Abstract
Associations between road traffic noise and hypertension have been repeatedly documented, whereas associations with rail or total road, rail, and air (RRA) traffic noise have rarely been investigated. Moreover, most studies of noise in the environment have only taken into account the residential neighborhood. Finally, few studies have taken into account individual/neighborhood confounders in the relationship between noise and hypertension. We performed adjusted multilevel regression analyses using data from the 7,290 participants of the RECORD Study to investigate the associations of outdoor road, rail, air, and RRA traffic noise estimated at the place of residence, at the workplace, and in the neighborhoods around the residence and workplace with systolic blood pressure (SBP), diastolic blood pressure (DBP), and hypertension. Associations were documented between higher outdoor RRA and road traffic noise estimated at the workplace and a higher SBP [+1.36 mm of mercury, 95% confidence interval (CI): +0.12, +2.60 for 65-80 dB(A) vs 30-45 dB(A)] and DBP [+1.07 (95% CI: +0.28, +1.86)], after adjustment for individual/neighborhood confounders. These associations remained after adjustment for risk factors of hypertension. Associations were documented neither with rail traffic noise nor for hypertension. Associations between transportation noise at the workplace and blood pressure (BP) may be attributable to the higher levels of road traffic noise at the workplace than at the residence. To better understand why only noise estimated at the workplace was associated with BP, our future work will combine Global Positioning System (GPS) tracking, assessment of noise levels with sensors, and ambulatory monitoring of BP.
Keywords: Blood pressure (BP), neighborhood environments, residence and workplace, transportation noise
Introduction
Transportation noise is reported as the first source of nuisance in the urban area of the Île-de-France (Paris) region.[1] Stress due to exposure to chronic noise may adversely affect the cardiovascular system,[2,3] including by increasing blood pressure (BP) and the risk of hypertension.[4,5] Hypertension is a major public health problem in developed countries, with a prevalence estimated at 30-40% in the adult population.[6,7] Associations with hypertension have consistently been documented for residential exposure to road traffic noise[8,9,10,11] and for aircraft noise.[2,12,13] The association between aircraft noise and hypertension was found to be stronger than that with road traffic noise.[2,11] However, few studies have investigated relationships between railway noise[14,15] or exposure to multiple sources of transportation noise and hypertension.[16] Individual/neighborhood socioeconomic factors were also shown to be associated with higher BP and hypertension,[17,18] but few studies have taken into account these confounding factors in the relationship between environmental noise and hypertension.[16,19]
In the present study, we examined the associations between outdoor road, rail, air, or total road, rail, and air (RRA) traffic noise and BP as well as hypertension in the Île-de-France region. We adjusted for individual and neighborhood confounders, including socioeconomic status, road traffic air pollution, and perceived occupational noise exposure. We also controlled for behavioral risk factors of hypertension that could mediate the noise-BP association of interest. We eliminated these indirect biasing pathways to ensure that the estimated associations only reflect the direct effect of noise on BP.[20] In the final step, we adjusted for road-traffic annoyance that was conceptualized as a potential mediator of the noise-BP association of interest. We compared associations with transportation noise estimated at the exact place of residence, at the exact workplace, and within the corresponding neighborhoods.
Methods
Population
The present cross-sectional analysis was based on data from the first wave of the RECORD Study. This first wave recruited 7,290 residents of the Île-de-France region between March 2007 and February 2008. The study benefited from free medical checkups, offered every 5 years by the French National Health Insurance System for Salaried Workers to all working and retired employees and their families. The participants were recruited without a priori sampling during 2-h medical checkups conducted in four of the health centers of the IPC Medical Center, located in the Paris metropolitan area. The eligibility criteria included participants who were 30-79 years old, able to complete study questionnaires, and residing in one of 10 administrative divisions of Paris or in one of 111 other municipalities selected in the Paris metropolitan area. These territories were selected to include suburban and urban areas from contrasted socioeconomic backgrounds. Among people presenting at the health centers and who were eligible based on age and residence, 10.9% were not selected for participation because of linguistic or cognitive difficulties in filling out the study questionnaires. Of the individuals selected for participation, 83.6% agreed to participate and completed the data collection protocol. All the 7,290 participants (100%) were geocoded based on their residential address in 2007-2008. Among the 7,290 participants, 4,331 participants (59.4%) were working the year before the recruitment and had their workplace geocoded based on their main workplace address [Appendix A (168.6KB, pdf) ]. Additional details on the RECORD Study have been reported elsewhere.[17,21] The study protocol was approved by the French Data Protection Authority.
WORKING PARTICIPANTS WITH AVAILABLE INFORMATION ON THEIR WORKPLACE
BP and hypertension
During the medical checkup conducted at the health center, supine brachial BP was measured by trained nurses for each participant three times in the right arm after a 10-min rest period, using a manual mercury sphygmomanometer. A standard cuff size was used, but a large cuff was employed if necessary. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were defined as the first and fifth Korotkoff phases, respectively, using the mean of the last two BP measurements.[22] The time of BP measurement was divided into four classes: 8 AM to ≤10 AM, 10 AM to ≤noon, noon to ≤2 PM, and <2 PM to ≤4 PM. An antihypertensive medication-use variable based on administrative health-care data linked to the RECORD Study indicated whether participants had been reimbursed for any antihypertensive medication over the previous year. Participants were defined as hypertensive (binary variable) if their measured SBP was ≥140 mm of mercury (mmHg) or if their DBP was ≥90 mmHg, or if they had used antihypertensive medications over the past year.[23]
Individual and neighborhood variables
Gender was coded as a binary variable and age as a continuous variable. Education was divided into four classes: No education (low), primary and low secondary education (mid-low), high secondary and low tertiary education (middle-high), and upper tertiary education (high). Employment status was categorized as follows: Employed, unemployed, retired, and other. Self-reported financial strain was assessed as a binary variable based on the following questionnaire item: “Do you have real financial problems to address your needs during some periods of the month (food, rent, bills)?” Nonownership of dwelling was coded with a binary variable. The 2004 Human Development Index of the country (HDI) was attributed to each individual's self-reported country of birth. A binary variable was defined to distinguish participants born in low-development countries from others. “Perceived occupational noise exposure” was assessed as a binary variable with the following questionnaire item: “In your work, are you or have you been exposed to noise nuisances?”
Neighborhood socioeconomic status was defined as the education of the residents in buffers of 500 m of radius centered on the residence of the participants. These buffers (defined with ArcInfo 10.0, ESRI, Redlands, California, USA and street network data from the French National Geographic Institute) took into account the street network around the residence. The educational level of neighborhood residents was defined as the proportion of residents aged >25 years with an upper tertiary education (2006 Census). A binary variable distinguished the upper quartile from the three other quartiles. Road traffic air pollution was defined within these buffers as the average annual concentrations of particulate matter with an aerodynamic diameter ≤10 μm (PM10) and of nitrogen dioxide (NO2) [Appendix B (260.6KB, pdf) ].
DEFINITION OF VARIABLES
Finally, we used a typology of neighborhoods elaborated for the RECORD Study in the Île-de-France region.[18] This typology, established with a two-step procedure (factor analysis and cluster analysis), provides a grouping of neighborhoods with comparable characteristics but which are not necessarily geographically adjacent. Different neighborhood types were identified from the combination of 13 neighborhood variables (among the numerous variables initially considered), including: Four indicators of the built environment (proportion of the neighborhood area covered with buildings, density of intersections, average street block length, and deterioration of the physical environment in the neighborhood); two indicators of air pollution (measured concentrations of PM10 and NO2 in the neighborhood); four indicators of the service environment (total number of destinations, number of supermarkets, number of grocery stores, and incoming and outgoing traffic by public transportation); and three indicators of neighborhood social interactions (neighborhood stressful social interactions, neighborhood mistrust and hostility, and stigmatized neighborhood identity). The detailed methodology to derive this neighborhood typology has been reported elsewhere.[18] Six neighborhood types were identified: Two urban central neighborhoods, two urban neighborhoods, and two suburban neighborhoods, with more or less advantaged social interactions in each urbanization stratum.
Personal risk factors of high BP
Family history of hypertension was self-reported. Alcohol consumption was coded in four categories: Never drinkers, former drinkers (who declared not drinking alcohol anymore), light drinkers (between one and ≤two glasses per day for women and between one and ≤three glasses per day for men), and drinkers (>two glasses per day for women and >three glasses per day for men). Regarding smoking, we used pack/year information to distinguish nonsmokers, light former smokers, heavy former smokers, light current smokers, and heavy current smokers [Appendix B (260.6KB, pdf) ]. Regarding physical activity, we considered an overall sport practice variable (not regularly; one or two times per week; ≥three times per week). Height (using a wall-mounted stadiometer) and weight (using calibrated scales) were recorded by a nurse.[24] Body mass index (BMI) (weight/height2 in kg/m2) was categorized as follows: Normal (<25 kg/m2), overweight (25 to <30 kg/m2), and obese (≥30 kg/m2).[25]
In a study of the concept of noise annoyance conducted by a panel of experts of different countries,[26] noise annoyance was closely associated with the notions of “nuisance” and “disturbance.” Annoyance was also linked to the concepts of negative feelings and evaluations.[26] Annoyance related to road traffic was based on the following item: “Do you find that in your neighborhood there is too much road traffic?” This item placed the emphasis on a negative aspect (“too much”) and therefore referred to “road traffic nuisance” or in other terms relating to annoyance due to road traffic (thus, a broader concept than “road traffic noise annoyance” itself, as the survey question was related to all aspects of road traffic nuisance indistinctively: Noise, air pollution, safety, etc.). The degree of annoyance was rated on the following scale: “yes, definitively,” “yes, probably,” “probably not,” and “definitely not.” A binary variable of annoyance was defined with a value of 1 for the “yes, definitely,” and 0 otherwise.
Transportation noise
The (road, rail, air) transportation noise data were provided by Bruitparif. This non-Governmental Organization is in charge of gathering published layers of noise modelled by each municipality or Government services in the Île-de-France region from 2007 onward. Noise in this database is measured in decibel with an A-weighted filter [dB(A)] and is expressed with the standard European Lden and Ln indicators. With the dB(A) unit of measurement, the filter A scale corresponds to the natural hearing sensitivity recognition of humans at different sound frequencies. Following previous work,[27] we chose to use the Lden indicator, defined as the A-weighted-equivalent continuous noise level (LAeq) over a 24-h period, but in which levels during the evening (LAeq, 6 PM-10 PM) and night (LAeq, 10 PM-6 AM) are increased by 5 dB(A) and 10 dB(A), respectively. According to the Environmental Noise Directive,[28] the municipalities had to elaborate complete maps of road, rail, and air traffic noise. Noise maps were determined using annual average daily traffic data collected during 1 year. The layers provided by the municipalities in the Île-de-France region were vector or raster files of noise points or noise lines, modelled every 2 m at 4 m from the ground and at 2 m from the buildings’ frontage, and taking into account the distribution of buildings.
An overall noise map was built by Bruitparif to comply with the Environmental Noise Directive Recommendations. When municipalities did not generate or release a noise database for their territory, Bruitparif completed the missing information with a noise database elaborated by Government services. The latter institution had to elaborate maps of road, rail, and air traffic noise that were less precise than those produced by the municipalities. Only roads with more than six million vehicles per year, railways with more than 60,000 trains per year, and airports with more than 50,000 movements per year were taken into account in this governmental modelling of noise. Bruitparif processed all these layers in order to create a noise database at the scale of the Île-de-France region. According to the Environmental Noise Directive,[28] from the vector layers of noise points or noise lines or the raster layers provided by municipalities and government services with noise levels ranging 30-80 dB(A), Bruitparif generated layers of polygons of noise levels with a subdivision in five to five dB(A) classes with noise ranging 55-80 dB(A). The raw data of the final Bruitparif map were collected between 2007 and 2011 [Figure 1: The Bruitparif layer D].
Figure 1.
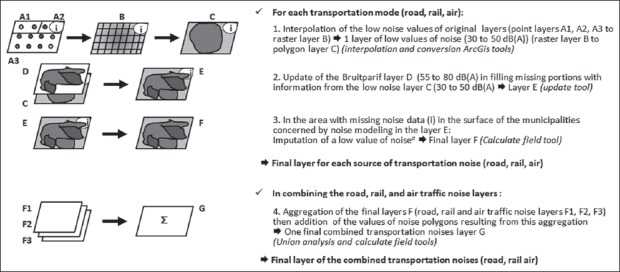
Main steps involved in the constitution of transportation noise layers (a) Low values of noise of 40 dB(A) for road traffic and of 30 dB(A) for rail and air traffic were assigned to locations that had missing data because they were too far from noise emission sources
The geographical processing of the noise database was performed with ArcInfo 10.0 Geographic Information System. The Environmental Noise Directive established that noise levels equal to or above 55 dB(A) could have an impact on human health. However, in order to take into account the heterogeneous environments in the Île-de-France region from quiet rural areas to busy urban areas, we also integrated levels of noise from the minimum level of 30 dB(A) corresponding to the rural environment at night to the established European level of 55 dB(A). To integrate all noise classes in the range 30-80 dB(A), we processed and homogenized the original layers of noise points elaborated by municipalities and Government services [that include noise classes ranging 30-50 dB(A)] [Figure 1: Point layers A1, A2, and A3 to raster layer B to polygon layer C] following the general process used by Bruitparif, to elaborate layers of noise polygons. The final layer of noise polygons for each transportation mode (road, rail, and air) [Figure 1: Layer E] at the scale of the Île-de-France region was generated by filling missing portions of the Bruitparif layer [Figure 1: Bruitparif layer D] [55-80 dB(A)] with information from the layers of polygons from the Government services/municipalities [Figure 1: Polygon layer C] [30-50 dB(A)]. The available noise data did not cover the entire study territory and differed in their coverage according to the source of transportation noise. As explained in the supplemental material [Appendix C (168KB, pdf) ], noise values were imputed in layer E [Figure 1] for areas excluded from the modelling because they were far from noise sources, but not for other areas excluded for administrative reasons [Figure 1: Layer E to Layer F]. Finally, with the updated final layer for each source of transportation [Figure 1: Final layer F (F1, F2, and F3)], an integrative noise layer, combining the final layers of road, rail, and air traffic noise, was elaborated [Figure 1: Layers F1, F2, F3 to Layer G].
MANAGEMENT OF MISSING DATA FOR TRANSPORTATION NOISE
In order to estimate noise exposure at the place of residence and workplace of the participants, outdoor road, rail, and air traffic noise and RRA traffic noise levels were extracted at each geocoded place of residence and workplace. We also extracted noise information for 500 m-radius buffer zones that take into account the street network centered on each geocoded place of residence and workplace. This buffer size was selected to take into consideration the outdoor transportation noise exposure of participants moving around their residence or workplace during the day. The portions of the different polygons of noise that fell into the buffer of each participant were identified (ArcGIS intersect analysis). Then, according to the proportion of the surface of each class of noise that fell into these buffers, the following noise variables were defined using SAS version 9.3 (SAS, Cary, NC, USA): Median noise value, and 25th and 75th percentiles of the noise value in the residential and workplace buffers of each participant. For each source of transportation noise and for the total transportation noise, the eight continuous noise variables (two for the exact residence and workplace, three for the residential buffer, and three for the workplace buffer) expressed on a 5-dB(A) unit scale, were then 1) standardized; or 2) categorized into three classes: A “low noise level” [30-<45 dB(A)] corresponding to the rural quiet areas, an “intermediate noise level” [45-<65 dB(A)], and “noise levels exceeding the European Union guidelines for road traffic” [65-<80 dB(A)].[28] In our sample, the number of participants who were exposed to aircraft noise was too low to investigate associations between aircraft noise and BP [Supplemental material, Table A (186.7KB, pdf) ]. However, aircraft noise was investigated as a component of the RRA traffic noise variable. Excluding the residual missing values for each noise variable resulted in different samples for each exposure variable [Supplemental material, Table A (186.7KB, pdf) ].
Distribution of the RECORD participants’ places of residence, workplaces, and corresponding neighborhoods across categories of noise
Statistical analysis
Multilevel linear and logistic regression models were estimated to examine associations for RRA, road, and rail traffic noise estimated at the place of residence, the workplace, and in the residential and workplace neighborhoods with BP and hypertension. As controlling for antihypertensive medication use in this analysis could have introduced bias (as the treatment is itself a consequence of a high underlying BP level),[29] we chose to add a constant to the observed BP (10 mmHg for SBP and 3.71 mmHg for DBP) in treated subjects to account for the treatment effect on BP, instead of adjusting [Appendix B (260.6KB, pdf) ].[29,30]
We ran sensitivity analyses to estimate the potential bias introduced by missing noise estimates for the participants living or working too far from noise sources [Supplemental material, Table B (256.3KB, pdf) ]. The main article reports analyses in samples where such missing noise values were set to 40 dB(A) for road traffic and to 30 dB(A) for rail and air traffic noise.
Adjusted associations estimated between road traffic noise at the workplace and BP, in the samples with complete data and with imputed noise values for unexposed places (RECORD Studya)
The multilevel models were estimated with participants nested within 1,602 census block group neighborhoods. These units, defined for the Population Census, were relatively homogeneous in terms of sociodemographic and housing characteristics. For each sample, a null model was estimated. Then, models for the associations with noise were adjusted for individual socioeconomic variables, time of BP measurement, neighborhood social factors, road traffic air pollution, and perceived occupational noise exposure. Models were then also adjusted for risk factors of hypertension, and finally for road traffic-related annoyance. At each step, only the variables that were associated with the outcomes in at least some of the models were retained. We report beta coefficients expressing increases/decreases in mmHg of BP for the linear models. For the logistic models, we report odds ratios for being hypertensive associated:
With an increase of one standard deviation in the continuous standardized variables of noise; and
With an intermediate noise level or a noise level exceeding European Union guidelines in comparison with a low noise level (categorical variable).
All analyses were conducted with SAS version 9.3.
Results
Participants had a higher outdoor noise exposure at their workplace than at their residence. Most study locations had the lowest possible level of rail and air traffic noise [Supplemental material, Table A (186.7KB, pdf) ].
BP tended to be higher among males, older participants, and among those retired, born in a low-HDI country, with a low education, and with a family history of hypertension [Table 1]. BP tended to be higher in the medium and high classes of RRA traffic noise, either at the place of residence, at the workplace, or in their neighborhoods. Unexpectedly, when considering the 75th percentile of noise values in the neighborhood buffer (that captured the highest levels of noise in each buffer), BP was sometimes higher in the low and medium classes [Table 2].
Table 1.
Descriptive statistics on the study population (RECORD Studya)
| Variables | Residence | Work | ||
|---|---|---|---|---|
| SBPb (N = 7068)c | DBPb (N = 7068)c | SBPb (N = 4199)c | DBPb (N = 4198)c | |
| Mean ± SD P for trend* | Mean ± SD P for trend* | Mean ± SD P for trend* | Mean ± SD P for trend* | |
| Gender | ||||
| Male | 130.4±17.3 | 78.5±10.8 | 128.0±16.0 | 77.5±10.5 |
| Female | 127.2±20.9 | 75.0±11.0 | 123.2±19.3 | 74.3±11.1 |
| <.0001* | <.0001* | <.0001* | <.0001* | |
| Age (years) | ||||
| 30-44 | 121.8±14.2 | 73.6±9.9 | 121.6±14.2 | 73.4±9.9 |
| 45-59 | 130.0±18.2 | 79.0±11.0 | 129.7±17.7 | 79.0±10.7 |
| 60-79 | 139.6±20.3 | 79.9±10.9 | 136.0±20.3 | 80.1±11.0 |
| <.0001* | <.0001* | <.0001* | <.0001* | |
| HDI of country of birth | ||||
| Low | 133.0±20.1 | 80.8±12.1 | 128.0±16.0 | 79.9±11.5 |
| High | 129.1±18.6 | 77.1±10.9 | 123.2±19.3 | 76.3±10.7 |
| 0.001* | <.0001* | <.0001* | <.0001* | |
| Employment statusd | ||||
| Employedd | 126.9±16.9 | 76.8±10.7 | 126.9±16.9 | 76.7±10.6 |
| Unemployedd | 125.6±17.6 | 76.4±11.0 | 125.6±17.6 | 75.2±11.0 |
| Retiredd | 140.9±20.1 | 80.1±10.9 | 140.9±20.1 | 80.3±10.7 |
| <.0001* | <.0001* | <.0001* | 0.2* | |
| Financial strain | ||||
| Yes | 129.3±18.4 | 77.9±11.8 | 127.1±18.5 | 76.7±11.2 |
| No | 129.2±19.9 | 77.2±10.8 | 126.5±16.8 | 76.5±10.7 |
| 0.08* | 0.13* | 0.4* | 0.47* | |
| Ownership of dwelling | ||||
| Owner | 129.7±18.3 | 77.3±10.8 | 126.8±16.7 | 76.9±10.7 |
| Nonowner | 128.8±19.1 | 77.2±11.2 | 126.4±17.6 | 76.2±10.8 |
| 0.001* | 0.12* | 0.07* | 0.01* | |
| Family history of hypertension | ||||
| Yes | 132.7±20.0 | 78.9±11.4 | 129.5±18.2 | 78.1±12.0 |
| No | 127.5±17.7 | 76.5±10.6 | 125.1±16.3 | 75.8±10.4 |
| <.0001* | <.0001* | <.0001* | <.0001* | |
| Individual education | ||||
| High | 126.8±17.4 | 76.2±10.6 | 124.6±15.6 | 75.6±10.3 |
| Middle-High | 128.5±18.6 | 76.9±11.0 | 126.1±17.0 | 76.3±11.02 |
| Mid-low | 133.0±19.3 | 78.9±11.0 | 130.1±18.5 | 78.2±10.9 |
| Low | 133.9±20.6 | 79.1±11.2 | 129.6±19.1 | 78.1±10.8 |
| <.0001* | <.0001* | <.0001* | <.0001* | |
BP = Blood pressure; SBP = Systolic blood pressure, DBP = Diastolic blood pressure; HDI = Human development index, *P values for trends were estimated from the Jonckheere-Terpstra test, aCross-sectional study based on data from the first wave of the RECORD Study. bSBP and DBP (in mmHg) were expressed as continuous variables with 10 mmHg added to the observed SBP values and with 3.71 mmHg added to the observed DBP values for the participants on antihypertensive treatment. cMeans and standard deviations of SBP and DBP were calculated after excluding individuals with missing values for total RRA traffic noise variables at the exact place of residence or at the exact workplace and for SBP or DBP. dDuring the geocoding of the workplace of the participants (N = 4331) [Appendix A (168.6KB, pdf) ], we assigned to each individual the main work establishment of the year preceding his/her inclusion in the study; it explains why certain participants were classified as retired or unemployed according to the employment status variable
Table 2.
Mean differences in BP associated with categories of noise exposure (RECORD Studya)
| RRA traffic noiseb | Residenceb | Workb | ||
|---|---|---|---|---|
| SBPc | DBPc | SBPc | DBPc | |
| Mean ± SD (P25, P75)d | Mean ± SD (P25, P75)d | Mean ± SD (P25, P75)d | Mean ± SD (P25, P75)d | |
| Exact placeb | ||||
| Classes of noise | N=7068 | N=7068 | N=4199 | N=4198 |
| [30-45 dB(A)] | 128.6±18.3 (116.0, 138.0) | 76.7±10.8 (69.0, 83.0) | 125.5±16.6 (114.0, 134.0) | 75.7±10.6 (68.0, 82.0) |
| [45-65 dB(A)] | 129.6±18.8 (117.0, 140.0) | 77.7±11.1 (70.0, 84.0) | 127.1±17.5 (115.0, 136.0) | 76.7±10.8 (69.0, 83.0) |
| [65-80 dB(A)] | 129.4±18.9 (116.0, 139.0) | 77.3±10.9 (69.0, 84.0) | 126.8±17.1 (115.0, 135.0) | 76.9±10.8 (69.0, 83.0) |
| P for trend* | 0.15* | 0.11* | 0.08* | 0.007* |
| P25b | ||||
| Classes of noise | N=7068 | N=7068 | N=4199 | N=4198 |
| [30-45 dB(A)] | 128.9±18.3 (116.0, 139.0) | 76.9±10.7 (69.0, 83.0) | 125.9±16.8 (114.0, 135.0) | 76.2±10.6 (69.0, 82.7) |
| [45-65 dB(A)] | 130.0±19.2 (116.0, 140.0) | 77.8±11.3 (70.0, 85.0) | 127.5±17.5 (115.0, 136.0) | 77.0±10.9 (70.0, 83.7) |
| [65-80 dB(A)] | 127.9±18.5 (115.0, 134.5) | 77.5±10.6 (69.0, 82.0) | 130.0±17.4 (119.0, 139.0) | 77.6±11.9 (69.0, 85.0) |
| P for trend* | 0.03* | 0.0009* | 0.0005* | 0.002* |
| P50b | ||||
| Classes of noise | N=7068 | N=7068 | N=4199 | N=4198 |
| [30-45dB(A)] | 128.4±18.3 (116.0, 138.0) | 76.5±10.6 (69.0, 83.0) | 125.9±17.0 (114.0, 135.0) | 76.2±10.7 (69.0, 82.7) |
| [45-65 dB(A)] | 129.8±18.7 (117.0, 140.0) | 77.8±11.1 (70.0, 84.0) | 126.9±17.5 (115.0, 135.0) | 76.8±10.8 (69.0, 83.0) |
| [65-80 dB(A)] | 130.3±20.8 (116.0, 140.0) | 77.7±11.5 (70.0, 84.0) | 127.3±16.3 (116.0, 137.0) | 76.9±10.9 (69.0, 83.7) |
| P for trend* | 0.002* | 0.0001* | 0.02* | 0.03* |
| P75b | ||||
| Classes of noise | N=7068 | N=7068 | N=4199 | N=4198 |
| [30-45 dB(A)] | 130.8±18.3 (118.0, 142.0) | 77.9±10.3 (71.0, 84.0) | 126.6±16.5 (116.0, 135.0) | 76.3±11.3 (69.0, 82.7) |
| [45-65 dB(A)] | 129.3±18.6 (117.0, 139.0) | 77.4±11.1 (70.0, 84.0) | 127.1±17.7 (115.0, 137.0) | 76.9±10.8 (70.0, 83.0) |
| [65-80 dB(A)] | 129.0±18.9 (116.0, 139.0) | 77.1±10.9 (69.0, 83.7) | 126.4±16.9 (115.0, 135.0) | 76.5±10.7 (69.0, 83.0) |
| P for trend* | 0.05* | 0.03* | 0.13* | 0.21* |
BP = Blood pressure; SBP = Systolic blood pressure, DBP = Diastolic blood pressure, RRA = Road, rail, and air, P25 = 25th percentile, P50 = Median, P75 = 75th percentile, *P values for trends were estimated from the Jonckheere-Terpstra test, aCross-sectional study based on data from the first wave of the RECORD Study. bRRA traffic noise variables [expressed in dB(A) and with the Lden indicator] were estimated at the exact place of residence and workplace, and in the residential and workplace neighborhoods (25th, 50th, and 75th percentiles of noise values in 500 m radius street network buffers around the place of residence and the workplace). cSBP and DBP (in mmHg) were expressed as continuous variables with 10 mmHg added to the observed SBP values and with 3.71 mmHg added to the observed DBP values for the participants on antihypertensive treatment. dMeans, standard deviations, and the 25th and 75th percentiles of SBP and DBP were calculated
After the successive adjustment for individual and neighborhood variables (social variables, air pollution, perceived occupational noise exposure) and risk factors of hypertension, the standardized RRA and road traffic noise variables assessed in the workplace neighborhood (25th percentile or median of noise values in the buffers) remained associated with SBP. These noise variables assessed at the workplace location also remained associated with DBP. Even though the 95% confidence interval (CI) included the null, a similar pattern for association between noise exposure at the exact workplace location and SBP was found [Table 3 and Supplemental material, Table C (259.4KB, pdf) ]. These associations were of comparable magnitude for RRA and road traffic noise. These noise variables remained associated even when excluding the participants with an imprecisely geocoded workplace. Specifically, RRA traffic noise at the workplace remained associated with SBP after such restriction of the sample size [Supplemental material, Table D (266KB, pdf) ].
Table 3.
Adjusted associations estimated between RRA traffic noise at the place of residence, the workplace, and in the corresponding neighborhoods and BP (RECORD Studya)
| RRA traffic noisec | Residencec | Workc | ||
|---|---|---|---|---|
| SBPb | DBPb | SBPb | DBPb | |
| β (95% CI) ICC Null./ICC Adj. | β (95% CI) ICC Null./ICC Adj. | β (95% CI) ICC Null./ICC Adj. | β (95% CI) ICC Null./ICC Adj. | |
| Exact placec | Model: (N=7068)d +0.13-0.24 to +0.51 0.035/0.013 |
Model: (N=7068)d,e +0.13-0.10 to +0.36 0.020/- |
Model: (N=4199)d +0.36-0.10 to +0.82 0.036/0.020 |
Model: (N=4198)d +0.40+0.11 to +0.69 0.013/0.003 |
| P25c | Model: (N=7068)d −0.02-0.44 to +0.40 0.035/0.013 |
Model: (N=7068)d −0.07-0.32 to +0.19 0.020/- |
Model: (N=4199)d +0.55+0.08 to +1.01 0.036/0.021 |
Model: (N=4198)d +0.22-0.08 to +0.51 0.013/0.003 |
| P50c | Model: (N=7068)d +0.07-0.38 to +0.51 0.035/0.013 |
Model: (N=7068)d,e −0.02-0.29 to +0.25 0.020/- |
Model: (N=4199)d +0.42-0.05 to +0.88 0.036/0.019 |
Model: (N=4198)d +0.19-0.10 to +0.49 0.013/0.002 |
| P75c | Model: (N=7068)d −0.10-0.49 to +0.29 0.035/0.013 |
Model: (N=7068)d,e −0.07-0.30 to +0.16 0.020/- |
Model: (N=4199)d −0.11-0.56 to +0.35 0.036/0.020 |
Model: (N=4198)d +0.01-0.29 to +0.30 0.013/0.003 |
BP = Blood pressure; RRA = Road, rail, and air, SBP = Systolic blood pressure, DBP = Diastolic blood pressure, ICC Null. = Intra-class correlation coefficient for the null model, ICC Adj. = Intra-class correlation coefficient, after adjustment for individual/neighborhood factors, and risk factors of hypertension, P25 = 25th percentile, P50 = Median, P75 = 75th percentile, aCross-sectional study based on data from the first wave of the RECORD Study. bSBP and DBP (in mmHg) were expressed as continuous variables with 10 mmHg added to the observed SBP values and with 3.71 mmHg added to the observed DBP values for the participants on antihypertensive treatment. cRRA traffic noise variables [expressed in dB(A) and with the Lden indicator] were estimated at the exact place of residence and workplace, and in the residential and workplace neighborhoods (25th, 50th, and 75th percentiles of noise values in 500 m radius street network buffers around the place of residence and the workplace). These continuous noise variables were standardized by subtracting the average and then dividing by the standard deviation of the variable [(noise variable-μ)/σ]. dMultilevel linear regression models were estimated after excluding individuals with missing values for RRA traffic noise and for SBP or DBP. These models estimated associations between RRA traffic noise variables and SBP and DBP, adjusted for individual/neighborhood factors and risk factors of hypertension. eIn certain models, the between-neighborhood variance could not be estimated after adjustment, probably due to the very low level of clustering
Adjusted associations estimated between road traffic noise at the place of residence, the workplace, or in the corresponding neighborhoods and BP (RECORD Studya)
Adjusted associations estimated between RRA or road traffic noise at the workplace or at the accurately geocoded workplace and BP (RECORD Studya)
Overall, no associations were documented between noise exposure at the exact place of residence or in the residential neighborhood and BP, even after excluding participants without a geocoded workplace [Table 3 and Supplemental material, Tables C (259.4KB, pdf) and E (256.2KB, pdf) ].
Adjusted associations estimated between RRA traffic noise at the residence and BP with 1) all the participants and 2) only among the workers (RECORD Studya)
After adjustment for individual variables [Tables 4 and 5], SBP and DBP were respectively 1.76 mmHg and 1.02 mmHg higher in the intermediate class of RRA traffic noise and 1.51 mmHg and 1.23 mmHg higher in the highest exposure category, as compared to the reference low-noise category (with the exposure assessed at the exact workplace). After additional adjustment for neighborhood variables (air pollution and perceived occupational noise exposure were not retained as not associated in the expected direction), RRA traffic noise at the workplace remained associated with BP, even if the relationships were reduced in magnitude. The associations between workplace RRA traffic noise and BP were reduced in magnitude but also tended to persist after adjustment for risk factors (the 95% CIs included the null value for SBP but not for DBP). Road traffic-related annoyance was not associated with BP. No associations were documented with hypertension [Supplemental material, Table F (187.2KB, pdf) ], or with rail traffic noise [Supplemental material, Table G (255.1KB, pdf) ].
Table 4.
Associations estimated between RRA traffic noise at the workplace and SBP, adjusted for individual/neighborhood factors and risk factors of hypertension (RECORDa; N = 4199)
| Variables | Model: SBPb,c | Model: SBPb,c | Model: SBPb,c | |||
|---|---|---|---|---|---|---|
| β (95% CI) | β (95% CI) | β (95% CI) | ||||
| Transportation noise | ||||||
| RRA traffic noise at the workplace (Lden indicator) (vs [30-45 dB(A)]) | ||||||
| [45-65 dB(A)] | +1.76 | +0.38 to +3.15 | +1.47 | +0.07 to +2.86 | +1.23 | −0.11 to +2.57 |
| [65-80 dB(A)] | +1.51 | +0.28 to +2.75 | +1.36 | +0.12 to +2.60 | +1.06 | −0.13 to +2.25 |
| Individual factors | ||||||
| Male (vs female) | +0.55 | +0.49 to +0.61 | +0.55 | +0.50 to +0.61 | +0.47 | +0.41 to +0.53 |
| Age (1-year increase) | +5.78 | +4.70 to +6.86 | +5.74 | +4.66 to +6.82 | +4.71 | +3.64 to +5.78 |
| Hour of BP measurement (vs 8-10 AM) | ||||||
| 10 AM-noon | +0.43 | −0.90 to +1.77 | +0.33 | −1.01 to +1.67 | +0.21 | −1.08 to +1.49 |
| Noon-2 PM | +0.97 | −0.30 to +2.24 | +0.86 | −0.41 to +2.13 | +0.41 | −0.81 to +1.63 |
| 2-4 PM | +1.26 | −0.22 to +2.75 | +1.22 | −0.27 to +2.70 | +0.85 | −0.57 to +2.27 |
| Low human development of country of birth (vs medium or high) | +5.97 | +3.89 to +8.06 | +5.66 | +3.56 to +7.75 | +4.59 | +2.56 to +6.63 |
| Employment status (vs employed)e | ||||||
| Unemployede | −2.44 | −3.82 to −1.05 | −2.35 | −3.75 to −0.96 | −2.02 | −3.36 to −0.68 |
| Retirede | +3.74 | +1.16 to +6.32 | +3.67 | +1.10 to +6.25 | +2.88 | +0.40 to +5.35 |
| Nonownership of dwelling (vs owner) | +1.35 | +0.28 to +2.43 | +1.55 | +0.46 to +2.64 | +1.24 | +0.19 to +2.29 |
| Family history of hypertension | +4.79 | +3.77 to +5.81 | +4.72 | +3.71 to +5.74 | +4.24 | +3.26 to +5.22 |
| Financial straind | +0.60 | −0.78 to +1.97 | +0.48 | −0.90 to +1.86 | −0.35 | −1.68 to +0.98 |
| Individual education (vs high) | ||||||
| Middle-high | +1.53 | +0.35 to +2.71 | +1.13 | −0.07 to +2.33 | +0.71 | −0.45 to +1.87 |
| Mid-low | +3.80 | +2.45 to +5.15 | +3.24 | +1.84 to +4.63 | +2.36 | +1.02 to +3.71 |
| Low | +4.74 | +2.75 to +6.73 | +4.20 | +2.17 to +6.22 | +2.91 | +0.94 to +4.89 |
| Neighborhood factors | ||||||
| Neighborhood type (vs type 6: central urban, intermediate social standing) | ||||||
| Type 1: Suburban, low social standing | +1.94 | -0.35 to +4.24 | +0.74 | −1.47 to +2.96 | ||
| Type 2: Suburban, high social standing | +2.53 | +0.88 to +4.17 | +1.86 | +0.27 to +3.45 | ||
| Type 3: Urban, low social standing | +2.54 | +0.76 to +4.32 | +2.02 | +0.31 to +3.73 | ||
| Type 4: Urban, high social standing | +1.29 | −0.25 to +2.84 | +0.98 | −0.51 to +2.47 | ||
| Type 5: Central urban, high social standing | +1.54 | −0.38 to +3.46 | +1.28 | −0.56 to +3.13 | ||
| Percentage of residents with university education (upper quartile vs the 3 other quartiles)d | −1.13 | −2.37 to +0.11 | −0.70 | −1.89 to +0.49 | ||
| Risk factors of hypertension Smoking (vs nonsmoker) | ||||||
| Light former smoker | −1.00 | −2.27 to +0.28 | ||||
| Heavy former smoker | −2.02 | −4.00 to −0.04 | ||||
| Light current smoker | −2.46 | −3.78 to −1.13 | ||||
| Heavy current smoker | +0.12 | −1.83 to +2.07 | ||||
| Alcohol consumption (vs never drinker) | ||||||
| Former drinker | +1.61 | −0.86 to +4.08 | ||||
| Light drinker | +1.97 | +0.49 to +3.45 | ||||
| Drinker | +7.04 | +4.80 to +9.28 | ||||
| BMI (vs normal) | ||||||
| Overweight | +5.22 | +4.21 to +6.24 | ||||
| Obese | +13.58 | +12.02 to +15.14 | ||||
| Sport practice (vs not regularly) | ||||||
| 1 or 2 times per week | −1.51 | −2.51 to −0.50 | ||||
| >3 times per week | −0.75 | −2.65 to +1.14 | ||||
| ICC Null. | 0.036 | 0.036 | 0.036 | |||
| ICC Adj. | 0.026 | 0.021 | 0.021 | |||
RRA = Road, rail, and air, SBP = Systolic blood pressure, ICC Null. = Intra-class correlation coefficient for the null model, ICC Adj. = Intra-class correlation coefficient, after adjustment for 1) invidual sociodemographic factors; 2) neighborhood factors; and 3) risk factors of hypertension; BMI = Body mass index, aCross-sectional study based on data from the first wave of the RECORD Study. bSBP (in mmHg) was expressed as a continuous variable with 10 mmHg added to the observed SBP values for the participants on antihypertensive treatment. cMultilevel linear regression models were estimated after excluding individuals with missing values for RRA traffic noise and for SBP. These models estimated associations between a categorical RRA traffic noise variable estimated at the workplace and SBP, adjusted for individual factors, neighborhood conditions, and risk factors of hypertension. dFinancial strain and the percentage of residents with university education were not associated with SBP, after excluding missing values for RRA traffic noise assessed at the workplace and for SBP (N = 4199); but these variables were associated with SBP after excluding missing values only for RRA traffic noise at the place of residence and for SBP (N = 7068). We therefore decided to keep these variables in the models. eDuring the geocoding of the workplace of the participants (N = 4331) [Appendix A (168.6KB, pdf) ], we assigned to each individual the main work establishment of the year preceding his/her inclusion in the study; this explains why certain participants were classified as retired or unemployed according to the employment status variable
Table 5.
Associations estimated between RRA traffic noise at the workplace and DBP, adjusted for individual/neighborhood factors and risk factors of hypertension (RECORDa; N = 4198)
| Variables | Model 1B: DBPb,c | Model 2B: DBPb,c | Model 3B: DBPb,c | |||
|---|---|---|---|---|---|---|
| β (95% CI) | β (95% CI) | β (95% CI) | ||||
| Transportation noise | ||||||
| RRA traffic noise at the workplace (Lden indicator) (vs [30-45 dB(A)]) | ||||||
| [45-65 dB(A)] | +1.02 | +0.14 to +1.90 | +0.73 | -0.16 to +1.62 | +0.59 | -0.27 to +1.45 |
| [65-80 dB(A)] | +1.23 | +0.44 to +2.02 | +1.07 | +0.28 to +1.86 | +0.92 | +0.16 to +1.68 |
| Individual factors | ||||||
| Male (vs female) | +0.34 | +0.30 to +0.38 | +0.34 | +0.31 to +0.38 | +0.28 | +0.25 to +0.32 |
| Age (1-year increase) | +3.62 | +2.93 to +4.30 | +3.59 | +2.90 to +4.28 | +2.86 | +2.18 to +3.55 |
| Hour of BP measurement (vs 8-10 AM) | ||||||
| 10 AM-noon | −0.26 | −1.11 to +0.59 | -0.34 | −1.19 to +0.51 | −0.45 | −1.27 to +0.38 |
| Noon-2 PM | −0.79 | −1.60 to +0.02 | -0.86 | −1.67 to -0.06 | −1.16 | −1.94 to −0.38 |
| 2-4 PM | −0.85 | −1.80 to +0.09 | -0.90 | −1.84 to +0.05 | −1.15 | −2.06 to −0.24 |
| Low human development of country of birth (vs medium or high) | +4.37 | +3.04 to +5.69 | +4.06 | +2.72 to +5.39 | +3.47 | +2.17 to +4.77 |
| Employment status (vs employed)e | ||||||
| Unemployede | −1.00 | −1.88 to -0.12 | −0.98 | −1.87 to -0.10 | −0.77 | −1.63 to +0.09 |
| Retirede | −1.43 | −3.07 to +0.21 | −1.45 | −3.09 to +0.19 | −1.79 | −3.38 to −0.21 |
| Financial straind | +0.29 | −0.58 to +1.17 | +0.21 | −0.66 to +1.09 | −0.32 | −1.18 to +0.53 |
| Nonownership of dwelling (vs. owner) | +0.38 | −0.31 to +1.06 | +0.58 | −0.11 to +1.27 | +0.35 | −0.32 to +1.02 |
| Family history of hypertension | +2.67 | +2.02 to +3.32 | +2.62 | +1.97 to +3.27 | +2.34 | +1.71 to +2.97 |
| Individual education (vs high) | ||||||
| Middle-high | +0.90 | +0.15 to +1.65 | +0.64 | −0.13 to +1.40 | +0.31 | −0.43 to +1.06 |
| Mid-low | +2.00 | +1.14 to +2.86 | +1.59 | +0.71 to +2.48 | +0.97 | +0.11 to +1.84 |
| Low | +2.58 | +1.31 to +3.85 | +2.24 | +0.95 to +3.52 | +1.34 | +0.08 to +2.61 |
| Neighborhood factors | ||||||
| Neighborhood type (vs type 6: Central urban, intermediate social standing) | ||||||
| Type 1: Suburban, low social standing | +2.31 | +0.87 to +3.74 | +1.68 | +0.29 to +3.08 | ||
| Type 2: Suburban, high social standing | +2.15 | +1.12 to +3.18 | +1.84 | +0.84 to +2.84 | ||
| Type 3: Urban, low social standing | +1.61 | +0.50 to +2.73 | +1.37 | +0.29 to +2.45 | ||
| Type 4: Urban, high social standing | +1.06 | +0.09 to +2.02 | +0.96 | +0.03 to +1.90 | ||
| Type 5: Central urban, high social standing | +0.69 | -0.51 to +1.90 | +0.56 | −0.60 to +1.73 | ||
| Percentage of residents with university education (upper quartile vs the three other quartiles)d | −0.39 | −1.17 to +0.38 | −0.16 | −0.91 to +0.59 | ||
| Risk factors of hypertension | ||||||
| Smoking (vs nonsmoker) | ||||||
| Light former smoker | −0.14 | −0.95 to +0.68 | ||||
| Heavy former smoker | −0.55 | −1.82 to +0.72 | ||||
| Light current smoker | −1.51 | −2.35 to −0.66 | ||||
| Heavy current smoker | +0.66 | −0.58 to +1.91 | ||||
| Alcohol consumption (vs nondrinker) | ||||||
| Former drinker | +0.61 | −0.97 to +2.19 | ||||
| Light drinker | +1.15 | +0.20 to +2.10 | ||||
| Drinker | +4.77 | +3.34 to +6.21 | ||||
| BMI (vs normal) | ||||||
| Overweight | +3.33 | +2.68 to +3.98 | ||||
| Obese | +7.53 | +6.53 to +8.53 | ||||
| Sport practice (vs not regularly) | ||||||
| 1 or 2 times per week | −1.43 | −2.07 to −0.78 | ||||
| >3 times per week | −1.26 | −2.47 to −0.05 | ||||
| ICC Null. | 0.013 | 0.013 | 0.013 | |||
| ICC Adj. | 0.007 | 0.002 | 0.004 | |||
BP = Blood pressure; RRA = Road, rail, and air, DBP = Diastolic blood pressure, ICC Null. = Intra-class correlation coefficient for the null model, ICC Adj. = Intra-class correlation coefficient, after adjustment for 1) invidual sociodemographic factors; 2) neighborhood factors; and 3) risk factors of hypertension; BMI = Body mass index, aCross-sectional study based on data from the first wave of the RECORD Study. bDBP (in mmHg) was expressed as a continuous variable with 3.71 mmHg added to the observed DBP values for the participants on antihypertensive treatment. cMultilevel linear regression models were estimated after excluding individuals with missing values for RRA traffic noise and for DBP. These models estimated associations between a categorical RRA traffic noise variable estimated at the workplace and DBP, adjusted for individual factors, neighborhood conditions, and risk factors of hypertension. dFinancial strain and the percentage of residents with university education were not associated with DBP, after excluding missing values for RRA traffic noise assessed at the workplace and for DBP (N = 4198); but financial strain remained associated with DBP after excluding missing values only for RRA traffic noise at the place of residence and for DBP (N = 7068). Percentage of residents with university education remained associated with SBP, after excluding missing values only for RRA traffic noise at the place of residence and for SBP (N = 7068). We therefore decided to keep these variables in the models. eDuring the geocoding of the workplace of the participants (N = 4331) [Appendix A (168.6KB, pdf) ], we assigned to each individual the main work establishment of the year preceding his/her inclusion in the study; it explains why certain participants were classified as retired or unemployed according to the of employment status variable
Adjusted associations estimated between RRA traffic noise at the place of residence or the workplace and hypertension (RECORD Studya)
Adjusted associations estimated between rail traffic noise at the place of residence, the workplace, or in the corresponding neighborhoods and BP (RECORD Studya)
Discussion
After adjusting for individual/neighborhood factors and risk factors of hypertension, RRA and road traffic noise at the workplace and in the workplace neighborhood were positively associated with BP, but not with hypertension. We did not find associations with residential noise exposure or rail traffic noise.
Strengths and limitations
The strengths of this study include: The large sample of participants with information available on a large spatial scale (a portion of the Île-de-France region); the fact that noise from the main transportation modes was taken into account and combined with a Geographic Information System; the different types of measures of noise that were compared (at the place of residence and workplace and within neighborhood buffers); and the fact that the models were adjusted for multiple individual/neighborhood confounders and potential mediators, such as air pollution or risk factors of hypertension.
A limitation of this study is the absence of a priori sampling in the recruitment of the participants, which led to the selective participation of individuals with certain neighborhood profiles. These profiles were adjusted for in the present analysis;[31] however, we could not examine whether high BP also influenced participation in the study. We also had no particular hypothesis suggesting that exposure to outdoor noise, after adjustment for the density of buildings (taken into account in our typology), might be associated with participation in the study. Another important limitation is the heterogeneity of the raw transportation noise data provided by the municipalities and Government services.[32] The noise values were expressed with the Lden indicator, which is not the most relevant indicator for analyzing noise effects at the workplace, including nighttime exposure information. As another limitation, dwelling characteristics (type of dwelling, floor level, orientation of rooms) were not available in our study. A standardized variable on noise annoyance was also not available; instead, we had to consider the broader construct of annoyance related to road traffic. Finally, certain workplaces were imprecisely geolocated. However, we found that the relationship between workplace noise exposure and BP persisted when the participants with an imprecisely geocoded workplace were excluded.
Exposure to transportation noise
Participants were exposed to higher levels of RRA or road traffic noise at their workplace and in the surrounding neighborhood than at their residence or in the surrounding neighborhood, which is probably due to workplaces being typically located near main roads.[33] The low degree of exposure to rail traffic noise may be attributable to the shorter total length of the rail network compared to the road network. Calculating the total length of railways and roads from data of the Institute of Urban Planning of the Île-de-France region and of the National Geographic Institute, we found that the total length of the rail network represented only 2.1% of the total length of the railway and road networks cumulated in the Île-de-France region.
The individual/environmental correlates of BP
As previously reported,[17,18] BP increased with decreasing individual education. After adjustment for individual/neighborhood social characteristics and even risk factors of hypertension, SBP was higher in the socially deprived urban neighborhoods of the immediate suburbs of Paris with deteriorated social interactions, while DBP tended to decrease from suburban to central urban neighborhoods.[18]
Our study suggests that the exposure to outdoor RRA or road traffic noise assessed at the workplace and in the workplace neighborhood was associated with BP, after adjustment for individual/neighborhood factors, but that it was not associated with hypertension. We calculated RRA traffic noise by adding the sound pressures of road, rail, and air traffic noise. For 95% of the workplaces, road traffic noise was higher than rail and air traffic noise, which likely explains why the strength of the association with BP was of comparable magnitude for RRA and road traffic noise.
After adjustment for individual/neighborhood variables, associations between noise and BP were documented in our study when outdoor noise was assessed at the workplace, but not when it was assessed at the place of residence. In previous literature, associations between noise at the residence and BP or hypertension were documented in certain studies.[11] However, recent studies that accounted for multiple sources of traffic noise (road and rail) documented no such association.[15,16,34] The pattern of associations in our study may be partly attributable to the higher levels of outdoor noise at participants’ workplaces compared to their places of residence, which is probably due to workplaces being typically located near main roads.[33] We did not document associations between noise at the place of residence or in the residential neighborhood and BP, either in the total sample or in the sample of workers. Thus, this result suggests that the observed association between workplace environment noise exposure and BP may not be attributable to the specific sample that was used (i.e., the workers) but to the specific exposure location that was considered (i.e., the geographic environment around the workplace). Although we cannot be sure of this, there are not sufficient empirical grounds to raise the concern that the absence of association between outdoor residential noise and BP may be attributable to the fact that hypertensive participants selectively move to neighborhoods with lower noise levels. Some participants with cardiovascular risk factors may, instead, want to live closer to health services and thus move to more urban and therefore noisier areas.
An alternative explanation for the noise-BP associations documented may have been that road traffic air pollution or perceived occupational noise exposure leads to elevated BP (as found previously for associations with myocardial infarction),[35] thus confounding the relationship of interest. However, in our study, road traffic air pollution and perceived occupational noise exposure were not associated with BP in the expected direction.
Regarding risk factors of hypertension and as previously reported,[17,18,36,37,38] physical activity and smoking were inversely associated with BP; high alcohol consumption, being overweight or obese were associated with higher BP. Even if reduced in magnitude, the relationships documented between noise exposure at the workplace and BP tended to persist after adjustment for these behavioral risk factors of hypertension. Our initial hypothesis was that these behavioral mediators might be on the pathway[20] between environmental noise and BP because excessive outdoor noise may discourage physical activity and induce stress. A sedentary lifestyle independent of stress or high stress levels leading to unhealthy lifestyle behaviors may, in turn, be related to higher BP levels. It is nonetheless difficult to conclude that the noise-BP association documented is attributable to a direct pathophysiological effect of noise, independent of behavior.
The absence of a relationship between rail traffic noise and BP in our study substantiates a previous meta-analysis and studies in which no association or weak associations with hypertension were documented.[8,15,16,39] The absence of association in our study may be attributable to the low prevalence of exposure and weak exposure levels to rail traffic noise around residences and workplaces, not enabling the detection of a potential association. This may be due to the fact that compared to roads, railways are typically located at a greater distance from pedestrian paths and buildings.
Conclusion
Overall, our study suggests that exposures around the workplace may contribute to the association between outdoor transportation noise and BP. Interestingly, the associations between total RRA and road traffic noise and BP were of comparable magnitude, which is likely attributable to the predominance over the entire territory of the road traffic network in the Île-de-France region as a main source of noise compared to the rail network and airports. Urban planning should focus on reducing road traffic noise exposure within employment and services areas, while health impact assessment studies should take into account exposures at the multiple daily activity locations of populations. To better understand our findings, including why exposure in the workplace environment but not in the residential environment was associated with BP, new technologies of continuous monitoring of mobility and health were used in the RECORD Study and in the RECORD GPSBruit project and will be used in the MobiliSense project. These projects combine Global Positioning System (GPS) tracking, assessment of individual noise exposure with noise sensors, and assessment of BP through ambulatory monitoring. Such an approach will allow us to better characterize the complex interactions between the daily life environments, multiexposure to noise, and hypertension.
Financial support and sponsorship
Julie Méline was supported during the present work by the Regional Council of Île-de-France (“Health, Environment and Toxicology” Program). The RECORD Study has received support from the Institute for Public Health Research (IReSP, Institut de Recherche en Santé Publique); the National Institute for Prevention and Health Education (INPES, Institut National de Prévention et d’Education pour la Santé) (Prevention Program 2007; 2010-2011 financial support; and 2011-2013 financial support); the National Institute of Public Health Surveillance (InVS, Institut de Veille Sanitaire) (Territory and Health Program); the French Ministries of Research and Health (Epidemiologic Cohorts Grant 2008); the National Health Insurance Office for Salaried Workers (CNAM-TS, Caisse Nationale d’Assurance Maladie des Travailleurs Salariés); the Île-de-France Regional Council (Conseil Régional d’Île-de-France, DIM SEnT and CODDIM); the National Research Agency (ANR, Agence Nationale de la Recherche) (Health-Environment Program 2005); the Île-de-France Regional Health Agency (ARS, Agence Régionale de Santé) (in 2009; 2010; and 2011); the City of Paris (Ville de Paris); and the Île-de-France Youth, Sports, and Social Cohesion Regional Direction (DRJSCS, Direction Régionale de la Jeunesse, des Sports et de la Cohésion Sociale). Andraea Van Hulst received support from a CIHR/Heart and Stroke Foundation of Canada Training Grant in Population Intervention for Chronic Disease Prevention, and a doctoral scholarship from the Fonds de la recherche en santé du Québec.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We are grateful to the National Institute for Prevention and Health Education (INPES) and Pierre Arwidson for continued support since the beginning of the RECORD Study. We are also grateful to INSEE, the French National Institute of Statistics and Economic Studies, which provided support for the geocoding of the participants and allowed us access to relevant geographical data (with special thanks to Pascale Breuil). We thank Geoconcept for allowing us to access to the Universal Geocoder software. We also thank the Caisse Nationale d’Assurance Maladie des Travailleurs Salariés (France) and the Caisse Primaire d’Assurance Maladie de Paris (France) for helping make this study possible. Bruitparif is also warmly thanked for providing access to the noise data and for the invaluable assistance and advices received (Marie-Alice d’Orléans, Fanny Mietlicki).
References
- 1.Grange D, Chatignoux E, Gremy I. Ile-de-France: Observatoire Régionale de Santé d’Ile-de-France; 2009. Les perceptions du Bruit en Ile-de-France. Exploitation Régionale du Baromètre Santé-Environnement; p. 158. [Google Scholar]
- 2.Babisch W, Kamp Iv. Exposure-response relationship of the association between aircraft noise and the risk of hypertension. Noise Health. 2009;11:161–8. doi: 10.4103/1463-1741.53363. [DOI] [PubMed] [Google Scholar]
- 3.Selander J, Bluhm G, Theorell T, Pershagen G, Babisch W, Seiffert I, et al. HYENA Consortium. Saliva cortisol and exposure to aircraft noise in six European countries. Environ Health Perspect. 2009;117:1713–7. doi: 10.1289/ehp.0900933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Babisch W. Cardiovascular effects of noise. Noise Health. 2011;13:201–4. doi: 10.4103/1463-1741.80148. [DOI] [PubMed] [Google Scholar]
- 5.Babisch W. Road traffic noise and cardiovascular risk. Noise Health. 2008;10:27–33. doi: 10.4103/1463-1741.39005. [DOI] [PubMed] [Google Scholar]
- 6.Godet-Thobie H, Vernay M, Noukpoape A, Salanave B, Malon A, Castetbon K, et al. Saint-Maurice, France: Institut de Veille Sanitaire (InVS); 2008. Niveau Tensionnel Moyen et Prévalence de l’hypertension Artérielle Chez les Adultes de 18 à 74 Ans, ENNS 2006-2007; pp. 478–83. [Google Scholar]
- 7.Hajjar I, Kotchen JM, Kotchen TA. Hypertension: Trends in prevalence, incidence, and control. Annu Rev Public Health. 2006;27:465–90. doi: 10.1146/annurev.publhealth.27.021405.102132. [DOI] [PubMed] [Google Scholar]
- 8.Barregard L, Bonde E, Ohrström E. Risk of hypertension from exposure to road traffic noise in a population-based sample. Occup Environ Med. 2009;66:410–5. doi: 10.1136/oem.2008.042804. [DOI] [PubMed] [Google Scholar]
- 9.Leon Bluhm G, Berglind N, Nordling E, Rosenlund M. Road traffic noise and hypertension. Occup Environ Med. 2007;64:122–6. doi: 10.1136/oem.2005.025866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. Bonn: World Health Organization (WHO); 2011. Burden of Disease from Environmental Noise — Quantification of Healthy Life Years Lost in Europe; p. 126. [Google Scholar]
- 11.van Kempen E, Babisch W. The quantitative relationship between road traffic noise and hypertension: A meta-analysis. J Hypertens. 2012;30:1075–86. doi: 10.1097/HJH.0b013e328352ac54. [DOI] [PubMed] [Google Scholar]
- 12.Eriksson C, Rosenlund M, Pershagen G, Hilding A, Ostenson CG, Bluhm G. Aircraft noise and incidence of hypertension. Epidemiology. 2007;18:716–21. doi: 10.1097/EDE.0b013e3181567e77. [DOI] [PubMed] [Google Scholar]
- 13.Jarup L, Babisch W, Houthuijs D, Pershagen G, Katsouyanni K, Cadum E, et al. HYENA study team. Hypertension and exposure to noise near airports: The HYENA study. Environ Health Perspect. 2008;116:329–33. doi: 10.1289/ehp.10775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dratva J, Phuleria HC, Foraster M, Gaspoz JM, Keidel D, Künzli N, et al. Transportation noise and blood pressure in a population-based sample of adults. Environ Health Perspect. 2012;120:50–5. doi: 10.1289/ehp.1103448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sorensen M, Hvidberg M, Hoffmann B, Andersen ZJ, Nordsborg RB, Lillelund KG, et al. Exposure to road traffic and railway noise and associations with blood pressure and self-reported hypertension: A cohort study. Environ Health. 2011;10:92. doi: 10.1186/1476-069X-10-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eriksson C, Nilsson ME, Willers SM, Gidhagen L, Bellander T, Pershagen G. Traffic noise and cardiovascular health in Sweden: The roadside study. Noise Health. 2012;14:140–7. doi: 10.4103/1463-1741.99864. [DOI] [PubMed] [Google Scholar]
- 17.Chaix B, Bean K, Leal C, Thomas F, Havard S, Evans D, et al. Individual/neighborhood social factors and blood pressure in the RECORD Cohort Study: Which risk factors explain the associations? Hypertension. 2010;55:769–75. doi: 10.1161/HYPERTENSIONAHA.109.143206. [DOI] [PubMed] [Google Scholar]
- 18.Van Hulst A, Thomas F, Barnett TA, Kestens Y, Gauvin L, Pannier B, et al. A typology of neighborhoods and blood pressure in the RECORD Cohort Study. J Hypertens. 2012;30:1336–46. doi: 10.1097/HJH.0b013e3283544863. [DOI] [PubMed] [Google Scholar]
- 19.Babisch W, Neuhauser H, Thamm M, Seiwert M. Blood pressure of 8-14 year old children in relation to traffic noise at home — Results of the German Environmental Survey for Children (GerES IV) Sci Total Environ. 2009;407:5839–43. doi: 10.1016/j.scitotenv.2009.08.016. [DOI] [PubMed] [Google Scholar]
- 20.Chaix B, Leal C, Evans D. Neighborhood-level confounding in epidemiologic studies: Unavoidable challenges, uncertain solutions. Epidemiology. 2010;21:124–7. doi: 10.1097/EDE.0b013e3181c04e70. [DOI] [PubMed] [Google Scholar]
- 21.Chaix B, Kestens Y, Bean K, Leal C, Karusisi N, Meghiref K, et al. Cohort profile: Residential and non-residential environments, individual activity spaces and cardiovascular risk factors and diseases — the RECORD Cohort Study. Int J Epidemiol. 2012;41:1283–92. doi: 10.1093/ije/dyr107. [DOI] [PubMed] [Google Scholar]
- 22.Benetos A, Thomas F, Pannier B, Bean K, Jégo B, Guize L. All-cause and cardiovascular mortality using the different definitions of metabolic syndrome. Am J Cardiol. 2008;102:188–91. doi: 10.1016/j.amjcard.2008.03.037. [DOI] [PubMed] [Google Scholar]
- 23.Chalmers J, MacMahon S, Mancia G, Whitworth J, Beilin L, Hansson L, et al. 1999 World Health Organization-International Society of Hypertension Guidelines for the management of hypertension. Guidelines sub-committee of the World Health Organization. Clin Exp Hypertens. 1999;21:1009–60. doi: 10.3109/10641969909061028. [DOI] [PubMed] [Google Scholar]
- 24.Thomas F, Bean K, Pannier B, Oppert JM, Guize L, Benetos A. Cardiovascular mortality in overweight subjects: The key role of associated risk factors. Hypertension. 2005;46:654–9. doi: 10.1161/01.HYP.0000184282.51550.00. [DOI] [PubMed] [Google Scholar]
- 25.Obesity: Preventing and managing the global epidemic. Report of a WHO consultation. (1-253).World Health Organ Tech Rep Ser. 2000;894:i–xii. [PubMed] [Google Scholar]
- 26.Guski R, Felscher-Suhr U. The concept of noise annoyance: How international experts see it. J Sound Vib. 1999;223:513–27. [Google Scholar]
- 27.Havard S, Reich BJ, Bean K, Chaix B. Social inequalities in residential exposure to road traffic noise: An environmental justice analysis based on the RECORD Cohort Study. Occup Environ Med. 2011;68:366–74. doi: 10.1136/oem.2010.060640. [DOI] [PubMed] [Google Scholar]
- 28.SECT; 2002. Directive 2002/49/EC of the European Parliament and of the Council of 25th June 2002 Relating to the Assessment and Management of Environmental Noise. p. 14; p. 189. [Google Scholar]
- 29.Tobin MD, Sheehan NA, Scurrah KJ, Burton PR. Adjusting for treatment effects in studies of quantitative traits: Antihypertensive therapy and systolic blood pressure. Stat Med. 2005;24:2911–35. doi: 10.1002/sim.2165. [DOI] [PubMed] [Google Scholar]
- 30.Cui JS, Hopper JL, Harrap SB. Antihypertensive treatments obscure familial contributions to blood pressure variation. Hypertension. 2003;41:207–10. doi: 10.1161/01.hyp.0000044938.94050.e3. [DOI] [PubMed] [Google Scholar]
- 31.Chaix B, Billaudeau N, Thomas F, Havard S, Evans D, Kestens Y, et al. Neighborhood effects on health: Correcting bias from neighborhood effects on participation. Epidemiology. 2011;22:18–26. doi: 10.1097/EDE.0b013e3181fd2961. [DOI] [PubMed] [Google Scholar]
- 32.Bruitparif . Paris: Bruitparif; 2011. Impact Sanitaire du Bruit dans l’agglomération Parisienne: Quantification des Années de vie en Bonne Santé Perdues: Note de Synthèse sur l’application à l’agglomération Parisienne de la Méthode de l’Organisation Mondiale de la Santé (OMS) Pour la détermination de la Morbidité liée au Bruit; p. 23. [Google Scholar]
- 33.IAU . Paris: IAU; 2013. La Circulation Routière en Ile-De-France en 2010; p. 105. [Google Scholar]
- 34.Babisch W, Wolf K, Petz M, Heinrich J, Cyrys J, Peters A. Associations between traffic noise, particulate air pollution, hypertension, and isolated systolic hypertension in adults: The KORA study. Environ Health Perspect. 2014;122:492–8. doi: 10.1289/ehp.1306981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Selander J, Bluhm G, Nilsson M, Hallqvist J, Theorell T, Willix P, et al. Joint effects of job strain and road-traffic and occupational noise on myocardial infarction. Scand J Work Environ Health. 2013;39:195–203. doi: 10.5271/sjweh.3324. [DOI] [PubMed] [Google Scholar]
- 36.Semlitsch T, Jeitler K, Hemkens LG, Horvath K, Nagele E, Schuermann C, et al. Increasing physical activity for the treatment of hypertension: A systematic review and meta-analysis. Sports Med. 2013;43:1009–23. doi: 10.1007/s40279-013-0065-6. [DOI] [PubMed] [Google Scholar]
- 37.Mikhail N, Golub MS, Tuck ML. Obesity and hypertension. Prog Cardiovasc Dis. 1999;42:39–58. doi: 10.1016/s0033-0620(99)70008-3. [DOI] [PubMed] [Google Scholar]
- 38.Briasoulis A, Agarwal V, Messerli FH. Alcohol consumption and the risk of hypertension in men and women: A systematic review and meta-analysis. J Clin Hypertens (Greenwich) 2012;14:792–8. doi: 10.1111/jch.12008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Munzel T, Gori T, Babisch W, Basner M. Cardiovascular effects of environmental noise exposure. Eur Heart J. 2014;35:829–36. doi: 10.1093/eurheartj/ehu030. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
WORKING PARTICIPANTS WITH AVAILABLE INFORMATION ON THEIR WORKPLACE
DEFINITION OF VARIABLES
MANAGEMENT OF MISSING DATA FOR TRANSPORTATION NOISE
Distribution of the RECORD participants’ places of residence, workplaces, and corresponding neighborhoods across categories of noise
Adjusted associations estimated between road traffic noise at the workplace and BP, in the samples with complete data and with imputed noise values for unexposed places (RECORD Studya)
Adjusted associations estimated between road traffic noise at the place of residence, the workplace, or in the corresponding neighborhoods and BP (RECORD Studya)
Adjusted associations estimated between RRA or road traffic noise at the workplace or at the accurately geocoded workplace and BP (RECORD Studya)
Adjusted associations estimated between RRA traffic noise at the residence and BP with 1) all the participants and 2) only among the workers (RECORD Studya)
Adjusted associations estimated between RRA traffic noise at the place of residence or the workplace and hypertension (RECORD Studya)
Adjusted associations estimated between rail traffic noise at the place of residence, the workplace, or in the corresponding neighborhoods and BP (RECORD Studya)


