Abstract
There is great concern regarding the development of noise-induced hearing loss (NIHL) in youth caused by high sound levels during various leisure activities. Health-orientated behavior of young adults might be linked to the beliefs and attitudes toward noise, hearing loss, and hearing protector devices (HPDs). The objective of the current study was to evaluate the effects of attitudes and beliefs toward noise, hearing loss, and HPDs on young adults’ hearing status. A questionnaire and an audiological test battery were completed by 163 subjects (aged 18-30 years). The questionnaire contained the Youth Attitude to Noise Scale (YANS) and Beliefs about Hearing Protection and Hearing Loss (BAHPHL). A more positive attitude or belief represented an attitude where noise or hearing loss is seen as unproblematic and attitudes and beliefs regarding HPDs is worse. Hearing was evaluated using (high frequency) pure tone audiometry (PTA), transient evoked and distortion product otoacoustic emissions. First, mean differences in hearing between the groups with different attitudes and beliefs were evaluated using one-way analysis of variance (ANOVA). Second, a χ2 test was used to examine the usage of HPDs by the different groups with different attitudes and beliefs. Young adults with a positive attitude had significantly more deteriorated hearing and used HPDs less than the other subjects. Hearing conservation programs (HCPs) for young adults should provide information and knowledge regarding noise, hearing loss, and HPDs. Barriers wearing HPDs should especially be discussed. Further, those campaigns should focus on self-experienced hearing related symptoms that might serve as triggers for attitudinal and behavioral changes.
Keywords: Attitudes, hearing, hearing protector devices (HPDs), noise-induced hearing loss (NIHL), recreational noise exposure, young adults
Introduction
It is widely accepted that excessive noise exposure can cause noise-induced hearing loss (NIHL). Besides occupational noise exposure, recreational noise exposure is a cause for concern. Since the early 1980s, there has been a decrease in the prevalence of occupational noise exposure, while social noise exposure has tripled.[1] High sound levels during various leisure activities, such as the use of personal music players[2,3,4,5,6,7] and attendance at clubs[8,9,10,11,12,13,14] and concerts,[15,16,17,18] might pose risks to hearing. However, the literature regarding the prevalence of NIHL caused by recreational noise has revealed inconsistent results. Some studies reported an increase in the prevalence of NIHL caused by recreational noise,[19,20,21] whereas others failed to prove such an increase.[22,23,24,25] Risk assessment of NIHL caused by recreational noise exposure is complicated by the lack of nonoccupational risk criteria and the accumulation of noise exposure at multiple recreational and occupational activities. Furthermore, risk assessment is liable for an individual's involvement in taking health risks, especially in the case of young adults. To prevent NIHL caused by recreational noise exposure in young adults, information regarding risk-taking behavior is necessary to adequately construct hearing conservation programs (HCPs) designed to induce more health-orientated behavior.
Several theoretical frameworks exist to explain an individual's risk-taking behavior, including the health belief model (HBM) and the theory of planned behavior (TPB). According to HBM,[26] the susceptibility to hearing loss and the seriousness of hearing loss symptoms will result in taking preventive action as long as the perceived benefits outweigh the barriers. Additionally, triggers to appropriate action are necessary, such as hearing loss-related symptoms. However, the consequences of an individual's risk behavior regarding recreational noise exposure are not immediately perceived[27] or are not experienced as serious enough.[28] Nevertheless, individuals reporting tinnitus and noise sensitivity are more worried about hearing loss and more likely to report the use of hearing protector devices (HPDs) than those without hearing loss-related symptoms.[29,30] Further, individuals with permanent tinnitus assess listening to loud music as more risky, and those with occasional tinnitus listen more often to loud music.[31] However, attitudes and subjective norms are not incorporated in HBM, but are considered key aspects in the TPB.[32] In this latter model, attitudes regarding recreational noise exposure, hearing loss and HPDs, and subjective norms and perceived behavioral control determine behavioral intentions such as the intention to use HPDs. Perceived behavioral control relates to the perception of the benefits of and barriers to preventive action as well as the perception of self-efficacy. In adolescents, HPD usage was significantly correlated to the norms, barriers, and hearing loss-related symptoms.[33] Nevertheless, misperceptions of social norms related to music-listening behavior were previously found.[34] However, in TPB, the individual's experience of behavioral outcomes that can be positive, such as the appreciation of loud music, or negative, such as having hearing loss-related symptoms that could be a trigger to behavioral change as well as behavioral intention are not identified. Therefore, a theoretical framework specifically constructed for recreational noise exposure was postulated by Widen.[33] It combines all the factors of TPB with barriers to behavioral change and triggers to action from HBM, and adds another factor “risk perception” to its model. Triggers, especially noise sensitivity, and norms and perceived behavioral control are negatively associated with attitudes, whereas the barriers against using HPDs are positively associated with attitudes.
Using these theoretical frameworks, it would be possible to identify important factors related to risk-taking behavior in young adults. The identified factors can then be used to optimize HCPs targeting young adults. Currently, HCPs provide information regarding the effects of hearing loss and knowledge concerning the availability and use of HPDs.[35] However, this might not be enough since some campaigns are found to induce a certain behavioral change,[36] while others do not have such an effect.[37,38]
Furthermore, to our knowledge, young adults’ hearing status in relation to the attitudes toward recreational noise exposure and beliefs regarding the susceptibility to and seriousness of hearing loss, the benefits of and barriers to using HPDs and norms have not yet been evaluated. The hypothesis is that young adults with more problematic health-orientated attitudes and beliefs use HPDs infrequently and already have a more deteriorated hearing status than other young adults.
Therefore, the purpose of the current study was to investigate the effects of the attitudes and beliefs regarding noise, hearing loss, and HPDs on young adults’ hearing as measured by (high frequency) pure tone audiometry (PTA) and evoked otoacoustic emissions (EOAEs).
Methods
Subjects
Hundred and sixty three subjects (127 females, 36 males) with age ranging 18-30 years (mean: 21.23 years, standard deviation (SD): 2.89 years), gathered through convenience sampling, voluntarily participated in the study. First, a questionnaire regarding the attitudes and beliefs toward noise, hearing loss, and HPDs during recreational activities was filled out by all the subjects. Second, the hearing status of all the subjects was evaluated during a single session in a double-walled sound attenuated booth. Before testing, a noise free period of at least 24 h was required. Otoscopic evaluation, admittance measures, PTA at conventional and extended high frequencies, and EOAEs were performed. Both ears were tested, but only one ear per subject was selected at random for statistical analysis.
The study design and all the procedures of the current study were approved by the local ethical committee. All the subjects received detailed information with regard to this study and only those agreeing with the informed consent in accordance with the statements of the Declaration of Helsinki participated in the study.
Questionnaire
The questionnaire was designed based on the available literature regarding the assessment of noise exposure during recreational activities among youth, and their attitudes and beliefs regarding noise exposure, hearing loss, and HPDs.[2,30,39,40] The translated preliminary version of the questionnaire was pretested by a semi-structured interview-based assessment on a group of young adults not included in the current study. Their responses were analyzed, and the questionnaire was refined.[41] The final version of the questionnaire contained five parts.
The first part consisted of questions regarding the subjective assessment of hearing and hearing loss symptoms. Further, the knowledge and concern regarding NIHL caused by recreational noise exposure were explored. In the second and third parts of the questionnaire, sources, participation in and loudness estimation of recreational noise exposure, and the use of personal music players were questioned. These results are presented elsewhere.[42] In the fourth part, the attitudes and beliefs regarding noise, hearing loss, and HPDs were evaluated by modified versions of the Youth Attitude to Noise Scale (YANS) and the Beliefs about Hearing Protection and Hearing Loss (BAHPHL).[41] Finally, in the demographic part, questions regarding gender, age, education or profession, and parental employment were added.
The modified YANS consisted of 19 items assessed using a five-degree Likert scale from “totally disagree” to “totally agree”, coded from one to five.[41] A higher score on the YANS indicated a more positive attitude representing an attitude where noise is seen as unproblematic. All items were categorized in four subscales representing the attitudes toward noise associated with elements of youth culture (eight items), the ability to concentrate in noisy environments (three items), daily noise (four items), and the intent to influence the sound environment (four items).[30] To enhance the reliability of the fourth factor,[41] items 3 and 19 were reformulated as: “I am prepared to make my environment quieter if I have to study or work” and “When I cannot get rid of sounds that bother me, I become agitated.”
The modified version of the BAHPHL questionnaire consisted of 24 items, which were reformulated focusing on youth and HPD usage during recreational noise exposure.[41] The items were categorized into seven subscales: susceptibility to hearing loss (six items), severity of the consequences of hearing loss (three items), benefits of preventive action (three items), barriers to preventive action (four items), behavioral intentions (three items), social norms (two items), and self-efficacy (three items). Consistent with YANS, the items were evaluated by a five-degree Likert scale; the higher the score, the more positive the subjects’ attitudes and beliefs regarding hearing loss and HPDs.
The quartiles of the scores on (subscales of) YANS and BAHPHL were used to categorize the subjects’ attitudes and beliefs into a negative (lower quartile) group, a neutral (two middle quartiles) group, and a positive (upper quartile) group. Subjects with more anti-noise, neutral and pro-noise attitudes and beliefs were categorized into the negative group, neutral group, and positive group, respectively.
Admittance measures
Tympanometry was performed with an 85 dB sound pressure level (SPL) 226 Hz probe tone. Ipsilateral and contralateral acoustic stapedial reflexes were registered at 1.0 kHz (TympStar, Grason-Stadler Inc., Minnesota, USA). All the participants had normal immittance values and present acoustic stapedial reflexes that were used as inclusion criteria in the study.
Audiometric evaluation
PTA was performed using the modified Hughson-Westlake method for air conduction thresholds at conventional octave frequencies 0.25 kHz to 8.0 kHz and half-octave frequencies 3.0 kHz and 6.0 kHz (Orbiter 922 Clinical Audiometer, MADSEN Eletronics, Taastrup Denmark). Furthermore, extended high frequency audiometry was measured at 10.0 kHz, 12.5 kHz, and 16 kHz using a HDA 200 headphone (Sennheiser, Connecticut USA).
OAEs
Transient evoked OAEs (TEOAEs) and distortion product OAEs (DPOAEs) were measured using the ILO 292 USB II module (Otodynamics Ltd., Hatfield UK), coupled with a laptop with ILOv6 software (Otodynamics Ltd., Hatfield UK). The DPOAE probe was used for all OAE measurements and was calibrated before each measurement using the 1-cc calibration cavity provided by the manufacturer.
The nonlinear differential method of stimulation was used for TEOAE measurements. Rectangular pulses of 80 μs at a rate of 50 clicks per second were delivered at an intensity of 80 ± 2 dB peSPL. The registration of TEOAEs was terminated after 260 accepted sweeps with a noise rejection setting of 4 mPa. Emission and noise amplitudes were calculated in half-octave frequency bands centered at 1.0 kHz, 1.5 kHz, 2.0 kHz, 3.0 kHz, and 4.0 kHz. A probe stability of 90% or better was needed, and TEOAEs were considered present if the signal-to-noise ratio (SNR) was at least 3 dB at each half-octave frequency band separately or across frequencies.
DPOAEs were measured with the simultaneous presentation of two primary tones, with primary tone level combination L1/L2 = 65/55 dB SPL at eight points per octave. The ratio of primary tone frequencies f2/f1 equaled 1.22, and f2 ranged 0.841-8.0 kHz. A noise artefact rejection level of 6 mPa was used and the whole frequency range was looped until the noise amplitude fell below -5 dB SPL at individual frequencies. DPOAEs were considered present when SNR at all individual frequencies was at least 3 dB. The emission and noise amplitudes present were averaged into half-octave frequency bands with center frequencies 1.0 kHz, 1.5 kHz, 2.0 kHz, 3.0 kHz, 4.0 kHz, 6.0 kHz, and 8.0 kHz. If DPOAEs were absent at all frequencies within a given half-octave band, emission and noise amplitudes were considered missing in that frequency band.
Data analysis
Statistical analysis was performed using SPSS version 22 (IBM Corp., New York, USA). First, one-way analysis of variance (ANOVA) was used to evaluate the mean differences in hearing between the groups with negative, neutral, and positive attitudes and beliefs. When the significance level was reached (P < 0.05), post hoc least significant difference (LSD) with Bonferroni correction was done between the groups of interest, i.e., negative versus positive, and neutral versus positive attitudes. Second, 2 × 3 contingency tables using a χ2 test were used to evaluate whether the usage of HDPs differed between the three groups with different attitudes and beliefs. When the significance level was reached (P < 0.05), χ2 test with Bonferroni correction of 2 × 2 tables was carried out on the groups with negative versus positive, and neutral versus positive attitudes.
Results
Table 1 reflects the mean and standard deviations (SDs) of the scores on (subscales of the) YANS and BAHPHL as well as the range of scores for the groups with negative, neutral, and positive attitudes and beliefs regarding noise, hearing loss, and HPDs. Concerning the subscales of YANS, the highest average score was found for the attitudes regarding daily noise, whereas the lowest average score was related to the attitudes intending to influence the sound environment. Thus, young adults regard daily noise in their environment as unproblematic while they intend to reduce their environmental sound levels. For the subscales of BAHPHL, the lowest and highest average scores were found for the beliefs related to the severity of consequences of hearing loss and the beliefs related to social norms, respectively. This indicates that young adults are well aware of the effects of hearing loss while the perceptions about norms are less important.
Table 1.
For the YANS and BAHPHL, the mean, SD, and range of scores of attitudes and beliefs (n = 163) are reflected
| Questionnaire | Subscales | Mean | SD | Groups of attitudes and beliefs | ||
|---|---|---|---|---|---|---|
| Negative | Neutral | Positive | ||||
| YANS | Elements of youth culture | 2.44 | 0.64 | 1.13-1.87 | 1.88-2.87 | 2.88-4.38 |
| Concentration in noisy environments | 2.60 | 0.89 | 1.00-1.99 | 2.00-2.99 | 3.00-5.00 | |
| Daily noise | 3.33 | 0.77 | 1.75-2.74 | 2.75-3.99 | 4.00-5.00 | |
| Intent to influence sound environment | 1.91 | 0.66 | 1.00-1.24 | 1.25-2.24 | 2.25-4.25 | |
| Entire YANS | 2.54 | 0.47 | 1.37-2.25 | 2.26-2.78 | 2.79-4.26 | |
| BAHPHL | Susceptibility to hearing loss | 1.72 | 0.50 | 1.00-1.32 | 1.33-1.99 | 2.00-3.17 |
| Severity of the consequences of hearing loss | 1.51 | 0.56 | 1.00-0.99 | 1.00-1.6 | 1.67-4.00 | |
| Benefits of preventive action | 1.84 | 0.62 | 1.00-1.32 | 1.33-2.32 | 2.33-4.00 | |
| Barriers to preventive action | 3.00 | 0.77 | 1.00-2.49 | 2.50-3.49 | 3.50-4.75 | |
| Behavioral intentions | 2.94 | 1.10 | 1.00-1.99 | 2.00-3.99 | 4.00-5.00 | |
| Social norms | 3.33 | 0.96 | 1.00-2.99 | 3.00-3.99 | 4.00-5.00 | |
| Self-efficacy | 2.94 | 0.79 | 1.00-2.32 | 2.33-3.32 | 3.33-5.00 | |
With regard to the research question, we evaluated whether young adults’ hearing status measured using PTA and EOAEs, depends on more problematich health-orientated attitudes and beliefs.
First, for PTA, there were significant mean differences in hearing thresholds at 6.0 kHz (F2, 160 = 6.52, P < 0.01) between the groups on the scores for the entire YANS. Hearing thresholds increased significantly by 5.68 dB on an average in the group representing a positive attitude toward noise as compared to the group with a negative attitude [Figure 1]. Young adults with attitudes where noise is seen as unproblematic have worse hearing thresholds than adults with the attitudes where noise is regarded as problematic. Also, for the YANS subscale related to the intent to influence sound environment, there was a significant increase in mean hearing thresholds at 4.0 kHz (F2, 160 = 4.27, P < 0.025) with 5.25 dB and 2.55 dB for the groups with negative or neutral attitude on the one hand, and positive attitude on the other hand, respectively. For the BAHPHL subscale related to barriers to preventive action, there was a significant increment in mean hearing thresholds at 1.0 kHz (F2, 160 = 6.05; P < 0.01) and 2.0 kHz (F2, 160 = 4.42; P < 0.01) of 3.58 dB and 3.39 dB for the subjects with negative versus positive attitudes and beliefs. Further, subjects with neutral attitudes and beliefs at this factor of BAHPHL had significantly higher hearing thresholds on an average of 2.54 dB at 2.0 kHz (F2, 160 = 4.42; P < 0.025) compared to those with positive attitudes [Figure 2]. This indicates that young adults with strong barriers to hearing protection during recreational noise exposure have worse hearing than other young adults.
Figure 1.
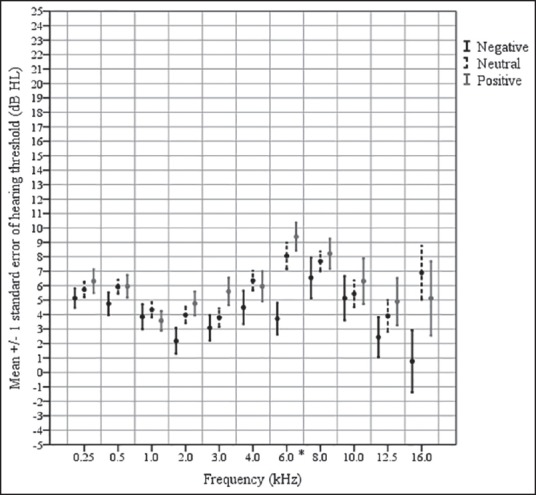
Hearing thresholds for subjects with different attitudes for the entire YANS
Figure 2.
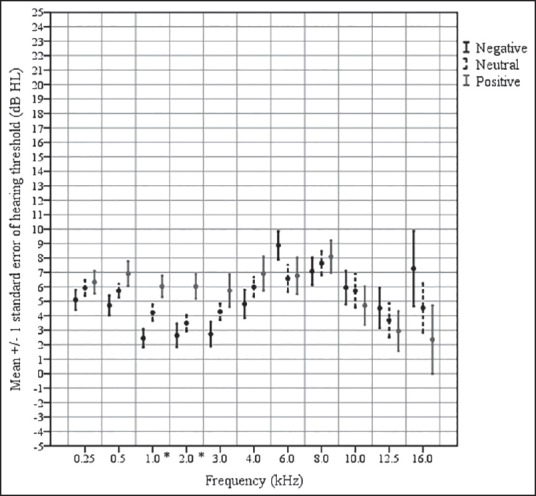
Hearing thresholds for subjects with different attitudes at the BAHPHL subscale related to the barriers to preventive action
For TEOAE amplitudes, groups with negative versus positive attitudes at the entire YANS had a significant mean decrease of 3.09 dB at half-octave frequency band 1.5 kHz (F2, 159 = 3.21, P < 0.025). Thus, if noise is seen as unproblematic, worse TEOAE amplitudes are found [Figure 3]. Moreover, mean TEOAE amplitudes decreased significantly by 2.81 dB in subjects with neutral versus positive attitudes for the YANS factor related to concentration in noisy environments at half-octave frequency band 1.5 kHz (F2, 159 = 4.51, P < 0.01). No significant mean differences in TEOAE amplitudes were found between the groups of different attitudes and beliefs at BAHPHL.
Figure 3.
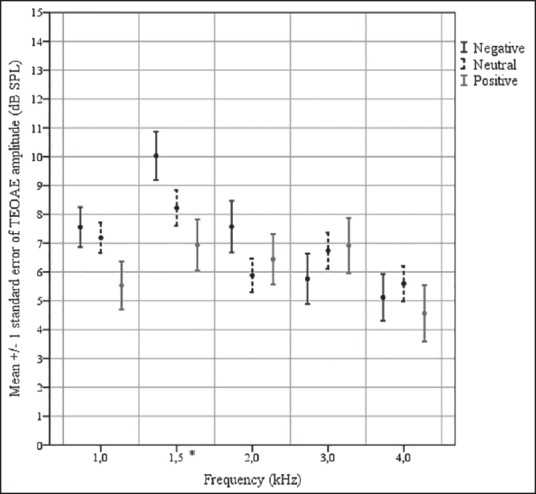
TEOAE amplitudes for subjects with different attitudes for the entire YANS
Mean DPOAE amplitudes between the group with a neutral attitude and the group with a positive attitude decreased significantly for the YANS factor related to concentration in noisy environments by 2.33 dB and 3.09 dB on an average at half-octave frequency bands 1.0 kHz (F2,159 = 4.10, P < 0.01) and 2.0 kHz (F2,159 = 5.07, P < 0.01), respectively. This is illustrated in Figure 4. No significant mean differences in DPOAE amplitudes were found between the groups of different attitudes and beliefs at BAHPHL.
Figure 4.
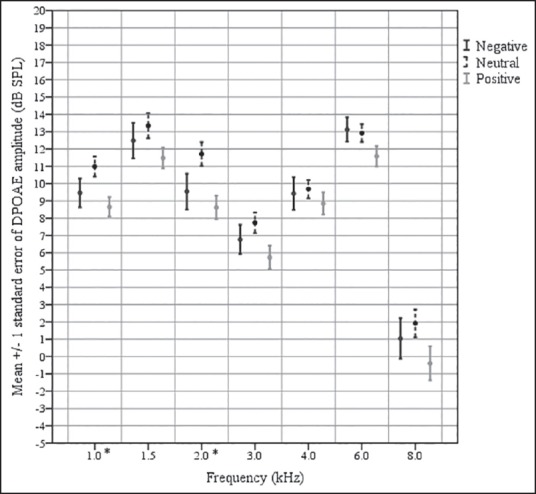
DPOAE amplitudes for subjects with different attitudes for the YANS subscale related to concentration in noisy environments
Second, the χ2 test revealed significant results of the usage of HDPs between the three groups with different attitudes and beliefs at several subscales of YANS and BAHPHL. Young adults with more health-orientated attitudes and beliefs regarding noise, hearing loss, and HPDs use HPDs more often than other young adults. As reflected in Table 2, the odds ratio (OR) ranged 2.70-23.04. Thus, HPDs are at least 2.70 times more used by adults with more negative or neutral attitudes and beliefs.
Table 2.
Differences in the use of HDPs between the groups with different attitudes and beliefs for YANS and BAHPHL are reflected (n = 163)
| Questionnaire | Subscales | Negative vs positive | Neutral vs positive |
|---|---|---|---|
| YANS | Elements of youth culture | χ2 (1)=6.641; P<0.025 OR=4.21 | NS |
| Concentration in a noisy environment | NS | χ2(1)=7.484; P<0.025 OR=2.70 | |
| Daily noises | NS | NS | |
| Intent to influence sound environment | NS | NS | |
| Entire YANS | NS | NS | |
| BAHPHL | Susceptibility to hearing loss | NS | NS |
| Severity of the consequences of hearing loss | NS | NS | |
| Benefits of preventive action | NS | NS | |
| Barriers to preventive action | NS | χ2(1)=6.149; P<0.025 OR=3.08 | |
| Behavioral intentions | χ2(1)=26.741; P<0.001 OR=23.04 | NS | |
| Social norms | NS | NS | |
| Self-efficacy | χ2(1)=15.640; P<0.001 OR=10.56 | χ2(1)=16.733; P<0.001 OR=4.30 |
NS = Nonsignificant results, ORs = Odds ratios
Discussion
Young people expose themselves voluntarily to loud music in many of their daily activities, by using their personal music player individually as well as in groups in discotheques, nightclubs, concerts, festivals, etc.[43] This behavior is risky since acquiring hearing damage during these recreational activities is possible. Several theoretical frameworks are constructed to explain risk-taking behavior. The most recent model specifically constructed for recreational noise exposure combines all the factors of TPB,[32] that is, attitudes, subjective norms, and perceived behavioral control, with barriers to behavioral change and triggers to action from HBM[26] and risk perception.[33] Information regarding these factors in young adults is important as it can optimize HCPs designed to induce more health-orientated behavior. In the literature, some of these factors are questioned in several populations in relation to confounding variables such as gender, cultural differences, and socioeconomic status,[30,44,45] or are used to evaluate the effectiveness of a preventive campaign.[36] However, to our knowledge, this is the first study that evaluates young adults’ hearing status in relation to all suggested variables.[33] Therefore, it is hypothesized that young adults with more problematic health-orientated attitudes and beliefs use HPDs infrequently and already have a more deteriorated hearing status.
In the current study, YANS and BAHPHL were used to evaluate young adults’ attitudes toward recreational noise exposure, their beliefs regarding the susceptibility to hearing loss, the seriousness of hearing loss, the benefits of and barriers to using HPDs and norms.
First, it was found that our subjects had a less problematic attitude regarding noise exposure based on YANS than the subjects from the studies of Widen et al.[30,46] and Gilles et al.[47] It was hypothesized that information and knowledge can explain such variation between studies. Further, significant deterioration in hearing thresholds, TEOAE, and DPOAE amplitudes was found for the scores on the entire YANS, and subscales associated with the ability to concentrate in noisy environments and the intent to influence the sound environment. Thus, it can be concluded that young adults with more problematic attitudes regarding noise exposure have already significant hearing damage in comparison to those with more negative or neutral attitudes. Since self-experienced symptoms, especially noise sensitivity,[33] are negatively associated with attitudes toward noise,[46] HCPs should provide information and knowledge on symptoms associated with excessive noise exposure.
Second, based on BAHPHL, it was found that the severity of consequences of hearing loss are on an average more negatively assessed, indicating that subjects are aware of reduced communication skills associated with hearing loss. In contradiction, the barriers to preventive action as well as behavioral intentions are on an average more positively evaluated. Thus, being aware of the consequences of hearing loss is not directly related to behavioral change. Moreover, it was found that hearing thresholds worsened significantly with positively evaluating barriers to preventive action. Experiencing more barriers wearing HPDs, such as a perceived pressure on the ears, uncomfortable feeling of the HPDs, being annoyed with having to wear HPDs as well as the impression to be less communicative lead to the reduced likelihood of taking preventative action.[27] This was confirmed by the current results whereby young adults with more health-orientated attitudes and beliefs regarding noise, hearing loss, and HPDs use HPDs significantly more often than others. This was seen for the attitudes as well as factors related to the barriers to preventive action, perceived behavioral control, and risk perception. Concerning the barriers against using HPDs, the comfort, appearance, and communication skills while using HPDs are found to be important;[48] therefore, the design, appearance, marketing, and packaging of HPDs should target young adults specifically.[49]
Considering the relation found between the attitudes and beliefs on the one hand, and the hearing status or use of HPDs on the other hand, the proposed model of Widen contains all the factors that could explain a certain amount of risk-taking behavior in young adults.[33] It is a challenge for health care providers to optimize HCPs based on those factors to induce behavioral change at an individual level, which is currently not always seen.[37,38] Further, as previously stated, behavioral change in norms on a societal level should also be aimed for.[33]
Regarding the audiological test battery, significant differences in hearing thresholds were found on conventional test frequencies, but not at extended high frequencies. Nevertheless, there was a tendency for increased mean thresholds in subjects with a more positive attitude regarding noise exposure. However, the large variability experienced at these extended high frequencies probably prevented significant results. Therefore, the role of extended high-frequency audiometry for the early detection of NIHL remains questionable.[50,51] Second, significant differences in TEOAE amplitudes were found at half-octave frequency band 1.5 kHz and DPOAE amplitudes at half-octave frequency bands 1.0 kHz and 2.0 kHz. The former is lower than the decline on TEOAE amplitudes at 2.0 kHz found by Mansfield et al.,[52] which was explained by a boost in this frequency region caused by the resonance of ear canal and ossicular chain.
Conclusion
In conclusion, young people's attitudes and beliefs regarding noise, hearing loss, and HPDs have a significant impact on their hearing status as measured with PTA and EOAEs as well as the use of HPDs. Therefore, HCPs for young adults should provide information on self-experienced symptoms after recreational noise exposure, besides providing information and knowledge regarding noise exposure, hearing loss, and HPDs. Moreover, barriers against the use of HPDs should be discussed in HCPs and efforts should be undertaken concerning the design, appearance, marketing, and packaging of HPDs for young adults. However, more research is needed to evaluate how other specific factors relate to risk-taking behavior with regard to recreational noise exposure, and how these can be targeted, e.g., norms on a societal level. Moreover, the effectiveness of HCPs by inducing attitudinal and behavioral changes and preventing further hearing deterioration caused by recreational noise exposure in young adults should be investigated. Finally, the prevalence of NIHL and tinnitus due to recreational activities in a representative sample of young adults should be evaluated.
Acknowledgement
Hannah Keppler was funded through an Aspirant Scholarship of the Research Foundation, Flanders (FWO), Belgium.
Footnotes
Source of Support: Hannah Keppler was funded through an Aspirant Scholarship of the Research Foundation, Flanders (FWO), Belgium
Conflict of Interest: There was no conflict of interest.
References
- 1.Smith PA, Davis A, Ferguson M, Lutman ME. The prevalence and type of social noise exposure in young adults in England. Noise Health. 2000;2:41–56. [PubMed] [Google Scholar]
- 2.Ahmed S, Fallah S, Garrido B, Gross A, King M, Morrish T, et al. Use of portable audio devices by university students. Can Acoust. 2007;35:35–54. [Google Scholar]
- 3.Torre P., 3rd Young adults’ use and output level settings of personal music systems. Ear Hear. 2008;29:791–9. doi: 10.1097/AUD.0b013e31817e7409. [DOI] [PubMed] [Google Scholar]
- 4.Keith SE, Michaud DS, Chiu V. Evaluating the maximum playback sound levels from portable digital audio players. J Acoust Soc Am. 2008;123:4227–37. doi: 10.1121/1.2904465. [DOI] [PubMed] [Google Scholar]
- 5.Kumar A, Mathew K, Alexander SA, Kiran C. Output sound pressure levels of personal music systems and their effect on hearing. Noise Health. 2009;11:132–40. doi: 10.4103/1463-1741.53357. [DOI] [PubMed] [Google Scholar]
- 6.Keppler H, Dhooge I, Maes L, D’haenens W, Bockstael A, Philips B, et al. Short-term auditory effects of listening to an MP3 player. Arch Otolaryngol Head Neck Surg. 2010;136:538–48. doi: 10.1001/archoto.2010.84. [DOI] [PubMed] [Google Scholar]
- 7.Portnuff CD, Fligor BJ, Arehart KH. Teenage use of portable listening devices: A hazard to hearing? J Am Acad Audiol. 2011;22:663–77. doi: 10.3766/jaaa.22.10.5. [DOI] [PubMed] [Google Scholar]
- 8.Meecham EA, Hume KI. Tinnitus, attendance at night-clubs and social drug taking in students. Noise Health. 2001;3:53–62. [PubMed] [Google Scholar]
- 9.Sadhra S, Jackson CA, Ryder T, Brown MJ. Noise exposure and hearing loss among student employees working in university entertainment venues. Ann Occup Hyg. 2002;46:455–63. [PubMed] [Google Scholar]
- 10.Bray A, Szymański M, Mills R. Noise induced hearing loss in dance music disc jockeys and an examination of sound levels in nightclubs. J Laryngol Otol. 2004;118:123–8. doi: 10.1258/002221504772784577. [DOI] [PubMed] [Google Scholar]
- 11.Serra MR, Biassoni EC, Richter U, Minoldo G, Franco G, Abraham S, et al. Recreational noise exposure and its effects on the hearing of adolescents. Part I: An interdisciplinary long-term study. Int J Audiol. 2005;44:65–73. doi: 10.1080/14992020400030010. [DOI] [PubMed] [Google Scholar]
- 12.Santos L, Morata TC, Jacob LC, Albizu E, Marques JM, Paini M. Music exposure and audiological findings in Brazilian disc jockeys (DJs) Int J Audiol. 2007;46:223–31. doi: 10.1080/14992020601188575. [DOI] [PubMed] [Google Scholar]
- 13.Twardella D, Wellhoefer A, Brix J, Fromme H. High sound pressure levels in Bavarian discotheques remain after introduction of voluntary agreements. Noise Health. 2008;10:99–104. doi: 10.4103/1463-1741.44348. [DOI] [PubMed] [Google Scholar]
- 14.Williams W, Beach EF, Gilliver M. Clubbing: The cumulative effect of noise exposure from attendance at dance clubs and night clubs on whole-of-life noise exposure. Noise Health. 2010;12:155–8. doi: 10.4103/1463-1741.64970. [DOI] [PubMed] [Google Scholar]
- 15.Yassi A, Pollock N, Tran N, Cheang M. Risks to hearing from a rock concert. Can Fam Physician. 1993;39:1045–50. [PMC free article] [PubMed] [Google Scholar]
- 16.Mercier V, Luy D, Hohmann BW. The sound exposure of the audience at a music festival. Noise Health. 2003;5:51–8. [PubMed] [Google Scholar]
- 17.Opperman DA, Reifman W, Schlauch R, Levine S. Incidence of spontaneous hearing threshold shifts during modern concert performances. Otolaryngol Head Neck Surg. 2006;134:667–73. doi: 10.1016/j.otohns.2005.11.039. [DOI] [PubMed] [Google Scholar]
- 18.Ryberg JB. A national project to evaluate and reduce high sound pressure levels from music. Noise Health. 2009;11:124–8. doi: 10.4103/1463-1741.50698. [DOI] [PubMed] [Google Scholar]
- 19.Montgomery JK, Fujikawa S. Hearing thresholds of students in the second, eighth, and twelfth grades. Lang Speech Hear Serv Sch. 1992;23:61–3. [Google Scholar]
- 20.Gissel S, Mortensen JT, Juul S. Evaluation of hearing ability in Danish children at the time of school start and at the end of school. Int J Adolesc Med Health. 2002;14:43–9. doi: 10.1515/ijamh.2002.14.1.43. [DOI] [PubMed] [Google Scholar]
- 21.Shargorodsky J, Curhan SG, Curhan GC, Eavey R. Change in prevalence of hearing loss in US adolescents. JAMA. 2010;304:772–8. doi: 10.1001/jama.2010.1124. [DOI] [PubMed] [Google Scholar]
- 22.Persson BO, Svedberg A, Göthe CJ. Longitudinal changes in hearing ability among Swedish conscripts. Scand Audiol. 1993;22:141–3. doi: 10.3109/01050399309046030. [DOI] [PubMed] [Google Scholar]
- 23.Holmes AE, Niskar AS, Kieszak SM, Rubin C, Brody DJ. Mean and median hearing thresholds among children 6 to 19 years of age: the Third National Health And Nutrition Examination Survey, 1988 to 1994, United States. Ear Hear. 2004;25:397–402. doi: 10.1097/01.aud.0000134553.60120.3a. [DOI] [PubMed] [Google Scholar]
- 24.Rabinowitz PM, Slade MD, Galusha D, Dixon-Ernst C, Cullen MR. Trends in the prevalence of hearing loss among young adults entering an industrial workforce 1985 to 2004. Ear Hear. 2006;27:369–75. doi: 10.1097/01.aud.0000224125.12338.9a. [DOI] [PubMed] [Google Scholar]
- 25.Henderson E, Testa MA, Hartnick C. Prevalence of noise-induced hearing-threshold shifts and hearing loss among US youths. Pediatrics. 2011;127:e39–e46. doi: 10.1542/peds.2010-0926. [DOI] [PubMed] [Google Scholar]
- 26.Rosenstock IM. The Health Belief Model and preventive health behavior. Health Educ Monogr. 1974;2:354–86. [Google Scholar]
- 27.Rawool VW, Colligon-Wayne LA. Auditory lifestyles and beliefs related to hearing loss among college students in the USA. Noise Health. 2008;10:1–10. doi: 10.4103/1463-1741.39002. [DOI] [PubMed] [Google Scholar]
- 28.Chung JH, Des Roches CM, Meunier J, Eavey RD. Evaluation of noise-induced hearing loss in young people using a web-based survey technique. Pediatrics. 2005;115:861–7. doi: 10.1542/peds.2004-0173. [DOI] [PubMed] [Google Scholar]
- 29.Widen SE, Erlandsson SI. Self-reported tinnitus and noise sensitivity among adolescents in Sweden. Noise Health. 2004;7:29–40. [PubMed] [Google Scholar]
- 30.Widén SE, Holmes AE, Erlandsson SI. Reported hearing protection use in young adults from Sweden and the USA: Effects of attitude and gender. Int J Audiol. 2006;45:273–80. doi: 10.1080/14992020500485676. [DOI] [PubMed] [Google Scholar]
- 31.Bohlin MC, Erlandsson SI. Risk behaviour and noise exposure among adolescents. Noise Health. 2007;9:55–63. doi: 10.4103/1463-1741.36981. [DOI] [PubMed] [Google Scholar]
- 32.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. [Google Scholar]
- 33.Widén SE. A suggested model for decision-making regarding hearing conservation: Towards a systems theory approach. Int J Audiol. 2013;52:57–64. doi: 10.3109/14992027.2012.728724. [DOI] [PubMed] [Google Scholar]
- 34.Gilliver M, Carter L, Macoun D, Rosen J, Williams W. Music to whose ears? The effect of social norms on young people's risk perceptions of hearing damage resulting from their music listening behavior. Noise Health. 2012;14:47–51. doi: 10.4103/1463-1741.95131. [DOI] [PubMed] [Google Scholar]
- 35.Peters RJ. The role of hearing protectors in leisure noise. Noise Health. 2003;5:47–55. [PubMed] [Google Scholar]
- 36.Gilles A, Paul Vde H. Effectiveness of a preventive campaign for noise-induced hearing damage in adolescents. Int J Pediatr Otorhinolaryngol. 2014;78:604–9. doi: 10.1016/j.ijporl.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 37.Weichbold V, Zorowka P. Effects of a hearing protection campaign on the discotheque attendance habits of high-school students. Int J Audiol. 2003;42:489–93. doi: 10.3109/14992020309081519. [DOI] [PubMed] [Google Scholar]
- 38.Weichbold V, Zorowka P. Can a hearing education campaign for adolescents change their music listening behavior? Int J Audiol. 2007;46:128–33. doi: 10.1080/14992020601126849. [DOI] [PubMed] [Google Scholar]
- 39.Svensson EB, Morata TC, Nylén P, Krieg EF, Johnson AC. Beliefs and attitudes among Swedish workers regarding the risk of hearing loss. Int J Audiol. 2004;43:585–93. doi: 10.1080/14992020400050075. [DOI] [PubMed] [Google Scholar]
- 40.Jokitulppo J, Toivonen M, Björk E. Estimated leisure-time noise exposure, hearing thresholds, and hearing symptoms of Finnish conscripts. Mil Med. 2006;171:112–6. doi: 10.7205/milmed.171.2.112. [DOI] [PubMed] [Google Scholar]
- 41.Keppler H. Ghent (Belgium): Ghent University; 2010. Optimization of the Diagnosis of Noise-Induced Hearing Loss with Otoacoustic Emissions; pp. 137–40. [Google Scholar]
- 42.Keppler H, Dhooge I, Vinck B. Hearing in young adults. Part II: The effects of recreational noise exposure. Noise Health. 2015 doi: 10.4103/1463-1741.165026. Submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Daniel E. Noise and hearing loss: A review. J Sch Health. 2007;77:225–31. doi: 10.1111/j.1746-1561.2007.00197.x. [DOI] [PubMed] [Google Scholar]
- 44.Widén SE, Erlandsson SI. The influence of socio-economic status on adolescent attitude to social noise and hearing protection. Noise Health. 2004;7:59–70. [PubMed] [Google Scholar]
- 45.Widen S, Bohlin M, Johansson I. Gender perspectives in psychometrics related to leisure time noise exposure and use of hearing protection. Noise Health. 2011;13:407–14. doi: 10.4103/1463-1741.90299. [DOI] [PubMed] [Google Scholar]
- 46.Widén SE, Holmes AE, Johnson T, Bohlin M, Erlandsson SI. Hearing, use of hearing protection, and attitudes towards noise among young American adults. Int J Audiol. 2009;48:537–45. doi: 10.1080/14992020902894541. [DOI] [PubMed] [Google Scholar]
- 47.Gilles A, Van Hal G, De Ridder D, Wouters K, Van de Heyning P. Epidemiology of noise-induced tinnitus and the attitudes and beliefs towards noise and hearing protection in adolescents. PLoS One. 2013;8:e70297. doi: 10.1371/journal.pone.0070297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Keppler H, Dhooge I, Degeest S, Vinck B. The effects of a hearing education programme on recreational noise exposure, attitudes and beliefs toward noise, hearing loss and hearing protector devices in young adults. Noise Health. 2015 doi: 10.4103/1463-1741.165028. Submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bockstael A, Keppler H, Botteldooren D. Musicians earplugs: Subjective appreciation and protection. Noise Health. 2015 doi: 10.4103/1463-1741.160688. Submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Biassoni EC, Serra MR, Richtert U, Joekes S, Yacci MR, Carignani JA, et al. Recreational noise exposure and its effects on the hearing of adolescents. Part II: Development of hearing disorders. Int J Audiol. 2005;44:74–85. doi: 10.1080/14992020500031728. [DOI] [PubMed] [Google Scholar]
- 51.Schmuziger N, Patscheke J, Probst R. An assessment of threshold shifts in nonprofessional pop/rock musicians using conventional and extended high-frequency audiometry. Ear Hear. 2007;28:643–8. doi: 10.1097/AUD.0b013e31812f7144. [DOI] [PubMed] [Google Scholar]
- 52.Mansfield JD, Baghurst PA, Newton VE. Otoacoustic emissions in 28 young adults exposed to amplified music. Br J Audiol. 1999;33:211–22. doi: 10.3109/03005369909090102. [DOI] [PubMed] [Google Scholar]


