Abstract
Excessive recreational noise exposure in young adults might result in noise-induced hearing loss (NIHL) and tinnitus. Inducing behavioral change in young adults is one of the aims of a hearing conservation program (HCP). The goal of the current study was to evaluate the effect of a hearing education program after 6 months in young adults in relation to knowledge regarding their individual hearing status. The results of a questionnaire regarding the weekly equivalent recreational noise exposure, attitudes and beliefs toward noise, and hearing loss and hearing protector devices (HPDs) were compared between both sessions. Seventy-eight young adults completed the questionnaire concerning recreational noise exposure, youth attitude to noise scale (YANS), and beliefs about hearing protection and hearing loss (BAHPHL). Their hearing status was evaluated based on admittance measures, audiometry, transient-evoked otoacoustic emissions (TEOAEs), and distortion-product otoacoustic emissions (DPOAEs). The main analysis consisted of a mixed model analysis of variance with dependent variables of either the noise exposure or the scores on (subscales of) YANS and BAHPHL. The independent variables were hearing status and session one versus session two. There was a significant decrease in recreational noise exposure and several (sub) scales of YANS and BAHPHL between both the sessions. This behavioral change resulted in a more frequent use of HPDs in 12% of the participants. However, the behavioral change was not completely related to the knowledge of young adults’ individual hearing status. To prevent hearing damage in young people, investing in HCPs is necessary, apart from regulating sound levels and its compliance at various leisure-time activities. Also, the long-term effect of HCPs and their most cost-efficient repetition rates should be further investigated.
Keywords: Attitudes, hearing education program, hearing protector devices (HPDs), recreational noise exposure, young adults
Introduction
Young people expose themselves frequently to high levels of noise during leisure-time activities,[1,2] in particular while visiting nightclubs and using personal music players (PMPs).[3,4,5,6,7,8,9] Excessive noise exposure might lead to damage predominantly on the cochlear outer hair cells resulting in noise-induced hearing loss (NIHL),[10] tinnitus, and sensitivity to loud sounds.[11,12,13,14] In young adults in Flanders (Belgium), it was found that already 7% have a noise-induced permanent threshold shift, between 73.5% and 85.9% experience temporary tinnitus, and 6.6-18.3% have chronic tinnitus due to recreational noise exposure.[9,15,16,17]
According to the health belief model[18] and theory of planned behavior,[19] health-related behavior of NIHL is determined by the vulnerability to and seriousness of NIHL, the perceived benefits of and experienced barriers to preventative action, social norms and self-efficacy. Young adults with a more problematic attitude regarding noise exposure had more deteriorated hearing than other subjects.[20] However, awareness of the consequences of hearing loss was not related to behavioral change[20] that can be regarded as risk-taking behavior.[21] As stated in Widen et al. health risk-taking behavior is a complex process in which biological, psychological, social, and cultural factors interact.[22] There is also a relation between hearing risk behavior and traditional risk behavior such as thrill-seeking, rebellious, reckless, and antisocial behavior,[23] or sensation-seeking behavior[24] and it might have similar characteristics as addiction behavior.[25]
In young people, there is still a great deal of unawareness and/or a lot of misconception regarding the effects of noise exposure.[26,27,28] Providing information and knowledge regarding recreational noise exposure can be important factors in inducing behavioral change.[22] Also, self-experienced symptoms might serve as a trigger for behavioral change[21] as those who report tinnitus and other hearing-related symptoms show more hearing protective behavior.[13] In recreational noise activities, direct control of noise levels as a method of hearing preservation is suggested, and limiting the frequency and duration of exposure and more specifically using hearing protector devices (HPDs) are valid options.[29] Nevertheless, up to 72% of young adults never wear HPDs[30] that can possibly be explained by the disadvantages of wearing HPDs, which are suggested in the literature to be the perceived pressure on the ears, uncomfortable feeling of HPDs, annoyance in wearing HPDs, and the self-perception of communication difficulties.[27,31] However, the exact reasons for not using HPDs in young adults seem to be insufficiently known.
Hearing conservation programs (HCPs) usually provide information regarding the effects of hearing loss, thus increasing the awareness of the risk of excessive noise exposure and knowledge concerning the availability and use of HPDs.[29] Some campaigns are found to induce behavioral change by increasing the intention of using or the use of HPDs.[32] Others however, failed to prove such an effect,[33] and also did not find listening behavior changes such as reducing exposures in discotheques[33,34] or the responsible use of PMPs.[32] Therefore, it is suggested to not only keep investing in HCPs but to undertake additional efforts from legislators and health care providers[34] as well as test hearing in young people to determine hearing acuity without only relying on self-reported hearing estimation in relation to the use of HPDs.[21,29]
The goal of the current study was to evaluate the effect of a hearing education program on the weekly equivalent recreational noise exposure, attitudes and beliefs toward noise, hearing loss, and HPD use after approximately 6 months following training in young adults and relate it to their knowledge regarding their individual hearing status measured using pure-tone audiometry and otoacoustic emissions (OAEs).
Methods
Study design
Seventy-eight young adults (68 females and 10 males) between 18 years and 30 years of age [mean 21.01 years, standard deviation (SD) 2.84 years] voluntary participated in this study consisting of two sessions. The mean time between the two sessions was 29.86 weeks (SD 5.11 weeks, range 21-46 weeks). At both sessions, a questionnaire regarding recreational noise exposure, attitudes and beliefs toward noise, hearing loss, and HPDs was administered. Further, the hearing status of both ears was evaluated during both sessions in a double-walled sound-attenuated booth. Hearing status was determined after otoscopic evaluation, using admittances measures, pure-tone audiometry, and registration of OAEs. Before each session, a noise-free period of at least 24 h was required for inclusion in the study. For further analysis of all hearing tests, one ear per subject was selected at random.
After the hearing tests of the first session, all subjects were individually informed about their hearing status based on the worst ear. Further, all subjects were educated about the risks of recreational noise exposure, the preventative actions to reduce the amount of exposure and intensity levels during exposure, and the benefits of and barriers for using HPDs. This education program was presented one-on-one between the audiologist and the subject using a structured slide show. It contained three major parts: Functioning of the normal auditory system, the effects of noise exposure on the auditory system, and the preventative measures including information regarding HPD. More specifically, the sensation of being less communicative and issues concerning the comfort and cost of different types of HPDs were discussed. The discussed types of HPDs intended for music exposure with regard to their cost were standard earplugs, premolded earplugs with flexible flanges, and custom-made earplugs. After this information was provided, five questions regarding the effects of noise exposure on hearing, the consequences of hearing loss, and benefits of and barriers to preventative action were formulated and answered by the participants to ensure that information of hearing education was understood. The five true or false statements were:
The environment is too loud if one has to shout over a distance of 1 m to be heard,
After prolonged loud noise exposure, it is sufficient to rest the ears for 1 h,
Hearing damage caused by loud noise exposure is always temporary,
Ears are less vulnerable if one is exposed frequently to loud noise, and
Hearing damage caused by excessive noise exposure can be prevented by wearing adequate hearing protectors.
After each answer was given by the participant, the statement was discussed in order to avoid any misunderstanding. The results of the individual hearing status were discussed using a color code whereby green, orange, and red indicated that all hearing tests in the worst ear were normal, one or two of the three hearing tests were abnormal, and all hearing tests were abnormal, respectively. Information regarding the hearing status lasted more or less 10 min while the educational part took about 20 min. Another 15 min was provided to answer individual questions of the subjects. The effect of the hearing education program was evaluated by comparing the results of the questionnaire between both the sessions.
The study was approved by the local ethical committee and all subjects signed the informed consent form in accordance with the statements of the Declaration of Helsinki.
Questionnaire
The questionnaire consisted of five parts based on the literature[2,22,35,36] and is described elsewhere more in detail.[9,20] It was pretested by a semi-structured interview on 30 subjects between 18 years and 30 years of age who were not included in the current study. The second refined version of the questionnaire was administered on paper to 31 different subjects in the same age range and evaluated. In summary, the first part questioned the subjective assessment of hearing, hearing-related symptoms, knowledge and concern of NIHL by recreational noise exposure as well as reasons for (not) using HPDs, or the willingness to use HPDs. Second, sources of recreational noise exposure were evaluated in the time spent per week or month (hours), the total time of exposure (in years), and the subjective estimation of loudness. The self-estimated loudness from sound levels of a normal conversation to sound levels that makes communication impossible corresponded to A-weighted equivalent sound pressure levels from 60 dBA to 100 dBA, respectively. These sound pressure levels, the time spent per week (in hours) per activity, and a 40-h reference value were used to calculate the weekly equivalent noise exposure (LAeq,w) per activity and for all activities. This method was adopted from Jokitulppo et al.[2] The third part consisted of questions about the use of PMPs. Fourth, attitudes regarding noise, hearing loss, and HPDs were evaluated by a modified version of the youth attitude to noise scale (YANS) and beliefs about hearing protection and hearing loss (BAHPHL).[37] The Dutch version of YANS consisted of 19 items that can be divided into four factors representing the attitudes toward noise associated with elements of youth culture (YANS-F1), the ability to concentrate in noisy environments (YANS-F2), daily noises (YANS-F3), and the intent to influence the sound environment (YANS-F4). In the second modified version of the YANS, two items were reformulated to enhance the reliability of the fourth factor.[37] Items of the Dutch version of the BAHPHL were reformulated focusing on youth and HPD usage during recreational noise exposure.[37] In this modified version of the BAHPHL, 24 items were used that were categorized into seven factors: Susceptibility to hearing loss (BAHPHL-F1), severity of consequences of hearing loss (BAHPHL-F2), benefits of preventive action (BAHPHL-F3), barriers to preventive action (BAHPHL-F4), behavioral intentions (BAHPHL-F5), social norms (BAHPHL-F6), and self-efficacy (BAHPHL-F7). Both YANS and BAHPHL were assessed using a five-degree Likert scale from “totally disagree” to “totally agree”; a higher score indicated a more positive, less desirable attitude or belief representing an attitude where noise or hearing loss was seen as unproblematic and the attitudes and beliefs regarding HPDs were worse. Finally, the last part of the questionnaire consisted of questions regarding the gender, age, education or profession, and parental employment.
Admittance measures
Inclusion criteria in the study were normal immitance values measured with an 85 dB sound pressure level (SPL) 226 Hz probe tone as well as the present ipsilateral and contralateral acoustic stapedial reflexes at 1.0 kHz (TympStar, Grason-Stadler Inc., Eden Prairie, Minnesota, USA).
Audiometric evaluation
The modified Hughson-Westlake method for air conduction thresholds at conventional octave frequencies of 0.25-8.0 kHz and half-octave frequencies of 3.0 kHz and 6.0 kHz were used for pure-tone audiometry (Orbiter 922 Clinical Audiometer, Madsen Electronics, Taastrup, Capital Region of Denmark, Denmark). Audiometry was performed in a double-walled sound-attenuated booth. Audiometry was considered normal if hearing thresholds at all individual frequencies were better than 20 dB HL in the selected ear (n = 65). Thus, 83% of the subjects’ selected ear had hearing thresholds better than 20 dB HL that was consistent with the age-corrected norms according to the 85th percentile of International Organization for Standardization (ISO) 7029.[38] The other subjects (n = 13) had abnormal audiometric results.
OAEs
Using the ILO 292 USB II module with calibrated probe and ILOv6 software (Otodynamics Ltd., Hatfield, Herfordshire, the UK), transient-evoked OAEs (TEOAEs) and distortion-product OAEs (DPOAEs) were registered. TEOAEs and DPOAEs were registered in a double-walled sound-attenuated booth.
TEOAEs were recorded using rectangular pulses of 80 μs at a rate of 50 clicks/s at an intensity of 80 ± 2 dBpeSPL according to the nonlinear differential method of stimulation. After 260 accepted sweeps with a noise artefact rejection setting of 4 mPa, emissions and noise amplitudes were determined in half-octave frequency bands centered at 1.0 kHz, 1.5 kHz, 2.0 kHz, 3.0 kHz, and 4.0 kHz. TEOAEs were considered present if the signal-to-noise ratio (SNR) per half-octave frequency band was at least 3 dB and TEOAE amplitudes fell within mean +/- one standard deviation according to the previously determined normative values[39] in at least four frequency bands in the selected ear (n = 37). The other ears (n = 41) showed absent TEOAEs.
DPOAEs using primary tone level combination L1/L2 = 65/55 dB SPL and primary tone frequency ratio f2/f1 = 1.22 with f2 range of 0.841–8.0 kHz at eight points per octave were measured. After the whole frequency range was looped until the noise amplitude per frequency fell below -5 dB SPL using a noise artifact rejection level of 6 mPa, emission and noise amplitudes were calculated in half-octave frequency bands with center frequencies 1.0 kHz, 1.5 kHz, 2.0 kHz, 3.0 kHz, 4.0 kHz, 6.0 kHz, and 8.0 kHz. DPOAEs were considered present if the SNR at half-octave frequency bands was at least 3 dB and DPOAE amplitudes were within mean +/- one standard deviation based on normative values[39] in at least five frequency bands in the selected ear (n = 50). The other ears (n = 28) presented absent DPOAEs.
Data analysis
Statistical analysis was performed using SPSS version 22 (SPSS Inc., IBM Corp., New York, USA). First, a mixed model analysis of variance (ANOVA) was performed. The dependent variables were either the weekly equivalent noise exposure for all activities and by each activity or the scores on (subscales of) YANS and BAHPHL. The independent variables were hearing status and sessions. The hearing status was categorized into normal versus abnormal audiometry or present versus absent TEOAEs and DPOAEs at the first session. One ear per subject was selected at random for all tests for statistical analysis. For the dependent variable “session,” there were two categories, namely, session one and session two. A significance level of P < 0.05 was used.
Further, Pearson correlation coefficients were calculated to explore the correlation between the difference in weekly equivalent noise exposure for all activities and attitudes between the first session and second session on the one hand and the age at the first session or time between both the sessions on the other hand (P < 0.05). Also, the regression equations were determined.
Third, between both the sessions, the effect of the difference in perceived hearing loss or temporary tinnitus after noise exposure and the difference in weekly equivalent noise exposure for all activities and in attitudes were evaluated using one-way ANOVA with post hoc least significant difference (LSD) (P < 0.05).
Finally, one-way ANOVA with LSD and Bonferroni correction was used to evaluate significant differences between the weekly equivalent noise exposure for all activities and the attitudes at the second session subtracted from those at the first session and increased use of HPDs between both the sessions (P < 0.017). More specifically, subjects with no change in the use of HPDs between both the sessions were compared to subjects showing an increased use of HPDs at the second session compared to the first session. In order to evaluate whether the reasons and willingness using HPDs differed between both the sessions, 2 × 2 contingency tables and a χ2 test were performed (P < 0.05).
Results
The calculated weekly equivalent noise exposure for all activities had a range of 51.54-86.20 dBA (mean 69.75 dB, SD 8.06 dB) and 43.60–89.83 dBA (mean 67.32 dB, SD 9.46 dB), respectively, at the first and second sessions. Concerning this weekly equivalent noise exposure for all activities, two-way ANOVA revealed no significant interaction effects between independent variables’ hearing status and sessions. There was, however, a statistical significant main effect of this weekly equivalent noise exposure for all activities between both the sessions (F(1,76) = 5.98, P < 0.05); it was on an average 2.54 dBA lower at the second session as compared to the first session. Table 1 reflects the calculated weekly equivalent noise exposure at every questioned activity for both the sessions. There was a statistically significant main effect of weekly equivalent noise exposure for the activity of visiting nightclubs or pubs between both the sessions [F(1, 67) = 7.63, P < 0.05] but no significant effect was seen for the other activities.
Table 1.
Percentage of subjects’ attendance (n = 78) and mean equivalent noise exposure (LAeq,w) in dBA by activity
| Activity | Session one | Session two | ||
|---|---|---|---|---|
| Attendance (%) | LAeq,w (dBA) | Attendance (%) | LAeq,w (dBA) | |
| Visiting nightclubs or pubs | 93.6 | 73.38* (11.52) | 91.0 | 70.34* (11.75) |
| Watching movies or plays | 89.7 | 55.20 (8.40) | 76.9 | 57.17 (10.61) |
| Listening to a PMP through headphones | 87.2 | 53.01 (9.01) | 75.6 | 55.09 (11.69) |
| Listening to a home stereo or radio | 84.6 | 57.26 (8.42) | 75.6 | 57.61 (8.31) |
| Attending musical concerts or festivals | 73.1 | 69.82 (9.01) | 46.2 | 67.63 (12.45) |
| Attending sport events | 53.8 | 55.99 (9.57) | 39.7 | 54.99 (10.47) |
| Practicing a musical instrument | 50.0 | 56.47 (8.75) | 30.8 | 55.06 (9.07) |
| Playing in a band or orchestra | 29.5 | 67.26 (11.26) | 10.3 | 73.19 (9.19) |
| Other noisy leisure-time activities | 19.2 | 62.67 (10.52) | 17.9 | 60.16 (6.45) |
| Using noisy tools | 12.8 | 63.57 (14.46) | 10.3 | 61.31 (9.33) |
| Watching television through headphones | 5.1 | 56.99 (2.46) | 3.8 | 56.63 (15.32) |
Significant difference in LAeq,w between both sessions is indicated with an asterisk
Table 2 reflects the mean and SD of (subscales of the) YANS and BAHPHL at the first session and second session. Two-way ANOVA revealed two significant interaction effects between the subscales of BAHPHL and hearing status based on audiometry and DPOAEs. Between the two sessions, the score on BAHPHL-F5 [Figure 1a] decreased significantly more for subjects with normal audiometry at the first session [F(1,76) = 4.35, P < 0.05] while the score on BAHPHL-F3 [Figure 1b] decreased significantly more for subjects with absent DPOAEs at the first session (F(1,76) = 10.30, P < 0.05). Further, significant main effects were seen between both sessions for several (sub) scales of YANS and BAHPHL. There was a significant decrease at YANS-F1 on an average of 0.17 between the first session and second session (F(1,76) = 13.39, P < 0.05). This effect was also significant for BAHPHL-F2 [F(1,76) = 4.28, P < 0.05], BAHPHL-F5 [F(1, 76) = 13.70, P < 0.05], BAHPHL-F6 [F(1,76) = 9.82, P < 0.05] and BAHPHL-F7 [F(1, 76) = 18.42, P < 0.05]. These results are illustrated in Figure 2. No significant main effects between normal versus abnormal audiometry, or present or absent TEOAEs and DPOAEs were revealed for (subscales of) YANS and BAHPHL.
Table 2.
For (subscales of) YANS and BAHPHL, mean, standard deviation (SD), and range during the first session and second session are reflected (n = 78)
| Questionnaire | Session one | Session two | |||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Range | Mean | SD | Range | ||
| YANS | |||||||
| F1 | Elements of youth culture* | 2.22 | 0.55 | 1.13-4.00 | 2.05 | 0.45 | 1.25-3.25 |
| F2 | Concentrate in noisy environment | 2.44 | 0.86 | 1.00-4.67 | 2.52 | 0.92 | 1.00-4.67 |
| F3 | Daily noises | 3.26 | 0.78 | 1.75-5.00 | 3.36 | 0.74 | 1.75-5.00 |
| F4 | Intent to influence the sound environment | 1.86 | 0.59 | 1.00-3.50 | 1.88 | 0.55 | 1.00-3.25 |
| Total | 2.40 | 0.41 | 1.37-3.79 | 2.36 | 0.37 | 1.53-3.68 | |
| BAHPHL | |||||||
| F1 | Susceptibility to hearing loss | 1.59 | 0.46 | 1.00-3.00 | 1.51 | 0.38 | 1.00-2.67 |
| F2 | Severity of consequences of hearing loss* | 1.54 | 0.56 | 1.00-4.00 | 1.38 | 0.47 | 1.00-2.67 |
| F3 | Benefits of preventive action | 1.68 | 0.53 | 1.00-3.67 | 1.56 | 0.50 | 1.00-3.00 |
| F4 | Barriers to preventive action | 2.84 | 0.82 | 1.00-4.75 | 2.80 | 0.85 | 1.00-4.75 |
| F5 | Behavioral intentions* | 2.66 | 1.08 | 1.00-5.00 | 2.30 | 1.06 | 1.00-5.00 |
| F6 | Social norms* | 3.36 | 0.93 | 1.00-5.00 | 3.01 | 0.99 | 1.00-5.00 |
| F7 | Self-efficacy* | 2.80 | 0.72 | 1.00-4.33 | 2.43 | 0.78 | 1.00-5.00 |
Significant differences in scores between both the sessions are indicated with an asterisk
Figure 1.
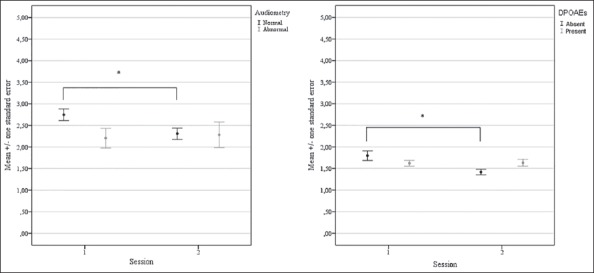
For both the sessions, the mean (+/- 1 standard error) scores on BAHPHL-F5 for subjects with normal versus abnormal audiometry (a) and BAHPHL-F3 for subjects with present versus absent DPOAEs (b). An asterisk indicates significant differences
Figure 2.
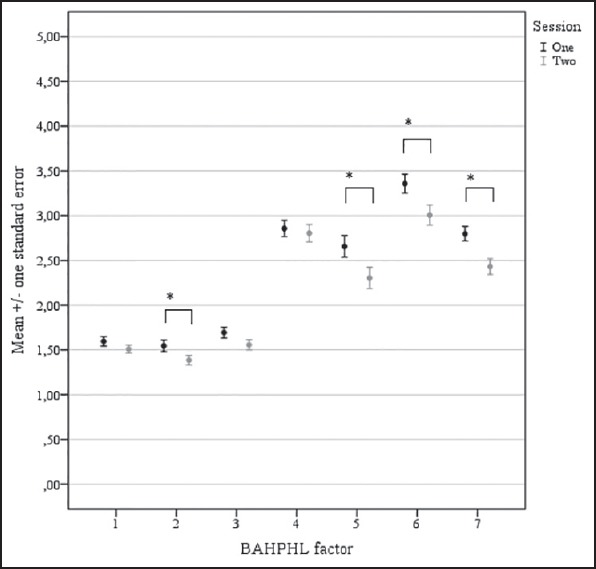
Mean +/- 1 standard error of the scores on the different BAHPHL factors for both sessions. Significant results are marked with an asterisk
Second, there were no significant results between the difference in weekly equivalent noise exposure for all activities between both sessions and age at the first session. However, there was a significant negative correlation between the differences in YANS-F1 (r = −0.28, P < 0.05) and BAHPHL-F5 (r = −0.34, P < 0.05) between both sessions on the one hand and age in the first session on the other hand. However, according to the regression equations for YANS-F1 (y = 1.03-0.04x) and BAHPHL-F5 (y = 2.43-0.1x), the time between both the sessions was too small to explain the change in attitudes with advancing age. Further, there were neither a significant correlation between the difference in noise exposure and time between both the sessions nor between the differences of the scores (on the subscales) of YANS and BAHPHL and time between both the sessions.
Third, between both the sessions, 22 (28.2%) subjects reported an increase in perceived hearing loss while 35 (44.9%) and 21 (26.9%) subjects indicated no change or a decrease in perceived hearing loss, respectively. With regard to temporary tinnitus between both the sessions, 16 (20.5%) subjects mentioned an increase in temporary tinnitus in contrast to 35 (44.9%) and 27 (34.6%) subjects reporting no change or a decrease in temporary tinnitus, respectively. There were no significant results between the differences in the calculated weekly equivalent noise exposure for all activities and scores on the attitude (sub) scales between both sessions, and an increase in perceived hearing loss or in temporary tinnitus after noise exposure between the first session and second session.
Fourth, the difference in the weekly equivalent noise exposure for all activities and the attitudes between both the sessions was calculated. Between both the sessions, subjects with no change in the use of HPDs (n = 65) and subjects with increased use of HPDs (n = 9) were determined. The ANOVA indicated that there was no significant difference in weekly equivalent recreational noise exposure for all activities between both the sessions depending on the increased use of HPDs at the second session. However, the differences in YANS-F1 [F(2, 77) = 6.38, P < 0.05], BAHPHL-F5 [F(2, 77) = 8.29, P < 0.05] and BAHPHL-F7 [F(2, 77) = 6.54, P < 0.05] between both the sessions was significantly higher, indicating a less positive attitude regarding noise, hearing loss, or HPDs for subjects using HPDs more often between the first session and second session [Table 3]. Reasons for using HPDs between both the sessions increased significantly due to concern for hearing-related symptoms (χ2 (1) = 6.24, P < 0.05) but not due to loudness of leisure noise activities. Reasons for not using HPDs between both the sessions increased significantly due to the cost of HPDs (χ2 (1) = 9.28, P < 0.05) but not related to the comfort, looks, music quality, speech understanding, or necessity of HPDs. The willingness in using HPDs between the two sessions was not significantly different if HPDs were distributed for free, if hearing damage was diagnosed, or if HPDs were legally required. These results are reflected in Table 4.
Table 3.
Mean and standard deviation (between brackets) are reflected for (subscales of) YANS, BAHPHL, and weekly equivalent noise exposure (LAeq,w) in dBA in both the sessions and for subjects with decreased (n = 4), no change in (n = 65), and increased (n = 9) use of HPDs
| Questionnaire | Session | Use of HPDs | ||||
|---|---|---|---|---|---|---|
| Decreased | No change | Increased | ||||
| YANS | F1 | Elements of youth culture | 1 | 1.94 (0.22) | 2.18 (0.55)* | 2.64 (0.46)* |
| 2 | 1.81 (0.26) | 2.07 (0.44)* | 2.03 (0.57)* | |||
| F2 | Concentrate in noisy environment | 1 | 2.25 (0.83) | 2.45 (0.86) | 2.52 (0.90) | |
| 2 | 2.42 (1.29) | 2.49 (0.93) | 2.74 (0.72) | |||
| F3 | Daily noises | 1 | 3.06 (0.43) | 3.23 (0.80) | 3.50 (0.80) | |
| 2 | 3.31 (0.63) | 3.33 (0.76) | 3.58 (0.56) | |||
| F4 | Intent to influence sound environment | 1 | 1.44 (0.43) | 1.89 (0.58) | 1.83 (0.68) | |
| 2 | 1.38 (0.32) | 1.89 (0.55) | 2.03 (0.52) | |||
| Total | 1 | 2.12 (0.17) | 2.38 (0.42) | 2.63 (0.36) | ||
| 2 | 2.13 (0.41) | 2.36 (0.38) | 2.47 (0.29) | |||
| BAHPHL | F1 | Susceptibility to hearing loss | 1 | 1.46 (0.58) | 1.60 (0.46) | 1.57 (0.43) |
| 2 | 1.21 (0.21) | 1.52 (0.39) | 1.54 (0.39) | |||
| F2 | Severity of consequences of hearing loss | 1 | 1.75 (1.50) | 1.55 (0.49) | 1.33 (0.41) | |
| 2 | 1.00 (0.00) | 1.42 (0.48) | 1.33 (0.44) | |||
| F3 | Benefits of preventive action | 1 | 1.42 (0.32) | 1.69 (0.53) | 1.78 (0.55) | |
| 2 | 1.17 (0.33) | 1.61 (0.51) | 1.33 (0.37) | |||
| F4 | Barriers to preventive action | 1 | 3.06 (1.25) | 2.80 (0.79) | 2.97 (0.93) | |
| 2 | 3.13 (1.36) | 2.78 (0.79) | 2.83 (1.08) | |||
| F5 | Behavioral intentions | 1 | 2.50 (0.58) | 2.58 (1.11)* | 3.30 (0.79)* | |
| 2 | 2.83 (0.58) | 2.31 (1.09)* | 2.04 (1.01)* | |||
| F6 | Social norms | 1 | 3.38 (1.11) | 3.26 (0.93) | 4.06 (0.63) | |
| 2 | 3.50 (1.08) | 2.96 (1.01) | 3.11 (0.86) | |||
| F7 | Self-efficacy | 1 | 2.67 (0.72) | 2.70 (0.67)* | 3.56 (0.73)* | |
| 2 | 2.92 (1.40) | 2.40 (0.77)* | 2.44 (0.44)* | |||
| LAeq,w | 1 | 65.98 (8.67) | 70.55 (8.13) | 69.39 (9.45) | ||
| 2 | 64.66 (12.30) | 67.49 (9.83) | 70.05 (9.95) | |||
Significant results between the difference in scores of attitudes and noise exposure at both sessions for different usage of HPDs are marked with an asterisk
Table 4.
Percentage of subjects indicating the wearing of HPDs (1-2), not wearing of HPDs (3-8), or willing to use HPDs (9-11) between the two sessions
| Item number | Item | Session one (%) | Session two (%) |
|---|---|---|---|
| 1 | Concern for hearing-related symptoms* | 46.3 | 69.5 |
| 2 | Loudness of leisure noise exposure | 63.0 | 74.6 |
| 3 | Cost of HPDs* | 16.7 | 38.5 |
| 4 | Comfort of HPDs | 37.2 | 26.9 |
| 5 | Looks of HPDs | 10.3 | 7.7 |
| 6 | Music quality using HPDs | 17.9 | 17.9 |
| 7 | Speech understanding using HPDs | 35.9 | 30.8 |
| 8 | Necessity of HPDs | 6.4 | 6.4 |
| 9 | Free distribution | 58.4 | 66.7 |
| 10 | Hearing damage | 85.7 | 87.2 |
| 11 | Legally required | 55.8 | 67.9 |
Significant differences in percentages between both the sessions are indicated with an asterisk
Discussion
Excessive recreational noise exposure in young adults might result in NIHL, as well as noise-induced tinnitus. Previous research indicated that young adults’ hearing status was significantly worse for those with a more problematic attitude regarding noise, hearing loss, and HPDs.[20] Behavior related to NIHL depends on the vulnerability to and seriousness of NIHL, the perceived benefits of and experienced barriers to preventative action, social norms, and self-efficacy.[18,19] Improvement of knowledge regarding NIHL and the willingness to use HPDs play an important role in inducing behavioral change in young adults through the use of HCPs. Nevertheless, listening behavior or the limited use of HPDs after such campaigns remain worrisome.[32,33,34]
Therefore, this study investigated the change in listening behavior and attitudes regarding noise, hearing loss, and HPDs after a hearing education program in young adults who were aware of their individual hearing status. At two sessions separated by approximately 6 months, the hearing status was extensively measured based on admittance measures, audiometry; a questionnaire regarding recreational noise exposure as well as YANS and BAHPHL were administered. At the first session, subjects were informed about their hearing, and information regarding the risks of recreational noise exposure, preventative actions to reduce the amount of exposure and intensity levels during exposure, and the benefits of and barriers using HPDs were discussed.
With regard to recreational noise exposure, visiting nightclubs or pubs was not only attended most by our subjects, it was also calculated as the highest weekly equivalent noise exposure. This in consistent with previous literature concluding that those activities might be more dangerous than using PMPs.[40] Nevertheless, the effects of listening to PMPs cannot be underestimated, especially in our subjects ranging in age from 18 to 30 years of which it is assumed that the use of PMPs is decreased as compared to younger adults.[1]
In this study, the lowest and highest average scores of YANS were found for the factors associated with intent to influence sound environment and daily noise. For BAHPHL, the factor with the lowest average was related to the severity of consequences of hearing loss; the one with the highest average to social norms. This, as well as the — not per se socially desirable — ranges of scores on YANS and BAHPHL was found previously.[15,20]
Between the two sessions, there were no (consistent) significant effects between recreational noise exposure or attitudes and beliefs on the one hand, and hearing status at the first session on the other hand. More specifically, for the factor of the BAHPHL associated with behavioral intentions, the score decreased significantly between both sessions for subjects with normal audiometry at the first session. Possibly, subjects with preserved hearing are motivated to maintain their normal hearing status. In contrast, for the factor of the BAHPHL associated with benefits of preventative action, the score between both sessions decreased significantly for subjects with absent DPOAEs perhaps because they estimate the benefits of preventative action more beneficial than other subjects. Since these effects are only seen on two subscales of YANS and BAHPHL, young adults’ knowledge of their hearing status seems only to have a small impact on behavioral change. It is, therefore, not necessary to verify hearing acuity extensively using admittance measure, audiometry, and OAEs in young people to increase behavioral change. Nevertheless, young adults frequently exposed to hazardous noise levels should be diagnosed as early as possible to provide auditory rehabilitation services to those who suffer from tinnitus, hypersensitivity, or hearing loss. Further, the current study did not investigate whether hearing screening techniques in HCPs can be necessary to identify individuals who are at risk of hearing loss.
In the current study, there was a significant decrease in weekly equivalent recreational noise exposure. This derived weekly equivalent noise exposure was based on a retrospective estimation of recreational noise exposure in hours per week or month, number of years, and subjective estimation of loudness per leisure-time activity that might have led to errors in the exact weekly equivalent noise exposure. Nevertheless, young adults determine the loudness of recreational events reasonably well[41] and for this study, the relative ranking of loudness of activities and the difference between the two sessions was of importance. Further, there was a significant decrease in the score on the YANS factor associated with elements of youth culture and the score on the BAHPHL factors related to the severity of consequences of hearing loss, behavioral intentions, social norms, and self-efficacy. Since this effect was not noted on all factors of YANS and BAHPHL and some factors yielded to negative as well as positive mean differences between both the sessions, an effect of familiarity or answering the questions more desirably to meet the expectations of the researchers was not found. Further, test-retest variability of YANS and BAHPHL cannot explain the differences found between both the sessions. With regard to the test-retest variability of YANS, mean values smaller than 0.002 are reported.[42,43] In the current study, all mean differences of YANS between the first session and second session exceeded this mean test-retest difference. Moreover, the significant differences in weekly equivalent noise exposure and in scores (on the subscales) of YANS and BAHPHL were neither related to age in the first session nor time between both the sessions. In contrast, the score on the BAHPHL factor related to the susceptibility to hearing loss was not significantly different between both the sessions. This might indicate that young adults, even after being aware of their individual hearing status, deny possible hearing loss because the consequences are not perceived as serious enough. Further, self-experienced hearing-related symptoms such as temporary tinnitus are believed to trigger behavioral change.[21] In the current study however, the change in attitudes and beliefs between both the sessions was not associated with an increase in subjectively perceived hearing loss or in temporary tinnitus after noise exposure at the second session. Therefore, the found behavioral change was induced by hearing education and translated directly into more frequent use of HPDs in 11.54% of the participants.
Although increased (intentions to) use (of) HPDs after a hearing prevention campaign was also found previously,[32] reasons for not using HPDs in young adults are not clear. The current study questioned several factors related to the (un) willingness to use HPDs. It was found that young adults use HPDs in the second session more often due to concern for hearing-related symptoms such as tinnitus and sensitivity to sound but are reluctant to use HPDs in the second session due to its cost. This could be related to a possible increased knowledge of the actual prices of different types of HPDs due to the hearing education, whereas in the first session subjects could have been unfamiliar with the cost of HPDs. Nevertheless, the number of subjects willing to use HPDs if they were distributed for free was 66.7% in the second session, indicating that one-third of the subjects still persevered in hearing risk behavior. Comfort, looks, and communication skills while wearing HPDs are also important. However, it should be emphasized that premolded earplugs targeting music exposure are well appreciated but the objective attenuation depends on variation in the design of the earplug.[44] Thus, more efforts should be undertaken for the design, looks, marketing and packaging of HPDs targeting recreational noise exposure in young adults[44] as well as their availability at a relatively low cost.
Although an effect of hearing education was found on all aspects of a more hearing preserved behavior, it is unclear if these results are stable over a longer span. According to the five stages of change,[45] the current study focuses on the action stage already passing through the (pre)contemplation and decision-making stage. However, it is unknown if our subjects engage in this new behavior for more than 6 months to an indeterminate period resulting in the maintenance stage. These long-term effects of hearing prevention campaigns and the most cost-efficient repetition rate of HCPs should be further investigated.
Nevertheless, apart from investing in (repetition of) HCPs for young people, control of noise levels during recreational activities is still the primary option for hearing preservation.[29] Since the current weekly equivalent noise exposure is dominated by visiting nightclubs and pubs, the importance of noise level limitations are stressed and recommended. This comprises not only a regulation of sound levels at indoor and outdoor music venues that were established in Flanders (Belgium),[46] but also supervision of the compliance with this legislation.
Conclusion
In conclusion, the change in listening behavior and attitudes regarding self-reported noise exposure, hearing loss, and HPDs after a hearing education program in young adults does not completely rely on knowledge of their hearing status. There was an effect of hearing education on all aspects of a more hearing preserved behavior that was translated directly into more frequent use of HPDs in 12% of the participants.
However, the current study would have strengthened the differences found in the listening behavior and attitudes regarding self-reported noise exposure, hearing loss, and HPDs after a hearing education program if a noneducational group was included or more information regarding the test-retest variability of the used Dutch version of YANS and BAHPHL was available. Nevertheless, legislators and health care providers should keep investing in HCPs, with emphas on the availability of relatively low budget premolded earplugs designed for music exposure. HCPs should be available for all youth, for example, by implementing it in the curriculum of high schools. Manufacturers of earplugs should target young adults more by improving the design, looks, marketing, and packaging of earplugs. Meanwhile better education programs to increase the percentage of young adults willing to use HPDs, the long-term effects of such campaigns, and their most cost-efficient repetition rates should be investigated. Finally, the regulation of sound levels and its compliance should be supervised by the government.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
Keppler Hannah was funded during this research project through an Aspirant Scholarship of the Research Foundation - Flanders (FWO), Belgium.
References
- 1.Smith PA, Davis A, Ferguson MA, Lutman ME. The prevalence and type of social noise exposure in young adults in England. Noise Health. 2000;2:41–56. [PubMed] [Google Scholar]
- 2.Jokitulppo J, Toivonen M, Björk E. Estimated leisure-time noise exposure, hearing thresholds, and hearing symptoms of Finnish conscripts. Mil Med. 2006;171:112–6. doi: 10.7205/milmed.171.2.112. [DOI] [PubMed] [Google Scholar]
- 3.Meecham EA, Hume KI. Tinnitus, attendance at night-clubs and social drug taking in students. Noise Health. 2001;3:53–62. [PubMed] [Google Scholar]
- 4.Petrescu N. Loud music listening. Mcgill J Med. 2008;11:169–76. [PMC free article] [PubMed] [Google Scholar]
- 5.Twardella D, Wellhoefer A, Brix J, Fromme H. High sound pressure levels in Bavarian discotheques remain after introduction of voluntary agreements. Noise Health. 2008;10:99–104. doi: 10.4103/1463-1741.44348. [DOI] [PubMed] [Google Scholar]
- 6.Williams W, Beach EF, Gilliver M. Clubbing: The cumulative effect of noise exposure from attendance at dance clubs and night clubs on whole-of-life noise exposure. Noise Health. 2010;12:155–8. doi: 10.4103/1463-1741.64970. [DOI] [PubMed] [Google Scholar]
- 7.Keppler H, Dhooge I, Maes L, D’haenens W, Bockstael A, Philips B, et al. Short-term auditory effects of listening to an MP3 player. Arch Otolaryngol Head Neck Surg. 2010;136:538–48. doi: 10.1001/archoto.2010.84. [DOI] [PubMed] [Google Scholar]
- 8.Serra MR, Biassoni EC, Hinalaf M, Abraham M, Pavlik M, Villalobo JP, et al. Hearing and loud music exposure in 14-15 years old adolescents. Noise Health. 2014;16:320–30. doi: 10.4103/1463-1741.140512. [DOI] [PubMed] [Google Scholar]
- 9.Keppler H, Dhooge I, Vinck BM. Hearing in young adults. Part II: The effects of recreational noise exposure. Noise Health. 2015 doi: 10.4103/1463-1741.165026. [In Press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Michigan, USA: Amercian College of Occupational and Environmental Medicine; 2002. American College of Occupational and Environmental Medicine. Position Statement: Noise-Induced Hearing Loss; pp. 1–4. [Google Scholar]
- 11.Davis AC, Lovell EA, Smith PA, Ferguson MA. The contribution of social noise to tinnitus in young people — A preliminary report. Noise Health. 1998;1:40–6. [PubMed] [Google Scholar]
- 12.Axelsson A, Prasher D. Tinnitus induced by occupational and leisure noise. Noise Health. 2000;2:47–54. [PubMed] [Google Scholar]
- 13.Widén SE, Erlandsson SI. Self-reported tinnitus and noise sensitivity among adolescents in Sweden. Noise Health. 2004;7:29–40. [PubMed] [Google Scholar]
- 14.Bohlin MC, Erlandsson SI. Risk behaviour and noise exposure among adolescents. Noise Health. 2007;9:55–63. doi: 10.4103/1463-1741.36981. [DOI] [PubMed] [Google Scholar]
- 15.Gilles A, De Ridder D, Van Hal G, Wouters K, Kleine Punte A, Van de Heyning P. Prevalence of leisure noise-induced tinnitus and the attitude toward noise in university students. Otol Neurotol. 2012;33:899–906. doi: 10.1097/MAO.0b013e31825d640a. [DOI] [PubMed] [Google Scholar]
- 16.Gilles A, Van Hal G, De Ridder D, Wouters K, Van de Heyning P. Epidemiology of noise-induced tinnitus and the attitudes and beliefs towards noise and hearing protection in adolescents. PLoS One. 2013;8:e70297. doi: 10.1371/journal.pone.0070297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Degeest S, Corthals P, Vinck BM, Keppler H. Prevalence and characteristics of tinnitus after leisure noise exposure in young adults. Noise Health. 2014;16:26–33. doi: 10.4103/1463-1741.127850. [DOI] [PubMed] [Google Scholar]
- 18.Rosenstock IM. The health belief model and preventive health behavior. Health Educ Monogr. 1974;2:354–86. [Google Scholar]
- 19.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. [Google Scholar]
- 20.Keppler H, Dhooge I, Vinck BM. Hearing in young adults. Part I: The effects of attitudes and beliefs toward noise, hearing loss and hearing protector devices. Noise Health. 2015 doi: 10.4103/1463-1741.165024. [In Press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Widen SE, Holmes AE, Johnson T, Bohlin MC, Erlandsson SI. Hearing, use of hearing protection, and attitudes towards noise among young American adults. Int J Audiol. 2009;48:537–45. doi: 10.1080/14992020902894541. [DOI] [PubMed] [Google Scholar]
- 22.Widen SE, Holmes AE, Erlandsson SI. Reported hearing protection use in young adults from Sweden and the USA: Effects of attitude and gender. Int J Audiol. 2006;45:273–80. doi: 10.1080/14992020500485676. [DOI] [PubMed] [Google Scholar]
- 23.Bohlin MC, Sorbring E, Widén SE, Erlandsson SI. Risks and music - Patterns among young women and men in Sweden. Noise Health. 2011;13:310–9. doi: 10.4103/1463-1741.82964. [DOI] [PubMed] [Google Scholar]
- 24.Hétu R, Fortin M. Potential risk of hearing damage associated with exposure to highly amplified music. J Am Acad Audiol. 1995;6:378–86. [PubMed] [Google Scholar]
- 25.Florentine M, Hunter W, Robinson M, Ballou M, Buus S. On the behavioral characteristics of loud-music listening. Ear Hear. 1998;19:420–8. doi: 10.1097/00003446-199812000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Weichbold V, Zorowka P. Effect of information about hearing damage caused by loud music. For adolescents the music in discoteques is too loud despite loudness limits. HNO. 2002;50:560–4. doi: 10.1007/s00106-001-0578-4. [DOI] [PubMed] [Google Scholar]
- 27.Rawool VW, Colligon-Wayne LA. Auditory lifestyles and beliefs related to hearing loss among college students in the USA. Noise Health. 2008;10:1–10. doi: 10.4103/1463-1741.39002. [DOI] [PubMed] [Google Scholar]
- 28.Shah S, Gopal B, Reis J, Novak M. Hear today, gone tomorrow: An assessment of portable entertainment player use and hearing acuity in a community sample. J Am Board Fam Med. 2009;22:17–23. doi: 10.3122/jabfm.2009.01.080033. [DOI] [PubMed] [Google Scholar]
- 29.Peters RJ. The role of hearing protectors in leisure noise. Noise Health. 2003;5:47–55. [PubMed] [Google Scholar]
- 30.Crandell C, Mills TL, Gauthier R. Knowledge, behaviors, and attitudes about hearing loss and hearing protection among racial/ethnically diverse young adults. J Natl Med Assoc. 2004;96:176–86. [PMC free article] [PubMed] [Google Scholar]
- 31.Daniel E. Noise and hearing loss: A review. J Sch Health. 2007;77:225–31. doi: 10.1111/j.1746-1561.2007.00197.x. [DOI] [PubMed] [Google Scholar]
- 32.Gilles A, Paul Vde H. Effectiveness of a preventive campaign for noise-induced hearing damage in adolescents. Int J Pediatr Otorhinolaryngol. 2014;78:604–9. doi: 10.1016/j.ijporl.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 33.Weichbold V, Zorowka P. Effects of a hearing protection campaign on the discotheque attendance habits of high-school students. Int J Audiol. 2003;42:489–93. doi: 10.3109/14992020309081519. [DOI] [PubMed] [Google Scholar]
- 34.Weichbold V, Zorowka P. Can a hearing education campaign for adolescents change their music listening behavior? Int J Audiol. 2007;46:128–33. doi: 10.1080/14992020601126849. [DOI] [PubMed] [Google Scholar]
- 35.Svensson EB, Morata TC, Nylén P, Krieg EF, Johnson AC. Beliefs and attitudes among Swedish workers regarding the risk of hearing loss. Int J Audiol. 2004;43:585–93. doi: 10.1080/14992020400050075. [DOI] [PubMed] [Google Scholar]
- 36.Ahmed S, Fallah S, Garrido B, Gross A, King M, Morrish T, et al. Use of portable audio devices by university students. Can Acoust. 2007;35:35–52. [Google Scholar]
- 37.Keppler H. Ghent (Belgium): Ghent University; 2010. Optimization of the diagnosis of noise-induced hearing loss with otoacoustic emissions (dissertation) pp. 137–40. [Google Scholar]
- 38.International Organization for Standardization 7029. Acoustics — Statistical distributions of hearing thresholds as a function of age. 2000:1–18. [Google Scholar]
- 39.Keppler H, Dhooge I, Corthals P, Maes L, D’haenens W, Bockstael A, et al. The effects of aging on evoked otoacoustic emissions and efferent suppression of transient evoked otoacoustic emissions. Clin Neurophysiol. 2010;121:359–65. doi: 10.1016/j.clinph.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 40.Serra MR, Biassoni EC, Richter U, Minoldo G, Franco G, Abraham S, et al. Recreational noise exposure and its effects on the hearing of adolescents. Part I: An interdisciplinary long-term study. Int J Audiol. 2005;44:65–73. doi: 10.1080/14992020400030010. [DOI] [PubMed] [Google Scholar]
- 41.Beach EF, Williams W, Gilliver M. The objective-subjective assessment of noise: Young adults can estimate loudness of events and lifestyle noise. Int J Audiol. 2012;51:444–9. doi: 10.3109/14992027.2012.658971. [DOI] [PubMed] [Google Scholar]
- 42.Zocoli AM, Morata TC, Marques JM. Youth attitude to noise scale (YANS) questionnaire adaptation into Brazilian Portuguese. Braz J Otorhinolaryngol. 2009;75:485–92. doi: 10.1016/S1808-8694(15)30484-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhu X, Bihi A, Hu X, Lv Y, Abbas A, Zhu X, et al. Chinese-adapted youth attitude to noise scale: Evaluation of validity and reliability. Noise Health. 2014;16:218–22. doi: 10.4103/1463-1741.137055. [DOI] [PubMed] [Google Scholar]
- 44.Bockstael A, Keppler H, Botteldooren D. Musicians earplugs: Appreciation and protection. Noise Health. 2015;17:198–208. doi: 10.4103/1463-1741.160688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Norcross JC, Krebs PM, Prochaska JO. Stages of change. J Clin Psychol. 2011;67:143–54. doi: 10.1002/jclp.20758. [DOI] [PubMed] [Google Scholar]
- 46.Flemish Government (Belgium) — Department of Environment, Nature and Energy. Technical Manual - New regulation for noise during musical activities. [Last accessed on 2015 Feb]. Available from: http://www.lne.be/themas/hinder-en-risicos/geluidshinder/beleid/muziek/technische_handleiding_geluidsnormen.pdf .


