Supplemental Digital Content is available in the text.
Key Words: pain management, randomized controlled trial, systematic review, psychological, needle pain
Abstract
Background:
This systematic review evaluated the effectiveness of simple psychological interventions for managing pain and fear in adults undergoing vaccination or related common needle procedures (ie, venipuncture/venous cannulation).
Design/Methods:
Databases were searched to identify relevant randomized and quasi-randomized controlled trials. Self-reported pain and fear were prioritized as critically important outcomes. Data were combined using standardized mean difference (SMD) or relative risk (RR) with 95% confidence intervals (CI).
Results:
No studies involving vaccination met inclusion criteria; evidence was drawn from 8 studies of other common needle procedures (eg, venous cannulation, venipuncture) in adults. Two trials evaluating the impact of neutral signaling of the impending procedure (eg, “ready?”) as compared with signaling of impending pain (eg, “sharp scratch”) demonstrated lower pain when signaled about the procedure (n=199): SMD=−0.97 (95% CI, −1.26, −0.68), after removal of 1 trial where self-reported pain was significantly lower than the other 2 included trials. Two trials evaluated music distraction (n=156) and demonstrated no difference in pain: SMD=0.10 (95% CI, −0.48, 0.27), or fear: SMD=−0.25 (95% CI, −0.61, 0.10). Two trials evaluated visual distraction and demonstrated no difference in pain (n=177): SMD=−0.57 (95% CI, −1.82, 0.68), or fear (n=81): SMD=−0.05 (95% CI, −0.50, 0.40). Two trials evaluating breathing interventions found less pain in intervention groups (n=138): SMD=−0.82 (95% CI, −1.21, −0.43). The quality of evidence across all trials was very low.
Conclusions:
There are no published studies of simple psychological interventions for vaccination pain in adults. There is some evidence of a benefit from other needle procedures for breathing strategies and neutral signaling of the start of the procedure. There is no evidence for use of music or visual distraction.
Vaccine injections are widely used across the lifespan, including in adults of all ages (eg, annual influenza vaccination, immunizations necessary for travel or employment). Multiple forms of interventions are available to manage pain from vaccinations, including pharmacological, psychological, procedural, physical, and process approaches. There are many benefits to simple and feasible psychological approaches, such as music distraction or simple verbal statements from health professionals, as they are time and cost efficient, use widely available resources, and often require little to no training for use; hence, can be easily implemented by health care providers carrying out the procedure. While pain management during vaccine injections has been emphasized in children,1 it is critical to also examine the efficacy of such strategies in adults, as adults report desiring treatment for their needle pain2 and report that decreased immunization pain is related to an increased willingness to be immunized.3 This highlights the importance of considering how pain can optimally be managed for adults in this context.
In previous reviews, support was found for several psychological interventions for use with children,4 which were incorporated as recommendations in a clinical practice guideline for vaccination pain management in children.1 The literature on psychological approaches for managing needle pain in children continues to grow,5 including attempts to identify specific characteristics of interventions that may contribute to their efficacy.6 To date, there has been no systematic synthesis of the available literature on psychological interventions for vaccination pain management in adults. Major developmental differences in cognitive domains could contribute to differential efficacy of treatments between children and adults, including differences in preferences, attention, executive and other cognitive functions, coping, and ability to regulate emotions.7 The objective of the current systematic review was to address this gap to synthesize existing literature to inform development of clinical practice guidelines for psychological approaches to managing vaccination pain in adults.
This review describes the synthesis of results from trials that examined the effect of the following simple psychological interventions on pain: (1) providing a signal about the impending procedure (eg, “ready?,” “beware”) as compared with providing a signal about the impending pain (eg, “sharp scratch,” “sting”); (2) the use of music as distraction during the procedure; (3) the use of visual distraction (looking in a kaleidoscope) during the procedure; and (4) the use of breathing intervention (eg, coughing, breath-holding). Given the lack of direct evidence for the effects of psychological interventions in adults undergoing vaccinations, our synthesis examined indirect evidence (ie, venipuncture and venous cannulation). Separate reviews explore the effectiveness of psychological interventions in young children (0 to 3 y old) and children and adolescents (>3 to 17 y old), as well as pharmacological, physical, and procedural approaches for infants, children, adolescents, and adults.8–13
METHODS
A consistent approach was used to carry out all systematic reviews examining various pain management intervention types; the methodological details of the approach are described elsewhere.14 Briefly, both the GRADE (Grading of Recommendations, Assessments, Development and Evaluation)15 and Cochrane16 methodologies were used to guide the review. The search strategy was developed with the assistance of an experienced librarian and was conducted in the following databases: EMBASE, Medline, PsycINFO, CINAHL, and ProQuest Dissertations & Theses Global. Relevant citations were screened and included as per the protocol described in a separate manuscript.14
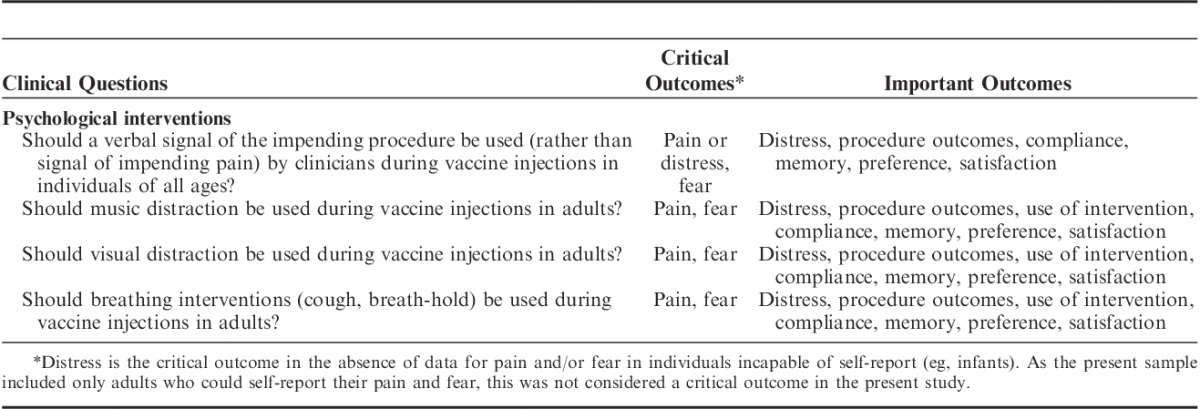
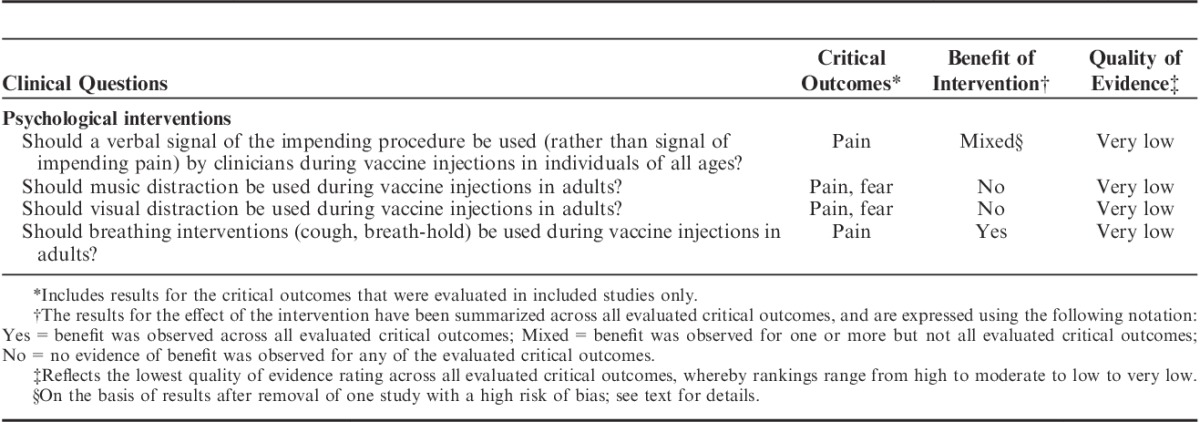
Given the purpose of this review was to inform the development of clinical practice guidelines for pain management for vaccine injections across the lifespan, this review prioritized studies including adults undergoing vaccination in any setting, or if not undergoing vaccination, the closest related needle procedure (venipuncture and venous cannulation). Only randomized or quasi-randomized study designs were examined. We included studies published as a full report, short report, or published academic theses. The included interventions and outcomes included in the review were identified by a national multidisciplinary team, Help ELiminate Pain in Kids and Adults (HELPinKids&Adults), assembled for the specific purpose of undertaking knowledge translation activities in immunization pain management. As described in the accompanying manuscript describing the methodology of this series of reviews,14 a broad search was used to identify relevant literature for consideration of clinical questions, including previously published clinical practice guidelines, existing research, and clinical experience of the team. The aforementioned team voted on candidate questions, and questions that at least two-thirds of the HELPinKids&Adults team considered to be important were included.14 For the present review, only simple psychological interventions (ie, interventions that could be implemented with minimal/no training and equipment, and that were time and cost efficient to deliver) were included due to feasibility and ease of implementation within the immunization context. Self-reported pain and fear were prioritized as critically important outcomes, and data from these outcomes were extracted as available. Important outcomes included distress (observer-rated), procedure outcomes, compliance, memory, preference, use of intervention, and satisfaction. A list of included clinical questions and critically important and important outcomes is shown in Table 1.
TABLE 1.
Clinical Questions and Outcomes
The Cochrane risk of bias tool (https://bmg.cochrane.org/assessing-risk-bias-included-studies) was used to evaluate the methodological quality of the included studies. Data were pooled and analyzed using the RevMan software program (version 5.2; Cochrane Collaboration, Copenhagen, Denmark). The effect of each intervention was expressed as a standardized mean difference (SMD) for continuous variables, or relative risk for dichotomous variables, with accompanying 95% confidence interval (CI). A random-effects model was used for all analyses, with the I2 and χ2 tests used to assess for statistical heterogeneity.14
When not reported in the published manuscript text, means and SDs were estimated from medians, ranges, SEs, 95% CI, and graphs provided in published papers. Authors of trials were contacted for further details and provision of original data when not available. As needed, the original data were modified (eg, range conversion to SD) on a very restricted predefined basis, according to established methods.14 Evidence profiles and summary of findings tables were created using the GRADE profiler software (version 3.6.1).
RESULTS
A total of 114,251 references were retrieved from the databases, with an additional 138 references identified separately from manual searches. All references were saved in an EndNote library that identified 32,155 duplicates. The remaining 82,234 references were reviewed by 2 of the authors (A.T., V.S.) against the inclusion criteria.14 No studies directly examining vaccination met inclusion criteria. Eight studies investigating psychological interventions for venipuncture/venous cannulation (ie, indirect evidence) were included in the review.17–24 The profile summarizing the trial flow is shown in Figure 1.
FIGURE 1.
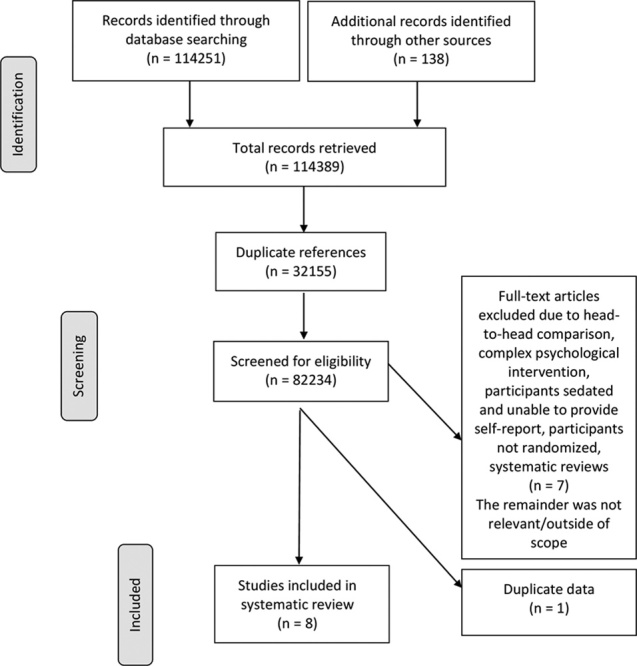
Flow of studies.
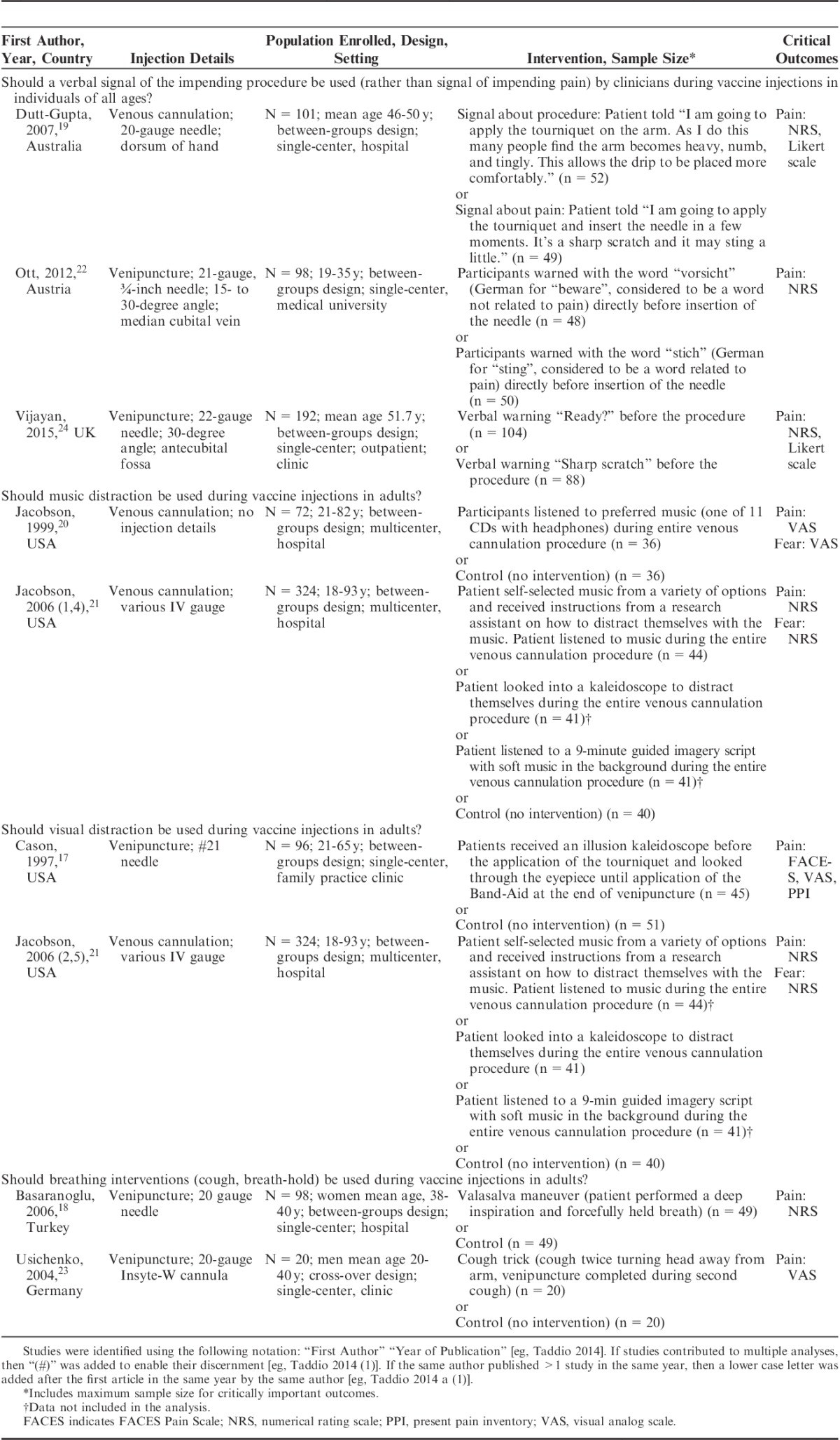
Characteristics of included trials are reported in Table 2. Excluded studies included: (1) complex psychological interventions (eg, functional relaxation)25 (n=1); (2) head-to-head comparisons26,27 (n=2); (3) studies in which participants were sedated with benzodiazepine and unable to give self-report28,29 (n=2); (4) studies where all participants had a choice of which intervention they preferred and were therefore not randomized30 (n=1); and (5) systematic reviews31 (n=1). In addition, 1 study was excluded as it presented data from the same sample as an included study, but did not examine any critical outcomes.32 Altogether, 7 studies used a between-groups (parallel) design, and 1 study used a cross-over design. All studies provided data for 2 or more treatment arms. Included studies took place in a variety of clinical settings (ie, tertiary care hospitals, outpatient clinics). Of the 8 included studies, 3 examined venous cannulation, and 5 examined venipuncture. Studies included both healthy participants as well as patients awaiting surgery.
TABLE 2.
Characteristics of Trials Included in the Systematic Review
Quality of Studies and Risk of Bias
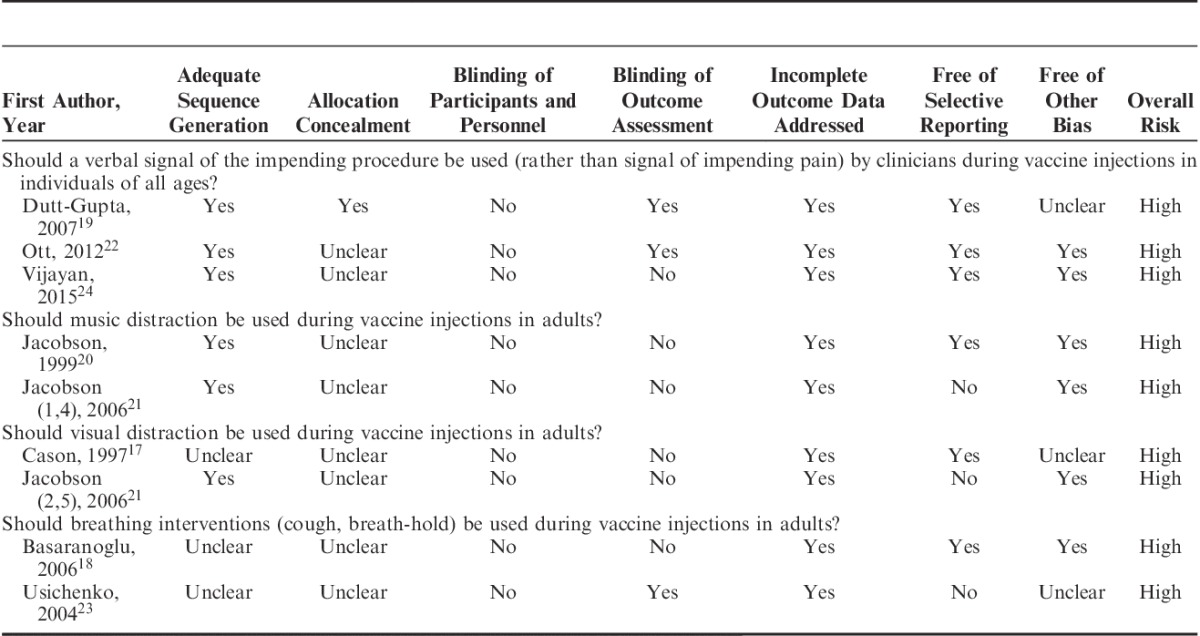
Table 3 shows the results for the risk of bias assessment for critically important outcomes. All trials had a high overall risk of bias primarily due to lack of blinding of important personnel, outcome assessors (eg, participants, immunizers), or both, and unclear allocation concealment.
TABLE 3.
Assessment of Risk of Bias of Included Trials for Critical Outcomes
Overall Quality of Evidence and Treatment Effects
A quantitative summary of the treatment effects for available critically important outcomes is provided below. Table 4 displays a qualitative summary of these results. In addition, GRADE evidence profiles and summary of findings tables (Tables, Supplemental Digital Contents 1 to 4, http://links.lww.com/CJP/A217, http://links.lww.com/CJP/A218, http://links.lww.com/CJP/A219, http://links.lww.com/CJP/A220) and accompanying forest plots (Figures, Supplemental Digital Contents 1 to 4, http://links.lww.com/CJP/A221, http://links.lww.com/CJP/A222, http://links.lww.com/CJP/A223, http://links.lww.com/CJP/A224) for critically important and important outcomes are included as Supplemental Digital Contents.
TABLE 4.
Summary of Results for Critically Important Outcomes
Should a Verbal Signal of the Impending Procedure be Used (Rather Than Signal of Impending Pain) by Clinicians During Vaccine Injections in Individuals of All Ages?
Three trials including 402 adults investigated the impact of signaling about the start of the procedure as compared with signaling about the impending pain during venous cannulation19 or venipuncture.22,24 There was very low quality of evidence because of high risk of bias and imprecision for all outcomes (Table, Supplemental Digital Content 1, http://links.lww.com/CJP/A217). All 3 studies measured self-reported pain intensity (n=391), and there was no evidence of a benefit for individuals who received a signal about the start of the procedure compared with those who received a signal about the impending pain: SMD=−0.60 (95% CI, −1.37, 0.16) (Figure, Supplemental Digital Content 1, http://links.lww.com/CJP/A221). However, participants in 1 study24 reported significantly lower self-reported pain intensity than in the other 2 included studies. When data from this study was removed, a significant difference was observed in pain, with participants who received the signal about the impending procedure reporting significantly lower pain as compared with those who received the signal about the impending pain (n=199): SMD=−0.97 (95% CI, −1.26, −0.68). Two studies22,24 examined whether the patient reported that they experienced pain or no pain during the procedure (ie, a score of ≥1 on a numerical rating scale22 or a rating of “no pain” on a verbal response scale24). No difference in whether pain was present or absent was observed based on the type of signal provided (n=290): relative risk=0.29 (95% CI, 0.01, 5.83).
Should Music Distraction be Used During Vaccine Injections in Adults?
Two trials including 156 adults investigated the effect of listening to music as distraction.20,21 Included studies compared listening to preferred music selected from a variety of musical selections on headphones during venous cannulation compared with a control group (no intervention). Music distraction was not associated with lower pain (n=156): SMD=−0.10 (95% CI, −0.48, 0.27), or fear (n=156): SMD=−0.25 (95% CI, −0.61, 0.10), when compared with a control group (Figure, Supplemental Digital Content 2, http://links.lww.com/CJP/A222). There was very low-quality evidence for critically important outcomes of pain and fear (Table, Supplemental Digital Content 2, http://links.lww.com/CJP/A218).
Should Visual Distraction be Used During Vaccine Injections in Adults?
Two trials including 177 adults investigated the effect of using kaleidoscopes as visual forms of distraction.17,21 Included studies compared looking through the eyepiece of a kaleidoscope during a needle procedure (either venous cannulation21 or venipuncture17) to a control group (no intervention). Both studies examined the critically important outcome of pain, with no benefit of visual distraction with a kaleidoscope for pain (n=177): SMD=−0.57 (95% CI, −1.82, 0.68) (Figure, Supplemental Digital Content 3, http://links.lww.com/CJP/A223). There was very low-quality evidence for pain, a critical outcome (Table, Supplemental Digital Content 3, http://links.lww.com/CJP/A219). One study21 also examined the critically important outcome of fear, with no benefit of visual distraction with a kaleidoscope (n=81): SMD=−0.05 (95% CI, −0.50, 0.40), also with very low quality of evidence.
Should Breathing Interventions (Cough, Breath-Hold) be Used During Vaccine Injections in Adults?
Two trial including 138 adults compared breathing interventions to a control group (no intervention) during venipuncture. This included the “cough trick” (a modification of acupuncture techniques that involves coughing twice, without moving the arms, with the venous cannulation being performed on the second cough23) and the Valsalva maneuver (a deep inhale, followed by a forceful holding of the breath during which the venous cannulation insertion occurs18). Less pain was observed for the breathing interventions: SMD=−0.82 (95% CI, −1.21, −0.43) (Figure, Supplemental Digital Content 4, http://links.lww.com/CJP/A224). The quality of the evidence was very low (Table, Supplemental Digital Content 4, http://links.lww.com/CJP/A220).
DISCUSSION
This systematic review was undertaken to determine the effectiveness of simple psychological interventions that can be employed to reduce pain and fear related to vaccine injections in adults. As the literature review did not identify any studies on simple psychological interventions for adults undergoing vaccinations, our synthesis included indirect evidence from other common needle procedures (ie, venipuncture or venous cannulation). There was some evidence for the use of breathing interventions (cough trick, Valsalva maneuver) for reducing pain during venipuncture. There was evidence of an effect of signaling about the procedure (without reference to pain or discomfort) as compared with signaling about the impending pain in studies where participants reported higher levels of pain. There was no evidence for music or visual distraction.
Although the studies examining breathing interventions suggested that the interventions may have provided a distraction to participants while the needle procedure was being completed, physiological mechanisms for treatment benefit are also possible. Usichenko et al23 suggested that the increased pressure in the subarachnoidal space induced by coughing may activate pain inhibition pathways. Basanranoglu et al18 provided a similar physiological explanation for the efficacy of the Valsalva maneuver, describing that the action stimulates the vagus nerve, which is involved in the modulation of the pain experience. The impact of breathing interventions on reducing adult procedural pain was observed across both types of breathing interventions, and despite differences in population and methodology in both studies: one study was a cross-over study comprised of only men and using the cough trick,23 whereas the other study was parallel comprised of only women comparing the Valsalva maneuver to a no-treatment control group.18 Overall, the mechanisms of treatment benefit from these breathing interventions remain unclear. These results differ to those found in the companion review of psychological interventions for vaccination pain management in children,10 which found no benefit of coughing for pain. The study of children identified numerous barriers to the implementation of the cough trick in the clinical setting (eg, children refusing to cough to delay the injection), which may have accounted for some of the differences between the findings for adults and children.33 As these findings are limited to only 2 trials, and support the efficacy of this intervention, additional trials of these breathing interventions for the adult vaccination setting is warranted.
Given the documented impact of health care provider and caregiver verbalizations on anxiety and pain experienced by adults and children during painful medical procedures,34,35 examining how health providers interact with patients during painful procedures is of great importance. When all 3 studies were combined in the meta-analysis, no effect of signal type on pain was observed, however, when 1 study which had participants with significantly lower pain scores was removed, signaling about the start of the procedure was associated with significantly lower pain scores than signaling about the impending pain. This suggests that this intervention may be more important for those who report higher levels of pain. Of note, there was wide variability in verbal instructions provided to participants across the 3 included studies. Although each study involved a condition in which participants were signaled about the impending procedure and a condition in which participants were signaled about the impending pain, they differed on a number of potentially important characteristics, including language of delivery (English, German), the extent to which the instructions drew attention to nonpain physical sensations in the arm, and the exact words used to describe the impending pain and procedure (eg, “scratch” and “sting” describe different physical sensations; “beware” may signal threat, while “ready” may convey a sense of control; each of these words perhaps evoking different expectancies which may influence the pain response36–38). In addition, previous research in children has suggested that vocal tone may impact the interpretation of statements provided during a painful procedure.35 Future research may benefit from examining not only the content of the statements provided to adults before needle procedures, but also the tone and quality in which the statements are delivered. Increasing the threat value of pain through the use of pain-related threatening words and descriptions increases catastrophizing and decreases tolerance of pain,39,40 and may reduce the efficacy of other interventions, such as distraction.41–44 Overall, given the variability in the included studies, and the experimental evidence that verbal statements can decrease pain, more research into this intervention is clearly needed.
The evidence was insufficient to support the use of music or visual distraction (ie, looking through a kaleidoscope) for the management of procedural pain and fear in adults. Distraction has been hypothesized to relieve procedural pain by actively drawing the patient’s finite attentional resources away from the pain,45 with music in particular being described as having the added benefit of inducing different emotional states.46 Although distraction has consistently been shown to reduce pain and distress during childhood vaccination,5,10 the use of distraction with adults has been a controversial subject in health psychology.47 A Cochrane review of the use of music for pain management has described the effects of music as being so small that they should not be a first-line choice of treatment, with music showing no effect on procedural pain.48 The results of the present review reflect previous findings in adult populations suggesting that distraction is not effective for the relief of procedural pain. In particular, findings of the present study are in line with what was reported in a head-to-head trial by Taddio et al,27 where it was found that self-directed distraction was less effective than liposomal lidocaine, providing support for the generalizability of the present finding to a vaccination context.
Previous research investigating the use of distraction in adult oncology patients described that some patients reported that they found the distraction interventions bothersome and intrusive in their attempts to attend to the procedure being performed.49 Individual differences, such as the desire to attend or not attend to a medical procedure, may impact an individual’s ability to engage with a distraction.50 As the studies involved in the present review did not measure engagement of the individual with the distractor, it is difficult to draw any conclusions regarding how effectively the distractor managed to capture the attention of the participants.51 This is an important area for future research and may inform treatment-tailoring efforts to maximize benefit to individuals.
A major limitation of the findings from this knowledge synthesis is that none of the included trials specifically examined vaccinations. As no studies involving vaccination were eligible for inclusion, related procedures, contexts (eg, venipuncture), or both were examined instead. There are numerous factors that differentiate the vaccination context from other needle procedures, which should be taken into consideration when extrapolating results to the vaccination setting. The lack of empirical evaluation of psychological interventions for vaccination pain in adults may reflect the belief that adults should be capable of coping with commonly experienced injections without the need for intervention. In addition, the present review only focused on simple psychological interventions, to prioritize interventions that are feasible, as well as time and cost efficient, to implement. However, for adults who require frequent needle procedures or who experience greater needle anxiety, more complex and longer interventions such as functional relaxation,25 or exposure-based interventions (also McMurtry CM, Taddio A, Noel M, et al., unpublished data, 2015),11 may be warranted. No research to date has synthesized the literature on complex psychological interventions for needle pain management.
The risk of bias was high for all included trials; in all cases blinding of participants or personnel was not performed, and blinding of outcome assessment was rarely employed. In addition, there was considerable heterogeneity in the included studies with regards to population and methodology. For example, several studies included successful and nonsuccessful procedures,20,21 whereas others only included successful first attempts.17,18,23,24 Many studies excluded participants if there were any factors involved that would make the needle procedure more difficult or painful than usual (eg, participants with a history of difficult venous access19), which limits the generalizability of the present findings to populations that may be at higher risk of experiencing pain during vaccination. With regards to the clinical relevance of the present research, it is important to also consider the role that fear may have in the efficacy and patient’s ability to engage in psychological interventions for needle pain, given the high prevalence of needle fears in the general population (also McMurtry CM, Taddio A, Noel M, et al., unpublished data, 2015).11,52 It is possible that individuals who agreed to participate in research involving needle procedures, particularly in those studies that involved healthy volunteers, may have a particularly low level of needle-related fear. In addition, some samples excluded individuals who reported fear of pain or blood draws,22 or participants who were crying or showing other overt signs of distress at the time of the procedure,17 which reduced the likelihood that individuals with higher needle fears would have been captured in the populations of the present review. This is of particular relevance given that needle fears are common in adults.3 The level of needle fear should be considered when determining the appropriateness of an intervention, as individuals with higher pain-related fear have demonstrated an attentional bias toward pain-related stimuli and as such may be more attuned to the specific language used by providers before the procedure.53 In addition, previous research has found that individuals with high pain-related fear benefit less from distraction, and may in fact derive greater benefit from a sensory-focused intervention instead.42
The present review only examined simple psychological interventions. This resulted in a synthesis of data that is relevant for health care providers that perform needle procedures (ie, the information is clinically relevant), and describes the efficacy of interventions that are time and cost effective to deliver. A rigorous approach to the analysis was used, guided by both GRADE and Cochrane methodologies. Other aspects of the methodological approach used in this systematic review14 and other related systematic reviews in this series are reviewed separately, as are limitations and future directions of this larger body of work by the HELPinKids&Adults Team.54 In light of current concerns about vaccine hesitancy across the lifespan,55 our review identifies a considerable need for future empirical work in the area of psychological interventions for procedure pain management in adults.
In conclusion, there is support for the use of breathing interventions for reducing pain during adult venipuncture and venous cannulation. There is evidence for providing a signal about the impending procedure for individuals who report experiencing higher levels of pain. There is no evidence of a benefit of music or visual distraction. This paper makes an important contribution as it provides the first synthesis of available evidence on psychological interventions for use with adults undergoing needle procedures. Our review provides insight into developmental differences in efficacy of these interventions relative to adolescents and children. More research is needed to explore the role of psychological interventions for vaccine pain management in adults.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank Dr Jennifer A. Parker, PhD, Research Associate, Centre for Pediatric Pain Research, IWK Health Centre; Adjunct Professor, Department of Pediatrics, Dalhousie University, Halifax, Nova Scotia for her contributions to this work.
Footnotes
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website, www.clinicalpain.com.
HELPinKids&Adults (Help ELiminate Pain in Kids and Adults) Team: MacDonald N. E., Rogers J., Bucci L., Mousmanis P., Lang E., Halperin S. A., Bowles S., Halpert C., Ipp M., Asmundson G. J. G., Rieder M., Robson K., Uleryk E., Antony M. M., Dubey V., Hanrahan A., Lockett D., Scott J., Votta Bleeker E.
Supported by the Canadian Institutes of Health Research (CIHR), Ottawa, ON, Canada (KRS 132031). Open access funding was provided by the Mayday Fund in the United States. K.E.B. was supported by a doctoral award from the Canadian Institutes of Health Research, Ottawa, ON, Canada during the completion of this project. K.A.B. was supported by a Vanier Canada Graduate Scholarship. C.T.C. was funded by a Canada Research Chair and by the CIHR during the completion of this work. K.E.B., K.A.B., and M.N. are trainee members of Pain in Child Health (PICH): a strategic training initiative funded by CIHR. A.T. declares a grant from Pfizer, and study supplies from Natus and Ferndale. C.T.C. declares consultation fees from Abbvie. E. Lang is a member of the GRADE working group and declares consultation fees from the International Liaison Committee on Resuscitation (ILCOR). L. Bucci declares a relationship with government agencies and grants from Merck, GSK, Novartis, Sanofi, and Pfizer. S.A. Halperin declares grants from GSK, Sanofi, Novartis, Pfizer, Merck, PREVENT, ImmunoVaccine, NovaVax, Janssen, and Folia. The remaining authors declare no conflict of interest.
Contributor Information
Collaborators: HELPinKids&Adults Team
REFERENCES
- 1.Taddio A, Appleton M, Bortolussi R, et al. Reducing the pain of childhood vaccination: an evidence-based clinical practice guideline (summary). CMAJ. 2010;182:1989–1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dalley JS, McMurtry CM, Creary P. Pain tolerance of parents and children during needle procedures. Pain Res Manag. 2014;19:e69. [Google Scholar]
- 3.Taddio A, Ipp M, Thivakaran S, et al. Survey of the prevalence of immunization non-compliance due to needle fears in children and adults. Vaccine. 2012;30:4807–4812. [DOI] [PubMed] [Google Scholar]
- 4.Chambers CT, Taddio A, Uman LS, et al. Psychological interventions for reducing pain and distress during routine childhood immunizations: a systematic review. Clin Ther. 2009;31:S77–S103. [DOI] [PubMed] [Google Scholar]
- 5.Uman LS, Birnie KA, Noel M, et al. Psychological interventions for needle-related procedural pain and distress in children and adolescents. Cochrane Database Syst Rev. 2013;10:CD005179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Birnie KA, Noel M, Parker JA, et al. Systematic review and meta-analysis of distraction and hypnosis for needle-related pain and distress in children and adolescents. J Pediatr Psychol. 2014;39:783–808. doi: 10.1093/jpepsy/jsu029. [DOI] [PMC free article] [PubMed]
- 7.Zimmer-Gembeck MJ, Skinner EA. Review: the development of coping across childhood and adolescence: an integrative review and critique of research. Int J Behav Dev. 2011;35:1–17. [Google Scholar]
- 8.Taddio A, Shah V, McMurtry CM, et al. Procedural and physical interventions for vaccine injections: systematic review of randomized controlled trials and quasi-randomized controlled trials. Clin J Pain. 2015;31(10S):S20–S37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pillai Riddell R, Taddio A, McMurtry CM, et al. Psychological interventions for vaccine injections in young children 0 to 3 years: systematic review of randomized controlled trials and quasi-randomized controlled trials. Clin J Pain. 2015;31(10S):S64–S71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Birnie KA, Chambers CT, Taddio A, et al. Psychological interventions for vaccine injections in children and adolescents: systematic review of randomized controlled trials and quasi-randomized controlled trials. Clin J Pain. 2015;31(10S):S72–S89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McMurtry CM, Noel M, Taddio A, et al. Interventions for individuals with high levels of needle fear: systematic review of randomized controlled trials and quasi-randomized controlled trials. Clin J Pain. 2015;31(10S):S109–S123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shah V, Taddio A, McMurtry CM, et al. Pharmacological and combined interventions to reduce vaccine injection pain in children and adults: systematic review and meta-analysis. Clin J Pain. 2015;31(10S):S38–S63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pillai Riddel R, Taddio A, McMurtry CM, et al. Process interventions for vaccine injections: systematic review of randomized controlled trials and quasi-randomized controlled trials. Clin J Pain. 2015;31(10S):S99–S108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taddio A, McMurtry CM, Shah V, et al. Methodology for knowledge synthesis of the management of vaccination pain and needle fear. Clin J Pain. 2015;31(10S):S12–S19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guyatt GH, Oxman AD, Schünemann HJ, et al. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011;64:380–382. [DOI] [PubMed] [Google Scholar]
- 16.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration, 2011.
- 17.Cason CL, Grissom NL. Ameliorating adults’ acute pain during phlebotomy with a distraction intervention. Appl Nurs Res. 1997;10:168–173. [DOI] [PubMed] [Google Scholar]
- 18.Basaranoglu G, Basaranoglu M, Erden V, et al. The effects of Valsalva manoeuvres on venipuncture pain. Eur J Anaesthesiol. 2006;23:591–593. [DOI] [PubMed] [Google Scholar]
- 19.Dutt-Gupta J, Brown T, Cyna AM. Effect of communication on pain during intravenous cannulation: a randomized controlled trial. Br J Anaesth. 2007;99:871–875. [DOI] [PubMed] [Google Scholar]
- 20.Jacobson AF. Intradermal normal saline solution, self-selected music, and insertion difficulty effects on intravenous insertion pain. Heart Lung. 1999;28:114–122. [DOI] [PubMed] [Google Scholar]
- 21.Jacobson AF. Cognitive-behavioral interventions for IV insertion pain. AORN J. 2006;84:1031–1048. [DOI] [PubMed] [Google Scholar]
- 22.Ott J, Aust S, Nouri K, et al. An everyday phrase may harm your patients: the influence of negative words on pain during venous blood sampling. Clin J Pain. 2012;28:324–328. [DOI] [PubMed] [Google Scholar]
- 23.Usichenko TI, Pavlovic D, Foellner S, et al. Reducing venipuncture pain by a cought trick: a randomized crossover volunteer study. Anesth Analg. 2004;98:343–345. [DOI] [PubMed] [Google Scholar]
- 24.Vijayan R, Scott G, Brownlie W, et al. How sharp is a “sharp scratch”? A mixed methods study of verbal warnings issued before venipuncture. Pain Pract. 2015;15:132–139. [DOI] [PubMed] [Google Scholar]
- 25.McWhorter LG, Gil-Rivas V. The effect of brief functional relaxation on college students’ needle anxiety during injected vaccinations. J Am Col Health. 2014;62:166–172. [DOI] [PubMed] [Google Scholar]
- 26.Suren M, Kaya Z, Ozkan F, et al. Comparison of the use of the Valsalva maneuver and the eutectic mixture of local anesthestics (EMLA[1]) to relieve venipuncture pain: a randomized controlled trial. J Anesth. 2013;27:407–411. [DOI] [PubMed] [Google Scholar]
- 27.Taddio A, Lord A, Hogan M, et al. A randomized controlled trial of analgesia during vaccination in adults. Vaccine. 2010;28:5365–5369. [DOI] [PubMed] [Google Scholar]
- 28.Agarwal A, Yadav G, Gupta D, et al. The role of a flash of light for attenuation of venous cannulation pain: a prospective, randomized, placebo-controlled study. Anesth Analg. 2008;106:814–816. [DOI] [PubMed] [Google Scholar]
- 29.Agarwal A, Sinha PK, Tandon M, et al. Evaluating the efficacy of the Valsalva maneuver on venous cannulation pain: a prospective, randomized study. Anesth Analg. 2005;101:1230–1232. [DOI] [PubMed] [Google Scholar]
- 30.Levitt FC, Ziemba-Davis M. An exploratory study of patient preferences for pain management during intravenous insertion: maybe we should sweat the small stuff. J Perianesth Nurs. 2013;28:223–232. [DOI] [PubMed] [Google Scholar]
- 31.Hogan M, Kikuta A, Taddio A. A systematic review of measures for reducing injection pain during adult immunization. Vaccine. 2010;28:1514–1521. [DOI] [PubMed] [Google Scholar]
- 32.Vijayan R, Scott G, Brownlie W. Out of sight, but not out of mind? Greater reported pain in patients who spontaneously look away during venipuncture. Eur J Pain. 2015;19:97–102. [DOI] [PubMed] [Google Scholar]
- 33.Wallace DP, Allen KD, Lacroix AE, et al. The “cough trick”: a brief strategy to manage pediatric pain from immunization injections. Pediatrics. 2010;125:e367–e373. [DOI] [PubMed] [Google Scholar]
- 34.Lang EV, Hatsiopoulou O, Koch T, et al. Can words hurt? Patient-provider interactions during invasive procedures. Pain. 2005;114:303–309. [DOI] [PubMed] [Google Scholar]
- 35.McMurtry CM, Chambers CT, McGrath PJ, et al. When “don’t worry” communicates fear: children’s perceptions of parental reassurance and distraction during a painful medical procedure. Pain. 2010;150:52–58. [DOI] [PubMed] [Google Scholar]
- 36.Koyama T, McHaffie JG, Laurienti PJ, et al. The subjective experience of pain: where expectations become reality. Proc Natl Acad Sci USA. 2005;102:12950–12955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Atlas LY, Wager TD. How expectations shape pain. Neurosci Lett. 2012;520:140–148. [DOI] [PubMed] [Google Scholar]
- 38.Goffaux P, Redmond WJ, Rainville P, et al. Descending analgesia—when the spine echoes what the brain expects. Pain. 2007;130:137–143. [DOI] [PubMed] [Google Scholar]
- 39.Jackson T, Pope L, Nagasaka T, et al. The impact of threatening information about pain on coping and pain tolerance. Br J Health Psychol. 2005;10:441–451. [DOI] [PubMed] [Google Scholar]
- 40.Friedman H, Thompson RB, Rosen EF. Perceived threat as a major factor in tolerance for experimentally induced cold-water pain. J Abnorm Psychol. 1985;94:624–629. [DOI] [PubMed] [Google Scholar]
- 41.Eccleston C, Crombez G. Pain demands attention: a cognitive-affective model of the interruptive function of pain. Psychol Bull. 1999;125:356–366. [DOI] [PubMed] [Google Scholar]
- 42.Roelofs J, Peters ML, van der Zijden M, et al. Does fear of pain moderate the effects of sensory focusing and distraction on cold pressor pain in pain-free individuals? J Pain. 2004;5:250–256. [DOI] [PubMed] [Google Scholar]
- 43.Verhoeven K, Goubert L, Jaaniste T, et al. Pain catastrophizing influences the use and the effectiveness of distraction in school children. Eur J Pain. 2012;16:256–267. [DOI] [PubMed] [Google Scholar]
- 44.Van Damme S, Crombez G, Van Nieuwenborgh-De Wever K, et al. Is distraction less effective when pain is threatening? An experimental investigation with the cold pressor task. Eur J Pain. 2008;12:60–67. [DOI] [PubMed] [Google Scholar]
- 45.Johnson MH, Breakwell G, Douglas W, et al. The effects of imagery and sensory detection distractors on different measures of pain: how does distraction work? Br J Clin Psychol. 1998;37:141–154. [DOI] [PubMed] [Google Scholar]
- 46.Brown CJ, Chen ACN, Dworkin SF. Music in the control of human pain. Music Ther. 1989;8:47–60. [Google Scholar]
- 47.Leventhal H. I know distraction works even though it doesn’t!. Health Psychol. 1992;11:208–209. [DOI] [PubMed] [Google Scholar]
- 48.Cepeda MS, Carr DB, Lau J, et al. Music for pain relief. Cochrane Database Syst Rev. 2006;19:CD004843. [DOI] [PubMed] [Google Scholar]
- 49.Kwekkeboom K. Music versus distraction for procedural pain and anxiety in patients with cancer. Oncol Nurs Forum. 2003;30:433–440. [DOI] [PubMed] [Google Scholar]
- 50.Miller SM, Fang CY, Diefenbach MA, et al. Baum A, Andersen BL. Tailoring psychosocial interventions to the individual’s health-information processing style: the influence of monitoring versus blunting in cancer risk and disease. Psychosocial Interventions for Cancer. Washington, DC: American Psychological Association; 2001:343–362. [Google Scholar]
- 51.Eccleston C. The attentional control of pain: methodological and theoretical concerns. Pain. 1995;63:63–3-10. [DOI] [PubMed] [Google Scholar]
- 52.McMurtry CM, Pillai Riddell R, Taddio A, et al. Far from “just a poke”: common painful needle procedures and the development of needle fear. Clin J Pain. 2015;31(10S):S3–S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Keogh E, Ellery D, Hunt C, et al. Selective attentional bias for pain-related stimuli amongst pain fearful individuals. Pain. 2001;91:91–100. [DOI] [PubMed] [Google Scholar]
- 54.Noel M, Taddio A, McMurtry CM, et al. HELPinKids&Adults knowledge synthesis of the management or vaccination pain and high levels of needle fear: limitations of the evidence and recommendations for future research. Clin J Pain. 2015;31(10S):S124–S131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dubé E, Vivion M, MacDonald NE. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: influence, impact and implications. Expert Rev Vaccines. 2015;14:99–117. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


