Abstract
Transcatheter embolization is the first-line treatment for massive hemoptysis and recurrent intractable hemoptysis. Proximal interruption of the pulmonary artery is a rare congenital anomaly characterized by hypertrophy and neovasculsarity of bronchial and nonbronchial aortopulmonary collaterals; hemoptysis complicates a minority of cases. We present a case of unilateral proximal interruption of the left pulmonary artery associated with a right-sided aorta, presenting in adulthood with hemoptysis. The patient was managed emergently with bronchial, intercostal, and inferior phrenic artery embolization.
Introduction
Proximal interruption of the pulmonary artery (PIPA) is a rare congenital anomaly with an estimated prevalence of 1 in 200,000 (1). Since patients can remain asymptomatic for a long period, the precise prevalence is difficult to establish. Furthermore, symptomatic PIPA may go unrecognized due to nonspecific symptoms, including recurrent pulmonary infections, decreased exercise tolerance, and mild dyspnea on exertion. The incidence of associated pulmonary hypertension is approximately 19–27% (2). Hemoptysis is a relatively rare presentation of PIPA, complicating approximately 10–20% of cases (2, 3). Historically, many symptomatic cases have been managed surgically with pneumonectomy; little is known about the outcomes of transcatheter embolization, given the rarity of this entity.
Case report
A 28-year-old white male presented with coughing and frank hemoptysis, preceded by a “moist and heavy” sensation in his chest. Following hemoptysis of approximately three quarters of a cup, the sputum eventually cleared with repetitive coughing. He reported similar episodes six months prior that occurred twice daily for a period of two weeks. These episodes resolved spontaneously without medical attention.
Chest radiography upon arrival at a community emergency room showed a right-sided aortic arch, diminutive left hilum, small left hemithorax, and left-sided rib notching (Fig. 1). A CT pulmonary angiogram revealed proximal interruption of the left pulmonary artery and enlarged systemic collaterals (Fig. 2). Ground glass opacity in the left lower lobe (not depicted), consistent with pulmonary hemorrhage, was also present. The patient remained hemodynamically stable and was transferred to our institution for further evaluation and treatment.
Figure 1.
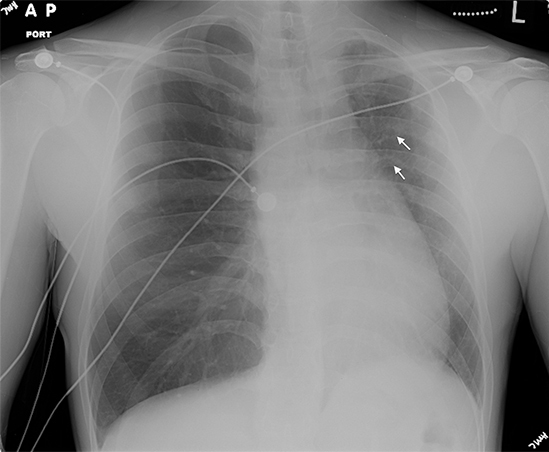
28-year-old male with massive hemoptysis and recurrent intractable hemoptysis. Frontal chest radiograph: right-sided aortic arch, diminutive left hilum, small left lung hemithorax, and left-sided rib notching (white arrows).
Figure 2.
28-year-old male with massive hemoptysis and recurrent intractable hemoptysis. CT pulmonary angiogram: right-sided aortic arch, absent left pulmonary artery, and dilated aortopulmonary collateral arteries.
Thoracic aortography showed multiple enlarged bronchial, intercostal, and phrenic collaterals with significant neovascularity (Fig. 3a). Selective angiography of these vessels was then performed with a 5-French diagnostic catheter. No active extravasation was identified. After stable, deeper catheterization was achieved with a Progreat microcatheter (Progreat Microcatheter System, Terumo, UK), embolization of two left bronchial arteries, the left eighth and tenth intercostal arteries, and the left inferior phrenic artery was performed to near stasis with 350–500 micron polyvinyl alcohol particles (PVA). Angiography of the seventh and ninth intercostal arteries demonstrated communication to the anterior spinal artery, preventing safe embolization of these vessels (Fig. 3b).
Figure 3A.
28-year-old male with massive hemoptysis and recurrent intractable hemoptysis. Catheter angiography: Dilated tortuous bronchial and intercostal arteries arising from a right-sided aortic arch.
Figure 3B.

28-year-old male with massive hemoptysis and recurrent intractable hemoptysis. Catheter angiography: Spinal artery communicating with the posterior ninth intercostal artery (arrow).
The patient tolerated the procedure well, with the exception of mild, left-sided chest pain. He was discharged one day after the embolization with near resolution of his hemoptysis. Four months after the embolization, he endorsed intermittent cough but no hemoptysis in the interim. There are no current plans for surgery.
Discussion
The exact pathogenesis of PIPA is unknown but is thought to be due to a connection failure between the sixth aortic arch and the pulmonary trunk during embryologic development (4). It may involve either the left or the right pulmonary artery. Although more commonly referred to as unilateral absence or agenesis of the pulmonary artery, the term “proximal interruption” has been used interchangeably and emphasizes the preservation of the intrapulmonary vascular network. PIPA of the left pulmonary artery is frequently associated with other cardiovascular abnormalities such as Tetralogy of Fallot, right aortic arch, patent ductus arteriosus, and septal defects—whereas the interruption of the right pulmonary artery is usually an isolated finding (1). Regardless of laterality, hypervascularity and hypertrophy of the systemic collateral blood supply formed by branches of the bronchial, intercostal, subclavian, or subdiaphragmatic arteries lead to vascular ectasia in the bronchial submucosa (2). The resultant rupture and hemoptysis complicates approximately 10–20% of reported cases, varying from self-limited to massive with life-threatening pulmonary hemorrhage (3).
Chest radiography may suggest the diagnosis with an absent hilar shadow, a small volume of the ipsilateral lung, and/or ipsilateral rib notching. In cases of hemoptysis, consolidation may be present. Cross-sectional imaging and/or angiography are diagnostic and better characterize the extent of collateral circulation.
Cases of PIPA complicated by hemoptysis, recurrent pulmonary infections, or intractable pulmonary hypertension necessitate intervention (2). Although pneumonectomy with ligation of collaterals or reanastomosis of the peripheral pulmonary artery with the main pulmonary artery is a more definitive treatment, these major operations carry significant risks and may not be feasible in the emergent setting. Transcatheter embolization of aortopulmonary collaterals, either alone or as an adjunct to surgery, has shown to be a safe and effective treatment of hemoptysis related to PIPA in a small number of case reports (5, 6, 7).
Fortunately, the literature regarding embolotherapy technique and outcomes for hemoptysis from other etiologies is more robust (8, 9, 10). Absorbable gelatin sponge (Gelfoam) is widely accessible. However, recanalization does occur over time, which could result in recurrent hemorrhage. Permanent embolics include particles such as polyvinyl alcohol (PVA) and spherical agents, liquid agents such as “glue” (n-butyl-2-cyanoacrylate), and mechanical agents such as coils. In cases of bronchial artery embolization, coils should be avoided due to their propensity to occlude more proximal vessels as well as due to the preclusion of subsequent embolization in case of recurrent hemorrhage.
Embolization of the bronchial artery and other systemic collaterals (in the setting of hemoptysis from all etiologies) has very good outcomes, with immediate technical success in 73–99% of patients (10). Unfortunately, recurrence is also relatively common, occurring in 10–55.3% of all patients embolized (10). Recurrent cases may be managed via repeated embolization or surgery, depending on the patient’s status and the underlying etiology of the hemoptysis. Although the outcomes for transcatheter management for PIPA in particular are not known, transcatheter embolization should be considered as a treatment modality with or without surgical intervention, based on the associated literature.
Proximal interruption of the pulmonary artery is rare, and hemoptysis complicates only 10–20% of reported cases. While pneumonectomy has been the definitive treatment historically, the operation carries significant risks, particularly in the emergent setting. In contrast, transcatheter embolization offers less risk with control of hemorrhage in the majority of cases, as demonstrated by our patient. Transcatheter management should be considered as a potential first-line treatment in the majority of cases, although the long-term outcomes of transcatheter management alone versus with delayed surgical treatment may warrant further investigation.
Footnotes
Published: August 24, 2013
References
- 1.Griffin N, Mansfield L, Redmond KC, Dusmet M, Goldstraw P, Mittal TK, Padley S. Imaging features of isolated unilateral pulmonary artery agenesis presenting in adulthood: a review of four cases. Clin Radiol. 2007;62(3):238–244. doi: 10.1016/j.crad.2006.10.006. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Cogswell TL, Singh S. Agenesis of the left pulmonary artery as a cause of hemoptysis. Angiology. 1986;37(3):154. doi: 10.1177/000331978603700303. [PubMed] [DOI] [PubMed] [Google Scholar]
- 3.Ten Harkel AD, Blom NA, Ottenkamp J. Isolated unilateral absence of a pulmonary artery: a case report and review of the literature. Chest. 2002;122(4):1471–1477. doi: 10.1378/chest.122.4.1471. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Apostolopoulou SC, Kelekis NL, Brountzos EN, Rammos S, Kelekis DA. Absent pulmonary artery in one adult and five pediatric patients: imaging, embryology, and therapeutic implications. AJR Am J Roentgenol. 2002;179:1253–1260. doi: 10.2214/ajr.179.5.1791253. [PubMed] [DOI] [PubMed] [Google Scholar]
- 5.Mehta AC, Livingston DR, Kawalek W, Golish JA, O'Donnell JK. Pulmonary artery agenesis presenting as massive hemoptysis: a case report. Angiology. 1987;38(1):67–71. doi: 10.1177/000331978703800110. [PubMed] [DOI] [PubMed] [Google Scholar]
- 6.Reñé M, Sans J, Dominguez J, Sancho C, Valldeperas J. Unilateral pulmonary artery agenesis presenting with hemoptysis: treatment by embolization of systemic collaterals. Cardiovasc Intervent Radiol. 1995;18(4):251. doi: 10.1007/BF00239422. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Sancho C, Domínguez J, Escalante E, Hernandez E, Cairols M, Martinez X. Embolization of an anomalous bronchial artery aneurysm in a patient with agenesis of the left pulmonary artery. J Vasc Interv Radiol. 1999;10:1122–1126. doi: 10.1016/s1051-0443(99)70202-2. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Yoon W, Kim JK, Kim YH, Chung TW, Kang HK. Bronchial and nonbronchial systemic artery embolization for life-threatening hemoptysis: a comprehensive review. Radiographics. 2002;22:1395–1409. doi: 10.1148/rg.226015180. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.Lopez JK, Lee HY. Bronchial artery embolization for treatment of life-threatening hemoptysis. Semin Intervent Radiol. 2006;23(3):223–229. doi: 10.1055/s-2006-948759. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chun JY, Morgan R, Belli AM. Radiological management of hemoptysis: a comprehensive review of diagnostic imaging and bronchial arterial embolization. Cardiovasc Intervent Radiol. 2010;33:240–250. doi: 10.1007/s00270-009-9788-z. [PubMed] [DOI] [PubMed] [Google Scholar]




