Abstract
MRI is well established in the diagnosis of female breast cancer, with an important role as a problem-solving tool in the postoperative breast and in implant evaluation. Little in the literature mentions the use of MRI in male breast cancer, with there is no clear role for its use at present. We present an unusual case of bilateral male breast carcinoma and demonstrate a similar enhancement pattern to that described in female breast cancer; we also suggest other potential applications of MRI for the male breast.
Abbreviations: MRI, magnetic resonance imaging
Case report
A 72-year-old man underwent a followup mammogram of the right breast as routine surveillance following a mastectomy for grade II, estrogen- and progesterone-positive, invasive ductal carcinoma of the left breast four years previously. He continued to take tamoxifen following the previous operation. The mammogram demonstrated a 6mm opacity deep to the breast tissue in the retroareolar region (Fig. 1) that was not present on the mammogram from the previous year and was impalpable on examination. An ultrasound was unable to identify a lesion.
Figure 1.
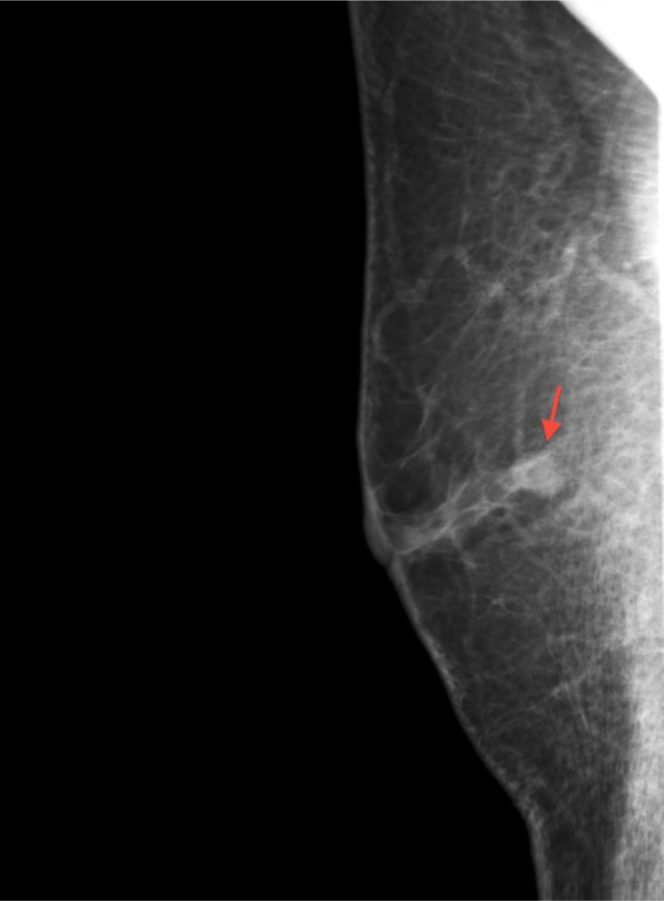
72-year-old man with breast carcinoma. Mediolateral oblique (MLO) mammogram of the right breast showing a 6mm retro-areolar rounded opacity (arrow) deep to the nipple.
Contrast-enhanced magnetic resonance imaging (MRI) demonstrated a 6mm, well-defined nodule deep to the retroareolar breast tissue that was of decreased signal intensity on the T1-weighted images and increased signal intensity on the STIR images. The lesion demonstrated a malignant-type enhancement curve after administration of IV gadolinium, with avid early enhancement and rapid washout (Fig. 2). A repeat ultrasound confirmed the anatomical location of the lesion and demonstrated a isoechoic solid nodule that correlated with the lesion seen on MRI (Fig. 3). Core biopsy revealed a grade I, estrogen-receptor-positive, invasive ductal carcinoma.
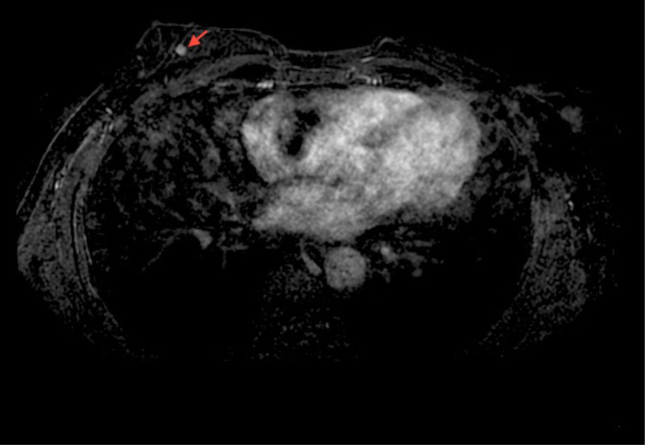
Figure 2.
72-year-old man with breast carcinoma. Axial, postcontrast, T1W fat-suppressed MRI image performed immediately after IV gadolinium administration, showing a circumscribed and avidly enhancing nodule in the right breast (arrow).
Figure 3.
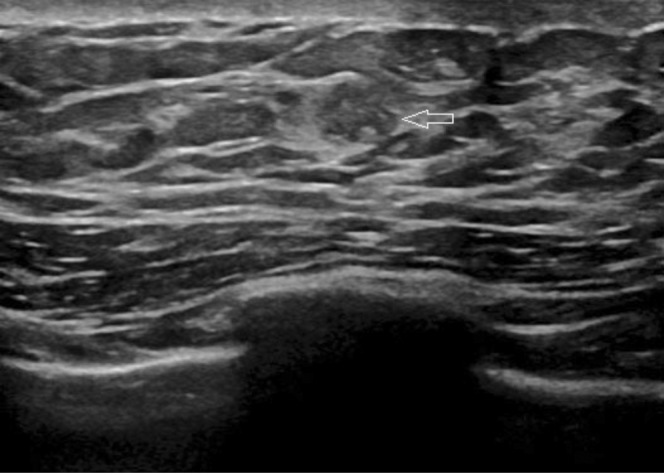
72-year-old man with breast carcinoma. Focused ultrasound of the right breast confirms an ill-defined and isoechoic nodule deep to the right nipple, correlating with the lesion seen on previous imaging (arrow).
The patient underwent a simple mastectomy, sparing the axilla, and remains well on tamoxifen with no evidence of recurrence.
Discussion
Male breast carcinoma is rare and accounts for only 1% of all breast cancers, less than 1% of all male cancers (1, 2), with the incidence of contralateral breast cancer reported as 2.7%(3).
Traditionally, single-view mammography is the first-line approach and is highly sensitive and specific for breast cancer in men, with mammographic features similar to those found in female breast cancer.
Ultrasound is also well described in the evaluation of male breast cancer; again, features are similar to those seen in the female. With the most common location of male breast cancer being eccentric to the nipple, location of the lesion can sometimes be difficult due to dense acoustic shadowing at the nipple level, obscuring the retroareolar region, as demonstrated in our case. Difficulty in location of the lesion was also compounded in this case because the lesion was of similar texture to surrounding breast tissue.
In our case, we were able to demonstrate a similar enhancement pattern to that described in female breast cancer. Other potential applications of MRI could be in lesion demonstration with associated gynecomastia; it could also improve demonstration of chest-wall invasion. Although it may be technically difficult, MRI can be used successfully in the evaluation of the male breast, and its use should be recommended particularly in cases where initial imaging is equivocal.
Footnotes
Published: July 20, 2011
References
- 1.Landis SH, Murray T, Bolden S, Wingo PA. Cancer statistics, 1999. CA Cancer J Clin. 1999;49:8. doi: 10.3322/canjclin.49.1.8. [PubMed] 3. [DOI] [PubMed] [Google Scholar]
- 2.Weiss JR, Moysich KB, Swede H. Epidemiology of male breast cancer. Cancer Epidemiol Biomarkers Prev. 2005 Jan;14(1):20–26. [PubMed] [PubMed] [Google Scholar]
- 3.Cutuli BF, Lacroze M, Dilhuydy JM, Florentz P, Velten M, Allavena C. Breast cancer in men: incidence and types of associated previous synchronous and metachronous cancers. Bull Cancer. 1992;79:689–696. [PubMed] [PubMed] [Google Scholar]