Abstract
Context:
Frequent incidence of early postoperative memory impairment (POMI) after cardiac surgery remains a concern because of associated morbidity, impaired quality of life, and increased health care cost.
Aim:
To assess the effect of preoperative statin therapy on POMI in patients undergoing off-pump coronary artery bypass (OPCAB) surgery.
Setting and Design:
Prospective observational study in a tertiary level hospital.
Methods:
Sixty patients aged 45–65 years undergoing OPCAB surgery were allocated into two groups of 30 each. Group A patients were receiving statin and Group B patients were not receiving statins. All patients underwent memory function assessment preoperatively after admission to hospital and on the 6th postoperative day using postgraduate institute memory scale.
Statistical Analysis:
Appropriate tests were applied with SPSS 20 to compare both groups. The value P < 0.05 was considered statistically significant. Multiple regression analysis was performed with confounding factors to determine the effect on memory impairment.
Results:
Patients in Group A showed significant postoperative deterioration in 6 of the 10 functions and in Group B showed deterioration in 9 of 10 functions tested compared to preoperative scores. Intergroup comparison detected less POMI in Group A compared to Group B and was statistically significant in 8 memory functions. Multiple regression analysis detected statin as an independent factor in preventing memory impairment.
Conclusions:
Preoperative statin therapy attenuates the early POMI in patients undergoing OPCAB. Future long-term studies will define the efficacy of statin on POMI.
Keywords: C-reactive protein, Coronary artery bypass grafting, Memory function, Postoperative cognitive dysfunctions, Statins
INTRODUCTION
Postoperative cognitive dysfunction is the short-term decrease in memory and executive functions of a person. Memory is one of the major components in cognitive function that is always associated with neurocognitive dysfunction. Postoperative memory impairment (POMI) after cardiac surgery is observed in 25–80% of patients in the 1st postoperative week.[1,2] Although POMI tends to improve slowly in the course of time, it persists 10–30% of cases for months to years after surgery.[2] Despite the improvement in cardiology, cardiac surgery, and anesthesia techniques, frequent incidence of POMI remained a concern because of associated morbidity, impaired quality of life and increased health care cost. Inflammation occurs in the brain after off-pump coronary artery bypass grafting (CABG) surgery.[3] Alteration in hippocampal function due to inflammation may adversely affect memory function.[4] The incidence of POMI was previously considered to be lower in off-pump coronary artery bypass (OPCAB) surgery compared to coronary artery bypass with cardiopulmonary bypass (CPB),[5] but recent studies proved the same incidence in both on and off-pump surgery.[6] OPCAB triggers repeated hemodynamic fluctuations, dislodgement of micro-emboli at the time of applying side clamp to the aorta and systemic inflammation due to tissue injury. Statin pretreatment reduces the incidence of stroke in CABG.[7] The study showed three-fold reductions in the rate of cerebrovascular events after carotid endarterectomy in statin pretreated patients.[8,9] Preoperative use of statin is associated with reduced early delirium rates after cardiac surgery with CPB.[10] Atorvastatin reduces systemic inflammatory response after coronary artery bypass surgery.[11] Some occasions in patients with a normal level of lipids, history of myalgia, and diabetes mellitus statins are withdrawn from routine treatment. We selected cohort of patients as control group.
With all the background knowledge, it was postulated that preoperative statin can reduce POMI in patients undergoing OPCAB surgery. The literature search did not find any study regarding the effects of preoperative statin on memory impairment in patients undergoing OPCAB surgery. The aim of this study was to assess the effects of statin on memory function in patients undergoing OPCAB surgery.
METHODS
This study was conducted after obtaining approval of Hospital Ethics Committee and informed written consent from the patients. The study was designed in a prospective observational pattern. Sixty patients aged between 45 and 65 years undergoing elective OPCAB surgery were enrolled in the study over a period of 2 years. Patients were allotted nonrandomly into two groups until completion of 30 patients in each. Group A patients were receiving atorvastatin 10 mg or 20 mg in the preoperative period for at least 1 month, whereas Group B patients were not receiving statin before admission to hospital because of some reason as decided by the primary physician.
Exclusion criteria
Patients with hepatic impairment (aspartate aminotransferase or alanine aminotransferase > twice the normal limit), renal disease (creatinine >2 mg/dl), preexisting cerebrovascular disease, psychiatric illness, psychotropic drug abuse, alcoholism, left ventricular ejection fraction <30%, critical coronary anatomy, severe left main stenosis, unstable angina, atheromatous ascending aorta, major hemodynamic fluctuations, and redo or emergency CABG surgery. For difficult assessment of memory tests, patients with <7th classes schooling or not able to read and write down the questionnaires were excluded from the study.
Patients in both the groups were managed perioperatively by same anesthesiologist and surgeon. Patients were premedicated with morphine 0.1 mg/kg and promethazine 0.5 mg/kg intramuscularly, 30 min before shifting to the operation room. Anesthesia was induced with intravenous thiopentone 3–5 mg/kg, fentanyl 2–3 μg/kg, midazolam 20 μg/kg and trachea was intubated after rocuronium 0.6 mg/kg. Anesthesia was maintained with O2 in air (1:1), sevoflurane and supplemental doses of intravenous fentanyl, midazolam, and vecuronium. Monitoring such as electrocardiogram, arterial blood pressure, pulse oximetry, central venous pressure, end-tidal CO2, transesophageal echocardiography (TEE) and near infrared spectroscopy were used throughout the surgery period. TEE was used to check for any ascending aorta atheroma. Systemic anticoagulation was achieved with intravenous heparin 200 IU/kg with a target ACT >400 s. The mean arterial pressures (MAP) were maintained at 70–80 mmHg. If MAP <50 mmHg, diluted phenylephrine 50–100 μg was given. For MAP above 80 mmHg, boluses of fentanyl, midazolam, and vecuronium were given. If these failed to lower pressures, nitroglycerine infusion at 0.5–1 μg/kg/min was started. The blood glucose levels were maintained below 180 mg/dl. None of the patients in both groups received any steroid, antifibrinolytic, and nonsteroidal anti-inflammatory drugs in the perioperative period. The core temperature was monitored in the nasopharynx. Warm intravenous fluids, warm fluid in the mister blower and blanket of temperature controlling machine (Sarns 3M Health Care, Ann Arbor) were used to maintain intraoperative normothermia (36–37°C). The ambient temperature was also kept at 21°C.
Off-pump CABG was carried out through a median sternotomy. Stabilization of target arteries was accomplished with Medtronic Octopus system (Medtronic, Minneapolis, MN, USA). Left internal mammary artery graft was used in all patients. Proximal venous graft anastomosis was performed after the distal anastomosis using a single side clamp. Systemic anticoagulation was reversed by protamine sulfate 1 mg/kg. Depending on hemodynamic parameters intravenous infusions of vasopressors and/or vasodilators were used. Postsurgery patients were ventilated mechanically in the Intensive Care Unit (ICU). Tracheal extubation was decided by the ICU physician who was not involved in the administration of anesthesia in the operating room or involved in the study.
High sensitivity C-reactive protein (CRP) concentration was assayed by immunonephelometry technique from the blood samples taken before anesthetic induction and 24 h thereafter. Serum creatinine was measured preoperatively and at 24 h after surgery. Postoperatively atorvastatin was continued from the 1st day in Group A and after the 6th day in Group B. Aspirin, nitrates, and calcium channel blockers were continued in both groups in the postoperative period to deliver the benefits of graft patency and atrial fibrillation.
The memory functions were assessed on the day before surgery and on the 6th postoperative day using the postgraduate institute (PGI) memory scale (PGI of Medical Education and Research, Chandigarh, India).[12,13] It includes a battery of different cognitive domains such as remote memory, recent memory, mental balance, attention and concentration, delayed recall, immediate recall, retention of similar, dissimilar pair, visual retention, and recognition. The independent investigator was a clinical psychologist performing these tests was blinded to both the groups. Duration of mechanical ventilation, ICU and hospital stay was noted.
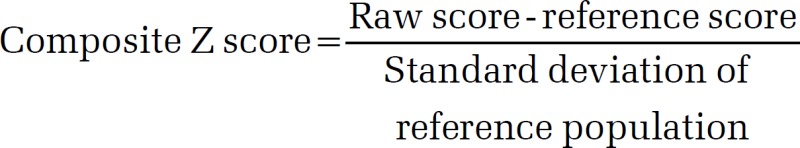
The PGI memory scale is one of the tests of PGI-battery of brain dysfunction.[12] The socioeconomic and educational background of Indian population is different from the western world, so PGI memory scale was used in the patients for neurocognitive assessment. This consists of a questionnaire in Hindi and English, which is to be read and answered. The “raw scores” are calculated based on the answers given by the patient. The nomograms for different age groups and educational levels derived for different age groups and educational levels derived from an Indian population are available along with the questionnaire. These nomograms give the mean reference scores along with the standard deviation for individuals of different age groups and educational levels. From the raw score, the reference score obtained from the nomogram is subtracted and the difference divided by the standard deviation of the population of the reference value’ to get the “composite score or Z score.”
Statistical analysis
The results were analyzed using statistical package for social science (SPSS) version 20 software (IBM Corporation, USA). The paired t-test and Student's t-test were used to compare normally distributed data. The Mann–Whitney U-test and Wilcoxon signed rank test were used to compare nonnormally distributed data. The categorical measures were compared using a Chi-square test; P < 0.05 was used to express statistical significance. Multiple regression analysis was performed with confounding factors such as age, sex, education, diabetes, chronic obstructive pulmonary disease (COPD), EURO score, number of grafts, duration of surgery, and preoperative CRP level to determine the effect on memory impairment.
RESULTS
Eighty patients were eligible for the study. Fourteen patients were excluded as per the exclusion criteria. Intraoperative complications leading to conversion to CPB supported CABG in 4 patients. Two patients were detected to have atheromatous ascending aorta from TEE examination. The remaining 60 patients completed the designed study procedure. The demographic data of patients are listed in Table 1. Both groups were comparable with regard to age, sex, education, number of patients with diabetes and COPD, number of grafts, and duration of surgery.
Table 1.
Demographic data
| Variables | Group A (n=30) | Group B (n=30) | P |
|---|---|---|---|
| Age (year) | 56.2±5.8 | 57.3±5.1 | 0.44 |
| Sex (male:female) | 29:1 | 28:2 | 1.00 |
| Education (year) | 12.5±2.2 | 12±2 | 0.8 |
| Diabetes (number of patients) | 9 | 9 | - |
| COPD (number of patients) | 3 | 3 | - |
| Euro score (median (IQR)) | 3 (1.5-5) | 3 (1.75-4) | - |
| Number of grafts | 3.7±0.7 | 3.5±0.7 | 0.87 |
| Duration of surgery (h) | 2.8±0.61 | 2.7±0.46 | 0.77 |
COPD: Chronic obstructive pulmonary disease, IQR: Interquartile range
CRPs levels were significantly higher in Group B compared to Group A in the postoperative period (93.16 ± 22 vs. 67.64 ± 19.29, P = 0.001) [Table 2]. Duration of postoperative mechanical ventilation was significantly prolonged in Group B (9.7 ± 0.65 vs. 5.64 ± 0.9, P = 0.001) [Table 2]. However, the duration of ICU stay and hospital stay were similar between the groups (P = 0.69, P = 0.17). There was no postoperative mortality.
Table 2.
Outcome parameters
| Variables | Group A (n=30) | Group B (n=30) | P |
|---|---|---|---|
| CRP (mg/L) | |||
| Preoperation | 9.5±15 | 11.24±9.7 | 0.59 |
| Postoperation (after 24 h) | 67.64±19.29 | 93.16±22 | 0.001 |
| Mechanical ventilation duration (h) | 5.64±0.9 | 9.7±0.65 | 0.001 |
| ICU stay (day) | 1.1±0.30 | 1.13±0.34 | 0.69 |
| Hospital stay (day) | 6.1±1.47 | 6.6±1.35 | 0.17 |
| Mortality | 0 | 0 | - |
ICU: Intensive Care Unit, CRP: C-reactive protein
The memory functions tested along with the preoperative and postoperative scores are summarized in Table 3. The patients in Group A showed significant postoperative deterioration in 6 of the 10 functions [Table 3], whereas the patients in Group B showed significant postoperative deterioration in 9 out of 10 functions when compared to the preoperative scores [Table 3]. When intergroup comparison was done, the preoperative scores were similar between the groups [Table 4]. The postoperative memory dysfunction was more in Group B patients compared to statin-treated group (Group A) and was statistically significant (P < 0.001) in 8 memory functions out of 10 tests [Table 4]. Delayed and immediate recall memory were less in postoperative period between Group A and B but not statistically significant (P = 0.14, 0.22) [Table 4].
Table 3.
Neurocognitive tests (PGI memory scale): Intragroup comparison
| Functions tested | Group A | Group B | ||||
|---|---|---|---|---|---|---|
| Preoperative score | Postoperative score | P | Preoperative score | Postoperative score | P | |
| Remote memory | 0.24±0.06 | 0.21±0.06 | 0.07 | 0.22±0.08 | 0.16±0.04 | 0.006 |
| Recent memory | 0.28±0.05 | 0.24±0.05 | 0.03 | 0.27±0.06 | 0.19±0.05 | 0.001 |
| Mental balance | 0.68 (0.35, 0.08)* | −0.27 (−0.74, −0.05)* | 0.001 | 0.67 (0.42, 0.85)* | −0.68 (−0.92, −0.34)* | 0.001 |
| Attention and concentration | −0.11 (−0.34, 0.11)* | −0.11 (−0.23, 0.15)* | 0.78 | −0.09 (−0.25, 0.14)* | −0.24 (−0.45, 0.19)* | 0.001 |
| Delayed recall | 1.54±0.59 | 1.32±0.13 | 0.075 | 1.4±0.61 | 1.28±0.05 | 0.31 |
| Immediate recall | 0.35±0.05 | 0.28±0.04 | 0.001 | 0.34±0.05 | 0.27±0.05 | 0.001 |
| Retention of similar pairs | 0.81±0.07 | 0.77±0.05 | 0.028 | 0.82±0.06 | 0.69±0.07 | 0.001 |
| Retention of dissimilar pair | 1.45±0.39 | 1.1±0.09 | 0.001 | 1.33±0.31 | 0.56±0.05 | 0.001 |
| Visual retention | −0.356±0.04 | −0.42±0.06 | 0.001 | −0.35±0.04 | −0.87±0.18 | 0.001 |
| Recognition | 0.45±0.06 | 0.42±0.05 | 0.084 | 0.45±0.07 | 0.36±0.05 | 0.001 |
*Nonparametric data expressed as median (minimum, maximum value). A Wilcoxon signed-rank test used for comparison of continuous variables; Lower score indicate greater deterioration in neurocognitive function. PGI: Postgraduate institute
Table 4.
Neurocognitive tests (PGI memory scale): Intergroup comparison
| Functions tested | Preoperative score | Postoperative score | ||||
|---|---|---|---|---|---|---|
| Group A | Group B | P | Group A | Group B | P | |
| Remote memory | 0.24±0.06 | 0.22±0.08 | 0.45 | 0.21±0.06 | 0.16±0.04 | 0.001 |
| Recent memory | 0.28±0.05 | 0.27±0.06 | 0.51 | 0.24±0.05 | 0.19±0.05 | 0.001 |
| Mental balance | 0.68 (0.35, 0.08)* | 0.67 (0.42, 0.85)* | 0.66 | −0.27 (0.74, −0.05)* | −0.68 (−0.92, −0.34)* | 0.001 |
| Attention and concentration | −0.11 (−0.34, 0.11)* | −0.09 (−0.25, 0.14)* | 0.60 | −0.11 (−0.23, 0.15)* | −0.24 (−0.45, 0.19)* | 0.001 |
| Delayed recall | 1.54±0.59 | 1.4±0.61 | 0.40 | 1.32±0.13 | 1.28±0.05 | 0.14 |
| Immediate recall | 0.35±0.05 | 0.34±0.05 | 0.27 | 0.28±0.04 | 0.27±0.05 | 0.22 |
| Retention of similar pairs | 0.81±0.07 | 0.82±0.06 | 0.68 | 0.77±0.05 | 0.69±0.07 | 0.001 |
| Retention of dissimilar pair | 1.45±0.39 | 1.33±0.31 | 0.20 | 1.1±0.09 | 0.56±0.05 | 0.001 |
| Visual retention | −0.356±0.04 | −0.35±0.04 | 0.41 | −0.42±0.06 | −0.87±0.18 | 0.001 |
| Recognition | 0.45±0.06 | 0.45±0.07 | 0.87 | 0.42±0.05 | 0.36±0.05 | 0.001 |
*Continuous data expressed as median (minimum, maximum value). A Mann-Whitney U-test used for comparison of continuous variables; Lower scores indicate greater deterioration in neurocognitive function. PGI: Postgraduate institute
After multiple regression analysis considering all demographic and other baseline studied confounding factors, we found that for each outcome the intervention with statin came out to be an independent factor for prevention of impairment in 8 mental functions of PGI memory scale (P < 0.05) [Table 5]. None of the demographic and baseline parameters had come out to be a statistically significant factor for reducing memory impairment (P > 0.05).
Table 5.
Effect intervention after adjusting confounding factors between the groups
| Memory function | Adjusted mean±SE | P* | |
|---|---|---|---|
| Group A | Group B | ||
| Remote memory | 0.21±0.05 | 0.16±0.05 | 0.003 |
| Recent memory | 0.24±0.05 | 0.19±0.05 | 0.000 |
| Mental balance | −0.34±0.16 | −0.64±0.16 | 0.000 |
| Attention and concentration | −0.06±0.12 | −0.24±0.12 | 0.000 |
| Delayed recall | 1.33±0.1 | 1.28±0.1 | 0.105 |
| Immediate recall | 0.28±0.05 | 0.27±0.05 | 0.404 |
| Retention of similar pairs | 0.77±0.06 | 0.69±0.06 | 0.000 |
| Retention of dissimilar pair | 1.09±0.07 | 0.56±0.07 | 0.000 |
| Visual retention | −0.42±0.14 | −0.88±0.14 | 0.000 |
| Recognition | 0.43±0.05 | 0.36±0.5 | 0.000 |
*Adjusted value after applying ANCOVA. ANCOVA: Analysis of covariance, SE: Standard error
DISCUSSION
Cognition is the mental activity in regard to the attention of working memory, comprehending and producing language, calculating, reasoning, problem-solving, and decision making. Cognition is typically assumed to be information processing in a participant's or operator's mind or brain.[14] Memory functions are essential for the daily activity of a person. Studies have detected that cardiac surgery performed with and without CPB reduce memory power of patients after surgery.[6] The POMI is associated with poor quality of life, delayed memory, and defective skillful functions after cardiac surgery.
This study detected impaired memory function in patients of both the groups when compared between presurgery and postsurgery score. This is supported by Grogan et al., who found a high incidence of POMI after CABG and they suggested for the need of preventive measures.[1] The memory functions such as recent memory, mental balance, immediate recall, retention of dissimilar pair, and visual retention were impaired significantly in statin-treated patients. However, all 10 memory functions except delayed recall showed significant impairment in patients not receiving statin. Hence, preoperative statin therapy was able to attenuate the memory impairment in OPCAB surgery patients. This might be due to the anti-inflammatory action of statin.[10,11] Katznelson et al. proved inflammation after cardiac surgery as one of the major cause of cognitive dysfunction.[10] Conflicting reports detected that statins use are associated with memory loss.[15] However, Strom et al. in a retrospective cohort study compared 482 543 statin users with 26 484 users of nonstatin and found that both statin and nonstatin users had acute memory loss.[16] They commented that the memory loss might be a detection bias rather than association with statin. Our study corroborates with the above study that both groups had POMI. However, statin group had less impairment compared to nonstatin. In our study, delayed recall was spared in both the groups. The exact mechanism was not known. The probable cause might be, the patients in both groups were >55 years age. In these subsets, the recent memories got impaired very easily then the delayed or old memory. As literature reported that the older patients have impaired recent memory and relatively less impairment in old memory.[17] Hence, delayed recall was less impaired, and recognition, as well as immediate recall, were significantly impaired in our patients.
The inter-group comparison in this study detected the PGI memory score in 10 tests in the preoperative period was similar. However, in the postoperative period, the statin-treated group showed less impairment of memory function in all parameters except delayed and immediate recall compared to control group patients. The multiple regression analysis of the confounding parameters also detected the significant impairment of memory in the nonstatin group compared to statin users. The independent factor that prevented POMI was statin. This might be because of the anti-inflammatory effect of statin as proved by Chello et al.[11] The immediate and delayed recall scores had a drop in value from preoperative value [Tables 3 and 4], but comparing the postoperative values did not find any significance difference. The reduction in delayed recall was less in postoperative period than immediate recall. This was because of the reason mentioned previously.[17]
Our study detected the low rise of CRP serum level and lesser duration of postoperative mechanical ventilation in patients receiving statin. Kálmán et al., showed elevated levels of inflammatory biomarkers in the cerebrospinal fluid even after OPCAB graft surgery.[18] They conclude that inflammation was a predictor of cognitive decline and affects the memory function. Heringa et al. detected that inflammation also affects the brain tissue resulting cerebral vascular endothelial dysfunction.[19] This contributes to reduced information processing speed and executive functioning in and reduction in memory. It has been detected in a study by Bettcher et al. that high levels of CRP displayed smaller left medial temporal lobe volumes relating to memory dysfunction.[20] Dantzer and Kelley showed irrespective of the underlying cause, these inflammatory changes may adversely affect learning, memory and other cognitive domains by altering hippocampal function.[21] Saleem et al. has demonstrated an association between CRP concentration during middle age and subsequent risk of dementia.[22] Chello et al. showed atorvastatin reduces systemic inflammatory response after coronary bypass surgery.[11] The significant reduction in CRP level in statin-treated group in this study corroborates with all the above studies and lower inflammation might explain less POMI in statin-treated patients.
In a meta-analysis, Liakopoulos et al. showed stroke rate was lower in patients who received statin therapy before cardiac surgery compared with controls.[23] Statin therapies were associated with a 26% reduction in the odds for stroke.[23] McGirt et al. showed statins reduces the risk of perioperative stroke and mortality after carotid endarterectomy.[7] Kennedy et al. also demonstrated statins are associated with better outcomes after carotid endarterectomy in symptomatic patients.[9] Katznelson et al. showed preoperative administration of statins is associated with reduced risk of postoperative delirium after cardiac surgery with CPB.[10] The probable reason for the reduction in stroke, delirium, and perioperative stroke was the pleotropic effect of statins such as antithrombotic, antioxidant, plaque stabilization, inhibiting the thrombogenic response, and improved vascular endothelial functions.[24] The same reasons would be the explanation for attenuation of POMI in patients receiving statin in preoperative period in our study.
Mathew et al. showed that the preoperative statin therapy did not decrease the rate of cognitive decline after CABG surgery.[25] However, Mathew et al. evaluated cognitive function 6 weeks after surgery and 46% of the patients receiving preoperative statins were withdrawn from statin therapy postoperatively due to lack of standardized protocol.
The authors found the duration of postoperative mechanical ventilation was significantly prolonged in nonstatin group, but the duration of ICU stay and hospital stay were similar between the groups. The prolonged mechanical ventilation in Group B might be due to the inflammatory mediator related pulmonary dysfunction.
Limitations
This study was a short-term observational study with small number of patients. The patients with high risk of neurological insults such as a prior cerebrovascular disease, cardiac dysfunction, and recent myocardial infarction were not included in this study. The use of epiaortic scanning would have been better than TEE to detect atheroma and select the patients. The patients in Group B were deprived of benefits of statin until the postoperative 6th day to avoid the impact on postoperative memory testing. Group A patients received statin from the postoperative day 1. Hence small anti-inflammatory effect might have been contributed on the postoperative memory function tests.
CONCLUSION
The study revealed that preoperative statin therapy attenuates POMIs based on PGI memory scale in patients undergoing OPCAB surgery. Further large-scale multicenter randomized controlled trials with long-term follow-up study may be required to derive the efficacy of preoperative statin on memory impairment in these patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors thank Mr. Ashish Upadhya for performing the statistical analysis.
REFERENCES
- 1.Grogan K, Stearns J, Hogue CW. Brain protection in cardiac surgery. Anesthesiol Clin. 2008;26:521–38. doi: 10.1016/j.anclin.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Royter V, M Bornstein N, Russell D. Coronary artery bypass grafting (CABG) and cognitive decline: A review. J Neurol Sci. 2005;229-230:65–7. doi: 10.1016/j.jns.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 3.Raja SG, Berg GA. Impact of off-pump coronary artery bypass surgery on systemic inflammation: Current best available evidence. J Card Surg. 2007;22:445–55. doi: 10.1111/j.1540-8191.2007.00447.x. [DOI] [PubMed] [Google Scholar]
- 4.Zheng L, Mack WJ, Chui HC, Heflin L, Mungas D, Reed B, et al. Coronary artery disease is associated with cognitive decline independent of changes on magnetic resonance imaging in cognitively normal elderly adults. J Am Geriatr Soc. 2012;60:499–504. doi: 10.1111/j.1532-5415.2011.03839.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stroobant N, Van Nooten G, Van Belleghem Y, Vingerhoets G. Relation between neurocognitive impairment, embolic load, and cerebrovascular reactivity following on- and off-pump coronary artery bypass grafting. Chest. 2005;127:1967–76. doi: 10.1378/chest.127.6.1967. [DOI] [PubMed] [Google Scholar]
- 6.Farhoudi M, Mehrvar K, Afrasiabi A, Parvizi R, Khalili AA, Nasiri B, et al. Neurocognitive impairment after off-pump and on-pump coronary artery bypass graft surgery – An Iranian experience. Neuropsychiatr Dis Treat. 2010;6:775–8. doi: 10.2147/NDT.S14348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aboyans V, Labrousse L, Lacroix P, Guilloux J, Sekkal S, Le Guyader A, et al. Predictive factors of stroke in patients undergoing coronary bypass grafting: Statins are protective. Eur J Cardiothorac Surg. 2006;30:300–4. doi: 10.1016/j.ejcts.2006.03.066. [DOI] [PubMed] [Google Scholar]
- 8.McGirt MJ, Perler BA, Brooke BS, Woodworth GF, Coon A, Jain S, et al. 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors reduce the risk of perioperative stroke and mortality after carotid endarterectomy. J Vasc Surg. 2005;42:829–36. doi: 10.1016/j.jvs.2005.08.039. [DOI] [PubMed] [Google Scholar]
- 9.Kennedy J, Quan H, Buchan AM, Ghali WA, Feasby TE. Statins are associated with better outcomes after carotid endarterectomy in symptomatic patients. Stroke. 2005;36:2072–6. doi: 10.1161/01.STR.0000183623.28144.32. [DOI] [PubMed] [Google Scholar]
- 10.Katznelson R, Djaiani GN, Borger MA, Friedman Z, Abbey SE, Fedorko L, et al. Preoperative use of statins is associated with reduced early delirium rates after cardiac surgery. Anesthesiology. 2009;110:67–73. doi: 10.1097/ALN.0b013e318190b4d9. [DOI] [PubMed] [Google Scholar]
- 11.Chello M, Patti G, Candura D, Mastrobuoni S, Di Sciascio G, Agrò F, et al. Effects of atorvastatin on systemic inflammatory response after coronary bypass surgery. Crit Care Med. 2006;34:660–7. doi: 10.1097/01.CCM.0000201407.89977.EA. [DOI] [PubMed] [Google Scholar]
- 12.Nehra A, Chopra S. Beating the odds: Intact neuropsychological functioning despite TLE. Ann Neurosci. 2014;21:155–9. doi: 10.5214/ans.0972.7531.210410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kohli A, Kaur M, Mohanty M, Malhotra S. Neuropsychological function in specific learning disorders - Reading, writing and mixed groups. J Indian Assoc Child Adolesc Ment Health. 2006;2:112–5. [Google Scholar]
- 14.Blomberg O. Conceptions of cognition for cognitive engineering. Int J Aviat Psychol. 2011;21:85–104. [Google Scholar]
- 15.Evans MA, Golomb BA. Statin-associated adverse cognitive effects: Survey results from 171 patients. Pharmacotherapy. 2009;29:800–11. doi: 10.1592/phco.29.7.800. [DOI] [PubMed] [Google Scholar]
- 16.Strom BL, Schinnar R, Karlawish J, Hennessy S, Teal V, Bilker WB. Statin therapy and risk of acute memory impairment. JAMA Intern Med. 2015;175:1399–405. doi: 10.1001/jamainternmed.2015.2092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cameron KA, Haarmann HJ, Grafman J, Ruchkin DS. Long-term memory is the representational basis for semantic verbal short-term memory. Psychophysiology. 2005;42:643–53. doi: 10.1111/j.1469-8986.2005.00357.x. [DOI] [PubMed] [Google Scholar]
- 18.Kálmán J, Juhász A, Bogáts G, Babik B, Rimanóczy A, Janka Z, et al. Elevated levels of inflammatory biomarkers in the cerebrospinal fluid after coronary artery bypass surgery are predictors of cognitive decline. Neurochem Int. 2006;48:177–80. doi: 10.1016/j.neuint.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 19.Heringa SM, van den Berg E, Reijmer YD, Nijpels G, Stehouwer CD, Schalkwijk CG, et al. Markers of low-grade inflammation and endothelial dysfunction are related to reduced information processing speed and executive functioning in an older population – The Hoorn study. Psychoneuroendocrinology. 2014;40:108–18. doi: 10.1016/j.psyneuen.2013.11.011. [DOI] [PubMed] [Google Scholar]
- 20.Bettcher BM, Wilheim R, Rigby T, Green R, Miller JW, Racine CA, et al. C-reactive protein is related to memory and medial temporal brain volume in older adults. Brain Behav Immun. 2012;26:103–8. doi: 10.1016/j.bbi.2011.07.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dantzer R, Kelley KW. Twenty years of research on cytokine-induced sickness behavior. Brain Behav Immun. 2007;21:153–60. doi: 10.1016/j.bbi.2006.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saleem M, Herrmann N, Swardfager W, Eisen R, Lanctôt KL. Inflammatory markers in mild cognitive impairment: A meta-analysis. J Alzheimers Dis. 2015;47:669–79. doi: 10.3233/JAD-150042. [DOI] [PubMed] [Google Scholar]
- 23.Liakopoulos OJ, Choi YH, Haldenwang PL, Strauch J, Wittwer T, Dörge H, et al. Impact of preoperative statin therapy on adverse postoperative outcomes in patients undergoing cardiac surgery: A meta-analysis of over 30,000 patients. Eur Heart J. 2008;29:1548–59. doi: 10.1093/eurheartj/ehn198. [DOI] [PubMed] [Google Scholar]
- 24.Liao JK, Laufs U. Pleiotropic effects of statins. Annu Rev Pharmacol Toxicol. 2005;45:89–118. doi: 10.1146/annurev.pharmtox.45.120403.095748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mathew JP, Grocott HP, McCurdy JR, Ti LK, Davis RD, Laskowitz DT, et al. Preoperative statin therapy does not reduce cognitive dysfunction after cardiopulmonary bypass. J Cardiothorac Vasc Anesth. 2005;19:294–9. doi: 10.1053/j.jvca.2005.03.004. [DOI] [PubMed] [Google Scholar]


