg (Br) 1992; 74 (5): 745–8. [DOI] [PubMed] [Google Scholar]
- Forster M C. Patellar resurfacing in total knee arthroplasty for osteoarthritis: a systematic review. Knee 2004; 11 (6): 427–30. [DOI] [PubMed] [Google Scholar]
- Gioe T J, Pomeroy D, Suthers K, Singh J A.. Can patients help with long-term total knee arthroplasty surveillance? Comparison of the American Knee Society Score self-report and surgeon assessment. Rheumatology 2009; 48 (2): 160–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grace J N, Sim F H.. Fracture of the patella after total knee arthroplasty. Clin Orthop Relat Res 1988; (230): 168–75. [PubMed] [Google Scholar]
- He J Y, Jiang L S, Dai L Y.. Is patellar resurfacing superior than nonresurfacing in total knee arthroplasty? A meta-analysis of randomized trials. Knee 2011; 18 (3): 137–44. [DOI] [PubMed] [Google Scholar]
- Khanna G, Singh J A, Pomeroy D L, Gioe T J.. Comparison of patient-reported and clinician-assessed outcomes following total knee arthroplasty. J Bone Joint Surg (Am) 2011; 93 (20): e117(1)–(7). [DOI] [PubMed] [Google Scholar]
- Kosek E, Roos E M, Ageberg E, Nilsdotter A.. Increased pain sensitivity but normal function of exercise induced analgesia in hip and knee osteoarthritis–treatment effects of neuromuscular exercise and total joint replacement. Osteoarthritis Cartilage 2013; 21 (9): 1299–307. [DOI] [PubMed] [Google Scholar]
- Lee J S, Hobden E, Stiell I G, Wells G A.. Clinically important change in the visual analog scale after adequate pain control. Acad Emerg Med 2003; 10 (10): 1128–30. [DOI] [PubMed] [Google Scholar]
- Li S, Chen Y, Su W, Zhao J, He S, Luo X.. Systematic review of patellar resurfacing in total knee arthroplasty. Int Orthop 2011; 35 (3): 305–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman J R, Dorey F, Shekelle P, Schumacher L, Thomas B J, Kilgus D J, et al. Differences between patients’ and physicians’ evaluations of outcome after total hip arthroplasty. J Bone Joint Surg (Am) 1996; 78 (6): 835–8. [DOI] [PubMed] [Google Scholar]
- Lygre S H, Espehaug B, Havelin L I, Vollset S E, Furnes O.. Does patella resurfacing really matter? Pain and function in 972 patients after primary total knee arthroplasty. Acta Orthop 2010; 81 (1): 99–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin H J, Yule V, Syddall H E, Dennison E M, Cooper C, Aihie Sayer A.. Is hand-held dynamometry useful for the measurement of quadriceps strength in older people? A comparison with the gold standard Bodex dynamometry. Gerontology 2006; 52 (3): 154–9. [DOI] [PubMed] [Google Scholar]
- Mayman D, Bourne R B, Rorabeck C H, Vaz M, Kramer J.. Resurfacing versus not resurfacing the patella in total knee arthroplasty: 8- to 10-year results. J Arthroplasty 2003; 18 (5): 541–5. [DOI] [PubMed] [Google Scholar]
- Nilsdotter A K, Toksvig-Larsen S, Roos E M.. A 5 year prospective study of patient-relevant outcomes after total knee replacement. Osteoarthritis Cartilage 2009; 17 (5): 601–6. [DOI] [PubMed] [Google Scholar]
- Nizard R S, Biau D, Porcher R, Ravaud P, Bizot P, Hannouche D, et al. A meta-analysis of patellar replacement in total knee arthroplasty. Clin Orthop Relat Res 2005; (432): 196–203. [DOI] [PubMed] [Google Scholar]
- Ortiguera C J, Berry D J.. Patellar fracture after total knee arthroplasty. J Bone Joint Surg (Am) 2002; 84-A (4): 532–40. [DOI] [PubMed] [Google Scholar]
- Pakos E E, Ntzani E E, Trikalinos T A.. Patellar resurfacing in total knee arthroplasty. A meta-analysis. J Bone Joint Surg (Am) 2005; 87 (7): 1438–45. [DOI] [PubMed] [Google Scholar]
- Parvizi J, Rapuri V R, Saleh K J, Kuskowski M A, Sharkey P F, Mont M A.. Failure to resurface the patella during total knee arthroplasty may result in more knee pain and secondary surgery. Clin Orthop Relat Res 2005; 438: 191–6. [DOI] [PubMed] [Google Scholar]
- Parvizi J, Mortazavi S M, Devulapalli C, Hozack W J, Sharkey P F, Rothman R H.. Secondary resurfacing of the patella after primary total knee arthroplasty does the anterior knee pain resolve? J Arthroplasty 2012; 27 (1): 21–6. [DOI] [PubMed] [Google Scholar]
- Pavlou G, Meyer C, Leonidou A, As-Sultany M, West R, Tsiridis E.. Patellar resurfacing in total knee arthroplasty: does design matter? A meta-analysis of 7075 cases. J Bone Joint Surg (Am) 2011; 93 (14): 1301–9. [DOI] [PubMed] [Google Scholar]
- Pilling R W, Moulder E, Allgar V, Messner J, Sun Z, Mohsen A.. Patellar resurfacing in primary total knee replacement: a meta-analysis. J Bone Joint Surg (Am) 2012; 94 (24): 2270–8. [DOI] [PubMed] [Google Scholar]
- Register N. The Norwegian Arthroplasty Register. http://nrlwebihelsenet/eng/defaulthtm 2015. [Google Scholar]
- Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L.. Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand 2000; 71 (3): 262–7. [DOI] [PubMed] [Google Scholar]
- Roos E M, Roos H P, Ekdahl C, Lohmander L S.. Knee injury and Osteoarthritis Outcome Score (KOOS)–validation of a Swedish version. Scand J Med Sci Sports 1998; 8 (6): 439–48. [DOI] [PubMed] [Google Scholar]
- SKAR Swedish Knee Arthroplasty Register. Annual report 2015, Lunds University Hospital, Lund, http://mykneese/2015. [Google Scholar]
- Tashjian R Z, Deloach J, Porucznik C A, Powell A P.. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elbow Surg 2009; 18 (6): 927–32. [DOI] [PubMed] [Google Scholar]
- Waters T S, Bentley G.. Patellar resurfacing in total knee arthroplasty. A prospective, randomized study. J Bone Joint Surg (Am) 2003; 85-A (2): 212–7. [DOI] [PubMed] [Google Scholar]
- Villadsen A, Roos E M, Overgaard S, Holsgaard-Larsen A.. Agreement and reliability of functional performance and muscle power in patients with advanced osteoarthritis of the hip or knee. Am J Phys Med Rehabil 2012; 91 (5): 401–10. [DOI] [PubMed] [Google Scholar]