Supplemental Digital Content is available in the text.
Key Words: fear, phobia, needle, blood-injection-injury, exposure, applied tension
Abstract
Background:
This systematic review evaluated the effectiveness of exposure-based psychological and physical interventions for the management of high levels of needle fear and/or phobia and fainting in children and adults.
Design/Methods:
A systematic review identified relevant randomized and quasi-randomized controlled trials of children, adults, or both with high levels of needle fear, including phobia (if not available, then populations with other specific phobias were included). Critically important outcomes were self-reported fear specific to the feared situation and stimulus (psychological interventions) or fainting (applied muscle tension). Data were pooled using standardized mean difference (SMD) or relative risk with 95% confidence intervals.
Results:
The systematic review included 11 trials. In vivo exposure-based therapy for children 7 years and above showed benefit on specific fear (n=234; SMD: −1.71 [95% CI: −2.72, −0.7]). In vivo exposure-based therapy with adults reduced fear of needles posttreatment (n=20; SMD: −1.09 [−2.04, −0.14]) but not at 1-year follow-up (n=20; SMD: −0.28 [−1.16, 0.6]). Compared with single session, a benefit was observed for multiple sessions of exposure-based therapy posttreatment (n=93; SMD: −0.66 [−1.08, −0.24]) but not after 1 year (n=83; SMD: −0.37 [−0.87, 0.13]). Non in vivo e.g., imaginal exposure-based therapy in children reduced specific fear posttreatment (n=41; SMD: −0.88 [−1.7, −0.05]) and at 3 months (n=24; SMD: −0.89 [−1.73, −0.04]). Non in vivo exposure-based therapy for adults showed benefit on specific fear (n=68; SMD: −0.62 [−1.11, −0.14]) but not procedural fear (n=17; SMD: 0.18 [−0.87, 1.23]). Applied tension showed benefit on fainting posttreatment (n=20; SMD: −1.16 [−2.12, −0.19]) and after 1 year (n=20; SMD: −0.97 [−1.91, −0.03]) compared with exposure alone.
Conclusions:
Exposure-based psychological interventions and applied muscle tension show evidence of benefit in the reduction of fear in pediatric and adult populations.
Needle procedures are highly prevalent in childhood but occur with high frequency across the lifespan in both healthy individuals and those with chronic illnesses. At approximately 12 billion injections per year, vaccinations are the most common painful procedure worldwide.1 Fear of needles is also common in children and adults and can result in a host of deleterious consequences, including vaccination noncompliance and avoidance of health care.2–15 Needle fears are a known contributor to vaccine hesitancy,12 which is a pressing public health concern worldwide.16 Therefore, effective management of needle fears has important implications for improving global public health.
Fear of needles exists on a continuum ranging from none or very little to severe needle fears that cause significant distress and impairment (eg, noncompliance with medical care resulting in adverse health outcomes). Individuals who have been diagnosed with blood-injection-injury phobia (ie, the type of specific phobia that needle phobia falls within in the Diagnostic and Statistical Manual of Mental Disorders—5th Edition17) are at the severe end of the needle fear spectrum. The lifetime prevalence of blood-injection-injury phobia is approximately 3% to 4.5%.3,18,19 The prevalence rises when individuals who have a high degree of needle fear, but not a diagnosis of needle-related phobia, are considered (estimated at approximately 10% of the population).4–6,12 It is important to note that individuals who have not been diagnosed with a needle phobia or who would be considered below the diagnostic threshold for the disorder are nevertheless at increased risk for adverse outcomes. Indeed, they may have sufficiently elevated levels of anxiety and fear about needles that lead to the avoidance of procedures entirely, their responses interfere with clinicians’ ability to carry out procedures (eg, due to fainting, flailing, attempts to escape), or their fear impedes the efficacy of traditional interventions for procedural pain.12,15,20 Individuals with high levels of needle fear who also have chronic health conditions requiring injections (eg, diabetes) are a particularly vulnerable group who require treatment of their fear to maximize adherence to their medical regimen and avoid negative health effects.6,15,21,22
In 2010, a multidisciplinary team from across Canada published a clinical practice guideline on the management of vaccination pain in infants and children.23 In 2013, HELPinKIDS 2.0 (herein, HELPinKids&Adults) was launched to address stakeholders’ interest in an update of the knowledge synthesis to: (1) include trials that had been published after 2010; (2) broaden the scope to include adults; and (3) provide guidance on the management of high levels of needle fear. It was recognized by this team that individuals with a high degree of needle fear present a significant challenge to front line immunizers and that traditional vaccination pain management strategies were not appropriate for this particularly vulnerable population.
Interventions that hold particular promise for reducing needle fears, as well as associated responses such as fainting, in this highly fearful or phobic group of individuals are exposure and applied tension (ie, muscle tension+exposure). Exposure is a psychological intervention that is considered an efficacious treatment for specific phobias in general24–27 and may be delivered in various formats (eg, in vivo, imaginal, single session, multiple session). Exposure-based therapy involves a hierarchical presentation of the feared stimulus. For needle procedures, aspects of needle procedures would be encountered in a hierarchical manner of ascending fear (eg, sitting in the waiting room, to seeing a syringe without a needle, to seeing a syringe with a needle, to holding a syringe with a needle, to holding the tip of a needle against one’s arm, and culminating in receipt of an injection). Exposure-based therapy also frequently includes instruction, participant modeling, and targeting of catastrophic thoughts (ie, cognitive distortions or thinking errors, such as magnifying the threat of the needle) made by the individual. The exposure must be of a sufficient duration that the individual’s fear decreases, he or she realizes the “catastrophe” did not occur, or that he or she can survive it (tests the catastrophic belief).28
Although phobias are often considered as a homogenous group, this may be an oversimplification and obscure important differences with implications for treatment, particularly for fear relating to needles. For example, individuals with high levels of needle fear or blood-injection-injury phobia have an increased risk of showing a vasovagal response (fainting) when confronting the feared situation3,5,10,11,29; indeed, this response is not seen in other specific phobias. The vasovagal response is typically described as diphasic (but see Ritz et al30); specifically, an increase in blood pressure and heart rate is followed by an overcompensatory, precipitous decrease in blood pressure and heart rate leading to reduced cerebral blood flow and eventual loss of consciousness (fainting). Muscle tension is a physical technique in which individuals are taught to: (1) tense their muscles (eg, abdominal, legs, arms) to raise their blood pressure and combat the vasovagal response; (2) recognize prodromal signs of impending vasovagal syncope (eg, visual disturbances, feeling dizzy, or clammy); and (3) apply the technique when prodromal signs occur.31 Muscle tension becomes “applied tension” when individuals practice the technique while being exposed to the object of their fear (eg, needles). This technique has been recommended to reduce fainting during voluntary blood donations32 and has also been investigated within the context of needle fear and fainting.30,33
There are narrative reviews on blood-injury phobia7,13 (as conceptualized in the Diagnostic and Statistical Manual of Mental Disorders-III34), blood-injection-injury phobia6,10,11,14 as well as injection phobia.35 Ayala et al33 published a more recent systematic review focused on the efficacy of applied tension for adults with blood-injection-injury phobia but did not provide a full meta-analysis. The aforementioned reviews also focused almost exclusively on adult populations with 2 exceptions, one of which is a brief commentary,36 whereas the other is a narrative review.14 Although the reviews typically list a variety of treatments that have been utilized for needle fear and needle phobia (eg, exposure, systematic desensitization, modeling, relaxation training, education, reassurance, pharmacological strategies including conscious sedation and anxiolytics, distraction, hypnosis, general cognitive-behavioral strategies, family interventions6,7,10,11,13,14,35), none have provided a systematic review and full meta-analysis of treatments in the context of the quality of the original studies. Furthermore, the management of these fears has never been reviewed in relation to the vaccination context. In sum, given the frequency of needle procedures, the consequences of unmitigated pain and fear,20 and the lack of systematic treatment evaluation, there is a clear and urgent need to systematically synthesize the literature on the treatment of high levels of needle fear, including, but not limited to, needle phobia.
The current systematic review synthesized the evidence for the following exposure-based, behavioral interventions with respect to management of needle fear in children and adults: (1) in vivo exposure (graduated exposure to the actual feared stimulus); (2) multiple versus single sessions of in vivo exposure; and (3) non in vivo exposure (indirect exposure to the feared stimulus using computer-based stimuli or individuals’ imaginations). In addition, applied tension (muscle tension with exposure) versus exposure alone was evaluated for reducing fainting among individuals with high needle fears.
METHODS
The current systematic review is part of a series of reviews using consistent search strategy, data extraction and pooling, and quality assessment processes following both the Grading of Recommendations Assessment, Development and Evaluation (GRADE37) and Cochrane methodologies.38 Details of the overarching methodology are provided elsewhere.39 Briefly, the HELPinKids&Adults Team was brought together to update and expand a previous knowledge synthesis and clinical practice guideline and provide cutting edge guidance on the management of vaccination pain across the lifespan as well as the management of high levels of needle fear. Consistent with the GRADE process, the selection of clinical questions and rating of the importance of outcomes was achieved using a team-based voting approach (described in detail in Taddio et al39). The systematic search strategy was developed by evidence leads under the guidance of a librarian with expertise in systematic reviews. The following databases were searched: EMBASE, Medline, PsycINFO, CINAHL, and ProQuest Dissertations & Theses Global. This broad search strategy yielded a large number of results that were screened for eligibility.39 Articles of potential interest to the current systematic review were then screened again by 2 reviewers (C.M.M. and D.L., a research assistant). Included articles were extracted in full on customized forms by the lead author (C.M.M.) and checked by the second author (M.N.).
The inclusion criteria for the current systematic review were as follows: (1) participants were individuals with a high degree of needle fear or phobia related to needles such as blood-injection-injury phobia or injection phobia (in the absence of data for individuals with needle fear, other specific phobias were accepted) undergoing vaccination or next closest procedure; (2) a randomized or quasi-randomized trial examining exposure-based interventions with at least 5 participants per group; (3) measurement of an outcome of interest; and (4) published report (short or full) or published academic thesis. Of note, the inclusion of individuals with non–needle-related specific phobias (eg, spider) occurred solely for the clinical questions regarding children. The pediatric treatment literature typically collapses across phobia subtypes (this was done in 3 of the 6 included trials; these trials had the largest numbers of participants40–42) and exposure-based treatments have been recommended for specific phobias in general.24,25 The foci of fear of participants of included trials are described within each clinical question.
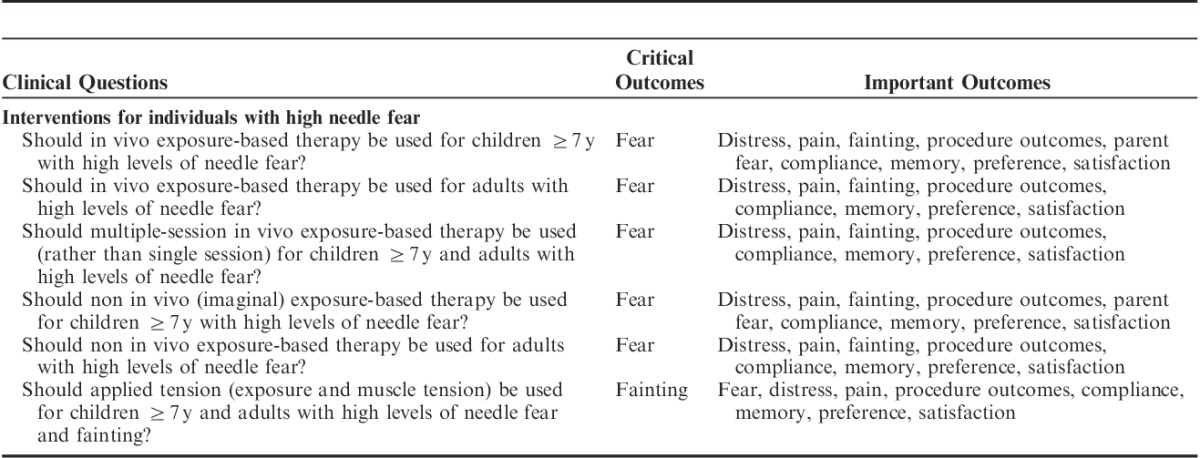
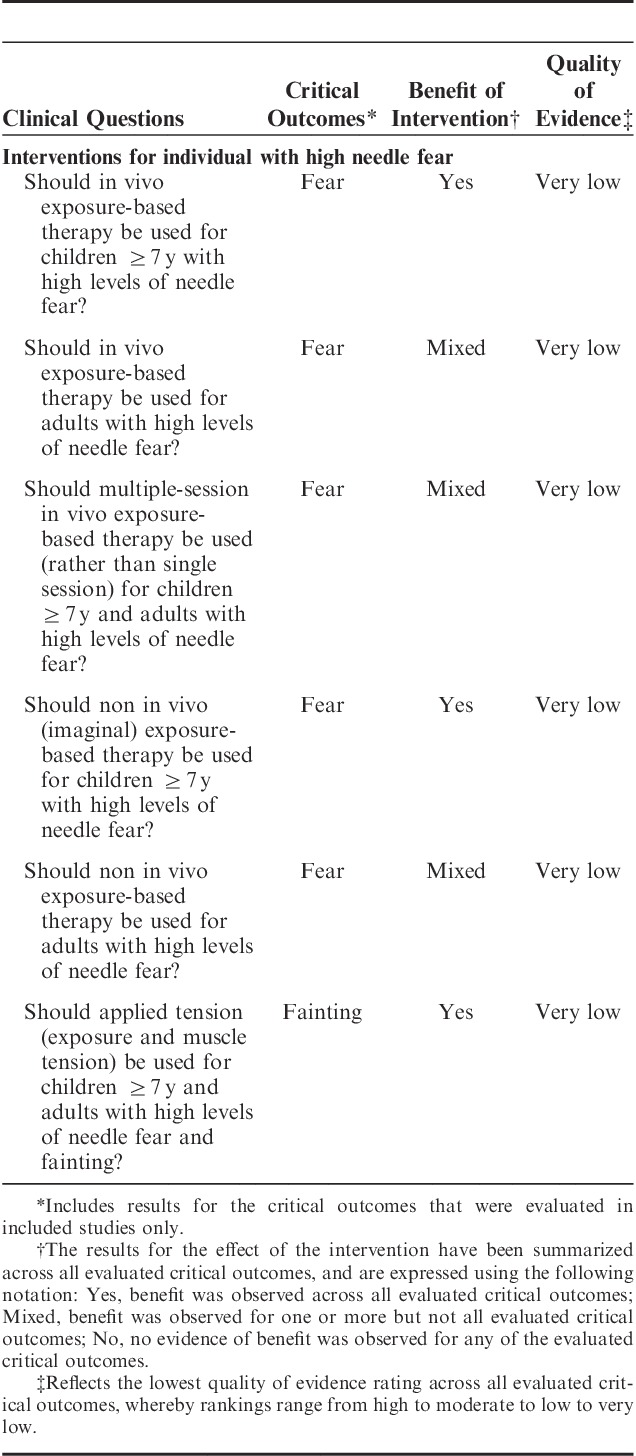
Critical outcomes (as voted upon by the HELPinKids&Adults Team) were specific fear (ie, fear particular to the situation, object, or both that is the focus of the individual’s apprehension; ideally, this would be needle fear but could be, for example, fear of spiders in individuals diagnosed with a phobia of spiders) for the questions relating to exposure therapy and fainting for the remaining question on applied tension. Specific fear was typically measured through multi-item questionnaires or using a rating of acute fear during an imagined or actual engagement with the feared stimulus as part of a behavioral avoidance test (described below). Important outcomes included: general fear (global apprehension regarding a host of situations and objects), compliance, parent fear, pain, distress, procedure outcomes, memory, and preferences. General fear was also measured through multi-item questionnaires. It is important to note that given the targeted nature of exposure-based interventions to the specific feared stimulus, a reduction in general fear is not necessarily expected. A behavioral avoidance test or BAT (also known as a behavioral approach test or task [The term “behavioral avoidance test” was chosen for consistency with Öst’s terminology; his work comprises much of the review.]) was typically used to measure compliance; in a BAT, the individual is asked to complete successive steps or tasks of engagement with the feared stimulus and is scored according to the number or percentage of steps successfully completed. Fainting was measured by observer report of fainting behavior during a BAT. Where possible, analyses were separated by age (children vs. adults). Table 1 presents the included clinical questions as well as critically important and important outcomes included in the review.
TABLE 1.
Clinical Questions and Outcomes
If more than 1 indicator of an outcome was available (eg, 2 or more questionnaires on specific fear), they were combined using established approaches before meta-analysis.43 As part of each article extraction, Cochrane’s risk of bias tool (https://bmg.cochrane.org/assessing-risk-bias-included-studies) was applied on an outcome level. Data were pooled using the RevMan software program (version 5.2, Cochrane Collaboration, Copenhagen, Denmark) using a random effects model; standardized mean difference (SMD) for continuous data or relative risk for dichotomous data along with 95% confidence intervals (CI) were used to assess the effectiveness of an intervention. If data were unavailable in the published paper, efforts were made to contact the authors for more information, or calculations were made from available data on a restricted basis using accepted formulae (eg, means and SDs were calculated from medians and ranges) or estimated from graphs.44 I2 and χ2 tests were used to assess statistical heterogeneity. The GRADE assessment of quality was used to summarize quality across studies using the GRADE profiler software (version 3.6.1); footnotes were used as explanatory aids.
RESULTS
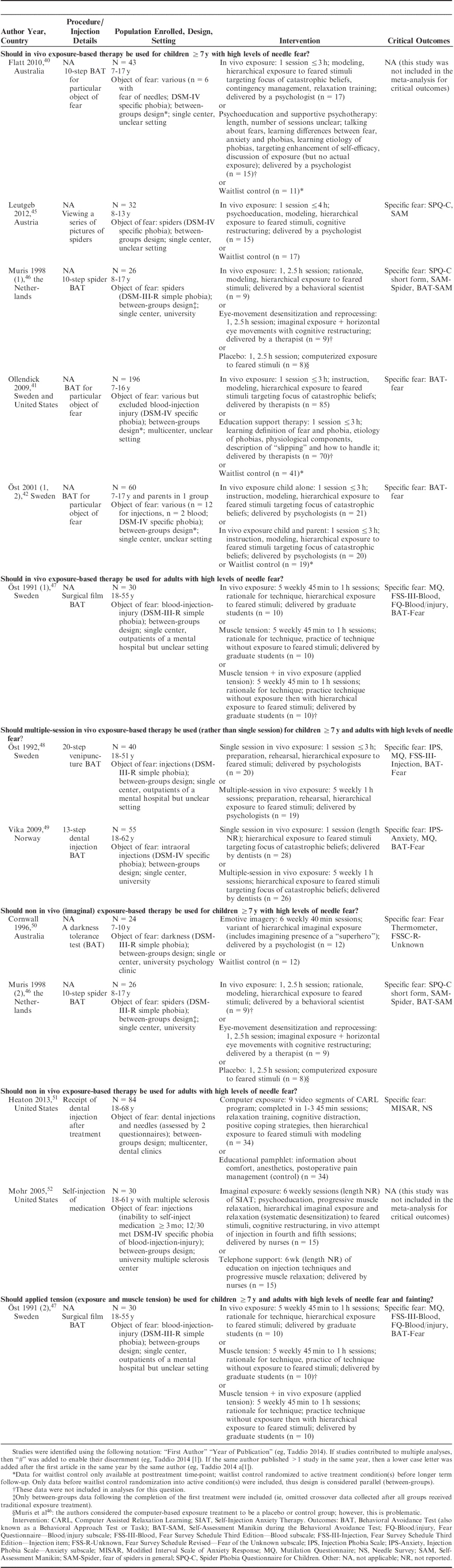
Figure 1 shows the flow of studies from database searching to inclusion in the current review. Eleven studies examining exposure-based treatments were retained for inclusion in the review and are described in Table 2. Six of the included trials focused on children, with the remainder enrolling adults only. One of the trials46 used a crossover design. However, only data from after completion of the first treatment were retained and, as a consequence, the included data represent a parallel, between-groups design. The remaining 10 trials40–42,45,47–52 used a parallel groups design with at least 2 treatment arms; for the 3 trials which used waitlist control groups that received treatment before the long-term follow-up, only data collected before the waitlist control group was randomized to active treatments were included in analyses.40–42
FIGURE 1.
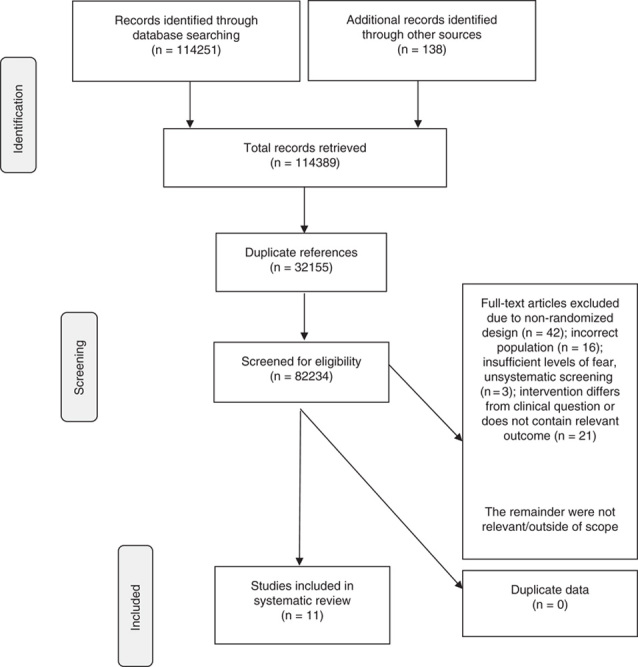
Flow of studies.
TABLE 2.
Characteristics of the Trials Included in the Systematic Review
Notable sources of exclusion were as follows (note that some citations could fall within more than 1 category but for clarity of reporting are described in the most applicable category): (1) nonrandomized design including case studies investigating exposure-based interventions (n=37)21,53–88 or case series (n=5)31,89–92; (2) incorrect population including RCTs with children with nonspecific phobias (n=2; eg, social phobia, agoraphobia)93,94 or adults with general or global dental fear, which is seen as a distinct issue29 (n=2)95,96; (3) incorrect population including muscle tension techniques explored in nonfearful populations (n=3),97–99 as well as a series of studies examining the muscle tension technique in voluntary blood donors (individuals who would volunteer to give blood are seen as unlikely to have high levels of needle fear100; n=9)101–109; (4) insufficient levels of fear, unsystematic screening process, or the potential that the fear was adaptive (ie, presence of a fear of water when it was unclear whether participants knew how to swim; n=3)110–112; and (5) treatment did not match clinical questions, dismantling trials, or no relevant outcomes (n=21).113–133
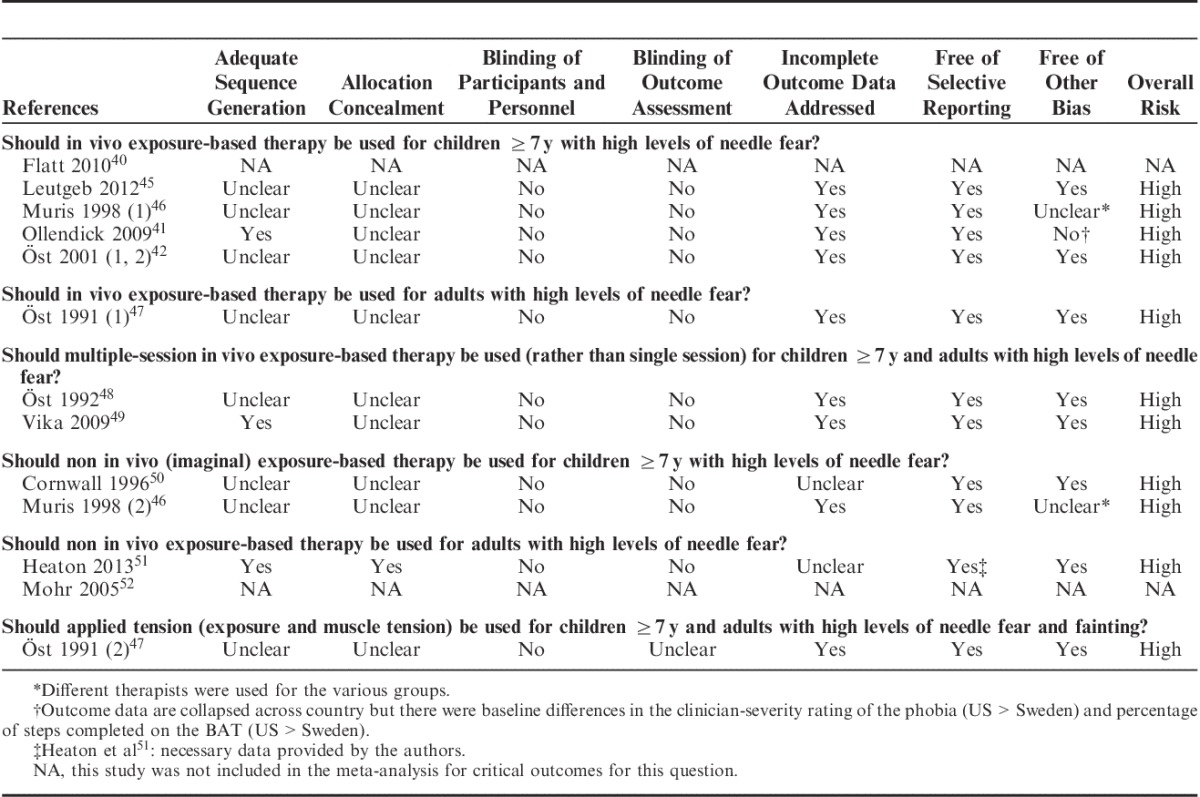
Quality of Studies and Risk of Bias
The risk of bias assessment (Cochrane methodology) for each trial is shown in Table 3. All of the included trials had a high risk of bias, which was primarily due to lack of blinding of participants, personnel, and outcome assessor. Generally, there were also insufficient descriptions of sequence generation and allocation concealment to permit judgment. Other potential sources of bias are noted using footnotes.
TABLE 3.
Assessment of Risk of Bias of Included Trials for Critical Outcomes
Overall Quality of Evidence and Treatment Effects
A quantitative review of the effects of each intervention is provided below, organized by clinical question. Only the results of critical outcomes are reported in text; however, the important outcomes for which data are available are named to guide readers. All results for both critically important and important outcomes are included as Supplemental Digital Content including GRADE Evidence Profiles and Summary of Findings tables (Tables, Supplemental Digital Content 1 to 6, http://links.lww.com/CJP/A225, http://links.lww.com/CJP/A226, http://links.lww.com/CJP/A227, http://links.lww.com/CJP/A228, http://links.lww.com/CJP/A229, http://links.lww.com/CJP/A230) and accompanying Forest plots (Figures, Supplemental Digital Content 7 to 12, http://links.lww.com/CJP/A231, http://links.lww.com/CJP/A232, http://links.lww.com/CJP/A233, http://links.lww.com/CJP/A234, http://links.lww.com/CJP/A235, http://links.lww.com/CJP/A236). It is important to note that no trials were identified that were specific to vaccine injections. Table 4 presents a summary of the findings for critical outcomes.
TABLE 4.
Summary of Results for Critically Important Outcomes
Should In Vivo Exposure-based Therapy be Used for Children 7 Years and Above With High Levels of Needle Fear?
No trials were identified that: (1) examined in vivo exposure-based therapy specifically for children with high levels of needle fear (including blood-injection-injury phobia), or (2) reported results separately for children with needle-related fear. Thus, 5 trials40–42,45,46 with 263 children aged 7 to 17 years meeting diagnostic criteria for a specific phobia according to the edition of the Diagnostic and Statistical Manual of Mental Disorders current at the time of the study were included in the analysis. In Flatt and King,40 6 of 43 participants had a fear of needles, whereas in Öst et al,42 12 of the 60 participants had a fear of injections and 2 had a fear of blood; the remaining participants had a variety of specific phobias including spiders,45,46 enclosed spaces, or animals.41,42 One study41 excluded participants with blood-injection-injury phobia.
Treatment was delivered in a single session ranging between 2.5 and 3 hours in 4 of the studies40–42,46 and 4 hours in the remaining study.45 All the treatments were modeled after Öst’s28 “One session treatment” and included modeling and hierarchical exposure to the feared stimuli; 4 of the trials40–42,45 specified some degree of cognitive restructuring or targeting of the catastrophic cognition. Comparison groups were waitlist control40–42,45 or a “placebo” group of a computerized exposure to spiders.46 In vivo exposure-based therapy demonstrated benefit on specific fear (4 trials; n=235; SMD: −1.71 [95% CI: −2.72, −0.7]) (Table, Supplemental Digital Content 1, http://links.lww.com/CJP/A225 and Figure, Supplemental Digital Content 7, http://links.lww.com/CJP/A231). Important outcomes with data shown in the supplemental digital content (Table, Supplemental Digital Content 1, http://links.lww.com/CJP/A225 and Figure, Supplemental Digital Content 7, http://links.lww.com/CJP/A231) include general fear, compliance (using a BAT), child satisfaction, and parent satisfaction.
Should In Vivo Exposure-based Therapy be Used for Adults With High Levels of Needle Fear?
One trial with 20 adult participants diagnosed with blood-injection-injury phobia (excluding those with only an injection phobia) according to the DSM-III-R134 was included in this analysis.47 Treatment was given in 5 weekly sessions of approximately 45 minutes and included hierarchical exposure to the feared stimuli. The comparison group was trained in muscle tension but did not undergo exposure. In vivo exposure-based therapy showed benefit on specific fear posttreatment (n=20; SMD: −1.09 [−2.04, −0.14]) but not at 1-year follow-up (n=20; SMD: −0.28 [−1.16, 0.6]) (Table, Supplemental Digital Content 2, http://links.lww.com/CJP/A226 and Figure, Supplemental Digital Content 8, http://links.lww.com/CJP/A232). Important outcomes with data shown in the supplemental digital content (Table, Supplemental Digital Content 2, http://links.lww.com/CJP/A226 and Figure, Supplemental Digital Content 8, http://links.lww.com/CJP/A232) include each of the following at posttreatment and 1-year follow-up: general fear, fainting, and compliance (using a BAT).
Should Multiple-session In Vivo Exposure-based Therapy be Used (Rather Than Single Session) for Children 7 Years and Above and Adults With High Levels of Needle Fear?
Two trials with 93 adults who were fearful of injections were included in this analysis comparing multiple and single sessions of in vivo exposure.48,49 Participants met the diagnostic criteria for specific phobia according to the version of the Diagnostic and Statistical Manual of Mental Disorders that was in use at the time of the study. According to study descriptions, both treatments followed Öst’s treatment principles28,42; in vivo exposure consisted of either preparation, rehearsal, hierarchical exposure to feared stimuli,48 or hierarchical exposure to feared stimuli targeting focus of catastrophic beliefs.49 Multiple-session in vivo exposure was given over 5 weekly 1 hour sessions in both trials; the 1 session treatment was maximized to 3 hours in 1 trial48 but the length of time was not reported for the other trial.49 Results were mixed for the critical outcome of specific fear (Table, Supplemental Digital Content 3, http://links.lww.com/CJP/A227 and Figure, Supplemental Digital Content 9, http://links.lww.com/CJP/A233). Multiple-session in vivo exposure-based therapy was superior to single session exposure for the reduction of specific fear measured posttreatment (n=93; SMD: −0.66 [−1.08, −0.24]) but not at 1-year follow-up (n=83; SMD: −0.37 [−0.87, 0.13]). Data for the following important outcomes measured at 2 time-points (posttreatment, 1-year follow-up) are presented in the supplemental digital content (Table, Supplemental Digital Content 3, http://links.lww.com/CJP/A227 and Figure, Supplemental Digital Content 9, http://links.lww.com/CJP/A233): general fear, compliance (using a BAT), and fainting. Compliance with a voluntary blood donation or voluntary dental injection over the 12-month follow-up period is also summarized.
Should Imaginal Exposure-based Therapy be Used for Children 7 Years and Above With High Levels of Needle Fear?
No trials were identified that studied children with a fear of needles or a related phobia. Thus, trials of other specific phobias were sought. Two trials with 41 children aged 7 to 17 years with phobias of spiders or darkness (diagnosed according to the DSM-III-R134) were included in the analysis.46,50 In 1 study,50 children received 6 weekly 40-minute sessions of “emotive imagery” therapy during which they engaged in a variant of imaginal hierarchical exposure in which the child was supported by his or her favorite superhero; the comparator was a waitlist control group. Of note, although the authors describe their intervention as focusing on imaginal exposure, the children were rewarded for initiating in vivo exposure between sessions.50 In the other study,46 children received a single 2.5-hour session of eye-movement desensitization and reprocessing therapy that included imaginal exposure combined with rapid horizontal eye movements and cognitive restructuring; the comparison group was considered a placebo group by the authors but consisted of 2.5 hours of computer-delivered exposure to the feared stimuli ranging in degree of realism (eg, cartoon-like spiders vs. ones that appeared more real). Imaginal exposure-based therapy led to a reduction in specific fear posttreatment (both trials; n=41; SMD: −0.88 [−1.7, −0.05]) and at 3-month follow-up (1 trial50; n=24; SMD: −0.89 [−1.73, −0.04]) (Table, Supplemental Digital Content 4, http://links.lww.com/CJP/A228 and Figure, Supplemental Digital Content 10, http://links.lww.com/CJP/A234). Data for the following important outcomes measured at 2 time-points (posttreatment, 3-month follow-up) are presented in the supplemental digital content (Table, Supplemental Digital Content 4, http://links.lww.com/CJP/A228 and Figure, Supplemental Digital Content 10, http://links.lww.com/CJP/A234): general fear, distress (parent-rated), and compliance (using a BAT).
Should Non In Vivo Exposure-based Therapy be Used for Adults With High Levels of Needle Fear?
Two studies of adults with high levels of fear were included in this analysis.51,52 One study51 included 84 otherwise healthy adults who were highly fearful and avoidant of dental injections and needles (assessed by 2 questionnaires). The other trial52 included 30 adults with multiple sclerosis who were afraid of injections and unable to perform necessary self-injections of their medication for at least 3 months; 12 of the 30 participants met diagnostic criteria for blood-injection-injury phobia according to the DSM-IV.135 In Heaton et al51 participants received computer-delivered exposure through a specialized program designed to be completed in 1 to 3, 45-minute sessions; the content of the program included relaxation training, cognitive distraction, positive coping strategies, and hierarchical exposure with modeling. The comparison group received an educational pamphlet.51 In Mohr et al,52 participants engaged in 6 weekly sessions (length of each session was not reported) involving psychoeducation, progressive muscle relaxation, hierarchical imaginal exposure and relaxation, cognitive restructuring, and in vivo injection attempts in the fourth and fifth sessions. The comparison group received 6 weeks of telephone support, including education on injection techniques and progressive muscle relaxation. Critically important outcomes were only available for Heaton et al.51 Non in vivo exposure reduced specific fear (n=68; SMD: −0.62 [−1.11, −0.14]) but not acute fear during a voluntary injection (n=17; SMD: 0.18 [−0.87, 1.23]) (Table, Supplemental Digital Content 5, http://links.lww.com/CJP/A229 and Figure, Supplemental Digital Content 11, http://links.lww.com/CJP/A235). The supplemental digital content (Table, Supplemental Digital Content 5, http://links.lww.com/CJP/A229 and Figure, Supplemental Digital Content 11, http://links.lww.com/CJP/A235) contains data for the important outcome of compliance measured through voluntary dental injection or self-injection of medication.
Should Applied Tension (Exposure and Muscle Tension) be Used for Children 7 Years and Above and Adults With High Levels of Needle Fear and Fainting?
One trial with adult participants diagnosed with blood-injection-injury phobia (excluding those with only an injection phobia) according to the DSM-III-R134 was included in this analysis.47 Participants received 5 weekly 45 minutes to 1 hour sessions of applied tension (muscle tension+exposure); treatment included outlining the rationale for the technique, practicing muscle tension without and then with (hierarchical) exposure to feared stimuli.47 The comparison group received 5 weekly 45 minutes to 1 hour sessions of in vivo exposure. Thus, this analysis compared 2 active treatments. Applied tension showed benefit on the critical outcome of fainting both posttreatment (n=20; SMD: −1.16 [−2.12, −0.19]) and at 1-year follow-up (n=20; SMD: −0.97 [−1.91, −0.03]) (Table, Supplemental Digital Content 6, http://links.lww.com/CJP/A230 and Figure, Supplemental Digital Content 12, http://links.lww.com/CJP/A236). Data for important outcomes of specific fear, general fear, and compliance at both time-points are presented in the supplemental digital content (Table, Supplemental Digital Content 6, http://links.lww.com/CJP/A230 and Figure, Supplemental Digital Content 12, http://links.lww.com/CJP/A236).
DISCUSSION
This systematic review and meta-analysis is the first to examine the efficacy of exposure-based interventions for the reduction of fear in individuals with high levels of needle fears or phobias across the lifespan. Consideration of this vulnerable population within the context of vaccine injections is critical given their heightened risk for fears and avoidance of medical care over their lifetime2–15,17,29,136 and complements the other systematic reviews on vaccine pain management in this series.137–142
There were no trials examining interventions specific to the vaccination context (which is perhaps not surprising given that these interventions need to take place outside of this context) and limited trials of children with high levels of needle fears or phobias, requiring us to include indirect evidence from nonvaccination and non-needle contexts. To our knowledge, there has been no published systematic examination of high levels of fear with regard to different types of needle procedures. The included trials enrolled participants with elevated fear of a particular situation, object (typically related to needles), or both and utilized interventions that exposed them to their particular fear. Findings suggest that in vivo exposure-based therapy is effective for reducing specific fear in children (7 y and above) and adults. Among adults with high levels of needle fears, there was limited efficacy found for the superiority of delivering in vivo exposure in multiple, shorter sessions (eg, 5×1 h) as compared with 1 relatively long session (eg, 3 h). Non in vivo (imaginal, computer-based) exposure was also found to have benefit on specific fear among children and adults. Finally, among adults, applied tension (exposure+muscle tension) was found to have additive beneficial effects on fainting, over and above exposure alone. Taken together, these findings support the use of these exposure-based interventions for reducing fear and fainting, respectively, among individuals with high levels of needle fears or phobias.
Interestingly, in comparison with single sessions, multiple sessions of in vivo exposure were only more efficacious for reducing specific fear immediately posttreatment but not at 1-year follow-up; these results then provide only limited support for the efficacy of a longer mode of delivery.48,49 Moreover, all of the trials of in vivo exposure in children, which were found to be efficacious for reducing specific fear, were single session.40–42,45,46 Unlike multiple sessions that are typically an hour in length and spread out over several weeks, single sessions often involve several hours (eg, 2.5 to 4 h; Öst’s traditional 1 session treatment is typically maximized to 3 h28) of exposure treatment. This results in the provision of a higher “dose” of treatment at one point in time. It is important to note that even in the single session approach, exposure still progresses in a hierarchical manner. Although there may be individual differences in terms of preferences, readiness, and tolerance for high versus low doses of this treatment, these findings suggest that effective treatment of high needle fears or phobias may need not be time intensive (ie, taking several weeks or even months); in fact, 1 session approaches for the treatment of a variety of specific phobias have increased in popularity over time.143–145 Beyond relative efficiency and feasibility, the utility of 1 session treatment of high levels of needle fear could be particularly high in preparing a fearful individual for required, imminent medical treatment.
The inclusion of physical interventions (applied tension) for the management of fainting in individuals with high levels of needle fears was important given that this response is common in those with an extreme fear of blood and needles (70% and 56%, respectively29). In the vaccination context, fainting is particularly concerning given the potential for injuries as a result of falling.146–149 There may be several mechanisms underlying the efficacy of applied tension, including both physiological (raising blood pressure) and psychological (interoceptive exposure leading to changes in cognitions about the uncontrollability of fainting) mechanisms. The evidence supports the additive benefit of muscle tension in addition to in vivo exposure in adults. Most impressive were the long-term effects found for fainting posttreatment and at 1-year follow-up, which speaks to the robustness of this technique. Although the current findings were based on the single trial that answered the clinical question, extant research also supports the use of applied tension for a reduction in fainting in the context of blood-injection-injury phobia.31,33,116,120 These findings warrant replication in individuals spanning various age groups to determine whether this technique can be developmentally tailored to younger populations.
Overall, there was a striking dearth of research examining interventions for individuals with high levels of needle fears or phobias. We included children and adults with high levels of needle fear and or phobias undergoing vaccination or other needle procedures, followed by the next closest context. We included individuals with a diagnosis of blood-injection-injury phobia or another related phobia (eg, injection phobia) as well as individuals with high levels of needle fear and related functional impairment (eg, being unable to self-inject medicine for their chronic illness management). There were limited trials of blood-injection-injury phobia in adults and no trials in children. In the absence of randomized or quasi-randomized controlled trials on individuals with high levels of needle fears or phobias, we were required to rely on trials of individuals with specific phobias that were unrelated to needles (eg, spider and darkness phobias). Although only occurring for children, this may threaten the generalizability of the current findings to needle contexts. Indeed, individuals with phobias and high levels of fear are not a homogenous group and their response to feared stimuli and intervention are invariably influenced by the specific catastrophic cognitions underlying their fears. In short, extrapolating findings from non–needle-related contexts to the vaccination context is potentially problematic. Nevertheless, this systematic review offers important, new knowledge about effective fear management in this vulnerable group that can be applied to vaccination to guide future research in this area.
Needle phobia has fallen under the diagnostic umbrella of blood-injection-injury phobia and substantial similarities between individuals with phobias of blood and phobias of injections have been documented.29 Nevertheless, given the breadth of the diagnostic category, the specific focus of the fear can be quite diverse across individuals (eg, seeing injuries or mutilation vs. receiving a needle).17 Thus, we were limited in our review by the field’s conceptualization of the phobia. Disgust sensitivity has been implicated in certain specific phobias, including blood-injection-injury phobia.150,151 Blood and injury stimuli (vs. injection) may be more likely to elicit disgust.152 In fact, disgust may emerge due to fears of contamination150,151; thus, the specific focus of fear may be critical (eg, is the individual fearful of the pain, being contaminated by the needle, fainting, or something else?). Only one of the trials (focused on children with spider phobias) included in the current review measured disgust, finding that exposure reduced both fear and disgust.45 It is important to note that even among people who fear needles specifically, the focus of individuals’ fears may differ (eg, they may fear blood, injections, insertion of foreign substance into their bodies, and/or the medical context153). Differences in the focus of fear would be expected to influence ones’ response to particular interventions.
Fears of needles can extend beyond the needle context and follow a chronic course17,29,136; therefore, longitudinal examinations that include the postintervention time period (weeks, months, and years later) are important. Unlike the other reviews in this series, many of the trials of interventions for individuals with high needle fears or phobias included long-term follow-up assessments as well as inclusion of other outcomes deemed to be important by stakeholders invested in vaccination (eg, compliance, fainting, satisfaction). This was a strength of this systematic review. Although immediate outcomes reflect the short-term efficacy of an intervention, the overall utility of an intervention is questionable if findings are not maintained over time. In vivo exposure was found to have effects on immediate posttreatment outcomes; however, less support was found for longer term outcomes (1 y posttreatment). Among children, non in vivo exposure had effects on specific fear that were maintained at 3-month follow-up, and applied tension had effects on fainting that were maintained at 1-year follow-up. This suggests that while some of these interventions have lasting effects, some individuals with high levels of needle fears or phobias may require additional intervention to retain reductions of fear over longer periods of time. The use of booster sessions in cognitive-behavioral treatments for many disorders (eg, anxiety, depression) is well known.154 Booster sessions may be particularly important for individuals with a high level of needle fear who may go relatively long periods without being exposed to a needle procedure.
Pain was not included as an outcome in the included trials (due to the indirectness of the evidence) but has important implications for needle fears and should be included in future research. The relationship between needle pain and fear is likely reciprocal and should be further delineated. An exploration of the likely complex etiology of needle fears is presented elsewhere in this series.20 However, most individuals with high needle fears or phobias can root their fear back to 1 traumatic needle procedure in their past.29,155,156 Early vicarious and instrumental learning processes may make individuals more vulnerable to experiencing and perceiving greater pain during needle procedures.20,157 Conversely, individuals whose pain is poorly managed during needle procedures are more likely to develop increasingly fearful memories of the procedure158 that then places them at risk for experiencing more distress at subsequent needle procedures.159 This can fuel a vicious self-perpetuating cycle of increased needle fear and pain over time.157 Effective pain management may serve to help prevent needle fears from developing. In short, effective management of pain and fear may serve to reduce future fear and pain and hold promise for preventing distress and impairment (eg, noncompliance) over time. Given that concerns about pain and fear are known contributors to vaccine hesitancy,12,16 effective management of both is paramount.
Consideration of the strengths and limitations of this body of work creates clear pathways for future research. High-quality RCTs of exposure-based interventions with individuals with high levels of needle fear are critically needed, for the vaccination context and otherwise. Ideally, these trials should: (1) enroll sufficient numbers of participants in narrow age ranges to adequately capture developmental differences; (2) assess and report fainting history as well as the specific focus of the needle fear (eg, pain from the needle, injection of a foreign substance) both at baseline and in response to treatment; (3) clearly report and connect the target(s) of the exposure with the focus of the needle fear; and (4) continue to gather longitudinal data as well as expanding the outcomes and follow-up time frame if possible (eg, beyond 1 y) with and without booster sessions. Discussion of implementation considerations is beyond the scope of the present paper and the reader is directed to our clinical practice guideline on the management of high levels of needle fear that explores these issues in detail160; however, future research should also be conducted on various delivery methods of these interventions to enhance feasibility and uptake.
In conclusion, we applied a rigorous methodological approach to conduct the first systematic review of exposure-based interventions for the reduction of fear in individuals of all ages with high levels of needle fears or phobias. No trials specifically examined interventions implemented in the vaccination context and trials of individuals with high levels of needle fears or phobias were limited. Support was found for the efficacy of in vivo and non in vivo exposure therapy for reducing specific fear in individuals with high levels of needle fears or phobias. Multiple sessions of in vivo exposure were not clearly superior to single sessions. Applied tension was efficacious for reducing fainting in adults. These findings suggest that these interventions hold promise for reducing vaccine injection fear in individuals who are particularly vulnerable for experiencing fear and avoidance of medical care over time.
Supplementary Material
Footnotes
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website, www.clinicalpain.com.
HELPinKids&Adults (Help ELiminate Pain in Kids&Adults) Team: N.E. MacDonald, J. Rogers, L. Bucci, P. Mousmanis, E. Lang, S.A. Halperin, S. Bowles, C. Halpert, M. Ipp, M. Rieder, K. Robson, E. Uleryk, V. Dubey, A. Hanrahan, D. Lockett, J. Scott, E. Votta Bleeker.
Supported by the Canadian Institutes of Health Research (CIHR), Ottawa, ON, Canada (KRS 132031). Open access funding was provided by the Mayday Fund in the United States. A. Taddio declares a grant from Pfizer, and study supplies from Natus and Ferndale. C.T. Chambers declares consultation fees from Abbvie. E. Lang is a member of the GRADE working group and declares consultation fees from the International Liaison Committee on Resuscitation (ILCOR). L. Bucci declares a relationship with government agencies and grants from Merck, GSK, Novartis, Sanofi, and Pfizer. S.A. Halperin declares grants from GSK, Sanofi, Novartis, Pfizer, Merck, PREVENT, ImmunoVaccine, NovaVax, Janssen, and Folia. The remaining authors declare no conflict of interest.
Contributor Information
Collaborators: HELPinKids&Adults Team
REFERENCES
- 1.Miller MA, Pisani E. The cost of unsafe injections. Bull World Health Organ. 1999;77:808–811. [PMC free article] [PubMed] [Google Scholar]
- 2.Armfield JM, Milgrom P. A clinician guide to patients afraid of dental injections and numbness. SAAD Dig. 2011;27:33–39. [PubMed] [Google Scholar]
- 3.Bienvenu OJ, Eaton WW. The epidemiology of blood-injection-injury phobia. Psychol Med. 1998;28:1129–1136. [DOI] [PubMed] [Google Scholar]
- 4.Cox AC, Fallowfield LJ. After going through chemotherapy I can’t see another needle. Eur J Oncol Nurs. 2007;11:43–48. [DOI] [PubMed] [Google Scholar]
- 5.Deacon B, Abramowitz J. Fear of needles and vasovagal reactions among phlebotomy patients. J Anxiety Disord. 2006;20:946–960. [DOI] [PubMed] [Google Scholar]
- 6.Hamilton JG. Needle phobia: a neglected diagnosis. J Fam Pract. 1995;41:169–175. [PubMed] [Google Scholar]
- 7.Marks I. Blood-injury phobia: a review. Am J Psychiatry. 1988;145:1213. [DOI] [PubMed] [Google Scholar]
- 8.Neale MC, Walters EE, Eaves LJ, et al. Genetics of blood-injury fears and phobias: a population-based twin study. Am J Med Genet. 1994;54:326–334. [DOI] [PubMed] [Google Scholar]
- 9.Oswalt RM, Napoliello M. Motivations of blood donors and nondonors. J Appl Psychol. 1974;59:122–124. [Google Scholar]
- 10.Page AC. Blood-injury phobia. Clin Psychol Rev. 1994;14:443–461. [Google Scholar]
- 11.Sokolowski CJ, Giovannitti JA, Boynes SG. Needle phobia: etiology, adverse consequences, and patient management. Dent Clin North Am. 2010;54:731–744. [DOI] [PubMed] [Google Scholar]
- 12.Taddio A, Ipp M, Thivakaran S, et al. Survey of the prevalence of immunization non-compliance due to needle fears in children and adults. Vaccine. 2012;30:4807–4812. [DOI] [PubMed] [Google Scholar]
- 13.Thyer BA, Himle J, Curtis GC. Blood-injury-illness phobia: a review. J Clin Psych. 1985;41:451–459. [DOI] [PubMed] [Google Scholar]
- 14.Willemsen H, Chowdhury U, Briscall L. Needle phobia in children: a discussion of aetiology and treatment options. Clin Child Psychol Psychiatry. 2002;7:609–619. [Google Scholar]
- 15.Wright S, Yelland M, Heathcote K, et al. Fear of needles: nature and prevalence in general practice. Aust Fam Physician. 2009;38:172–176. [PubMed] [Google Scholar]
- 16.World Health Organization. Report of the SAGE Working Group on vaccine hesitancy. 2015. Available at: http://www.who.int/immunization/sage/meetings/2014/october/SAGE_working_group_revised_report_vaccine_hesitancy.pdf. Accessed April 2, 2015.
- 17.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Publishing; 2013. [Google Scholar]
- 18.LeBeau RT, Glenn D, Liao B, et al. Specific phobia: a review of DSM-IV specific phobia and preliminary recommendations for DSM-V. Depress Anxiety. 2010;27:148–167. [DOI] [PubMed] [Google Scholar]
- 19.Stinson FS, Dawson DA, Chou SP, et al. The epidemiology of DSM-IV specific phobia in the USA: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2007;37:1047–1059. [DOI] [PubMed] [Google Scholar]
- 20.McMurtry CM, Pillai Riddell R, Taddio A, et al. Far from “just a poke”: common painful needle procedures and the development of needle fear. Clin J Pain. 2015;31(10S):S3–S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ellinwood EH, Hamilton JG. Case report of a needle phobia. J Fam Pract. 1991;32:420–422. [PubMed] [Google Scholar]
- 22.Mohr DC, Boudewyn AC, Likosky W, et al. Injectable medication for the treatment of multiple sclerosis: the influence of self-efficacy expectations and injection anxiety on adherence and ability to self-inject. Ann Behav Med. 2001;23:125–132. [DOI] [PubMed] [Google Scholar]
- 23.Taddio A, Appleton M, Bortolussi R, et al. Reducing the pain of childhood vaccination: an evidence-based clinical practice guideline (summary). CMAJ. 2010;182:1989–1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Choy Y, Fyer AJ, Lipsitz JD. Treatment of specific phobia in adults. Clin Psychol Rev. 2007;27:266–286. [DOI] [PubMed] [Google Scholar]
- 25.Wolitzky-Taylor KB, Horowitz JD, Powers MB, et al. Psychological approaches in the treatment of specific phobias: a meta-analysis. Clin Psychol Rev. 2008;28:1021–1037. [DOI] [PubMed] [Google Scholar]
- 26.Hood HK, Antony MM.Davis TEI, Ollendick TH, Öst L-G. Evidence-based assessment and treatment of specific phobias in adults. Intensive One-Session Treatment of Specific Phobias. New York, NY: Springer; 2012:19–42. [Google Scholar]
- 27.Ollendick TH, Davis TEI.Davis TEI, Ollendick TH, Öst L-G. Evidence-based assessment and treatment of specific phobias in children and adolescents. Intensive One-Session Treatment of Specific Phobias. New York, NY: Springer; 2012:43–56. [Google Scholar]
- 28.Öst L-G. One-session treatment for specific phobias. Behav Res Ther. 1989;27:1–7. [DOI] [PubMed] [Google Scholar]
- 29.Öst L-G. Blood and injection phobia: background and cognitive, physiological, and behavioral variables. J Abnorm Psychol. 1992;101:68–74. [DOI] [PubMed] [Google Scholar]
- 30.Ritz T, Meuret AE, Ayala ES. The psychophysiology of blood-injection-injury phobia: looking beyond the diphasic response paradigm. Int J Psychophysiol. 2010;78:50–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Öst L-G, Sterner U. Applied tension: a specific behavioral method for treatment of blood phobia. Behav Res Ther. 1987;25:25–29. [DOI] [PubMed] [Google Scholar]
- 32.Wieling W, France CR, Van Dijk N, et al. Physiologic strategies to prevent fainting responses during or after whole blood donation. Transfusion. 2011;51:2727–2738. [DOI] [PubMed] [Google Scholar]
- 33.Ayala ES, Meuret AE, Ritz T. Treatments for blood-injury-injection phobia: a critical review of current evidence. J Psychiatr Res. 2009;43:1235–1242. [DOI] [PubMed] [Google Scholar]
- 34.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association; 1980. [Google Scholar]
- 35.Patel MX, Baker D, Nosarti C. Injection phobia: a systematic review of psychological treatments. Behav Cogn Psychother. 2005;33:343–349. [Google Scholar]
- 36.Du S, Jaaniste T, Champion GD, et al. Theories of fear acquisition: the development of needle phobia in children. Pediatric Pain Letter. 2008;10:13–17. [Google Scholar]
- 37.Guyatt GH, Oxman AD, Schunemann HJ, et al. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011;64:380–382. [DOI] [PubMed] [Google Scholar]
- 38.Higgins JPT, Green S. eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. [updated September 2011]. The Cochrane Collaboration; 2011. Available at: www.cochranehandbook.org. [Google Scholar]
- 39.Taddio A, McMurtry CM, Shah V, et al. Methodology for knowledge synthesis of the management of vaccination pain and needle fear. Clin J Pain. 2015;31(10S):S12–S19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Flatt N, King N. Brief psycho-social interventions in the treatment of specific childhood phobias: a controlled trial of a 1-year follow-up. Behav Change. 2010;27:130–153. [Google Scholar]
- 41.Ollendick TH, Öst L-G, Reuterskiöld L, et al. One-session treatment of specific phobias in youth: a randomized clinical trial in the United States and Sweden. J Consult Clin Psychol. 2009;77:504–516. [DOI] [PubMed] [Google Scholar]
- 42.Öst L-G, Svensson L, Hellström K, et al. One-session treatment of specific phobias in youths: a randomized clinical trial. J Consult Clin Psychol. 2001;69:814–824. [PubMed] [Google Scholar]
- 43.Borenstein M, Hedges LV, Higgins JPT, et al. Introduction to Meta-analysis. West Sussex, UK: John Wiley & Sons; 2009. [Google Scholar]
- 44.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Leutgeb V, Schäfer A, Köchel A, et al. Exposure therapy leads to enhanced late frontal positivity in 8- to 13-year-old spider phobic girls. Biol Psychol. 2012;90:97–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Muris P, Merckelbach H, Holdrinet I, et al. Treating phobic children: effects of EMDR versus exposure. J Consult Clin Psychol. 1998;66:193–198. [DOI] [PubMed] [Google Scholar]
- 47.Öst L-G, Fellenius J, Sterner U. Applied tension, exposure in vivo, and tension-only in the treatment of blood phobia. Behav Res Ther. 1991;29:561–574. [DOI] [PubMed] [Google Scholar]
- 48.Öst L-G, Hellström K, Kåver A. One versus five sessions of exposure in the treatment of injection phobia. Behav Ther. 1992;23:263–281. [Google Scholar]
- 49.Vika M, Skaret E, Raadal M, et al. One- vs. five-session treatment of intra-oral injection phobia: a randomized clinical study. Eur J Oral Sci. 2009;117:279–285. [DOI] [PubMed] [Google Scholar]
- 50.Cornwall E, Spence SH, Schotte D. The effectiveness of emotive imagery in the treatment of darkness phobia in children. Behav Change. 1996;13:223–229. [Google Scholar]
- 51.Heaton LJ, Leroux BG, Ruff PA, et al. Computerized dental injection fear treatment: a randomized clinical trial. J Dent Res. 2013;92(suppl):37S–42S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mohr DC, Cox D, Merluzzi N. Self-injection anxiety training: a treatment for patients unable to self-inject injectable medications. Mult Scler. 2005;11:182–185. [DOI] [PubMed] [Google Scholar]
- 53.Camner L, Andersson E, Eurenius M. Treatment of a dental patient with injection phobia. Quintessence Int. 1983;14:759–760. [PubMed] [Google Scholar]
- 54.Dash J. Rapid hypno-behavioral treatment of a needle phobia in a five-year-old cardiac patient. J Pediatr Psychol. 1981;6:37–42. [DOI] [PubMed] [Google Scholar]
- 55.Davis TEI, Kurtz PF, Gardner AW, et al. Cognitive-behavioral treatment for specific phobias with a child demonstrating severe problem behavior and developmental delays. Res Dev Disabil. 2007;28:546–558. [DOI] [PubMed] [Google Scholar]
- 56.Fernandes PP. Rapid desensitization for needle phobia. Psychosomatics. 2003;44:253–254. [DOI] [PubMed] [Google Scholar]
- 57.Grassick P. The fear behind the fear: a case study of apparent simple injection phobia. J Behav Ther Exp Psychiatry. 1990;21:281–287. [DOI] [PubMed] [Google Scholar]
- 58.Grider B, Luiselli JK, Turcotte-Shamski W. Graduated exposure, positive reinforcement, and stimulus distraction in a compliance-with-blood-draw intervention for an adult with autism. Clin Case Stud. 2012;11:253–260. [Google Scholar]
- 59.Jacobsen PB. Treating a man with needle phobia who requires daily injections of medication. Hosp Community Psychiatry. 1991;42:877–878. [DOI] [PubMed] [Google Scholar]
- 60.Kleinknecht RA. Rapid treatment of blood and injection phobias with eye movement desensitization. J Behav Ther Exp Psychiatry. 1993;24:211–217. [DOI] [PubMed] [Google Scholar]
- 61.Koppel SM, Thapar A. Treating blood needle phobia. Hosp Med. 1998;59:730–732. [PubMed] [Google Scholar]
- 62.Mason RF. Treatment of fear induced conditioned response. A case report. Aust Dent J. 1973;18:309–310. [DOI] [PubMed] [Google Scholar]
- 63.Nakamura BJ, Schiffman J, Cecilia W. A modularized cognitive-behavioral intervention for water phobia in an adolescent with childhood-onset schizophrenia. Child Fam Behav Ther. 2006;28:29–41. [Google Scholar]
- 64.Osborn EL. Effects of participant modeling and desensitization on childhood warm water phobia. J Behav Ther Exp Psychiatry. 1986;17:117–119. [DOI] [PubMed] [Google Scholar]
- 65.Öst L-G. Single-session exposure treatment of injection phobia: a case study with continuous heart rate measurement. Scand J Behav Ther. 1985;14:125–131. [Google Scholar]
- 66.Pomerantz PB, Peterson NT, Marholin DI, et al. The in vivo elimination of a child’s water phobia by a paraprofessional at home. J Behav Ther Exp Psychiatry. 1977;8:417–421. [Google Scholar]
- 67.Ricciardi JN, Luiselli JK, Camare M. Shaping approach responses as intervention for specific phobia in a child with autism. J Appl Behav Anal. 2006;39:445–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Savide NL, Blain SM, Jedrychowski JR. The use of systematic desensitization in the dental treatment of a mentally retarded adolescent. J Dent Handicap. 1978;4:10–13. [PubMed] [Google Scholar]
- 69.Seim RW, Willerick MS, Gaynor ST, et al. Circumventing the vasovagal fainting response: a novel method of in vivo exposure for injection phobia. Clin Case Stud. 2008;7:409–422. [Google Scholar]
- 70.Shabani DB, Fisher WW. Stimulus fading and differential reinforcement for the treatment of needle phobia in a youth with autism. J Appl Behav Anal. 2006;39:449–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Turnage JR, Logan DL. Treatment of a hypodermic needle phobia by in vivo systematic desensitization. J Behav Ther Exp Psychiatry. 1974;5:67–69. [Google Scholar]
- 72.Van Dijk N, Velzeboer SC, Destree-Vonk A, et al. Psychological treatment of malignant vasovagal syncope due to bloodphobia. Pacing Clin Electrophysiol. 2001;24:122–124. [DOI] [PubMed] [Google Scholar]
- 73.Chapman LK, DeLapp RCT. Nine session treatment of a blood-injection-injury phobia with manualized cognitive behavioral therapy: an adult case example. Clin Case Stud. 2014;13:299–312. [Google Scholar]
- 74.Slifer KJ, Eischen SE, Busby S. Using counterconditioning to treat behavioural distress during subcutaneous injections in a paediatric rehabilitation patient. Brain Inj. 2002;16:901–916. [DOI] [PubMed] [Google Scholar]
- 75.Sanders MR, Jones L. Behavioural treatment of injection, dental and medical phobias in adolescents: a case study. Behav Psychother. 1990;18:311–316. [Google Scholar]
- 76.Thompson A. Cognitive-behavioural treatment of blood-injury-injection phobia: a case study. Behav Change. 1999;16:182–190. [Google Scholar]
- 77.Baralt AR, Dolan JD. Systematic desensitization & cognitive restructuring in the treatment of a self-injection phobia. J Rehabil. 1985;51:35–37. [Google Scholar]
- 78.Lisowska P, Zoitopoulos L. Cognitive behavioural therapy and severe needle phobia—a case study. J Disabil Oral Health. 2009;10:135–138. [Google Scholar]
- 79.Simon EP, Canonico MM. Use of hypnosis in controlling lumbar puncture distress in an adult needle-phobic dementia patient. Int J Clin Exp Hypn. 2001;49:56–67. [DOI] [PubMed] [Google Scholar]
- 80.Trijsburg RW, Jelicic M, van den Broek WW, et al. Exposure and participant modelling in a case of injection phobia. Psychother Psychosom. 1996;65:57–61. [DOI] [PubMed] [Google Scholar]
- 81.Cox D, Mohr DC, Epstein L. Treating self-injection phobia in patients prescribed injectable medications: a case example illustrating a six-session treatment model. Cogn Behav Pract. 2004;11:278–283. [Google Scholar]
- 82.Gow MA. Hypnosis with a 31-year-old female with dental phobia requiring an emergency extraction. Contemp Hypn. 2006;23:83–91. [Google Scholar]
- 83.Daniels LK. Rapid in office and in vivo desensitization of an injection phobia utilizing hypnosis. Am J Clin Hypn. 1976;18:200–203. [DOI] [PubMed] [Google Scholar]
- 84.Perczel-Forintos D, Hackmann A. Transformation of meaning and its effects on cognitive behavioural treatment of an injection phobia. Behav Cogn Psychother. 1999;27:369–375. [Google Scholar]
- 85.Hagopian LP, Crockett JL, Keeney KM. Multicomponent treatment for blood-injury-injection phobia in a young man with mental retardation. Res Dev Disabil. 2001;22:141–149. [DOI] [PubMed] [Google Scholar]
- 86.Horne DJDL, McCormack H. Behavioural psychotherapy for a blood and needle phobic mastectomy patient receiving adjuvant chemotherapy. Behav Psychother. 1984;12:342–348. [Google Scholar]
- 87.Ferguson JM, Wermuth BM, Taylor CB. Rapid desensitization of a needle phobia by participant modeling. West J Med. 1976;124:174–176. [PMC free article] [PubMed] [Google Scholar]
- 88.Wolff JJ, Symons FJ. An evaluation of multi-component exposure treatment of needle phobia in an adult with autism and intellectual disability. J Appl Res Intellect Disabil. 2013;26:344–348. [DOI] [PubMed] [Google Scholar]
- 89.Rainwater N, Sweet AA, Elliott L, et al. Systematic desensitization in the treatment of needle phobias for children with diabetes. Child Fam Behav Ther. 1988;10:19–31. [Google Scholar]
- 90.Ferguson JM, Taylor CB, Wermuth B. A rapid behavioral treatment for needle phobics. J Nerv Ment Dis. 1978;166:294–298. [DOI] [PubMed] [Google Scholar]
- 91.Morse DR, Cohen BB. Desensitization using meditation-hypnosis to control “needle” phobia in two dental patients. Anesth Prog. 1983;30:83–85. [PMC free article] [PubMed] [Google Scholar]
- 92.Taylor CB, Ferguson JM, Wermuth BM. Simple techniques to treat medical phobias. Postgrad Med J. 1977;53:28–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Silverman WK, Kurtines WM, Ginsburg GS, et al. Contingency management, self-control, and education support in the treatment of childhood phobic disorders: a randomized clinical trial. J Consult Clin Psychol. 1999;67:675–687. [DOI] [PubMed] [Google Scholar]
- 94.Last CG, Hansen C, Franco N. Cognitive-behavioral treatment of school phobia. J Am Acad Child Adolesc Psychiatry. 1998;37:404–411. [DOI] [PubMed] [Google Scholar]
- 95.Del Gaudio DJ, Nevid JS. Training dentally anxious children to cope. J Dent Child. 1991;58:31–37. [PubMed] [Google Scholar]
- 96.Haukebø K, Skaret E, Öst L-G, et al. One- vs. five-session treatment of dental phobia: a randomized controlled study. J Behav Ther Exp Psychiatry. 2008;39:381–390. [DOI] [PubMed] [Google Scholar]
- 97.Bodycoat N, Grauaug L, Olson A, et al. Constant versus rhythmic muscle tension in applied tension. Behav Change. 2000;17:97–102. [Google Scholar]
- 98.Krediet CT, van Dijk N, Linzer M, et al. Management of vasovagal syncope: controlling or aborting faints by leg crossing and muscle tensing. Circulation. 2002;106:1684–1689. [DOI] [PubMed] [Google Scholar]
- 99.Krediet CT, de Bruin IG, Ganzeboom KS, et al. Leg crossing, muscle tensing, squatting, and the crash position are effective against vasovagal reactions solely through increases in cardiac output. J Appl Physiol. 2005;99:1697–1703. [DOI] [PubMed] [Google Scholar]
- 100.Vögele C, Coles J, Wardle J, et al. Psychophysiologic effects of applied tension on the emotional fainting response to blood and injury. Behav Res Ther. 2003;41:139–155. [DOI] [PubMed] [Google Scholar]
- 101.Ditto B, France CR, Albert M, et al. Effects of applied muscle tension on the likelihood of blood donor return. Transfusion. 2009;49:858–862. [DOI] [PubMed] [Google Scholar]
- 102.Ditto B, France CR, Holly C. Applied tension may help retain donors who are ambivalent about needles. Vox Sang. 2010;98(3A):e225–e230. [DOI] [PubMed] [Google Scholar]
- 103.Ditto B, France CR, Lavoie P, et al. Reducing reactions to blood donation with applied muscle tension: a randomized controlled trial. Transfusion. 2003;43:1269–1275. [DOI] [PubMed] [Google Scholar]
- 104.Ditto B, France CR. The effects of applied tension on symptoms in French-speaking blood donors: a randomized trial. Health Psychol. 2006;25:433–437. [DOI] [PubMed] [Google Scholar]
- 105.Ditto B, Wilkins JA, France CR, et al. On-site training in applied muscle tension to reduce vasovagal reactions to blood donation. J Behav Med. 2003;26:53–65. [DOI] [PubMed] [Google Scholar]
- 106.Ditto B, France CR, Albert M, et al. Dismantling applied tension: mechanisms of a treatment to reduce blood donation-related symptoms. Transfusion. 2007;47:2217–2222. [DOI] [PubMed] [Google Scholar]
- 107.France CR, Ditto B, Wissel ME, et al. Predonation hydration and applied muscle tension combine to reduce presyncopal reactions to blood donation. Transfusion. 2010;50:1257–1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Holly CD, Balegh S, Ditto B. Applied tension and blood donation symptoms: the importance of anxiety reduction. Health Psychol. 2011;30:320–325. [DOI] [PubMed] [Google Scholar]
- 109.Holly CD, Torbit L, Ditto B. Applied tension and coping with blood donation: a randomized trial. Ann Behav Med. 2012;43:173–180. [DOI] [PubMed] [Google Scholar]
- 110.Lewis S. A comparison of behavior therapy techniques in the reduction of fearful avoidance behavior. Behav Ther. 1974;5:648–655. [Google Scholar]
- 111.Menzies RG, Clarke JC. A comparison of in vivo and vicarious exposure in the treatment of childhood water phobia. Behav Res Ther. 1993;31:9–15. [DOI] [PubMed] [Google Scholar]
- 112.Ultee CA, Griffioen D, Schellekens J. The reduction of anxiety in children: a comparison of the effects of systematic desensitization in vitro and systematic desensitization in vivo. Behav Res Ther. 1982;20:61–67. [DOI] [PubMed] [Google Scholar]
- 113.Bernstein GA, Peterson SE, Perwien AR, et al. Management of blood-drawing fears in adolescents with comorbid anxiety and depressive disorders. J Child Adolesc Psychopharmacol. 1996;6:53–61. [DOI] [PubMed] [Google Scholar]
- 114.Cisler JM. Treatment of disgust in blood-injection-injury-phobia: A randomized controlled trial. Dissertation Abstracts International: Section B: The Sciences and Engineering. 2010;70(8-B):5154. [Dissertation]. [Google Scholar]
- 115.Graziano AM, Mooney KC. Family self-control instruction for children’s nighttime fear reduction. J Consult Clin Psychol. 1980;48:206–213. [DOI] [PubMed] [Google Scholar]
- 116.Hellström K, Fellenius J, Öst L-G. One versus five sessions of applied tension in the treatment of blood phobia. Behav Res Ther. 1996;34:101–112. [DOI] [PubMed] [Google Scholar]
- 117.Hirai M, Cochran HM, Meyer JS, et al. A preliminary investigation of the efficacy of disgust exposure techniques in a subclinical population with blood and injection fears. Behav Change. 2008;25:129–148. [Google Scholar]
- 118.Oliver NS, Page AC. Fear reduction during in vivo exposure to blood-injection stimuli: distraction vs. attentional focus. Br J Clin Psychol. 2003;42(pt 1):13–25. [DOI] [PubMed] [Google Scholar]
- 119.Oliver NS, Page AC. Effects of internal and external distraction and focus during exposure to blood-injury-injection stimuli. J Anxiety Disord. 2008;22:283–291. [DOI] [PubMed] [Google Scholar]
- 120.Öst L-G, Sterner U, Fellenius J. Applied tension, applied relaxation, and the combination in the treatment of blood phobia. Behav Res Ther. 1989;27:109–121. [DOI] [PubMed] [Google Scholar]
- 121.Penfold K, Page AC. The effect of distraction on within-session anxiety reduction during brief in vivo exposure for mild blood-injection fears. Behav Ther. 1999;30:607–621. [Google Scholar]
- 122.Weiss MR, McCullagh P, Smith AL, et al. Observational learning and the fearful child: influence of peer models on swimming skill performance and psychological responses. Res Q Exerc Sport. 1998;69:380–394. [DOI] [PubMed] [Google Scholar]
- 123.Cyna AM, Tomkins D, Maddock T, et al. Brief hypnosis for severe needle phobia using switch-wire imagery in a 5-year old. Paediatr Anaesth. 2007;17:800–804. [DOI] [PubMed] [Google Scholar]
- 124.Weigold C. The use of hypnosis in the management of needle phobia. Aust J Clin Exp Hypn. 2011;39:189–195. [Google Scholar]
- 125.Kleinhauz M, Eli I. When pharmacologic anesthesia is precluded: the value of hypnosis as a sole anesthetic agent in dentistry. Spec Care Dentist. 1993;13:15–18. [DOI] [PubMed] [Google Scholar]
- 126.Moore KA. “Hypnosis or not?”: brief intervention with hypodermic needle phobic. Aust J Clin Exp Hypn. 1992;20:49–53. [Google Scholar]
- 127.Hoyle DE. Use of visual placebo in desensitization of a needle-phobic child. J Dent Child. 1982;49:214–216. [PubMed] [Google Scholar]
- 128.Gow MA. Treating dental needle phobia using hypnosis. Aust J Clin Exp Hypn. 2002;30:198–202. [Google Scholar]
- 129.Abramowitz EG, Lichtenberg P. Hypnotherapeutic olfactory conditioning (HOC): case studies of needle phobia, panic disorder, and combat-induced PTSD. Int J Clin Exp Hypn. 2009;57:184–197. [DOI] [PubMed] [Google Scholar]
- 130.Dennis B. Care study: severe needle phobia. Midwives Chron. 1994;107:58–61. [PubMed] [Google Scholar]
- 131.Brenes GA, Milo KM. A pregnant woman’s fear of her baby. Psychosomatics. 2000;41:531–534. [DOI] [PubMed] [Google Scholar]
- 132.Morgan S. Brief hypnosis for needle phobia. Aust J Clin Exp Hypn. 2001;29:107–115. [Google Scholar]
- 133.Medd DY. Fear of injections: the value of hypnosis in facilitating clinical treatment. Contemp Hypn. 2001;18:100–106. [Google Scholar]
- 134.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association; 1987. [Google Scholar]
- 135.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 136.Goisman RM, Allsworth J, Rogers MP, et al. Simple phobia as a comorbid anxiety disorder. Depress Anxiety. 1998;7:105–112. [PubMed] [Google Scholar]
- 137.Birnie KA, Chambers CT, Taddio A, et al. Psychological interventions for vaccine injections in children and adolescents: systematic review of randomized and quasi-randomized controlled trials. Clin J Pain. 2015;31(10S):S72–S89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Boerner KE, Birnie KA, Chambers CT, et al. Simple psychological interventions for reducing pain from common needle procedures in adults: systematic review of randomized and quasi-randomized controlled trials. Clin J Pain. 2015;31(10S):S90–S98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Pillai Riddell R, Taddio A, McMurtry CM, et al. Psychological interventions for vaccine injections in young children 0 to 3 years: systematic review of randomized controlled trials and quasi-randomized controlled trials. Clin J Pain. 2015;31(10S):S64–S71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Pillai Riddell R, Taddio A, McMurtry CM, et al. Process interventions for vaccine injections: systematic review of randomized controlled trials and quasi-randomized controlled trials. Clin J Pain. 2015;31(10S):S99–S108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Taddio A, Shah V, McMurtry CM, et al. Procedural and physical interventions for vaccine injections: systematic review of randomized controlled trials and quasi-randomized controlled trials. Clin J Pain. 2015;31(10S):S20–S37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Shah V, Taddio A, McMurtry CM, et al. Pharmacological and combined interventions to reduce vaccine injection pain in children and adults: systematic review and meta-analysis. Clin J Pain. 2015;31(10S):S38–S63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Davis TEI, Ollendick TH, Reuther ET, et al. Davis TEI. One-session treatment: principles and procedures with children and adolescents. Intensive One-Session Treatment of Specific Phobias. New York, NY: Springer; 2012:97–125. [Google Scholar]
- 144.Ollendick TH, Davis TEI. One-session treatment for specific phobias: a review of Öst’s single-session exposure with children and adolescents. Cogn Behav Ther. 2013;42:275–283. [DOI] [PubMed] [Google Scholar]
- 145.Öst L-G.Davis TEI, Ollendick TH, Öst L-G. One-session treatment: principles and procedures with adults. Intensive One-Session Treatment of Specific Phobias. New York, NY: Springer; 2012:59–95. [Google Scholar]
- 146.Braun MM, Patriarca PA, Ellenberg SS. Syncope after immunization. Arch Pediatr Adolesc Med. 1997;151:255–259. [DOI] [PubMed] [Google Scholar]
- 147.Centers for Disease Control and Prevention. Syncope after vaccination—United States, January 2005-July 2007. JAMA. 2008;299:2502–2506. [Google Scholar]
- 148.Newman BH, Graves S. A study of 178 consecutive vasovagal syncopal reactions from the perspective of safety. Transfusion. 2001;41:1475–1479. [DOI] [PubMed] [Google Scholar]
- 149.Woo EJ, Ball R, Braun MM. Fatal syncope-related fall after immunization. Arch Pediatr Adolesc Med. 2005;159:1083. [DOI] [PubMed] [Google Scholar]
- 150.Cisler JM, Olatunji RO, Lohr JM. Disgust, fear and the anxiety disorders: a critical review. Clin Psychol Rev. 2009;29:34–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Olatunji BO, Cisler J, McKay D, et al. Is disgust associated with psychopathology? Emerging research in the anxiety disorders. Psychiatry Res. 2010;175:1–10. [DOI] [PubMed] [Google Scholar]
- 152.Sawchuk CN, Lohr JM, Tolin DF, et al. Disgust sensitivity and contamination fears in spider and blood-injection-injury phobias. Behav Res Ther. 2000;38:753–762. [DOI] [PubMed] [Google Scholar]
- 153.Dalley JS, Creary P, McMurtry CM. What are you afraid of? Exploring the specific fears of children and adults regarding painful and other aspects of needle procedures. Poster presented at the International Association for the Study of Pain’s 15th World Congress on Pain, Buenos Aires, Argentina, October 2014.
- 154.Gearing RE, Schwalbe CS, Lee R, et al. The effectiveness of booster sessions in CBT treatment for child and adolescent mood and anxiety disorders. Depress Anxiety. 2013;30:800–808. [DOI] [PubMed] [Google Scholar]
- 155.Kleinknecht RA. Acquisition of blood, injury, and needle fears and phobias. Behav Res Ther. 1994;32:817–823. [DOI] [PubMed] [Google Scholar]
- 156.Öst L-G. Acquisition of blood and injection phobia and anxiety response patterns in clinical patients. Behav Res Ther. 1991;29:323–332. [DOI] [PubMed] [Google Scholar]
- 157.Noel M, Chambers CT, Petter M, et al. Pain is not over when the needle ends: a review and preliminary model of acute pain memory development in childhood. Pain Manag. 2012;2:487–497. [DOI] [PubMed] [Google Scholar]
- 158.Noel M, McMurtry CM, Chambers CT, et al. Children’s memory for painful procedures: the relationship of pain intensity, anxiety, and adult behaviors to subsequent recall. J Pediatr Psychol. 2010;35:626–636. [DOI] [PubMed] [Google Scholar]
- 159.Chen E, Zeltzer LK, Craske MG, et al. Children’s memories for painful cancer treatment procedures: implications for distress. Child Dev. 2000;71:933–947. [DOI] [PubMed] [Google Scholar]
- 160.McMurtry CM, Taddio A, Noel M, et al. Clinical practice guideline for the management of individuals with high levels of needle fear across the lifespan: exposure-based psychological and physical interventions. Clin Pract Pediatr Psychol. Under review. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


