Abstract
We present a patient with a remote history of splenectomy and recent hemicolectomy for colon adenocarcinoma. On routine surveillance chest/abdomen/pelvis CT, a lesion suspicious for hepatic metastasis was identified. Followup MRI was inconclusive. For more specific tissue characterization, imaging with Tc-99m heat-damaged RBCs was obtained to guide further patient management. Tc-99m–labeled, heat-damaged RBC scintigraphy is an underused modality that is highly specific for detecting ectopic or accessory splenic tissue. There have been many reported cases of patients undergoing unnecessary biopsies or laparotomies to remove suspicious masses that were subsequently found to be ectopic splenic tissue.
Case report
The patient was a 60-year-old female with a recent diagnosis of colon adenocarcinoma. She had undergone hemicolectomy and presented for postoperative restaging. The chest/abdomen/pelvis CT scan with IV contrast (Figure 1A, Figure 1B) showed a nodular mass extending from the medial hepatic contour of the right lobe of the liver, adjacent to the adrenal gland. The focus was isointense to the liver, and there were several lesions of similar attenuation in the left upper quadrant, near the expected location of the spleen. The patient had had a remote splenectomy. Although these imaging findings would be compatible with splenosis, ectopic splenic tissue does not have a specific CT appearance (1). Therefore, metastatic etiology for the perihepatic mass could not be excluded based on the CT alone (2, 3).
Figure 1A.
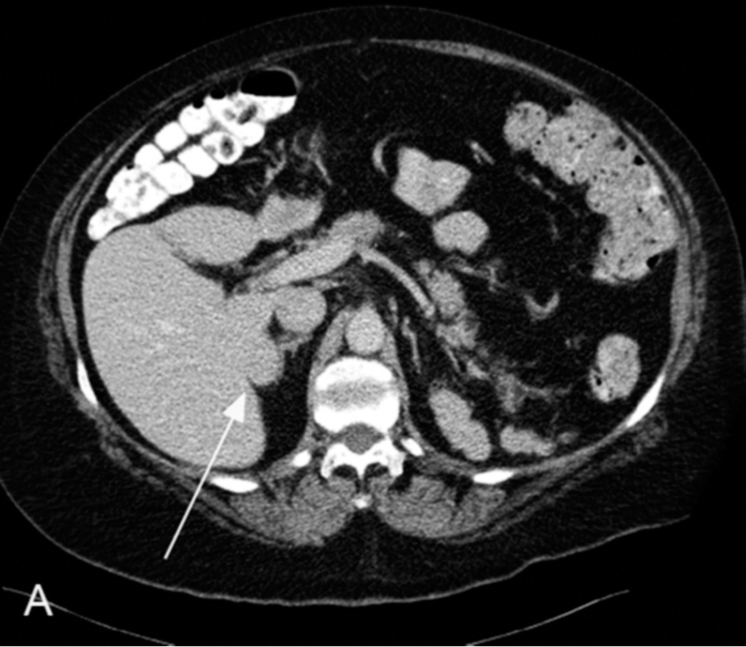
60-year-old female with suspected hepatic metastasis. Axial CT in the soft-tissue window; arrow points to the suspicious mass.
Figure 1B.

60-year-old female with suspected hepatic metastasis. Same image as above in the liver window.
An MRI was performed for further characterization (Figure 2A, Figure 2B, Figure 2C). The images showed the mass to be definitely extrinsic to the liver and the right adrenal gland. The mass had similar imaging characteristics to the known splenic remnants in the left upper quadrant of the abdomen. However, it lacked the homogeneity on T1, and the hypodense rim of fibrous capsule, both typically seen in splenosis (4). The slight hypo- and hyperintensity to liver on T1 and T2 respectively, and heterogeneous enhancement, are imaging features that favor intraperitoneal metastases (6). Additionally, there was a small area of hyperintense T2 signal in the anterior aspect of the lesion (arrow) that mimicked the appearance of viable tumor surrounding a hyperintese area of liquefactive necrosis, commonly seen with metastases (7). The final impression was inconclusive; therefore, spleen imaging with radiolabeled, heat-damaged red blood cells was obtained to characterize the lesion definitively.
Figure 2A.
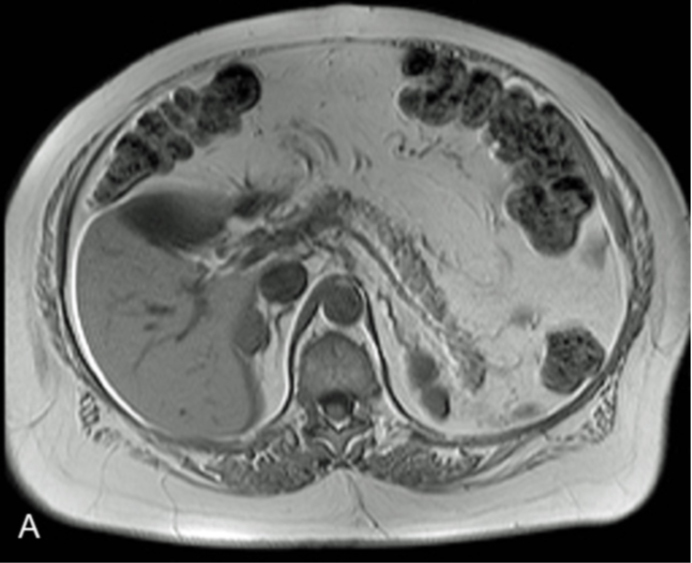
60-year-old female with suspected hepatic metastasis. T1 MRI without contrast.
Figure 2B.
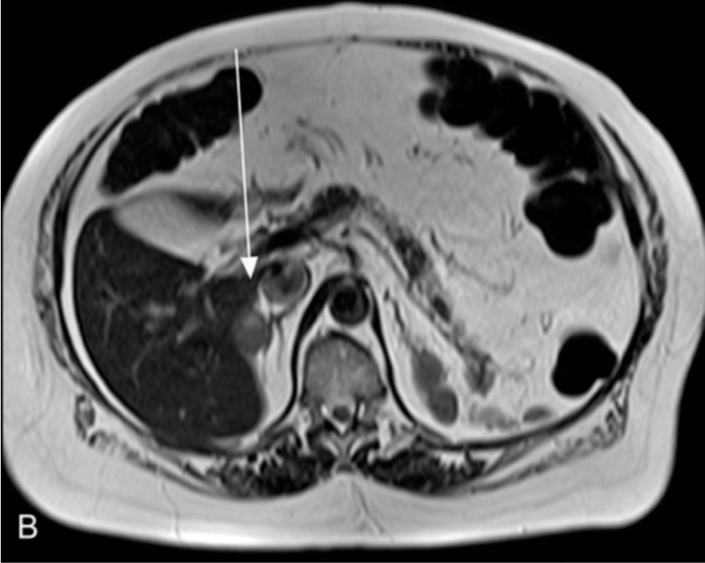
60-year-old female with suspected hepatic metastasis. T2 MRI with arrow pointing to the area of heterogeneity that mimics the appearance of liquefactive necrosis.
Figure 2C.
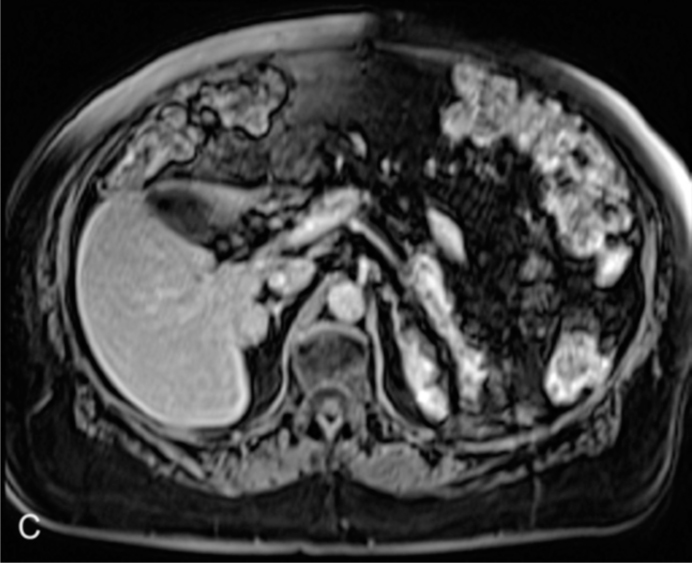
60-year-old female with suspected hepatic metastasis. Gadolinium-enhanced T1 MRI showing some enhancement within the mass.
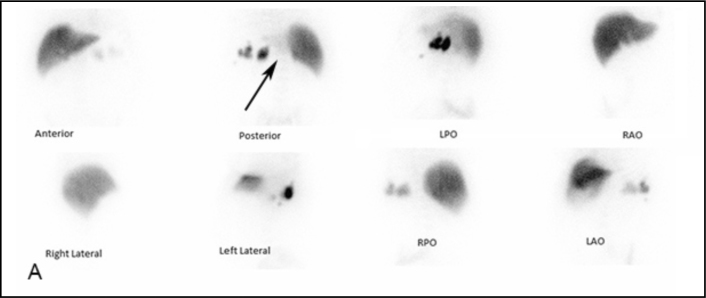
The patient was injected with 10.0 mCi (370 MBq) of heat-denatured, Tc-99m–labeled autologous RBCs. (The tracer is prepared by labeling RBCs removed from the patient with Tc-99m in vitro. Then, the labeled RBCs are damaged by heating them in a water bath at 49° C for 20 minutes.) Fig. 3A shows planar images of the abdomen taken in the anterior, posterior, lateral, and oblique projections. The retained splenic tissue is seen as several foci of radiotracer uptake in the left upper abdomen, and is more intense than the liver. There is normal diffuse hepatic uptake. Since no definite uptake corresponding to the lesion in question was identified on the planar images, SPECT imaging was performed for further evaluation. Fig. 3B shows an axial slice, at approximately the same level as the CT and MRI images shown in Figure 1A, Figure 2A. There is focal increased uptake at the medial border of the right hepatic lobe, corresponding to the location of the lesion in question, identifying it as ectopic splenic tissue (8).
Figure 3A.
60-year-old female with suspected hepatic metastasis. Planar scintigraphic images in multiple projections show intense uptake in the known splenic remnants in the left upper quadrant (arrow), but nothing in definite focus abutting the posterior aspect of the right lobe of the liver.
Figure 3B.
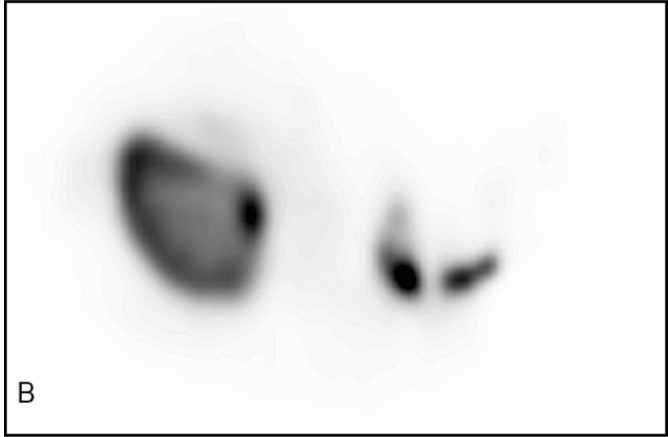
60-year-old female with suspected hepatic metastasis. Axial slice from the SPECT images that is analogous to the CT and MRI images, clearly demonstrating uptake in nodular mass adjacent to the liver.
By identifying the mass in question as a benign splenule, the patient’s cancer was downstaged. She was treated with a shorter course of chemotherapy, and a repeated CT scan performed 6 months postoperatively showed no evidence of recurrent or residual disease.
Discussion
A splenule is a small nodule of splenic tissue found apart from the main body of the spleen. These can form by developmental anomalies or (more commonly) following trauma, and they occur in approximately 10% of the population (9). Splenules are a frequent cause of interpretation errors in diagnostic imaging, as they can be confused with lymphadenopathy or neoplastic growth (10). In our case, the patient underwent a splenectomy during which displaced fragments of splenic tissue underwent autotransplantation onto well-vascularized surfaces in the abdomen (11). This process is known as splenosis.
Since the splenic remnants are functional, we can use that to our advantage in scintigraphy. The splenules sequester the damaged RBCs, including the radiolabeled ones, resulting in intense uptake in any retained tissue. According to the Society of Nuclear Medicine Procedure Guidelines (12), a positive finding is highly specific, while false negatives are almost uniformly due to laboratory error in the preparation of the heat-damaged RBCs.
Given the rarity of hepatic splenosis (13), these lesions are often mistaken for hepatocellular carcinoma or metastases on conventional anatomic imaging (14, 15); this sometimes leads to unnecessary procedures such as exploratory laparotomies and even partial liver resections (16). Because of the appropriate use of scintigraphy in our case, the correct diagnosis was made. As a result, the referring physicians avoided pursuing potential unnecessary invasive therapy, and most importantly, allowed for the correct staging of the colon adenocarcinoma.
Footnotes
Published: February 14, 2013
References
- 1.De Vuysere S, Van Steenbergen W, Aerts R, Van Hauwaert H, Van Beckevoort D, Van Hoe L. Intrahepatic splenosis: imaging features. Abdom Imaging. 2000;25(2):187–189. doi: 10.1007/s002619910042. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Nordlinger B, Rougler P. Liver metastases from colorectal cancer: The turning point. J Clin Oncol. 2002;20(6):1442–1445. doi: 10.1200/JCO.2002.20.6.1442. [PubMed] [DOI] [PubMed] [Google Scholar]
- 3.Des Guetz G, Montravers F, Spatzierer M. Isolated metastatic adrenal involvement with colon cancer and FDG coincidence detection imaging. Clin Nucl Med. 2003;28(3):238. doi: 10.1097/01.RLU.0000053537.01664.BF. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Tsitoridis I, Michaelides M, Sotiriadis C, Arvaniti M. CT and MRI of intrapertoneal splenosis. Diagn Interv Radiol. 2010;16(2):145–149. doi: 10.4261/1305-3825.DIR.1855-08.1. [PubMed] [DOI] [PubMed] [Google Scholar]
- 6.Sica GT, Ji H, Ros PR. CT and MR imaging of hepatic metastases. AJR. 2000;174(3):691–698. doi: 10.2214/ajr.174.3.1740691. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Outwater E, Tomaszewski JE, Daly JM, Kressel HY. Hepatic colorectal metastases: correlation of MR imaging and pathologic appearance. Radiology. 1991;180(2):327–332. doi: 10.1148/radiology.180.2.2068294. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Gunes I, Yilmazlar T, Sarikaya I, Akbunar T, Irgil C. Scintigraphic detection of splenosis: superiority of tomographic selective spleen scintigraphy. Clin Radiol. 1994;49(2):115–117. doi: 10.1016/s0009-9260(05)83452-x. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.Gayer G, Zissin R, Apter S, Atar E, Portnoy O, Itzchak Y. CT findings in congenital anomalies of the spleen. Br J Radiol. 2009;77(884):767–772. doi: 10.1259/bjr.74.884.740767. [PubMed] [DOI] [PubMed] [Google Scholar]
- 10.Abu Hilal M, Harb A, Zeidan B, Steadman B, Primrose JN, Pearce NW. Hepatic Splenosis mimicking HCC in a patient with hepatitis C liver cirrhosis and mildly raised alpha feto protein; the important role of explorative laparoscopy. World J Surg Oncol. 2009;7(1):1. doi: 10.1186/1477-7819-7-1. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Madjar S, Weissberg D. Thoracic splenosis. Thorax. 1994;49(10):1020–1022. doi: 10.1136/thx.49.10.1020. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Royal HD, Brown ML, Drum DE, Nagle CE, Sylvester JM, Ziessman HA. Procedure guideline for hepatic and splenic imaging. Society of Nuclear Medicine. J Nucl Med. 1998;39(6):1114–1116. [PubMed] [PubMed] [Google Scholar]
- 13.D'Angelica M, Fong Y, Blumgart LH. Isolated hepatic splenosis: first reported case. HPB Surgery. 1998;11:39–42. doi: 10.1155/1998/72067. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nakajima T, Fujiwara A, Yamaguchi M. Intrahepatic splenosis with severe iron deposition presenting with atypical magnetic resonance images. Intern Med. 2008;47(8):743–746. doi: 10.2169/internalmedicine.47.0689. [PubMed] [DOI] [PubMed] [Google Scholar]
- 15.Yoshimitsu K, Aibe H, Nobe T. Intrahepatic splenosis mimicking a liver tumor. Abdom Imaging. 1993;18(2):156–158. doi: 10.1007/BF00198054. [PubMed] [DOI] [PubMed] [Google Scholar]
- 16.Kang KC, Cho GS, Chung GA. Intrahepatic splenosis mimicking liver metastasis in a patient with gastric cancer. J Gastric Cancer. 2011;11(1):64–68. doi: 10.5230/jgc.2011.11.1.64. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
Uncited Reference
- 5.Storm BL, Abbitt PL, Allen DA, Ros PR. Splenosis: superparamagnetic iron oxide-enhanced MR imaging. AJR. 1992;159(2):333–335. doi: 10.2214/ajr.159.2.1632350. [PubMed] [DOI] [PubMed] [Google Scholar]