Abstract
This study aimed to evaluate the impact of traffic noise along the motorway on sleep quality, sleepiness, and vigilant attention in long-haul truck drivers. This was a randomized, crossover, within-subject controlled study. Healthy long-haul truck drivers spent 6 consecutive nights in a real truck berth with full sleep laboratory equipment. During 3 nights, subjects were exposed to replayed traffic noise alongside motorways, whereas the other 3 nights were without traffic noise. Polysomnography was recorded during the nights and numerous sleepiness tests and vigilance examinations were performed during the following standardized working day. Outcome measures were compared between noisy and silent nights using the paired Wilcoxon test. Ten healthy long-haul truck drivers with a mean age of 36.3 ± 7.3 years completed the study as planned. On noisy nights, subjects had greater latencies to the rapid eye movement (REM) phase (90 ± 32 min vs 69 ± 16 min, P = 0.074) and higher percentages of sleep stage 1 (13.7 ± 5.5% vs 11.2 ± 4.4%; P = 0.059). Subjects also rated their sleep quality as having been better during nights without noise (28.1 ± 3.7 vs 30.3 ± 6.2, P = 0.092). The impact of these differences on daytime sleepiness and vigilance was rather low; however, mean Karolinska Sleepiness Scale (KSS) scores measured during the course of the following day were higher on six out of eight occasions after noisy nights. The effects of overnight traffic noise on sleep quality are detectable but unlikely to have any major impact on the vigilant attention and driving performance of long haul-truck drivers with low nocturnal noise sensitivity. This might not be true for subgroups prone to sleeping disorders.
Keywords: Fitness to drive, polysomnography, sleepiness, sleep quality, vigilance
Introduction
Sleep is essential for human recovery and well-being. Impaired sleep or the lack of sleep overnight generally impairs daytime alertness and accordingly may affect fitness to drive as well. Patients with obstructive sleep apnea showed lower car driving performance[1,2] and a significantly greater risk of being involved in traffic accidents than the general population.[3,4,5,6,7,8,9,10] However, daytime sleepiness is far from being relevant only to subgroups with specific sleep disorders. It is a major cause of work and traffic accidents in general.[11] Several independent studies quite consistently revealed sleepiness to be involved in one out of four to five traffic accidents.[11] In a large survey in the UK, 29% out of the 4621 interviewed male car drivers admitted to having at least once almost fallen asleep while driving during the preceding year;[12] about 25% of such instances were reported by long-haul truck drivers.[13]
One of the most obvious exogenous factors by which sleep might be affected in the general population is traffic noise. It is a major cause of extrinsic sleep disturbances and negatively affects performance, mood, and health.[14,15] It is also well established that nocturnal road traffic noise causes sound-induced awakenings and autonomic arousals during sleep.[16,17] These physiological reactions lead to sleep fragmentation, which in turn can impair daytime functioning. Whereas the negative impact of traffic noise on sleep quality and sleep structure is well recognized, its relevance for daytime alertness or sleepiness has hardly been investigated yet.[18] It may be of particular interest in long-haul truck drivers because:
They are more exposed to traffic noise than average road users,
they are often forced to sleep during rest times along noisy motorways, and
prevalence of daytime sleepiness, poor sleep quality, and sleeping disorders is known to be higher in truck drivers compared to the general population.[19,20,21]
Therefore, the current study aimed to evaluate the impact of overnight traffic noise on the nocturnal sleep quality, daytime sleepiness, and vigilant attention of long-haul truck drivers over during a mostly standardized but still realistic working week.
Methods
Design
This was a randomized, crossover, within-subject controlled study in a setting simulating the typical working conditions of professional long-haul truck drivers. The subjects had to spend six consecutive nights in a real truck berth (Mercedes Benz Actros II, 1860 Megaspace) furnished with sleep laboratory equipment and to pass further sleepiness assessments during the following standardized working day, with two defined round trips on another truck (Mercedes Benz Actros II, 1841 Largespace, Powershift 16, with a truckload of 40t). During three consecutive nights the sleeping subjects were exposed to the usual traffic noise along motorways replayed from tape, whereas the other three nights served as control nights without noise. Half of the group started with the “silent nights” and the other one with the “noisy nights” before they crossed over, with the order of both conditions having been assigned randomly.
The study was compliant with all applicable legal obligations, the requirements of the Declaration of Helsinki, and Good Clinical Practice. It was approved by the local University Ethics Committee.
Sound presentation
For a maximum standardization throughout all “noisy nights,” traffic noise was once recorded by a PAK MKII system (Müller-BBM VibroAkustik Systeme GmbH, Planegg, Germany) in an original truck berth (Mercedes Benz Actros II, 1860 Megaspace) at the interstate service area Denkendorf, Germany, during a November night from 10 PM to 6 AM. For data reduction, 10-min sequences were recorded every hour in waveform audio file format (.wav). During the nights with traffic noise exposure, each recorded audio file sequence was subsequently repeated six times using a playlist generated by the software Winamp® 5.0 (Nullsoft Inc., San Francisco, USA, 2003). Thus, 8 h of audiotaped traffic noise was presented via a loudspeaker (KH O 98 active studio monitor, Klein + Hummel GmbH, Ostfildern, Germany) at the original loudness according to the recording of a calibration signal (94 dB). Mean sound pressure level of the recordings was 44.7 dB(A) [minimum: 37.4 dB(A) and maximum: 48.0 dB(A)]. Subjective ratings on the realistic noise exposure of the presented sound were comparable to those on traffic noise usually perceived by subjects during night rest along motorways.
Study population
Those eligible for inclusion in this study were male professional long-haul truck drivers accustomed to overnight stays in their trucks along motorways. They had to be 25-50 years of age and their regular bedtimes were in their spare time, usually between 9 PM and midnight. Subjects were excluded if they had any concomitant disease or symptoms affecting sleep or alertness according to International Classification of Sleep Disorder (ICSD) 2 criteria, self-rating scores for depression >40[22] and for anxiety >36,[23] any relevant visual or auditory impairments, or a medical history of drug abuse/dependence according to criteria of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR™). For all participants, subjective noise sensitivity was assessed by the Noise Sensitive Questionnaire (NoiSeQ).[24] Strong smokers (>20 cigarettes/day) and coffee drinkers (>5 cups/day, i.e., > 400 mg caffeine per day) were also excluded. Coffee had to be discontinued the evening before and any psychoactive drugs at least 1 week prior to the experiments. Smoking was not allowed 15 min before and until the end of any examination. All patients had to give written informed consent to participate in the study.
Outcome measures
Objective measurements were performed on sleep quality using standard sleep parameters measured by polysomnography during all six nights and on daytime sleepiness using pupillography in the morning and at noon. Corresponding subjective assessments were made in parallel, on sleep quality in the morning and on sleepiness throughout the day; in the morning and at noon using the Stanford Sleepiness Scale (SSS)[25,26] and the Tiredness Symptom Scale (TSS)[27] (at noon twice, at the beginning and at the end of a series of examinations) and about every 2 h as self-test using the Karolinska Sleepiness Scale (KSS).[28] Vigilance and sustained attention were tested using the Mackworth Clock test (MCT) according to Quatember and Maly[29] at noon as well as by the psychomotor vigilance task (PVT)[30] presented as a self-test on a Palm device about every 2 h. In addition, attention, reactive stress tolerance, and reaction speed was assessed by the Determination Test (DT) of the Vienna Test System at noon [Table 1]. All participating subjects were sufficiently trained on all testing procedures and received written instructions beforehand. All assessments were always performed in the same order.
Table 1.
Overview of used techniques and outcome measures
| Dimensions and measures | Parameters | Time point |
|---|---|---|
| Sleep quality, objective | ||
| Polysomnography[28] | Total sleep duration, sleep efficiency, latencies to sleep stage 1 and REM, sleep stage distribution, arousal index, waketime after sleep onset, changes of sleep stages based on standard measurements | During time in bed (TIB) from 11:15 PM to 6:15 AM (wakening) |
| Sleep quality, subjective | ||
| Three-dimensional questionnaire[31] | Subjective sleep quality rated in three dimensions addressing sleep, awakening, and physical complaints separately. Sum scores of the three range 20-80, with high scores translating to low sleep quality | 8 AM |
| Sleepiness, objective | ||
| Pupillographic Sleepiness Test (PST)[30] | Pupil unrest index (PUI) as measure for occurrence of fatigue waves | 8:15 AM, 12:15 PM (2×) |
| Sleepiness, subjective | ||
| Stanford Sleepiness Scale (SSS)[21,22] | Sleepiness score on a 7-item scale from 1 (fully awake) to 7 (almost sleeping) | 8 AM, noon (2×) |
| Tiredness Symptom Scale (TSS)[23] | Sum score for the presence (=1) or absence (=0) of 14 different symptoms of tiredness. Accordingly, score ranges from 0 (none present) to 14 (all present) | 8 AM, noon (2×) |
| Karolinska Sleepiness Scale (KSS)[24] | Sleepiness score on a 9-item scale from 1 (extremely awake) to 9 (extremely sleepy) | every 2 h, throughout the day |
| Vigilance, sustained attention and reaction speed, objective | ||
| Mackworth Clock test (MCT)[25] | Mean RT; number of false, omitted and true reactions as measure for the sustained vigilance under monotonous conditions | noon |
| Palm pychomotor vigilance task (PalmPVT)[26] | Mean RT during the day as measure for changes in vigilance | every 2 h, throughout the day |
| Determination test (DT)[27] | Mean RT, number of false and true reactions as well as of omitted, delayed, and timely reactions (reaction mode) as measure for reactive stress tolerance and attention in situations requiring continuous, swift, and varying responses to rapidly changing visual and acoustic stimuli | noon |
Polysomnography was recorded in a standardized way[32] with the digital polysomnography system PTMS1-comlab 44 (Schwarzer GmbH, Munich, Germany). Horizontal and vertical eye movements were recorded by electrooculogram (EOG, four channels), muscle tonus at the chin by electromyogram (EMG, one channel), leg movements (EMG, two channels), electroencephalogram (EEG, six channels: C3, C4, O1, O2, A1, A2), and heart rate (one channel). In addition, subjects were connected to a microphone and thermistor to record snoring and nasal respiration, respectively; to sensors of thoracic and abdominal respiration movements; and to a pulse oximeter for the determination of arterial oxygen saturation. EEG electrodes were placed 10:20 as recommended by the German Society of Sleep Research and Medicine.[33] For all channels, the default settings of filters, frequencies, and sampling rates were adopted according to the American Academy of Sleep Medicine Manual for the scoring of sleep and associated events (Westchester, IL, USA). Sleep scoring data were based on sampling rates of 125 Hz for EOG and of 250 Hz for EEG and chin EMG. The high frequency filter was set at 35 Hz for EOG recordings and at 70 Hz for EEG and chin EMG records. The low frequency filters were 4.0 Hz for EOG, 0.3 Hz for EEG, and 0.032 Hz for chin EMG. Throughout the night, sleeping subjects were videotaped and monitored by clinical staff of the sleep disorder center. Polysomnographic recording times were standardized to 7 h of bedtime (from 11:15 PM to 6:15 AM). The noise level inside the cabin was recorded with a sound level meter (Cirrus Research, Frankfurt, Germany). Room temperature within the truck berth was automatically logged (TFA, Dostmann, Germany) and ranged 16-19°C.
Pupillography: The Pupillographic Sleepiness Test (PST, AMTech Pupilknowlogy GmbH, Dossenheim, Germany) was used to measure physiological sleepiness. Variations of the pupil diameter in the darkness correlate with autonomic sleepiness and are mostly unaffected by psychological factors. Those variations were measured by infrared videography during eight intervals of 82.5 s with a sampling frequency of 25 Hz and a spatial resolution of 0.05 mm. For each interval, the pupil unrest index (PUI) was measured in mm/min.[34,35] The mean PUI-scores were calculated only if the interpolation rate (substitution of lost values because of an interrupted recording) for an interval was less than 25% and if at least four of the eight intervals could be included. A normal range in healthy non–sleep-deprived adults is determined at 3.5-6.6 mm/min (AMTech Pupilknowlogy GmbH).
The MCT according to Quatember and Maly is a computer-based vigilance test (VIGIL, S1, Quatember and Maly) of the Vienna Test System (Version 5.10, Schuhfried GmbH, Mödling, Austria) assessing sustained attention in a low-stimulus observation situation. A white dot jumped along a circular path of small circles from one to the next. Sometimes the dot skipped a circle and made a double jump, in which case subjects were supposed to press a button as soon as possible. Overall, 100 double jumps were to be recognised over 25 min. The number of omitted and false positive reactions and the mean reaction time (RT) were recorded.
The Palm psychomotor vigilance task (PalmPVT) is an easy-to-use, field-portable RT test on sustained attention over 5 min. The test runs on Palm-OS–based personal data assistants (PDAs) and is based on the fully digital “psychomotor vigilance test” (Model PVT-192; Ambulatory Monitoring Inc., Ardsley, NY, USA). Subjects had to press a button on the device at each occurrence of the same visual stimulus on the display. After each reaction, subjects received immediate feedback on their RT. The test comprised of 100 stimuli that were pseudo-randomly presented at intervals ranging 1-5 s. Outcome measure was the mean RT per session.
The DT was also a computer-based standard attention test (DT, S4, Hannover variant) of the Vienna Test System (as above) to assess reaction speed (in the action mode) and reactive stress tolerance (in the reactive mode). Subjects were presented in random order with one out of two different visual and one acoustic stimulus, to which they had to respond by pressing previously assigned buttons. The stimuli were differently presented in two separate runs: in the action mode, only the number of stimuli was fixed and the speed of presentation was paced by the response of the subject. Measured outcomes were mean RTs, and the number of false and true reactions. In the reaction mode, the time limit and speed of presentation were also fixed. This is cognitively more demanding than the action mode, as the task requires continuous and varying responses to very rapidly changing stimuli. In addition to the outcome measures of the action mode, the number of omissions, of delayed and of timely responses were counted.
Subjective evaluations of sleep quality and sleepiness were made based on standard rating tools, summarized in Table 1.
Data analysis
For the statistical analysis, data of each outcome measure were averaged per subject for noisy and silent nights and afterward compared using the paired Wilcoxon test (repeated measures analysis of variance or other parametric data analyses were not feasible because of the small sample size and the violation of statistical assumptions). Due to the exploratory nature of the study, there was no correction for multiplicity, and significance level was set at alpha = 0.1. Data were analyzed using SPSS version 15.0 statistical software (SPSS Inc., Chicago, IL, USA).
Results
Characteristics of truck drivers
All 10 recruited subjects completed the study as planned. They were all male, with a mean age of 36.3 ± 7.3 [standard deviation (SD); range: 25-46] years and a body mass index (BMI) of 25.2 ± 2.6 (range 21.7-30.0) kg/m2. On average, they had been working as truck drivers for more than 10 (10.4 ± 6.6; range: 2-23) years with an average of 133,600 km travelled per year. All of them were regularly consuming caffeinated beverages, with an average of 2.6 ± 0.5 cups/day. Nine of them were also smokers with an average consumption of 12.3 ± 6.6 cigarettes/day. The personal sleep requirement was estimated at 7.1 ± 1.3 h, although sleep during a usual working week in fact lasted 6.1 ± 0.7 h. Noise sensitivity was 1.8 ± 0.4 on a scale 0-3 and lowest on the sleep subscale (1.9 ± 0.5).
Sleep quality
On silent nights the subjects had a longer total sleep time on average, greater sleep efficiency, shorter time to rapid eye movement (REM) sleep, fewer arousals and changes of sleep phases, shorter waketime after sleep onset, and a subjectively better rated sleep quality. Although none of these differences was actually significant, the greater latency to REM sleep, the greater percentage of sleep stage 1, and the better subjective rating achieved P values <0.1 [Table 2].
Table 2.
Sleep quality: Results of polysomnography and subjective assessment
| Measures | Silent | Noisy | P |
|---|---|---|---|
| Global sleep parameters | |||
| Total sleep duration [min] | 382±16 | 372±22 | 0.241 |
| Sleep efficiency [%] | 92±4 | 89±6 | 0.203 |
| Latencies [min] | |||
| to sleep state 1 | 7.6±7.1 | 7.5±6.6 | 0.878 |
| to REM sleep | 69±16 | 90±32 | 0.074 |
| Sleeping stage distribution [%] | |||
| Stage 1 | 11.2±4.4 | 13.7±5.5 | 0.059 |
| Stage 2 | 52.1±4.9 | 49.8±6.2 | 0.386 |
| Stage 3 | 10.1±3.8 | 11.0±3.8 | 0.241 |
| Stage 4 | 3.8±4.5 | 3.8±3.8 | 0.674 |
| REM | 22.8±3.7 | 21.7±5.2 | 0.333 |
| Sleep interruptions | |||
| Arousal index [/h] | 14.3±5.7 | 16.2±4.9 | 0.139 |
| Waketime after sleep onset [min] | 23.8±11.4 | 32.4±25.7 | 0.878 |
| Changes of sleep stages | 7.8±2.4 | 9.0±4.3 | 0.507 |
| Subjective sleep quality | |||
| Total score (20: High to 80: Low sleep quality) | 28.1±3.7 | 30.3±6.2 | 0.092 |
Daytime sleepiness
On the following morning, pupillography did not reveal any difference in PUI after silent and noisy nights. No difference was observed in subjective assessments of sleepiness using the SSS or the TSS. At noon, there was still no difference in PUIs between silent and noisy nights, but both had significantly increased as compared to the morning measurement. No such trend was observed in the two subjective scales, although there were significant differences between the ratings at the beginning and the end of examinations after control nights [Table 3]. Differences on the KSS showed no significant difference between both conditions except at 8:30 AM [Figure 1] (P = 0.040). Mean scores were consistently higher after noisy nights on six out of eight occasions through the day and lower than after control nights on only one occasion [Figure 1]. The KSS significantly increased during the afternoon.
Table 3.
Results of wakefulness testing the day following experimental nights
| Measures | Silent | Noisy | P |
|---|---|---|---|
| Sleepiness | |||
| Pupillary Unrest Index (PUI) [mm/min] | |||
| morning (8:15 AM) | 4.9±1.4 | 4.9±1.5 | 0.799 |
| noon (12:15 PM) | 6.2±2.6 | 6.0±1.9 | 0.959 |
| Stanford Sleepiness Scale (SSS) (1: Low to 8: High sleepiness) | |||
| Morning (8 AM) | 1.7±0.8 | 1.8±0.8 | 0.932 |
| Noon, start of assessment | 1.4±0.5 | 1.5±0.7 | 0.552 |
| Noon, end of assessment | 1.7±0.5 | 1.7±0.4 | 0.674 |
| Tiredness Symptom Scale (TSS) (0: Low to 14: High tiredness) | |||
| Morning (8 AM) | 0.7±1.2 | 0.95±1.8 | 0.279 |
| Noon, start of assessment | 0.1±0.2 | 0.4±0.5 | 0.344 |
| Noon, end of assessment | 0.6±0.7 | 0.6±0.8 | 0.893 |
| Mackworth Clock test (MCT) (according to Quatember and Maly) | |||
| RT [s] | 0.47±0.06 | 0.47±0.07 | 1.000 |
| Omissions | 2.28±2.21 | 3.60±5.45 | 0.330 |
| False positive reactions | 2.53±2.12 | 2.35±2.20 | 0.540 |
| Determination tests | |||
| Action mode | |||
| RT [s] | 0.83±0.13 | 0.86±0.24 | 0.838 |
| True reactions | 350.1±50.6 | 357.8±41.1 | 0.575 |
| False reactions | 12.5±14.2 | 14.2±16.6 | 0.093 |
| Reaction mode | |||
| RT [s] | 0.66±0.13 | 0.66±0.10 | 0.919 |
| Correct reactions | 212.0±41.3 | 208.2±28.8 | 0.721 |
| False reactions | 15.5±15.2 | 17.8±17.0 | 0.678 |
| Omissions | 26.4±37.1 | 26.4±25.4 | 0.959 |
| Delayed reactions | 37.1±29.0 | 34.6±21.7 | 0.799 |
| Timely reactions | 171.5±52.3 | 173.6±43.8 | 0.799 |
Figure 1.
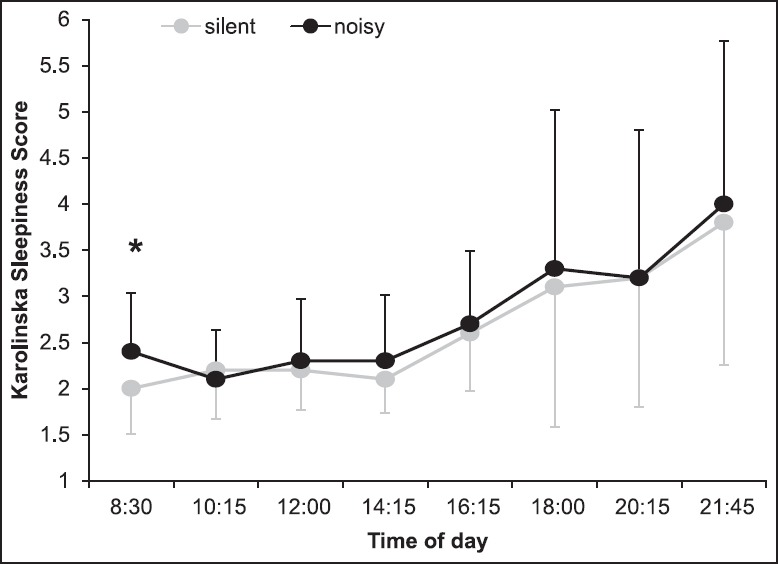
Mean subjective assessment of sleepiness (+ and − SD) on the Karolinska Sleepiness Scale (KSS) during the working day following the experimental nights *Asterisk marks P levels <0.05
Vigilance, sustained attention, and reaction speed
On the MCT on vigilance, subjects had a greater average number of omitted reactions and a lower number of false positive reactions after noisy than after control nights, although none of these differences were significant; mean RTs were the same [Table 3].
On the DT, the mean number of false reactions was higher in both modes after noisy nights and reached borderline significance in the action mode (P = 0.093). All remaining differences were far from being significant and average readouts did not consistently indicate a better performance in favor of one or the other condition either [Table 3]. In particular, there was no noteworthy difference in RTs on either test. However, those showed significantly variations on the Palm self-test during the course of the day after control nights. They continuously increased from 6 PM with values greater than after noisy nights [Figure 2].
Figure 2.
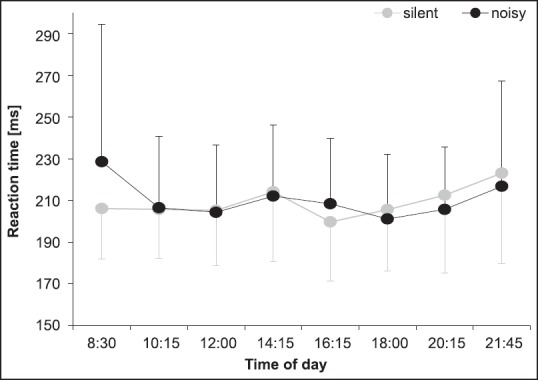
Mean RTs (+ and − SD) on the Palm psychomotor vigilance task (PalmPVT) during the working day following the experimental nights
Discussion
This was the first experimental study investigating the impact of overnight traffic noise on sleep quality, daytime sleepiness, and vigilance specifically in long-haul truck drivers. It was performed in a most naturalistic but standardized setting, and a most comprehensive test program was used. Overall, negative effects of traffic noise were detectable on both sleep quality and daytime sleepiness. However, the negative impact of traffic noise was generally rather small, so our study turned out to be potentially underpowered and able to only reach borderline significance at best. Lacking power may thus be considered a weakness. Nevertheless, a larger study at the same level of standardization and with the same comprehensive test program would have hardly been feasible. We assume that by increasing the sample size, the observed differences could have reached statistical significance. However, as we found only subtle changes in sleepiness and performance outcome measures, these differences might not be of practical relevance. We speculate that even significant changes would have only a minor negative impact on overall daytime alertness and real-life performance in our subjects.
This is endorsed by the accordance of our results with those from a comparable Swedish pilot study exploring the impact of traffic noise on sleep quality in a truck berth and morning sleepiness in 6 male non-truck drivers.[36] The study also revealed only a few borderline significant differences related to REM latency and subjective sleep quality ratings. In another study in 72 healthy adults, air, road, and rail traffic noise were also found to affect ratings of sleep quality and recuperation primarily, whereas changes in sleep structure and performance measures were only subtle.[18] Thus, the observed small effects in our study might not be due to habituation or the generally rather low noise sensitivity of our study population.
However, even though the observed effects of traffic noise were small and thus unlikely to affect vigilant attention and sleepiness, they may still be of relevance due to chronicity and as they add to other known negative influences on sleep quality, specifically of long-haul truck drivers. Recent Australian studies revealed sleep quality in truck berths to be generally lower[37,38] and less restorative than at home,[37] and long-term exposure to road traffic noise to be associated with increased morning tiredness.[39] In addition, evidence is growing of an association between long-term exposure to traffic noise and cardiovascular disease[40] and diabetes.[41] Beyond the known lower average health status of truck drivers in general, chronic sleep disorders appear to be common. Up to almost half of them were reported to suffer from poor sleep quality and hypersomnolence,[19,21] more than one out of four might be at risk of having obstructive sleep apnea;[20] one out of five was reported to suffer from chronic sleep disturbances; and 27% and 15% from depression and anxiety, respectively.[31] Although this can hardly be shown, chronic exposure to overnight traffic noise is likely to contribute to this greater prevalence of sleeping disorders, even though it might not have any major short-term impact. Thus, efforts to reduce exposure to traffic noise, particularly in long-haul truck drivers, remain well justified.
However, these considerations also raise the question of the external validity of our data, as only healthy drivers without sleeping or mental disorders were enrolled and our standardized working day simulation excluded common naps, nighttime driving, or consumption of coffee. Whether exposure to overnight traffic noise may have greater “acute” effects on prone subgroups of long-haul truck drivers with sleeping disorders therefore remains an open question.
Financial support and sponsorship
Daimler AG.
Conflicts of interest
Siegfried Rothe has been employed by Daimler AG, the sponsor of the study.
Acknowledgment
The authors would like to thank all the drivers participating in this study and Uwe Totzke for medical writing support. This work was supported by Daimler Benz.
References
- 1.Juniper M, Hack MA, George CF, Davies RJ, Stradling JR. Steering simulation performance in patients with obstructive sleep apnoea and matched control subjects. Eur Respir J. 2000;15:590–5. doi: 10.1034/j.1399-3003.2000.15.27.x. [DOI] [PubMed] [Google Scholar]
- 2.Risser MR, Ware JC, Freeman FG. Driving simulation with EEG monitoring in normal and obstructive sleep apnea patients. Sleep. 2000;23:393–8. [PubMed] [Google Scholar]
- 3.Basoglu OK, Tasbakan MS. Elevated risk of sleepiness-related motor vehicle accidents in patients with obstructive sleep apnea syndrome: A case-control study. Traffic Inj Prev. 2014;15:470–6. doi: 10.1080/15389588.2013.830213. [DOI] [PubMed] [Google Scholar]
- 4.Findley LJ, Unverzagt ME, Suratt PM. Automobile accidents involving patients with obstructive sleep apnea. Am Rev Respir Dis. 1988;138:337–40. doi: 10.1164/ajrccm/138.2.337. [DOI] [PubMed] [Google Scholar]
- 5.George CF, Nickerson PW, Hanly PJ, Millar TW, Kryger MH. Sleep apnoea patients have more automobile accidents. Lancet. 1987;2:447. doi: 10.1016/s0140-6736(87)90974-3. [DOI] [PubMed] [Google Scholar]
- 6.Horstmann S, Hess CW, Bassetti C, Gugger M, Mathis J. Sleepiness-related accidents in sleep apnea patients. Sleep. 2000;23:383–9. [PubMed] [Google Scholar]
- 7.Lloberes P, Levy G, Descals C, Sampol G, Roca A, Sagales T, et al. Self-reported sleepiness while driving as a risk factor for traffic accidents in patients with obstructive sleep apnoea syndrome and in non-apnoeic snorers. Respir Med. 2000;94:971–6. doi: 10.1053/rmed.2000.0869. [DOI] [PubMed] [Google Scholar]
- 8.Teran-Santos J, Jimenez-Gomez A, Cordero-Guevara J. The association between sleep apnea and the risk of traffic accidents. Cooperative Group Burgos-Santander. N Engl J Med. 1999;340:847–51. doi: 10.1056/NEJM199903183401104. [DOI] [PubMed] [Google Scholar]
- 9.Wu H, Yan-Go F. Self-reported automobile accidents involving patients with obstructive sleep apnea. Neurology. 1996;46:1254–7. doi: 10.1212/wnl.46.5.1254. [DOI] [PubMed] [Google Scholar]
- 10.Young T, Blustein J, Finn L, Palta M. Sleep-disordered breathing and motor vehicle accidents in a population-based sample of employed adults. Sleep. 1997;20:608–13. doi: 10.1093/sleep/20.8.608. [DOI] [PubMed] [Google Scholar]
- 11.åkerstedt T. Consensus statement: fatigue and accidents in transport operations. J Sleep Res. 2000;9:395. doi: 10.1046/j.1365-2869.2000.00228.x. [DOI] [PubMed] [Google Scholar]
- 12.Maycock G. Sleepiness and driving: The experience of UK car drivers. J Sleep Res. 1996;5:229–37. doi: 10.1111/j.1365-2869.1996.00229.x. [DOI] [PubMed] [Google Scholar]
- 13.McCartt AT, Rohrbaugh JW, Hammer MC, Fuller SZ. Factors associated with falling asleep at the wheel among long-distance truck drivers. Accid Anal Prev. 2000;32:493–504. doi: 10.1016/s0001-4575(99)00067-6. [DOI] [PubMed] [Google Scholar]
- 14.Griefahn B. Noise control during the night. Acoust Aust. 1992;20:43–7. [Google Scholar]
- 15.Ising H, Kruppa B. Health effects caused by noise: Evidence in the literature from the past 25 years. Noise Health. 2004;6:5–13. [PubMed] [Google Scholar]
- 16.Marks A, Griefahn B, Basner M. Event-related awakenings caused by nocturnal transportation noise. Noise Control Eng J. 2008;56:52–62. [Google Scholar]
- 17.Griefahn B, Brode P, Marks A, Basner M. Autonomic arousals related to traffic noise during sleep. Sleep. 2008;31:569–77. doi: 10.1093/sleep/31.4.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Basner M, Muller U, Elmenhorst EM. Single and combined effects of air, road, and rail traffic noise on sleep and recuperation. Sleep. 2011;34:11–23. doi: 10.1093/sleep/34.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Braeckman L, Verpraet R, Van Risseghem M, Pevernagie D, De Bacquer D. Prevalence and correlates of poor sleep quality and daytime sleepiness in Belgian truck drivers. Chronobiol Int. 2011;28:126–34. doi: 10.3109/07420528.2010.540363. [DOI] [PubMed] [Google Scholar]
- 20.Catarino R, Spratley J, Catarino I, Lunet N, Pais-Clemente M. Sleepiness and sleep-disordered breathing in truck drivers: Risk analysis of road accidents. Sleep Breath. 2014;18:59–68. doi: 10.1007/s11325-013-0848-x. [DOI] [PubMed] [Google Scholar]
- 21.de Pinho RS, da Silva-Júnior FP, Bastos JP, Maia WS, de Mello MT, de Bruin VM, et al. Hypersomnolence and accidents in truck drivers: A cross-sectional study. Chronobiol Int. 2006;23:963–71. doi: 10.1080/07420520600920759. [DOI] [PubMed] [Google Scholar]
- 22.Zung WW. A Self-rating depression scale. Arch Gen Psychiatry. 1965;12:63–70. doi: 10.1001/archpsyc.1965.01720310065008. [DOI] [PubMed] [Google Scholar]
- 23.Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12:371–9. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- 24.Schutte M, Marks A, Wenning E, Griefahn B. The development of the noise sensitivity questionnaire. Noise Health. 2007;9:15–24. doi: 10.4103/1463-1741.34700. [DOI] [PubMed] [Google Scholar]
- 25.Hoddes E, Dement WC, Zarcone V. The development and use of the stanford sleepiness scale (SSS) Psychophysiology. 1972;10:431–6. doi: 10.1111/j.1469-8986.1973.tb00801.x. [DOI] [PubMed] [Google Scholar]
- 26.Shahid A, Wilkinson K, Marcu S, Shapiro CM. Stanford sleepiness scale (SSS) In: Shahid A, Wilkinson K, Marcu S, Shapiro CM, editors. STOP, THAT and One Hundred Other Sleep Scales. New York: Springer; 2012. pp. 369–70. [Google Scholar]
- 27.Schulz H, Volk S, Yassouridis A. Measuring tiredness by symptoms. J Sleep Res. 1991;20A:515. [Google Scholar]
- 28.Akerstedt T, Gillberg M. Subjective and objective sleepiness in the active individual. Int J Neurosci. 1990;52:29–37. doi: 10.3109/00207459008994241. [DOI] [PubMed] [Google Scholar]
- 29.Nachreiner F, Hänecke K. Vigilance. In: Smith AP, Jones DM, editors. Handbook of Human Performance. Vol. 3. State and Trait. London: Academic Press; 1992. pp. 261–88. [Google Scholar]
- 30.Thorne DR, Johnson DE, Redmond DP, Sing HC, Belenky G, Shapiro JM. The Walter Reed palm-held psychomotor vigilance test. Behav Res Methods. 2005;37:111–8. doi: 10.3758/bf03206404. [DOI] [PubMed] [Google Scholar]
- 31.Shattell M, Apostolopoulos Y, Collins C, Sönmez S, Fehrenbacher C. Trucking organization and mental health disorders of truck drivers. Issues Ment Health Nurs. 2012;33:436–44. doi: 10.3109/01612840.2012.665156. [DOI] [PubMed] [Google Scholar]
- 32.Rechtschaffen A, Kales A. Los Angeles: Brain Information Service/Brain Research Institute; 1968. A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. [Google Scholar]
- 33.Höller L. Grundlagen und technische Ausbildung: Technik der Polysomnographie im Schlaflabor. In: Schulz H, editor. Kompendium Schlafmedizin für Ausbildung, Klinik und Praxis. Vol. 1. Landsberg: Ergänzungslieferung Deutsche Gesellschaft für Schlafforschung und Schlafmedizin, eco-med; 1997. [Google Scholar]
- 34.Ludtke H, Wilhelm B, Adler M, Schaeffel F, Wilhelm H. Mathematical procedures in data recording and processing of pupillary fatigue waves. Vision Res. 1998;38:2889–96. doi: 10.1016/s0042-6989(98)00081-9. [DOI] [PubMed] [Google Scholar]
- 35.Wilhelm B, Wilhelm H, Ludtke H, Streicher P, Adler M. Pupillographic assessment of sleepiness in sleep-deprived healthy subjects. Sleep. 1998;21:258–65. [PubMed] [Google Scholar]
- 36.Kecklund G, Akerstedt T. Sleep in a truck berth. Sleep. 1997;20:614–9. doi: 10.1093/sleep/20.8.614. [DOI] [PubMed] [Google Scholar]
- 37.Baulk SD, Fletcher A. At home and away: Measuring the sleep of Australian truck drivers. Accid Anal Prev. 2012;45(Suppl):36–40. doi: 10.1016/j.aap.2011.09.023. [DOI] [PubMed] [Google Scholar]
- 38.Darwent D, Roach G, Dawson D. How well do truck drivers sleep in cabin sleeper berths? Appl Ergon. 2012;43:442–6. doi: 10.1016/j.apergo.2011.06.019. [DOI] [PubMed] [Google Scholar]
- 39.de Kluizenaar Y, Janssen SA, van Lenthe FJ, Miedema HM, Mackenbach JP. Long-term road traffic noise exposure is associated with an increase in morning tiredness. J Acoust Soc Am. 2009;126:626–33. doi: 10.1121/1.3158834. [DOI] [PubMed] [Google Scholar]
- 40.Bluhm G, Eriksson C. Cardiovascular effects of environmental noise: Research in Sweden. Noise Health. 2011;13:212–6. doi: 10.4103/1463-1741.80152. [DOI] [PubMed] [Google Scholar]
- 41.Sorensen M, Andersen ZJ, Nordsborg RB, Becker T, Tjønneland A, Overvad K, et al. Long-term exposure to road traffic noise and incident diabetes: A cohort study. Environ Health Perspect. 2013;121:217–22. doi: 10.1289/ehp.1205503. [DOI] [PMC free article] [PubMed] [Google Scholar]


