Abstract
Background:
Vaccine injections are the most common painful needle procedure experienced throughout the lifespan. Many strategies are available to mitigate this pain; however, they are uncommonly utilized, leading to unnecessary pain and suffering. Some individuals develop a high level of fear and subsequent needle procedures are associated with significant distress.
Objective:
The present work is part of an update and expansion of a 2009 knowledge synthesis to include the management of vaccine-related pain across the lifespan and the treatment of individuals with high levels of needle fear. This article will provide a conceptual foundation for understanding: (a) painful procedures and their role in the development and maintenance of high levels of fear; (b) treatment strategies for preventing or reducing the experience of pain and the development of fear; and (c) interventions for mitigating high levels of fear once they are established.
Results:
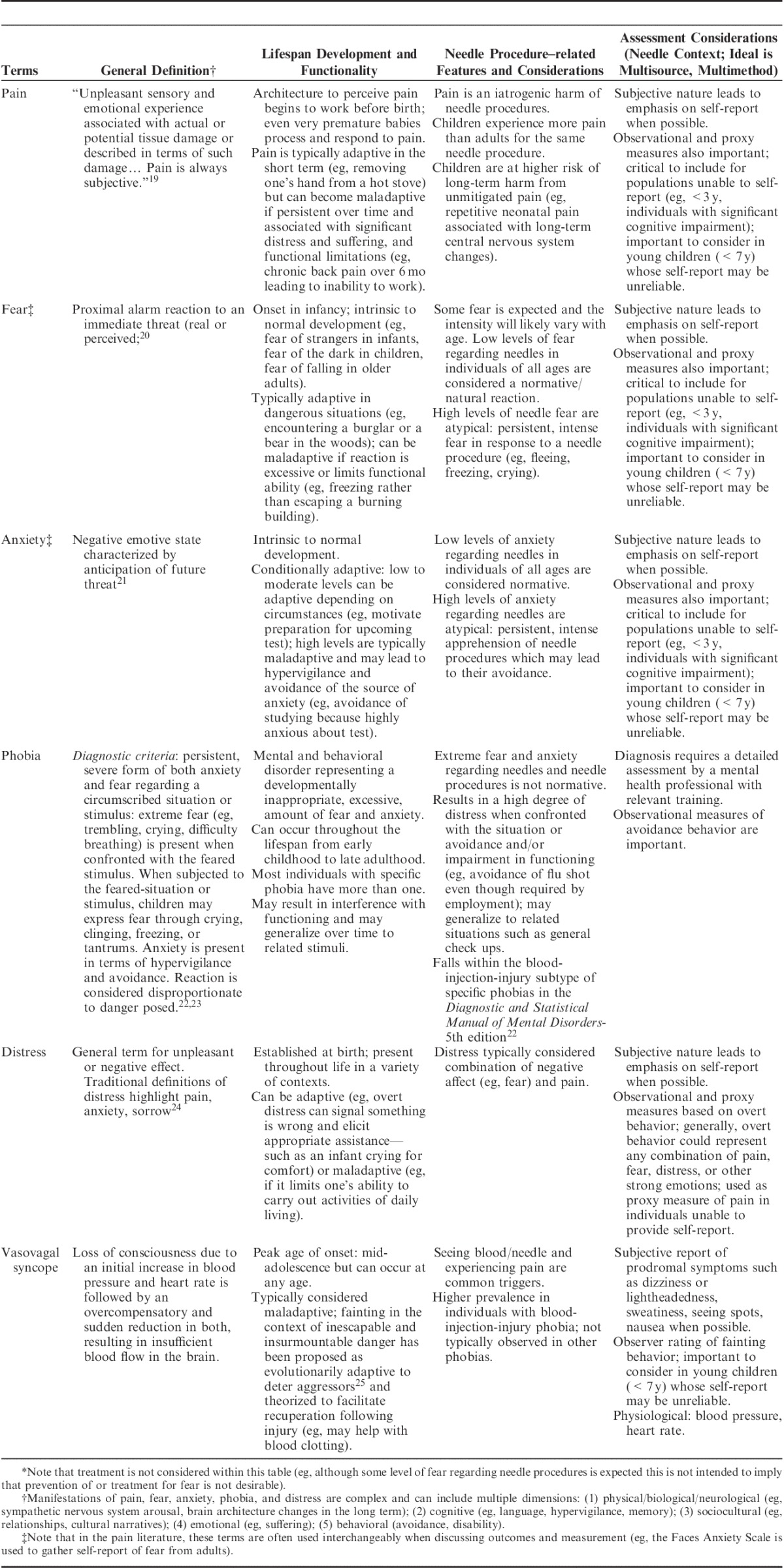
First, the general definitions, lifespan development and functionality, needle procedure-related considerations, and assessment of the following constructs are provided: pain, fear, anxiety, phobia, distress, and vasovagal syncope. Second, the importance of unmitigated pain from needle procedures is highlighted from a developmental perspective. Third, the prevalence, course, etiology, and consequences of high levels of needle fear are described. Finally, the management of needle-related pain and fear are outlined to provide an introduction to the series of systematic reviews in this issue.
Discussion:
Through the body of work in this supplement, the authors aim to provide guidance in how to treat vaccination-related pain and its sequelae, including high levels of needle fear.
Key Words: needle, vaccination, pain, fear, phobia
Vaccinations are responsible for promoting human health by reducing morbidity and mortality from infectious diseases.1 However, the usual method of their administration, which involves needle puncture, is often painful. Vaccinations are the most common painful needle procedure worldwide, with an estimated 12 billion injections given per year.2
Despite the availability of evidence-based strategies for mitigating pain during vaccination, there is a lack of consistent implementation of these interventions; consequently, the majority of individuals receiving vaccination experience pain.3,4 Recently, increasing attention has been paid to pain as an adverse event of vaccination5,6 and, in 2010, the Help ELiminate Pain in Kids team (HELPinKIDS) published the first clinical practice guideline for pain mitigation during vaccination in childhood.7 The present work is part of a series of articles outlining an update and expansion of the original knowledge synthesis8–10 for the management of vaccine-related pain in individuals across the lifespan (ie, the 5Ps of pain management: pharmacological, physical, procedural, psychological, and process) as well as the treatment of individuals with high levels of needle fear or a phobia of needles through exposure-based psychological and physical intervention strategies (Fig. 1).11–17 As the presence of high levels of needle fear interferes with the implementation and success of traditional pain management strategies at the time of vaccination, individuals with a high degree of needle fear must be treated before they can fully benefit from the 5 Ps approach. Together, the evidence base from this series informed the development of a set of new (2015) clinical practice guidelines encompassing the management of vaccination pain18 and high levels of needle fear (McMurtry CM, Taddio A, Noel M, et al., unpublished data, 2015) across the lifespan. The expanded scope of the project led to a change in the team name to HELPinKids&Adults.
FIGURE 1.
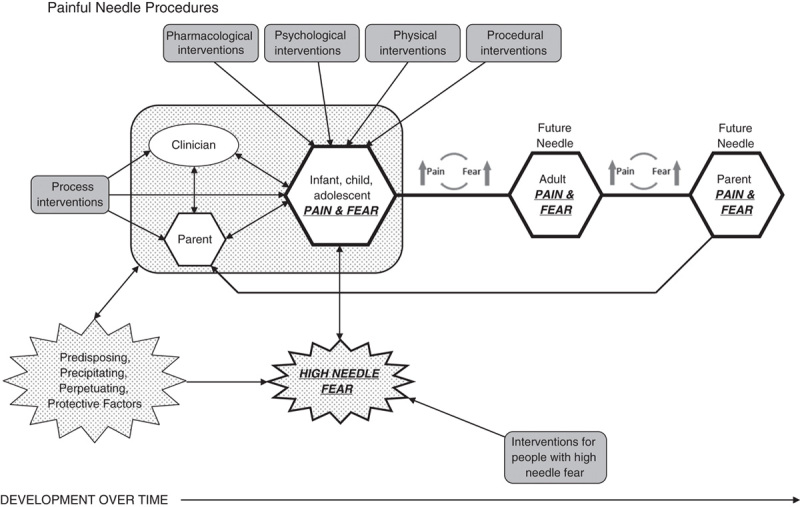
Needle procedures (eg, vaccine injections) across the lifespan. Predisposing, precipitating, perpetuating, and protective factors contribute to the entire needle context (shown in the patterned box) as they influence the clinician, parent, and child (eg, behaviors, experience). The critical role of a high degree of needle fear is highlighted. Unmitigated pain during these procedures may increase fear which in turn can exacerbate future pain in an escalating relationship. Thus, the consequences of unmitigated pain and fear during a given needle procedure extend beyond that particular procedure. Interventions in the systematic reviews in this series of articles are shown in gray-filled boxes; of note, the interventions for individuals with a high degree of needle fear must be implemented before the other interventions more proximal to the procedural context itself (ie, process, pharmacological, psychological, physical, procedural).
The objective of the present article is to lay the conceptual groundwork for understanding: (1) painful procedures and their role in the development and maintenance of high levels of fear; (2) treatment strategies for preventing or reducing the experience of pain and the development of fear; and (3) interventions for mitigating high levels of fear once they are established. Unlike previous reviews on this topic, this paper focuses on the iatrogenic effects of pain beyond the immediate event; that is, we examine the sequelae of pain after the needle procedure, in particular, the development of high levels of needle fear. This is accomplished through uniting typically disparate areas of research (ie, pain management proximal to needle procedures and the anxiety literature), which requires conceptual clarity. Table 1 delineates important terminology and concepts related to needle fear and pain. We will also introduce treatment strategies to mitigate pain at the time of needle procedures to reduce acute pain and suffering, and to help prevent the development of high levels of needle fear. Finally, we introduce strategies for treating high levels of needle fear once they have been established. Through this content, this commentary will provide readers with a foundation to understand the other articles in this supplement.
TABLE 1.
Terminology and Concepts Related to Needle Fear and Pain: Definition, Lifespan Development, and Assessment*
VACCINATION: A PAINFUL AND FEAR-INDUCING EXPERIENCE
Needle procedures (eg, vaccine injections, venipunctures) are prevalent throughout the lifespan, particularly in childhood. The resulting pain may be considered “mild” by some individuals; however, for others, these needle procedures are far from benign (ie, not “just a poke”) and are associated with a high degree of pain and fear.26,27 Children in particular, are concerned about needle pain27,28 and report wanting to receive interventions for their pain at lower levels of pain intensity compared with adults.29 Across the lifespan, individuals report an absolute increase of approximately 10% in willingness to be vaccinated if the delivery were painless.27
Pain management is a human right.30 Evidence-based strategies for the management of pain and related outcomes (eg, fear, distress) during vaccinations have been reported7,31–34 and should be applied. Unfortunately, most individuals undergoing vaccination do not receive evidence-based treatments for their pain.3,4,35,36 In fact for pediatric populations, rather than prioritize pain management to address children’s strong concerns about pain, adult caregivers and clinicians have typically underprioritized and undertreated procedural pain.37,38 Thus, there is a large gap between scientific evidence and current practice that translates into continued unnecessary suffering for those undergoing needle procedures. In the current paper, we will argue that consideration of and intervention for acute pain during medical procedures undertaken in childhood is a necessary step toward reducing, and/or preventing longer-term sequelae of unmitigated pain. In particular, we focus on the development and consequences of needle fears and phobia that have been largely unappreciated by the health care community but have significant deleterious impact on the health outcomes of affected individuals.
Much more than a simple noxious stimulus leading to an individual’s sensory experience, the experience of pain also involves a host of other features including biological, psychological, social, and contextual factors39–41 (see also Fig. 1 which is consistent with the cited models). An integrative developmental framework is critical for understanding pain and fear in the vaccination context for several reasons. Firstly and perhaps most importantly, the amount of distress observed and pain reported during needle procedures tends to decrease as individuals get older (ie, younger children tend to be more at risk when undergoing the same procedure than older individuals.42–45 For example, the vast majority (90%) of 14- to 18-month-old infants and 45% of 4- to 6-year olds demonstrate severe distress during vaccination.45 Thus, individuals in early childhood who are subjected to the greatest number of vaccine injections,46 may be at most risk for acute suffering from these procedures. Secondly, the appropriate measurement of pain, fear, distress, and related constructs are influenced by age (Table 1); for example, young children may not be able to provide reliable self-report of their pain experience,47–49 but instead are dependent on others’ accurate interpretations of their behavioral distress to receive appropriate treatment. Thirdly, not only does an individual’s cognitive development impact his or her ability to understand the context of the pain, it also dictates appropriate intervention. Young children, for example, will not understand explanations for why vaccinations are needed, nor have the same arsenal of internal coping strategies to deal with pain as adults do. Rather, pain treatments should be provided and these should be tailored to the individual’s developmental stage.
Beyond acute suffering during vaccinations, developmental considerations are also important to understand the long-term risks of unmitigated pain, including the development of high levels of needle fear. Needle fear typically develops in early to middle childhood with peak age of onset between 5 and 10 years of age.50–52 Hence, efforts to mitigate procedural pain must also consider this developmentally sensitive window, which justifies a comprehensive treatment approach for young children to avoid both short-term and long-term suffering. As a particularly significant long-term risk of unmitigated pain, needle fear was incorporated into the HELPinKids&Adults knowledge synthesis and will be explored in detail in this paper.
After many decades of research, the Gate Control Theory and biopsychosocial models of pain all clearly indicate that emotions shape one’s pain experience and expression39,41,53; however, negative emotions regarding needle procedures such as vaccinations are often ignored. In the case of fear, this is particularly problematic, as fear seems to have a bidirectional relationship with pain. For example, greater perceived pain during needle procedures has been associated with higher levels of fear.27,54,55 Although acute pain from needles typically dissipates in the minutes, hours, or days after a needle, the emotional sequelae of unmanaged pain, most notably a fear of needles, can have a much longer lasting impact. Indeed, for some, pain and fear are not over when needle procedures end. Poorly managed needle pain can lead individuals to develop more fearful memories of pain over time,56 which may predict distress at future needle procedures.57 Thus, individuals can become fearful of the pain associated with the procedure, which may result in an escalating relationship between pain and fear over time (Fig. 1). In addition to fear of pain, individuals may also be apprehensive regarding other factors related to needle procedures, such as sitting in the waiting room, seeing blood, seeing the point of the needle, seeing the needle inserted, being “poked” multiple times with a needle, and being restrained.58
NEEDLE FEAR AND PHOBIA
Prevalence and Course
Children have long reported that receiving a needle is one of their most feared and painful experiences, and they are preoccupied with concerns about needles across health care settings.26,28,59,60 For example, “am I getting a shot today?” is a common question posed by children when they visit their doctor’s office.33 However, concerns regarding needle procedures do not simply vanish over the course of childhood; in fact, needle-related apprehension is common in adults as well.27,54,61,62 A recent study found that 63% of children endorsed a fear of needles,27 whereas several studies have reported adult prevalence rates of some degree of needle fear ranging from 14% to 38%.27,54,61,63–65 Because of clustering of phobia subtypes in traditional diagnostic classification systems (eg, Diagnostic and Statistical Manual of Mental Disorders by the American Psychiatric Association22), research is scarce on the epidemiology of needle phobia specifically. However, the lifetime prevalence of blood-injection-injury phobia (the broader categorization in which needle phobia is included) is estimated to be between 3% and 4.5%.50,51 Once established, and if left untreated, severe needle fear appears to follow a relatively stable, chronic course which can last for decades22,66,67; however, there is some evidence of a slight decrease in prevalence over time.68,69
Etiology
Although individuals may not disclose their fear of needles to a health professional until much later in life, the onset of needle fear and phobia is thought to occur in early to middle childhood (∼5 to 10 y of age50–52). By this time, individuals who are compliant with vaccination schedules will typically have received well over a dozen needles.46 Unfortunately, as previously noted, for the majority of children, there is a failure to implement evidence-based pain management strategies during these procedures.3,4 These repeated painful procedures in early childhood without benefit of treatment represent a risk factor for the development of high levels of needle fear. Figure 1 depicts the experience of needle procedures in childhood and over the lifespan, emphasizing the interplay between pain and fear; the following sections will focus on the development of fear in the context of these painful procedures and the impact of high levels of needle fear.
There is no 1 biological vulnerability, personality construct, life event, or combination thereof that can guarantee or protect against the development of a high degree of needle fear or needle phobia.70 A significant painful or traumatic event or set of events may, in isolation, lead to the development of severe needle fear and/or phobia (eg, engaging in painful cancer treatments63). However, a more broadly applicable perspective contends that high levels of needle fear likely emerge as the result of a number of factors present in childhood that either continued or amplified the fear into adulthood.
The developmental psychopathology perspective71,72 can be applied to help understand the factors that lead to high levels of needle fear and phobia in children and the adults they will become (see Racine et al73 for a related review). Using this organizational framework, each individual with severe needle fear or phobia is seen to arrive at this outcome through his or her own unique set of characteristics and behaviors, which differentially interact with his or her environment over the lifespan.74 Furthermore, an individual is seen as having both risk and protective factors influencing the pathway by which the severe needle fear would develop. These factors can predispose, precipitate, perpetuate, or protect against the development of pathologic fear.74,75
Predisposing, precipitating, perpetuating, and protective factors are frequently used to approach the conceptualization of psychopathology in children and adults (ie, provide a case formulation).75–77 Predisposing factors may include genetic factors, life events, or temperament, which put the individual at risk. There has been speculation that humans are biologically prepared to fear needles given (adaptive) fear of pain and fear of injury.70,78 Female sex and younger age have been shown to be significantly related to needle fear and phobia.27,50,54,62,63,79,80 Moreover, a hereditary component to blood-injection-injury phobia has been demonstrated with correlations between monozygotic twins reported as 0.49 and dizygotic twins as 0.10.81 A meta-analysis by Van Houtem et al82 reported the mean heritability of blood-injection-injury fears to be 41% (±SEM 0.06) and blood-injection-injury phobia to be 33% (±SEM 0.06).
Precipitating factors refer to triggering or catalytic events that have led to the onset of the current problem. Although not necessary nor sufficient to lead to the development of needle phobia in and of itself, having a history of fainting (vasovagal syncope) is positively related to needle fear.54,61,62,67 Moreover, having had a significant fear conditioning event either through directly experiencing needle-related negative sequelae (eg, experiencing pain, bleeding), watching someone else (eg, an older sibling) have these experiences, or simply being given negative information from a trusted source (eg, a parent; Fig. 1) are the most common precipitating events for the development of phobia.70,83 Although based on retrospective methods, individuals with needle fears typically report a traumatic conditioning experience, supporting the importance of conditioning events and unmitigated pain in this context.67,84,85
Perpetuating, or maintaining, factors are those that maintain the problem once it has become established. How individuals remember pain is one such factor. Distressing memories of needle pain and associated fear can develop from one poorly managed or negative procedure (a precipitating event) and are most likely to develop among highly anxious individuals.86,87 Individuals who are anxious about pain are likely to experience the needle procedure as more unpleasant, painful, and distressing. They are also likely to selectively attend to and encode threatening aspects of the needle procedure, which can lead to their memories of pain and fear becoming increasingly distressing over time such that they remember more pain and fear than they initially reported. This can fuel a negative cycle of increased fear, anxiety, and pain that becomes perpetuated and maintained over time and further reinforced at each subsequent procedure.88 This is likely why individuals who are highly apprehensive and fearful of needles can often root their concerns back to 1 poorly managed needle procedure in childhood.
Protective factors are strengths of the child or adult that reduce the severity of problems or promote healthy and adaptive functioning. For example, in 1 study, adults who self-selected to look at (ie, expose themselves to) the needle going into their arm reported less pain compared with those who chose to look away (ie, avoided)89 (but also see Goodenough et al43). Having a behavioral predisposition to face a fear-inducing stimulus could be a protective factor against developing a high level of needle fear; in fact, a key component of evidence-based treatments for phobias is exposure.90–92 One’s social context can also serve as a powerful protective factor.39 Adaptive responses from caregivers and significant others can encourage and reinforce coping as well as focus individuals’ attention on nonthreatening aspects of the needle procedure. Indeed, contingent on their content (eg, distraction, encouraging coping vs. reassurance, empathy), parental behavioral responses to child pain in the context of needle procedures have been shown to promote adaptive coping and decreased pain and fear.93–95 As well, anxiety and pain behaviors can be acquired through observational learning from others.40,96,97 Therefore, individuals can acquire adaptive cognitive and behavioral coping responses to pain experiences through such observational learning processes. Furthermore, caregivers and significant others can serve as strong advocates for individuals in helping them access and implement effective pain management interventions.
Consequences
Fear of needles has both proximal and distal negative consequences, particularly when it is of a moderate to high level. Proximal to the procedure: (1) children and adults with needle fear are more likely to report experiencing pain from procedures and fear of health care professionals20,54,61,98; (2) fear of needles is associated with a higher risk of experiencing physiological symptoms, including fainting and seizures,62,78,99 which can lead to serious safety concerns100 and have been highlighted as a major source of dental office emergencies80; and (3) parents of children with needle fears report challenges during the procedures, including flailing, running away, fainting, and requiring restraint to successfully complete the procedure.27 These consequences result in a negative, and potentially traumatic, experience for the needle recipient, the health care provider, and caregivers.
In terms of more distal consequences, those with acquired fears may require higher doses of analgesics for the same effects, resulting in further vulnerability to inadequately managed pain.101 Beyond a reluctance to donate blood,65 individuals of all ages who are afraid of needles are more likely to avoid preventative health care requiring needles, including blood tests, vaccinations, and dental care.27,61,62,102–105 Noncompliance with vaccinations is highly problematic given the importance of herd immunity in protecting communities from infectious diseases as well as the risk to individuals in vulnerable groups (eg, those over >65 y if they contract influenza102; the patients of health care providers who refuse influenza vaccination due to a fear of injections).104,106 A salient recent example is the outbreak of measles in the United States with 178 cases and 4 outbreaks in 17 states between January 1 and March 20, 2015 and 644 cases in 27 states in 2014.107 People with a chronic condition requiring treatment through needle procedures are particularly at risk because they avoid not only preventive care (eg, vaccination) but also their required, potentially lifesaving, therapeutic regimens (eg, insulin injections for diabetes, interferon injections for multiple sclerosis) leading to poorer health outcomes.62,78,108–111
Elevated fear and anxiety toward needles may generalize over time resulting in noncompliance with other health care behaviors; in fact, extreme levels of apprehension about, or refusal to comply with, blood tests can lead to avoidance of travel plans, education, career decisions, pregnancy, and even result in legal problems.78,80 Taken together, avoidance associated with fear of needles could lead to a significant economic burden through increased health care expenditures over time; that is, avoidance of preventative as well as lifesaving health care could lead to greater severity of ill health/disease/disorder and complications which in turn will cost society more in the long term than if the individual had been initially adherent. Not surprisingly, given these deleterious consequences, there has been a mounting concern regarding our understanding of these fears and their management.26,27,61,78,80,112 In response to these concerns, the current knowledge synthesis takes a novel, comprehensive approach by examining interventions for both the acute pain context and for high levels of needle fear.
IMPROVED MANAGEMENT OF NEEDLE-RELATED PAIN AND HIGH LEVELS OF NEEDLE FEAR: SYSTEMATIC REVIEWS IN THIS SERIES
Through broad and rigorous syntheses of the literature, the articles in this series provide evidence on the best care for infants, children, adolescents, and adults undergoing vaccination through pharmacological, physical, procedural, psychological, and process strategies11,12,14–17; limitations and future research directions cutting across the systematic reviews are also explored.113 Consistent application of effective pain management strategies for childhood vaccinations not only serves to reduce acute pain and suffering at the time of vaccination, but may also substantially reduce the development of high levels of needle fear and/or phobia. Individuals with a high degree of needle fear must be treated before they can fully benefit from the pharmacological, physical, procedural, and psychological strategies designed to make the procedure itself more comfortable; as such, a systematic review on the treatment of high levels of needle fear is also included in this series focusing on exposure-based psychological and physical strategies.13 This special series of papers is predominantly intended for researchers, but is also useful for health care professionals administering vaccinations and vaccination program managers across the world.
CONCLUSIONS
Vaccinations are one of the most beneficial lifesaving interventions of modern medicine.1,114 However, the significance of the vaccination-related adverse events of pain and associated needle fear has been neglected until recently, particularly in childhood. Health care providers need to incorporate pain management strategies into their clinical practice; parents and individuals being immunized should also be taught appropriate strategies. The purpose of this paper was to provide an overview of pain and fear in the context of needle procedures. Long after the acutely painful sensation is gone, the emotional sequelae surrounding the experience can linger. Over time, unmitigated pain may increase fear, which in turn, may increase pain at future procedures. Ideally, parents play a large role in having children face their needle fears and phobias by ensuring children comply with vaccination recommendations. However, children with high degrees of needle fear who struggle and are forced into what have become highly aversive needle situations grow up into adults who are responsible for their own health care decisions. These individuals can choose to avoid preventative care or experience these procedures with extremely negative physical and emotional reactions; furthermore, highly fearful adults may become parents themselves who may model needle fear to their children (Fig. 1). Acknowledging the psychological sequelae of needle procedures draws attention to the fact that unmanaged pain hurts more than just an individual’s body. The interventions included in the following series of articles are reviewed regarding their effectiveness for reducing the pain caused by vaccinations and for the management of needle fear. The evidence was used to inform the new (2015) HELPinKids&Adults clinical practice guidelines (also McMurtry CM, Taddio A, Noel M, et al., unpublished data, 2015).18
Footnotes
HELPinKids&Adults (Help ELiminate Pain in Kids & Adults) Team: MacDonald N. E., Rogers J., Bucci L., Mousmanis P., Halperin S. A., Bowles S., Halpert C., Ipp M., Rieder M., Robson K., Antony M. M., Dubey V., Hanrahan A., Lockett D., Scott J., Votta Bleeker E.
Supported by the Canadian Institutes of Health Research (CIHR), Ottawa, ON, Canada (KRS 132031). Open access funding was provided by the Mayday Fund in the United States. A. Taddio declares a grant from Pfizer, and study supplies from Natus and Ferndale. C.T. Chambers declares consultation fees from Abbvie. E. Lang is a member of the GRADE working group and declares consultation fees from the International Liaison Committee on Resuscitation (ILCOR). L. Bucci declares a relationship with government agencies and grants from Merck, GSK, Novartis, Sanofi, and Pfizer. S.A. Halperin declares grants from GSK, Sanofi, Novartis, Pfizer, Merck, PREVENT, ImmunoVaccine, NovaVax, Janssen, and Folia. The remaining authors declare no conflict of interest.
Contributor Information
Collaborators: HELPinKids&Adults Team
REFERENCES
- 1.Ulmer JB, Valley U, Rappuoli R. Vaccine manufacturing: challenges and solutions. Nat Biotechnol. 2006;24:1377–1383. [DOI] [PubMed] [Google Scholar]
- 2.Miller MA, Pisani E. The cost of unsafe injections. Bull World Health Organ. 1999;77:808–811. [PMC free article] [PubMed] [Google Scholar]
- 3.Lisi D, Campbell L, Pillai Riddell R, et al. Naturalistic parental pain management during immunizations during the first year of life: observational norms from the OUCH cohort. Pain. 2013;154:1245–1253. [DOI] [PubMed] [Google Scholar]
- 4.Taddio A, Manley J, Potash L, et al. Routine immunization practices: use of topical anesthetics and oral analgesics. Pediatrics. 2007;120:e637–e643. [DOI] [PubMed] [Google Scholar]
- 5.Chorney JM, McGrath PJ, Finley GA. Pain as the neglected adverse event. CMAJ. 2010;182:732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gidudu JF, Walco GA, Taddio A, et al. Immunization site pain: case definition and guidelines for collection, analysis, and presentation of immunization safety data. Vaccine. 2012;30:4558–4577. [DOI] [PubMed] [Google Scholar]
- 7.Taddio A, Appleton M, Bortolussi R, et al. Reducing the pain of childhood vaccination: an evidence-based clinical practice guideline (summary). CMAJ. 2010;182:1989–1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chambers CT, Taddio A, Uman LS, et al. Psychological interventions for reducing pain and distress during routine childhood immunizations: a systematic review. Clin Ther. 2009;31(suppl B):S77–S103. [DOI] [PubMed] [Google Scholar]
- 9.Shah V, Taddio A, Rieder MJ, et al. Effectiveness and tolerability of pharmacological and combined interventions for reducing injection pain during routine childhood immunizations: systematic review and meta-analyses. Clin Ther. 2009;31(suppl 2):s104–s151. [DOI] [PubMed] [Google Scholar]
- 10.Taddio A, Ilersich AL, Ipp M, et al. Physical interventions and injection techniques for reducing injection pain during routine childhood immunizations: systematic review of randomized controlled trials and quasi-randomized controlled trials. Clin Ther. 2009;31(suppl 2):s48–s76. [DOI] [PubMed] [Google Scholar]
- 11.Birnie KA, Chambers CT, Taddio A, et al. Psychological interventions for vaccine injections in children and adolescents: systematic review of randomized and quasi-randomized controlled trials. Clin J Pain. 2015;31(Supplement 10):S72–S89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boerner KE, Birnie KA, Chambers CT, et al. Simple Psychological Interventions for Reducing Pain From Common Needle Procedures in Adults Systematic Review of Randomized and Quasi-Randomized Controlled Trials. Clin J Pain. 2015;31(Supplement 10):S90–S98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McMurtry CM, Noel M, Taddio A, et al. Interventions for Individuals With High Levels of Needle Fear: Systematic Review of Randomized Controlled Trials and Quasi-Randomized Controlled Trials. Clin J Pain. 2015;31(Supplement 10):S109–S123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pillai Riddell R, Taddio A, McMurtry CM, et al. Psychological interventions for vaccine injections in young children 0 to 3 years: systematic review of randomized controlled trials and quasi-randomized controlled trials. Clin J Pain. 2015;31(Supplement 10):S64–S71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pillai Riddell R, Taddio A, McMurtry CM, et al. Process interventions for vaccine injections: systematic review of randomized controlled trials and quasi-randomized controlled trials. Clin J Pain. 2015;31(Supplement 10):S99–S108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shah V, Taddio A, McMurtry CM, et al. Pharmacological and combined interventions to reduce vaccine injection pain in children and adults: systematic review and meta-analysis. Clin J Pain. 2015;31(Supplement 10):S38–S63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taddio A, Shah V, McMurtry CM, et al. Procedural and physical interventions for vaccine injections: systematic review of randomized controlled trials and quasi-randomized controlled trials. Clin J Pain. 2015;31(Supplement 10):S20–S37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Taddio A, McMurtry CM, Shah V, et al. Reducing pain during vaccine injections: clinical practice guideline. CMAJ. 2015; Aug 24. [Epub ahead of print]. DOI:10.1503?/cmaj.150391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Merskey H, Bogduk N. Classification of chronic pain: Descriptions of chronic pain syndromes and definitions of pain terms, 2nd ed. Seattle, WA: IASP Press; 1994. [Google Scholar]
- 20.Gullone E. The development of normal fear: a century of research. Clin Psychol Rev. 2000;20:429–451. [DOI] [PubMed] [Google Scholar]
- 21.Barlow DH. Anxiety and Its Disorders: The Nature and Treatment of Anxiety and Panic, 2nd ed New York: Guilford Press; 2002. [Google Scholar]
- 22.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Publishing; 2013. [Google Scholar]
- 23.World Health Organization. The International Classifications of Diseases. Available at: http://apps.who.int/classifications/icd10/browse/2015/en. Accessed July 9, 2015.
- 24.Oxford Dictionaries. 2015. Available at: http://www.oxforddictionaries.com/definition/english/distress. Accessed July 9, 2015.
- 25.Bracha HS, Ralston TC, Matsukawa JM, et al. Does “fight or flight” need updating? Psychosomatics. 2004;45:448–449. [DOI] [PubMed] [Google Scholar]
- 26.Taddio A, Chambers CT, Halperin SA, et al. Inadequate pain management during routine childhood immunizations: the nerve of it. Clin Ther. 2009;31:s152–s167. [DOI] [PubMed] [Google Scholar]
- 27.Taddio A, Ipp M, Thivakaran S, et al. Survey of the prevalence of immunization non-compliance due to needle fears in children and adults. Vaccine. 2012;30:4807–4812. [DOI] [PubMed] [Google Scholar]
- 28.Taddio A, Ilersich AF, Ilersich AN, et al. From the mouth of babes: getting vaccinated doesn’t have to hurt. Can J Infect Dis Med Microbiol. 2014;25:196–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dalley JS, McMurtry CM, Creary P. Pain tolerance of parents and children during needle procedures. Poster presented at the Canadian Pain Society 35th Annual Scientific Meeting.Quebec, QC; 2014.
- 30.Brennan F, Carr DB, Cousins M. Pain management: a fundamental human right. Anesth Analg. 2007;105:205–221. [DOI] [PubMed] [Google Scholar]
- 31.Birnie KA, Noel M, Parker JA, et al. Systematic review of psychological interventions of distraction and hypnosis for needle related pain and distress in children and adolescents. J Pediatr Psychol. 2014;39:783–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pillai Riddell RR, Racine NM, Turcotte K, et al. Non-pharmacological management of infant and young child procedural pain. Cochrane Database Syst Rev. 2015. (In press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schechter NL, Zempsky WT, Cohen LL, et al. Pain reduction during pediatric immunizations: evidence-based review and recommendations. Pediatrics. 2007;19:e1184–e1198. [DOI] [PubMed] [Google Scholar]
- 34.Uman LS, Birnie KA, Noel M, et al. Psychological interventions for needle-related procedural pain and distress in children and adolescents. Cochrane Database Syst Rev. 2013;10Art. No.: CD005179. DOI: 10.1002/14651858.CD005179.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Berberich FR, Schechter NL. Pediatric office pain: crying for attention. Pediatrics. 2012;129:1057–1059. [DOI] [PubMed] [Google Scholar]
- 36.Harrison D, Elia S, Royle J, et al. Pain management strategies used during early childhood immunisation in Victoria. J Pediatr Child Health. 2013;49:313–318. [DOI] [PubMed] [Google Scholar]
- 37.Stevens B, Abbott LK, Yamada J, et al. Epidemiology and management of painful procedures in children in Canadian hospitals. CMAJ. 2011;19:e403–e410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Taddio A.McGrath PJ, Stevens BJ, Walker SM, et al. Needle procedures. Oxford Textbook of Paediatric Pain. Oxford, UK: Oxford University Press; 2013:184–193. [Google Scholar]
- 39.Craig KD. The social communication model of pain. Can Psychol. 2009;50:22–32. [Google Scholar]
- 40.Hadjistavropoulos T, Craig KD, Duck S, et al. A biopsychosocial formulation of pain communication. Psychol Bull. 2011;137:910–939. [DOI] [PubMed] [Google Scholar]
- 41.Pillai Riddell RR, Racine N, Craig K, et al. McGrath PJ, Stevens BJ, Walker SM, et al. Psychological theories and biopsychosocial models in paediatric pain. Oxford Textbook of Paediatric Pain. Oxford, UK: Oxford University Press; 2013:85–94. [Google Scholar]
- 42.Fradet C, McGrath PJ, Kay J, et al. A prospective survey of reactions to blood tests by children and adolescents. Pain. 1990;40:53–60. [DOI] [PubMed] [Google Scholar]
- 43.Goodenough B, Champion GD, Laubreaux L, et al. Needle pain severity in children: does the relationship between self-report and observed behaviour vary as a function of age. Aust J Psychol. 1998;50:1–9. [Google Scholar]
- 44.Humphrey GB, Boon CM, van Linden van den Heuvell GF, et al. The occurrence of high levels of acute behavioral distress in children and adolescents undergoing routine venipunctures. Pediatrics. 1992;90:87–91. [PubMed] [Google Scholar]
- 45.Jacobson RM, Swan A, Adegbenro A, et al. Making vaccines more acceptable—methods to prevent and minimize pain and other common adverse events associated with vaccines. Vaccine. 2001;19:2418–2427. [DOI] [PubMed] [Google Scholar]
- 46.Public Health Agency of Canada. Canadian immunization guide [Public Health Agency of Canada website]. Available at: http://www.phac-aspc.gc.ca/publicat/cig-gci/index-eng.php. Accessed July 9, 2015.
- 47.Chambers CT, Johnston C. Developmental differences in children’s use of rating scales. J Pediatr Psychol. 2002;27:27–36. [DOI] [PubMed] [Google Scholar]
- 48.von Baeyer CL, Chambers CT, Forsyth SJ, et al. Developmental data supporting simplification of self-report pain scales for preschool-age children. J Pain. 2013;14:1116–1121. [DOI] [PubMed] [Google Scholar]
- 49.von Baeyer CL, Forsyth SJ, Stanford EA, et al. Response biases in preschool children’s ratings of pain in hypothetical situations. Eur J Pain. 2009;2:209–213. [DOI] [PubMed] [Google Scholar]
- 50.Bienvenu OJ, Eaton WW. The epidemiology of blood-injection-injury phobia. Psychol Med. 1998;28:1129–1136. [DOI] [PubMed] [Google Scholar]
- 51.LeBeau RT, Glenn D, Liao B, et al. Specific phobia: a review of DSM-IV specific phobia and preliminary recommendations for DSM-V. Depress Anxiety. 2010;27:148–167. [DOI] [PubMed] [Google Scholar]
- 52.Thyer BA, Himle J, Curtis GC. Blood-injury-illness phobia: a review. J Clin Psychol. 1985;41:451–459. [DOI] [PubMed] [Google Scholar]
- 53.Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150:971–979. [DOI] [PubMed] [Google Scholar]
- 54.Deacon B, Abramowitz J. Fear of needles and vasovagal reactions among phlebotomy patients. J Anxiety Disord. 2006;20:946–960. [DOI] [PubMed] [Google Scholar]
- 55.McMurtry CM, Noel M, Chambers CT, et al. Children’s fear during procedural pain: preliminary investigation of the Children’s Fear Scale. Health Psychol. 2011;30:780–788. [DOI] [PubMed] [Google Scholar]
- 56.Noel M, McMurtry CM, Chambers CT, et al. Children’s memory for painful procedures: the relationship of pain intensity, anxiety, and adult behaviors to subsequent recall. J Pediatr Psychol. 2010;35:626–636. [DOI] [PubMed] [Google Scholar]
- 57.Chen E, Zeltzer LK, Craske MG, et al. Children’s memories for painful cancer treatment procedures: implications for distress. Child Dev. 2000;71:933–947. [DOI] [PubMed] [Google Scholar]
- 58.Dalley JS, Creary P, McMurtry CM. What are you afraid of? Exploring the specific fears of children and adults regarding painful and other aspects of needle procedures. Poster presented at the International Association for the Study of Pain’s 15th World Congress on Pain. Argentina: Buenos Aires; 2014.
- 59.Broome ME, Hellier AP. School-age children’s fears of medical experiences. Issues Compr Pediatr Nurs. 1987;10:77–86. [DOI] [PubMed] [Google Scholar]
- 60.Hart D, Bossert E. Self-reported fears of hospitalized school-aged children. J Pediatr Nurs. 1994;9:83–90. [PubMed] [Google Scholar]
- 61.Armfield JM, Milgrom P. A clinician guide to patients afraid of dental injections and numbness. SAAD Dig. 2011;27:33–39. [PubMed] [Google Scholar]
- 62.Wright S, Yelland M, Heathcote K, et al. Fear of needles: nature and prevalence in general practice. Aust Fam Physician. 2009;38:172–176. [PubMed] [Google Scholar]
- 63.Cox AC, Fallowfield LJ. After going through chemotherapy I can’t see another needle. Eur J Oncol Nurs. 2007;11:43–48. [DOI] [PubMed] [Google Scholar]
- 64.Nir Y, Paz A, Sabo E, et al. Fear of injections in young adults: prevalence and associations. Am J Trop Med Hyg. 2003;68:341–344. [PubMed] [Google Scholar]
- 65.Oswalt RM, Napoliello M. Motivations of blood donors and nondonors. J Appl Psychol. 1974;59:122–124. [Google Scholar]
- 66.Goisman RM, Allsworth J, Rogers MP, et al. Simple phobia as a comorbid anxiety disorder. Depress Anxiety. 1998;7:105–112. [PubMed] [Google Scholar]
- 67.Öst L-G. Blood and injection phobia: background and cognitive, physiological, and behavioral variables. J Abnorm Psychol. 1992;101:68–74. [DOI] [PubMed] [Google Scholar]
- 68.Agras S, Sylvester D, Oliveau D. The epidemiology of common fears and phobia. Compr Psychiatry. 1969;10:151–156. [DOI] [PubMed] [Google Scholar]
- 69.Stinson FS, Dawson DA, Chou SP, et al. The epidemiology of DSM-IV specific phobia in the USA: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2007;37:1047–1059. [DOI] [PubMed] [Google Scholar]
- 70.Du S, Jaaniste T, Champion GD, et al. Theories of fear acquisition: the development of needle phobia in children. Pediatr Pain Letter. 2008;10:13–17. [Google Scholar]
- 71.Cicchetti DE, Cohen DJ. Developmental Psychopathology, Vol 1: Theory and Methods. New York: John Wiley & Sons; 1995. [Google Scholar]
- 72.Sroufe LA, Rutter M. The domain of developmental psychopathology. Child Dev. 1984;55:17–29. [PubMed] [Google Scholar]
- 73.Racine N, Pillai Riddell R, Khan M, et al. Systematic review: Predisposing, precipitating, perpetuating and present factors predicting anticipatory distress to painful medical procedures. J Pediatr Psychol 2015. (In press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Vasey MW, Dadds MR. The Developmental Psychopathology of Anxiety. New York: Oxford University Press; 2001. [Google Scholar]
- 75.Carr A. Handbook of Child and Adolescent Clinical Psychology: a Contextual Approach. London: Routledge; 1999. [Google Scholar]
- 76.Havighurst SS, Downey L. Clinical reasoning for child and adolescent mental health practitioners: the mindful formulation. Clin Child Psychol Psychiatry. 2009;14:251–271. [DOI] [PubMed] [Google Scholar]
- 77.Macneil CA, Hasty MK, Conus P, et al. Is diagnosis enough to guide interventions in mental health? Using case formulation in clinical practice. BMC Med. 2012;10:111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hamilton JG. Needle phobia: a neglected diagnosis. J Fam Pract. 1995;41:169–175. [PubMed] [Google Scholar]
- 79.Page AC. Blood-injury phobia. Clin Psychol Rev. 1994;14:443–461. [Google Scholar]
- 80.Sokolowski CJ, Giovannitti JA, Boynes SG. Needle phobia: etiology, adverse consequences, and patient management. Dent Clin North Am. 2010;54:731–744. [DOI] [PubMed] [Google Scholar]
- 81.Neale MC, Walters EE, Eaves LJ, et al. Genetics of blood-injury fears and phobias: a population-based twin study. Am J Med Genet. 1994;54:326–334. [DOI] [PubMed] [Google Scholar]
- 82.Van Houtem CM, Laine ML, Boomsma DI, et al. A review and meta-analysis of the heritability of specific phobia subtypes and corresponding fears. J Anxiety Disord. 2013;27:379–388. [DOI] [PubMed] [Google Scholar]
- 83.Rachman S. The conditioning theory of fear-acquisition: a critical examination. Behav Res Ther. 1977;15:375–387. [DOI] [PubMed] [Google Scholar]
- 84.Kleinknecht RA. Acquisition of blood, injury, and needle fears and phobias. Behav Res Ther. 1994;32:817–823. [DOI] [PubMed] [Google Scholar]
- 85.Öst L-G. Acquisition of blood and injection phobia and anxiety response patterns in clinical patients. Behav Res Ther. 1991;29:323–332. [DOI] [PubMed] [Google Scholar]
- 86.Noel M, Chambers CT, McGrath PJ, et al. The influence of children’s pain memories on subsequent pain experience. Pain. 2012;153:1563–1572. [DOI] [PubMed] [Google Scholar]
- 87.Noel M, Chambers CT, McGrath PJ, et al. The role of state anxiety in children’s memories for pain. J Pediatr Psychol. 2012;37:567–579. [DOI] [PubMed] [Google Scholar]
- 88.Noel M, Chambers CT, Petter M, et al. Pain is not over when the needle ends: a review and preliminary model of acute pain memory development in childhood. Pain Manag. 2012;2:487–497. [DOI] [PubMed] [Google Scholar]
- 89.Vijayan R, Scott G, Brownlie W. Out of sight, but not out of mind? Greater reported pain in patients who spontaneously look away during venepuncture. Eur J Pain. 2015;19:97–102. [DOI] [PubMed] [Google Scholar]
- 90.Ayala ES, Meuret AE, Ritz T. Treatments for blood-injury-injection phobia: a critical review of current evidence. J Psychiatr Res. 2009;43:1235–1242. [DOI] [PubMed] [Google Scholar]
- 91.Choy Y, Fyer AJ, Lipsitz JD. Treatment of specific phobia in adults. Clin Psychol Rev. 2007;27:266–286. [DOI] [PubMed] [Google Scholar]
- 92.Wolitzky-Taylor KB, Horowitz JD, Powers MB, et al. Psychological approaches in the treatment of specific phobias: a meta-analysis. Clin Psychol Rev. 2008;28:1021–1037. [DOI] [PubMed] [Google Scholar]
- 93.Blount RL, Bachanas PJ, Powers SW, et al. Training children to cope and parents to coach them during routine immunizations: effects on child, parent, and staff behaviors. Behav Ther. 1992;23:689–705. [Google Scholar]
- 94.Blount RL, Corbin SM, Sturges SM, et al. The relationship between adults’ behavior and child coping and distress during BMA/LP procedures: a sequential analysis. Behav Ther. 1989;20:585–601. [Google Scholar]
- 95.McMurtry CM, Chambers CT, McGrath PJ, et al. When “don’t worry” communicates fear: children’s perceptions of parental reassurance and distraction during a painful medical procedure. Pain. 2010;150:52–58. [DOI] [PubMed] [Google Scholar]
- 96.Goubert L, Vlaeyen JWS, Crombez G, et al. Learning about pain from others: an observational learning account. J Pain. 2011;12:167–174. [DOI] [PubMed] [Google Scholar]
- 97.Mineka S, Zinbarg R. A contemporary learning theory perspective on the etiology of anxiety disorders: it’s not what you thought it was. Am Psychol. 2006;61:10–26. [DOI] [PubMed] [Google Scholar]
- 98.Meade MA, France CR, Peterson LM. Predicting vasovagal reactions in volunteer blood donors. J Psychosom Res. 1996;40:495–501. [DOI] [PubMed] [Google Scholar]
- 99.Marks I. Blood-injury phobia: a review. Am J Psychiatry. 1988;145:1207–1213. [DOI] [PubMed] [Google Scholar]
- 100.Centers for Disease Control and Prevention. Syncope After Vaccination—United States, January 2005-July 2007. JAMA. 2008;299:2502–2506. [Google Scholar]
- 101.Weisman SJ, Bernstein B, Schechter NL. Consequences of inadequate analgesia during painful procedures in children. Arch Pediatr Adolesc Med. 1998;152:147–149. [DOI] [PubMed] [Google Scholar]
- 102.Centers for Disease Control and Prevention. Reasons reported by Medicare beneficiaries for not receiving influenza and pneumococcal vaccinations—United States. MMWR Morb Mortal Wkly Rep. 1999;48:886–890. [PubMed] [Google Scholar]
- 103.Johnson DR, Nichol KL, Lipczynski K. Barriers to adult immunization. Am J Med. 2008;121(suppl 2):S28–S35. [DOI] [PubMed] [Google Scholar]
- 104.Naz H, Cevik F, Aykin N. Influenza vaccination in healthcare workers. J Infect Dev Ctries. 2009;3:50–54. [DOI] [PubMed] [Google Scholar]
- 105.Zimmerman RK, Santibanez TA, Janosky JE, et al. What affects influenza vaccination rates among older patients? An analysis from inner-city, suburban, rural, and Veterans Affairs practices. Am J Med. 2003;114:31–38. [DOI] [PubMed] [Google Scholar]
- 106.Hofmann F, Ferracin C, Marsh G, et al. Influenza vaccination of healthcare workers: a literature review of attitudes and beliefs. Infection. 2006;34:142–147. [DOI] [PubMed] [Google Scholar]
- 107.Centers for Disease Control and Prevention. Measles cases and outbreaks [Centers for Disease Control and Prevention website]. Available at: http://www.cdc.gov/measles/casesoutbreaks.html. Accessed April 1, 2015.
- 108.Ellinwood EH, Hamilton JG. Case report of a needle phobia. J Fam Pract. 1991;32:420–422. [PubMed] [Google Scholar]
- 109.Howe C, Ratcliffe S, Tuttle A, et al. Needle anxiety in children with type 1 diabetes and their mothers. MCN Am J Matern Child Nurs. 2011;36:25–31. [DOI] [PubMed] [Google Scholar]
- 110.Mohr DC, Boudewyn AC, Likosky W, et al. Injectable medication for the treatment of multiple sclerosis: the influence of self-efficacy expectations and injection anxiety on adherence and ability to self-inject. Ann Behav Med. 2001;23:125–132. [DOI] [PubMed] [Google Scholar]
- 111.Rzeszut JR. Children with diabetes: the impact of fear of needles. J Pediatr Nurs. 2011;26:589–592. [DOI] [PubMed] [Google Scholar]
- 112.Willemsen H, Chowdhury U, Briscall L. Needle phobia in children: a discussion of aetiology and treatment options. Clin Child Psychol Psychiatry. 2002;7:609–619. [Google Scholar]
- 113.Noel M, Taddio A, McMurtry CM, et al. HELPinKids&Adults knowledge synthesis of the management of vaccination pain and high levels of needle fear: limitations of the evidence and recommendations for future research. Clin J Pain. 2015;31:S124–S131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.World Health Organization, UNICEF, World Bank. State of the World’s Vaccines and Immunization, 3rd Geneva, Switzerland: World Health Organization; 2009. [Google Scholar]


