Abstract
Healthcare workers (HCW) in general are considered to be at high risk during epidemics. Their training for Ebola provided by Médecins sans frontières (MSF) is presently based on imparting factual information, which does not necessarily translate into knowledge or appropriate practices. We aimed to understand the importance of risk perception during training. A total of 130 MSF-trained HCW traveling to Africa during the Ebola epidemic of 2014–2015 participated in this longitudinal cohort study. Their baseline knowledge was good but did not significantly increase after training except for minor symptoms, case fatality rate and wearing personal protective equipment as a preventive measure. Additionally, they underestimated their likelihood for contracting Ebola compared to their colleagues of same age and sex, and despite their high-risk status, they showed little concern about contracting Ebola during their mission. Our findings suggest that the use of individualized risk feedback during training in appraising erroneous perceptions will increase adherence to preventive measures.
Keywords: Comparative optimism, Ebola, healthcare workers, risk perception, training
Introduction
The ongoing Ebola viral disease (EVD) epidemic in West Africa is one of the biggest Ebola epidemics so far, infecting close to 28 073 people and killing approximately 40% (11 290) of those infected (http://apps.who.int/ebola/current-situation/ebola-situation-report-2-september-2015). The lethality of the epidemic, its easy transmissibility and open global mobility are causes enough to warrant international concern and humanitarian aid. Médecins sans frontières (MSF) alone has more than 5500 healthcare workers (HCW) spread across the affected regions, with more than 1300 expatriate workers. According to a recent World Health Organization report, 509 of 874 infected HCW died from Ebola virus in Guinea, Liberia and Sierra Leone as of 1 July 2015 (http://www.msf.org/article/ebola-pushed-limit-and-beyond). Consequently, HCW could be 21 to 32 times more at risk of infection compared to the general population (http://www.odihpn.org/the-humanitarian-space/news/announcements/blog-articles/ebola-healthcare-workers-a-hazardous-and-isolating-job#HCW).
HCW form a specialized group because they have better exposure to information as well as experience. MSF organizes training sessions for HCW before they embark on their mission. Recently they have also provided an online briefing for the aid workers (http://www.msf.org/article/ebola-online-briefing-now-available-public). The training covers a wide range of topics, including the history and epidemiology of Ebola virus, characteristics of EVD, outbreak intervention strategies, use of personal protective equipment (PPE) and sociocultural aspects of EVD (http://ecampus.msf.org/moodlemsf/mod/page/view.php?id=22246). However, some studies have reported prevalence of misinformation among voluntary health providers [1], [2], [3]. Also, a study on HCW in Lagos concluded that knowledge of Ebola did not translate into good practices for preventive measures and that on-the-job training was necessary to reinforce good practices [4]. Evidence suggests that even if environmental factors (e.g. availability of PPE, quality of PPE) and organizational factors (e.g. management policies, training) are maintained to acceptable standards, the compliance to PPE is attributed to a number of personal factors, including knowledge, beliefs and attitudes (http://www.who.int/features/2014/ebola-myths/en/). These broadly fall in the spectrum of risk perception, which in the literature has been placed at the core of health behavior models [5].
Risk perception involves two components: likelihood and severity. Severity estimate is given by the perception of severity of the disease like mortality and morbidity. Likelihood estimates are influenced by psychological components like emotions (e.g. worry, concern), illusion of control (the tendency to overestimate one's personal control over events) and comparative optimism (CO) (the tendency to consider that bad events are more likely to happen to others than to oneself) [6], [7]. An illusion of control over adverse events can decrease anxiety; as a result, a person can become more relaxed and engage in risky behaviors (http://www.nsc.org/CambpellInstituteandAwardDocuments/WP-Risk%20Preception.pdf). Comparative optimism, which is also called unrealistic optimism because it refers to the erroneous estimate that one's personal risk is less than that of the average peer of the same sex and age, has been documented in over a thousand studies and for various undesirable events such as diseases and natural disasters [8]. In general, optimistic biases lead to underestimation of risks, and those who perceive lower risks are routinely less likely to show interest in taking preventive action [9]. Personal control and CO play an important role in risk perceptions and risk acceptability. As such, they are important constructs to understand health behavior.
To our knowledge, there have been no previous Ebola-related risk perception studies in a MSF HCW cohort, and the efficacy of the training session organized by MSF has never been tested. The present prospective study was designed to fill this gap. The first objective was to identify among HCW the interrelationships between their personal control, CO, concerns about Ebola, perceived likelihood of contracting Ebola, perceived efficacy of preventive measures and risk acceptability. The second objective was to understand the knowledge spectrum of the cohort and its relationship to risk perception. The third objective was to identify changes in risk perception over time due to training session and during the mission.
Material and Methods
Participants and procedure
This study was conducted in collaboration with MSF and based in two training stations: Brussels and Geneva. The participants in this study were HCWs travelling to Ebola camps in Africa through MSF. The cohort included doctors, nurses, paramedical staff (e.g. microbiologists, epidemiologists, pathologists) and nonmedical staff (e.g. technicians, data managers, project leaders). The training sessions for Ebola were held once a week from 1 November 2014 to 28 February 2015. We contacted 300 potential MSF HCW by e-mail before their training session. Each participant was supplied with three different set of questionnaires, to be filled before the training (questionnaire 1), after the training (questionnaire 2) and after completion of their mission (questionnaire 3). Personal details and an informed consent form were taken only in the first questionnaire. Each questionnaire had both open-ended and scoring-based questions.
In questionnaire 1, open-ended questions were used to ascertain the knowledge about EVD, including symptoms of the disease, mode of transmission, case fatality and preventive measures. Two infectious disease specialists, in consensus, formulated a scoring guideline for the knowledge questions (Supplementary Material). Existing literature on Ebola as of January 2015 was used to create these guidelines. The maximum possible scores for each category were knowledge of symptoms (10), transmission (2.5), case fatality (3) and preventive measures (10). A total knowledge score was also computed by adding the four subscores (maximum possible score, 25.5). Participants were also asked about their use of different information sources for Ebola (Internet, television, print media, organizations, doctors and other) and their credibility on a 7-point Likert scale. Risk perceptions about Ebola were recorded using 7-point Likert scales with appropriate labels depending on the question (Supplementary Material). Participants were asked to indicate their perceived exposure to Ebola and concerns for contracting it. CO was measured separately using colleagues and the local African population as comparison groups. Participants were also asked about their perception of transmission, severity and likelihood for contracting Ebola during the mission. Other variables included perceived efficacy of preventive measures against Ebola, risk acceptability for contracting Ebola and perceived personal control against it.
Questionnaire 2 included additional questions to assess participants' satisfaction regarding the training. Participants were also asked to evaluate the impact of the training on their knowledge about Ebola and on their confidence to carry out their mission. Questionnaire 3 was e-mailed to all participants upon their completion of the mission and their return from Africa. It contained the same risk perception items as questionnaires 1 and 2 as well as a detailed probe on exposure during the mission.
Data analysis
Statistical analyses were conducted by SPSS 20 software (IBM SPSS, Chicago, IL, USA) and included descriptive analyses using the chi-square test, ANOVA, Student's t tests and bivariate correlations. Multiple regression analyses were performed to investigate the potential interrelationships between risk perception variables (questionnaire 1). For that purpose, we first created an optimum set of predictors by repeatedly testing and eliminating the nonsignificant variables. In addition to participants' sex and working position, the other predictors were perception about transmission, personal control, both CO measures and their two-way interactions with, respectively, sex and working position. (The interaction of sex by working position was not computed because of the small number of women among the medical staff.) We used the computational tool of Preacher et al. [10] for probing significant interaction effects. We tested this same set of predictors on different outcomes such as perceived likelihood of contracting Ebola, perceived efficacy of preventive measures, concern and knowledge scores (total and individual for each category of knowledge). Predictors that were never significant (i.e. personal control and its interaction terms, the two-way interaction terms implying perceived transmission) were deleted from the final model (resulting in nine predictors). Then we used these outcome variables as predictors for risk acceptability. Because we did not have enough participants for questionnaires 2 and 3, we did not perform multiple regression analysis on them. A complete longitudinal analysis using three time points (1, 2 and 3) could not be done because only 22 participants had completed all three questionnaires. It should be noted that in the following section, the degrees of freedom for each test may vary (1–7%) depending on how many participants answered it.
Results
Out of 300 participants whom we contacted, we received 130 first questionnaires (response rate 43.3%), with a male-to-female ratio of 1.4:1. There were 59 medical (doctors and nurses) and 70 nonmedical personnel to be posted in Sierra Leonne (53), Liberia (32) and Guinea (29). The chi-square test revealed a significant gender difference among the medical personnel (χ2(1, n = 129) = 20.1, p <0.01), where 15 were women and 44 were men. This difference was less pronounced in the nonmedical positions, where out of 70 staff there were 38 women and 32 men. From the initial 130 responses, we received 70 second (53% response rate) and 37 third (28.4% response rate) questionnaires.
Information sources and knowledge scores
Organization was the most commonly used source of information (M 5.48, SD 1.36) which was also rated as very credible (M 6.08, SD 0.94). This was closely followed by the Internet (Musage = 5.4, SD 1.42; Mcred = 4.44, SD 1.27), print media (Musage = 4, SD 1.72; Mcred = 4.2, SD 1.27), television (Musage = 3.25, SD 1.86; Mcred = 3.46, SD 1.41) and doctors (Musage = 2.69, SD 2.1; Mcred = 5.06, SD 1.55). Student's t tests revealed no significant effect of participants' sex or working position. Credibility and usage of all the sources were positively correlated (Pearson's correlation 0.45 < rs <0.59, ps < .01), indicating that the more frequently used sources were also rated highly credible.
Comparison of total knowledge scores before training (M 11.86, SD 2.8) and after training (M 11.74, SD 2.26) using the paired t test revealed no significant differences (even after considering effect of sex and position). It is noteworthy that the knowledge score of the sample was significantly below the midpoint (12.75) of the possible maximum score (M 12.09, SD 2.89, t(126) = −2.59, p <0.02). Although the training had no impact on the global knowledge scores, it did have an impact on specific answers within the symptom, case fatality and preventive measure categories. As indicated by McNemar's chi-square test, there was a posttraining increase in respondents answering arthralgia (p 0.004) and conjunctivitis (p 0.001). Among the major symptoms, fever, vomiting and diarrhoea were well identified by the participants both before and after training. There was a tendential decrease in participants responding haemorrhage as the main symptom (Table 1). There were no significant posttraining changes in responses for knowledge of transmission. For knowledge of transmission, more than 90% of the participants were aware of Ebola virus transmission through the body fluids of infected persons. The response rates for nonhuman modes of transmission, such as animal-to-human transmission (18.6%), infected dead bodies (12–16%) and eating bush meat (1.4%) were very low. A negligible percentage of participants (2%) had indicated aerosol transmission before training. For preventive measures, no significant knowledge was acquired between the two sessions except for wearing PPE (i.e. 77.1–80%, p <0.05). There was a significant increase in posttraining reporting the correct fatality rates (i.e. 50–80%, p 0.011).
Table 1.
Percentage of correct responses to knowledge questions before (questionnaire 1) and after (questionnaire 2) training session
| Knowledge category | Before training | After training |
|---|---|---|
| Transmission (M 1.22, SEM 0.04) | ||
| Animal to human | 18.6 | 18.6 |
| Body fluids (living) | 94.3 | 94.3 |
| Body fluids (dead) | 12.9 | 15.7 |
| Eating bush meat | 1.4 | 1.4 |
| Eating meat (unspecified) | 5.7 | 4.3 |
| Aerosol transmission | 2.9 | 0 |
| Don't know | 0 | 0 |
| Symptoms (M 5.48, SEM 0.16) | ||
| Haemorrhage† | 62.9 | 47.1 |
| Fever | 88.6 | 80.0 |
| Myalgia | 37.1 | 34.3 |
| Vomiting* | 71.4 | 67.1 |
| Headache | 40.0 | 45.0 |
| Diarrhoea | 62.9 | 68.9 |
| Rash | 0 | 4.3 |
| Sore throat | 12.9 | 15.7 |
| Fatigue | 37.1 | 51.4 |
| Flulike symptoms | 8.6 | 11.4 |
| Hiccups† | 11.4 | 21.4 |
| Arthralgia* | 15.7 | 35.7 |
| Cough | 1.4 | 7.1 |
| Dyspnoea | 1.4 | 1.4 |
| Blurred vision | 2.9 | 1.4 |
| Neurologic symptoms | 8.6 | 2.9 |
| Multiple organ failure | 14.3 | 10 |
| Conjunctivitis* | 4.3 | 20 |
| Fatality (M 1.74, SEM 0.05) | ||
| 50–80%* | 71.4 | 87.1 |
| 35–50% | 1.4 | 0 |
| <35 | 2.9 | 0 |
| >80 | 7.1 | 0 |
| 20–90% | 4.3 | 5.7 |
| Don't know | 0 | 1.4 |
| Preventive measures (M 3.25, SEM 0.14) | ||
| Avoid contact (2 m distance) | 78.6 | 87.1 |
| Wear PPE* | 77.1 | 80 |
| Disinfection (self or surfaces) | 57.1 | 68.6 |
| Safe burial | 10 | 5.7 |
| Surveillance of contacts | 8.6 | 1.4 |
| Avoid contact with sick animals/use gloves | 2.9 | 0 |
| Avoid consumption of specific meat (or have well-cooked meat) | 5.7 | 0 |
| Safe sex for 3 months after recovery | 4.3 | 0 |
PPE, personal protective equipment.
*p <0.05, †p <0.07.
Training satisfaction
Regardless of their sex and working position, the participants reported (as indicated by one-sample t tests with the midpoint of the scale as the test value) that the training session added to their knowledge (M 5.93, SD 1.05, t(71) = 47.51, p <0.01) and increased their confidence in the mission (M 5.5, SD 1.08, t(71) = 42.91, p <0.01). They also reported being highly satisfied with their training (M 6.3, SD 0.81, t(71) = 66.77, p <0.01). It is interesting to note that though the participants reported satisfactory knowledge gain by the training, no correlation was observed between these scores and knowledge scores after training.
Exposure and adverse events during the mission
Among the 37 participants who completed the third questionnaire, ten participants reported experiencing adverse events. Three of them indicated accidental exposure during their mission (either due to failure of protective equipment, like a mask falling off or exposure without equipment among staff) and the lack of training provided for such situations. Two participants reported a lack of training regarding interaction with local children. The need for differential training for those serving in Ministry of Health hospitals compared to those serving in MSF camps was also stressed by two respondents.
Relationships between risk perception variables
One-sample t tests revealed that the scores of concern (M 2.99, SD 1.31, t(128) = 25.87, p <0.001) were significantly below the midpoint of the scale, suggesting that participants were only slightly worried about Ebola. CO with colleagues (M 4.17, SD 0.85, t(127) = 55.59, p <0.01) and with the local population (M 5.23, SD 1.23, t(127) = 48.04, p <0.01) were both significantly above the midpoint of the scale. A paired t test confirmed that participants' CO was higher when the target group was the local population rather than other colleagues (t(125) = −8.3, p <0.001).
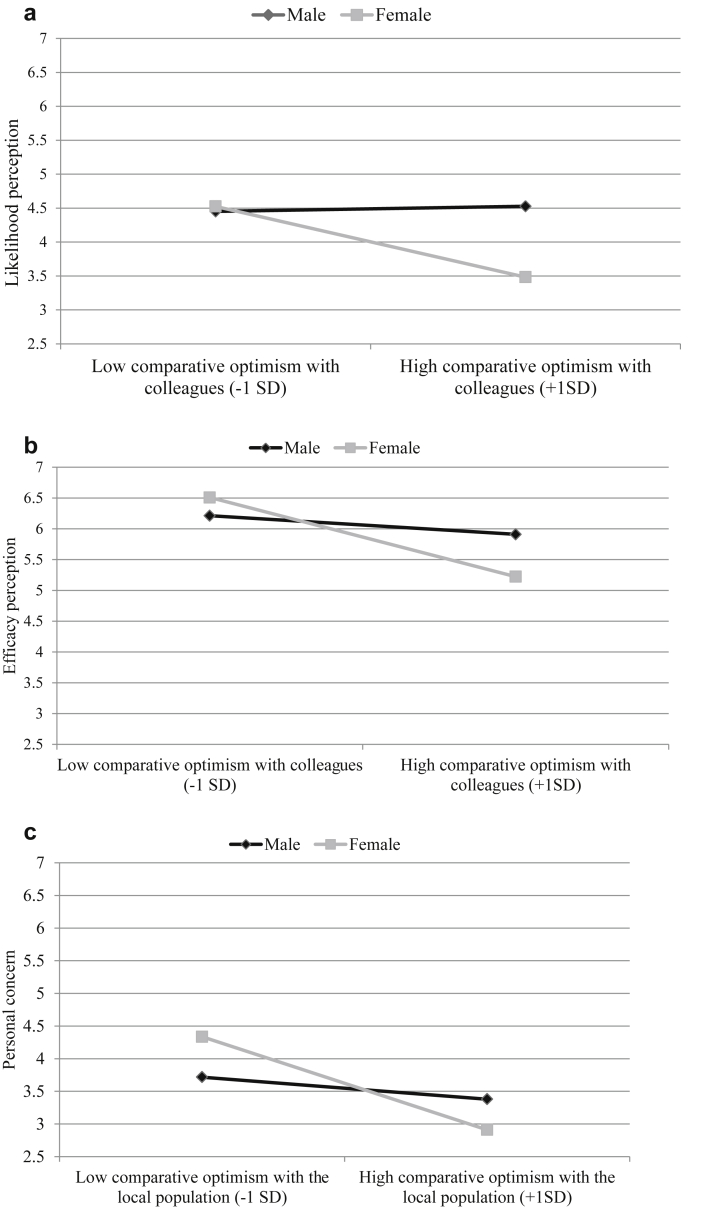
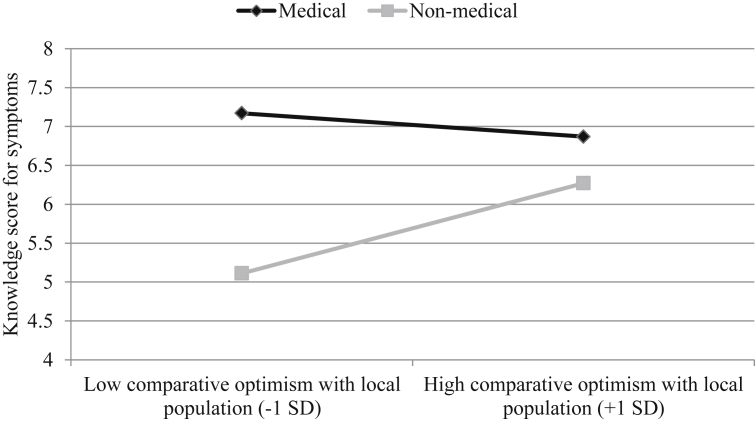
Table 2 presents the results of regression models with significant variances (bivariate correlations are provided in the Supplementary Material). The perceived likelihood of contracting Ebola was significantly predicted by participants' sex: women reported a lower likelihood of contracting Ebola than men. Interestingly, this effect was moderated by CO with colleagues (Fig. 1a). Higher CO with colleagues was associated with lower perceived likelihood for contracting Ebola only among women (b = −0.62, t = −2.3, p 0.02). Perceived efficacy of preventive measures was also a function of CO with colleagues only in women (b = −0.76, t = −4.7, p <0.01), with higher CO being associated with lower perceived efficacy of preventive measures against Ebola (Fig. 1b). For concern as outcome, interaction between participants' sex and CO with local population showed borderline significance. Simple slope analysis revealed that higher CO with local population was associated with lower concern for contracting Ebola among women only (b = −0.56, t = −2.54, p 0.01; Fig. 1c). In the fourth model, the knowledge score of symptoms was significantly predicted by participants' working position. Not surprisingly, nonmedical staff possessed a lower knowledge of symptoms than medical staff. This effect was moderated by CO with the local population (Fig. 2): the difference of knowledge between medical and nonmedical staff was observed among participants with lower CO with the local population (b = −2.06, t = −4.03, p <0.01).
Table 2.
Summary of multiple regression analyses for variables predicting perceived likelihood, perceived efficacy, concern and knowledge of symptoms
| Predictor | Perceived likelihood |
Perceived efficacy |
Concern |
Knowledge of symptoms |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b | p | 95% CI | b | p | 95% CI | b | p | 95% CI | b | p | 95% CI | |
| Sexa | −0.49 | 0.04* | −0.96, −0.01 | −0.2 | 0.19 | −0.48, 0.1 | 0.25 | 0.31 | −0.24, 0.73 | 0.11 | 0.76 | −0.59, 0.81 |
| Working positionb | −0.19 | 0.43 | −0.66, 0.28 | −0.09 | 0.54 | −0.38, 0.2 | 0.07 | 0.78 | −0.41, 0.55 | −1.32 | 0.01** | −2.02, −0.64 |
| Perceived transmission | 0.33 | 0.01** | 0.18, 0.49 | 0.001 | 0.98 | −0.09, 0.1 | 0.02 | 0.18 | −0.14, 0.18 | −0.14 | 0.22 | −0.37, 0.09 |
| CO colleagues | 0.05 | 0.86 | −0.43, 0.52 | −0.18 | 0.23 | −0.47, 0.11 | 0.23 | 0.35 | −0.26, 0.72 | 0.25 | 0.49 | −0.46, 0.95 |
| CO local population | −0.09 | 0.51 | −0.38, 0.19 | −0.07 | 0.43 | −0.24, 0.11 | −0.04 | 0.79 | −0.33, 0.25 | −0.12 | 0.56 | −0.54, 0.29 |
| Sexa CO colleagues | −0.66 | 0.04* | −1.28, −0.05 | −0.58 | 0.01** | −0.96, −0.2 | 0.09 | 0.79 | −0.55, 0.72 | 0.48 | 0.3 | −0.44, 1.4 |
| Sexa CO local | 0.15 | 0.46 | −0.25, 0.54 | 0.05 | 0.73 | −0.21, 0.3 | −0.37 | 0.07† | −0.77, 0.04 | −0.03 | 0.93 | −0.61, 0.55 |
| Positiona CO colleagues | −0.06 | 0.83 | −0.64, 0.52 | 0.51 | 0.01** | 0.16, 0.87 | −0.33 | 0.27 | −0.93, 0.26 | −0.05 | 0.91 | −0.92, 0.82 |
| Positiona CO local | −0.24 | 0.22 | −0.64, 0.15 | 0.16 | 0.2 | −0.09, 0.41 | −0.21 | 0.31 | −0.61, 0.19 | 0.59 | 0.05* | 0.01, 1.18 |
| % of variance explained by model | 22.7 | 17.3 | 7.1 | 12 | ||||||||
CI, confidence interval; CO, comparative optimism.
*p <0.05; †p = 0.07.
**p = 0.01
Male coded 0, female coded 1.
Medical coded 0, nonmedical coded 1.
Fig. 1.
(a) Perceived likelihood of contracting Ebola among HCW as function of sex and CO with colleagues. (b) Perceived efficacy of preventive measures against Ebola as function of sex and CO with colleagues. (c) Reported personal concern about Ebola as function of sex and CO with local population. CO, comparative optimism; HCW, healthcare worker.
Fig. 2.
Knowledge scores for symptoms as function of working position and comparative optimism with local population.
Finally, to ascertain determinants of risk acceptability, we regressed it on sex, working position, perceived likelihood (mean centred), efficacy perception (mean centred), personal control measures (mean centred) and knowledge scores. These accounted for 6.8% of the variance in risk acceptability measures (p 0.035). Those having a higher efficacy perception (b = 0.46 s(95% confidence interval 0.08–0.85), t = 2.36, p 0.02) and higher personal control (b = 0.21 (95% confidence interval 0.01–0.41), t = 2.08, p 0.04) exhibited a higher risk acceptability of Ebola.
Discussion
To our knowledge, this is the first risk perception study on expatriate HCW travelling to Africa during an Ebola epidemic. Considering the specialized nature of our sample, we expected differences in knowledge relative to other cohorts. In studies among regular travellers, a sizeable percentage reported airborne transmission of Ebola (range 17–74%), human transmission by asymptomatic individuals (74%) or not knowing the mode of transmission (22%) [11], [12], [13]. Studies among local healthcare volunteers in Africa also reported misinformation like airborne transmission (range 23–53.1%), insect transmission (20.2%) and environment-to-human transmission (range 73–78%) [1], [2], [3]. In comparison to this, the percentage of participants reporting misinformation in our cohort was negligible. Therefore, and not surprisingly, MSF-trained HCW had a greater expertise on Ebola than the general population. In addition, they used different sources of information relative to the general population. Local population in African settings relied on radio (85–95%) for their information on Ebola (http://newswire.crs.org/wp-content/uploads/2014/10/Ebola-Virus-Disease-National-KAP-Study-Final-Report_-final.pdf; http://www.unicef.org/cbsc/files/KAP-Study-Liberia-March-2015.pdf) [14]. Other studies among regular travellers conducted in Germany [12], Australia [11] and the United States [15] showed that Internet was the most common source of information. Here, we observed that health organizations were the most preferred source of information, closely followed by the Internet.
It is noteworthy that the knowledge of the HCW in the present study was below the average score. A very high response for human-to-human transmission and a very low response for other modes of transmission indicated a lack of complete knowledge. Similarly, preventive measure like PPE, disinfection and avoidance of contact were cited much more than other modes of prevention. A recent study on HCW in Nigeria reported a similar observation: a posttraining decrease in the correct response to the statement, “Ebola is found only in humans,” which was attributed to selective stressing on certain subjects and overlooking the others [1]. Our findings also revealed a discrepancy between how participants perceived the training session and its real impact on their knowledge about Ebola. Despite no significant knowledge gain after training, the HCW perceived that the training added to their existing knowledge. Few participants reported the lack of the training and preparation for addressing some key issues during the mission, including accidental exposure, dealing with children, community interaction and working practices in health centres other than those run by MSF. Thus, disseminating the complete information on Ebola (rather than stressing a few key points) and equipping the HCW adequately for adverse situations will help improve the observed impact of the training.
Risk perception, measured by subjective probability of contracting Ebola (likelihood) and associated negative emotion (concern), was strongly influenced by constructs of positive illusions (CO and personal control). There is strong evidence in psychological research that these positive illusions can reduce perceptions of vulnerability to health threats and reduce preventive behavior [7], [16], [17], [18]. In line with this, we found that the illusion of control made the risk of contracting Ebola more acceptable. In addition, the participants underestimated their personal risk of contracting Ebola compared to average peers of the same sex and age. This unrealistic optimism led to women reporting lower likelihood of contracting Ebola, lower perceived efficacy of preventive measures and lower concern for contracting Ebola relative to men. These differences can explain why knowledge and practices of HCW do not correlate linearly and shed light on the need for differential training.
Participation in the study was voluntary, and only those motivated enough responded to the questionnaires. We also observed attrition of participants over time and thus could not exploit longitudinal data. In November and December, the first two questionnaires were sent by e-mail, and the response rate was approximately 30%. From January, the first and second questionnaires were administered manually before and after the training session, respectively. This ensured high response rates. The last questionnaire could be sent only by e-mail, and this again reduced the response rate. The return dates of the participants frequently varied, and thus, despite repeated e-mails, there was no response. Additionally, e-mails going to the spam folder, Internet access and motivation of the participants could be responsible for the high attrition rate. Manual administration of the last questionnaire (either before departure from Africa or at the postmission briefing) could help reduce attrition. Given this sampling bias, one could have expected higher knowledge from motivated participants, which was not the case. Despite these limitations, our study has statistically exploited the available data enough to make some useful recommendations that could help improve risk communication to HCW.
Risk communication for Ebola by MSF presently includes a description of the disease and its epidemiology, diagnosis, treatment and prevention, without mentioning the individual probability of contracting Ebola for a HCW (http://ecampus.msf.org/moodlemsf/mod/page/view.php?id=22246). However, simply stating the risks impersonally and quoting existing data may not have the desired effect. It has been demonstrated that although risk communication leads to an increase in general awareness, it may also foster an underestimation of the magnitude of risk for oneself [19]. Debiasing CO, though challenging, is necessary in light of the available results. Some previous studies have attempted this by, first, focusing on self-risk estimates [20]. A randomized trial demonstrated that individualized risk feedback was effective in increasing the perceived stroke risk in people who underestimated it and in decreasing perceived cancer risk in those who overestimated it [21]. It will thus be useful to provide HCW with individual risk estimates considering both sex and working position, expected efficacy of preventive measure (100% vs. less than 100%) and transmission (low vs. high) to correct false perceptions. Second, providing feedback about the comparison group (in this case, peers and the local African population) and explaining the risk differences will also appraise CO among HCW, leading to a more precise self-estimate [20]. It could be argued that precise estimates might induce fear among participants, but it could also prove profitable by making them adhere more strongly to preventive measures.
Conclusion
The present findings suggest that understanding HCW knowledge and risk perception would form an integral part of HCW training session (in general) and that risk appraisals should be customized according to these data. Present studies using the knowledge, attitude and practices method do not take into consideration variables of positive illusions, which could explain the low knowledge and wrong practices among HCW. However, more research is needed to observe the impact of targeted approach, and longitudinal studies are required to observe the size of the impact. Also, maintaining the sample size through the study would be essential in observing the longitudinal changes in attitudes of HCW. This information will help all organizations to provide an improved training for future epidemics whereby erroneous health behavior due to erroneous risk perception could be minimized.
Acknowledgements
We extend our gratitude to all the participants who volunteered for this study. We also thank M. Ferrier, MSF Paris, our contact for MSF, for introducing us to the MSF team in Geneva and Brussels.
Footnotes
Targeted training is necessary to improve healthcare workers' knowledge about Ebola and appraise their erroneous risk perceptions.
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.nmni.2016.04.010.
Conflict of Interest
None declared.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Patel U., Pharr J.R., Ihesiaba C., Oduenyi F.U., Hunt A.T., Patel D. Ebola outbreak in Nigeria: increasing Ebola knowledge of volunteer health advisors. Global J Health Sci. 2015;8:72–78. doi: 10.5539/gjhs.v8n1p72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iliyasu G., Ogoina D., Otu A.A., Dayyab F.M., Ebenso B., Otokpa D. A multi-site knowledge attitude and practice survey of Ebola virus disease in Nigeria. PLoS One. 2015;10:e0135955. doi: 10.1371/journal.pone.0135955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alfaki M.M., Salih A.M., Elhuda D.A., Egail M.S. Knowledge, attitude and practice of health care providers toward Ebola virus disease in hotspots in Khartoum and White Nile states, Sudan, 2014. Am J Infect Control. 2016;44(1):20–23. doi: 10.1016/j.ajic.2015.07.035. [DOI] [PubMed] [Google Scholar]
- 4.Oladimeji A.M., Gidado S., Nguku P., Nwangwu I.G., Patil N.D. Ebola virus disease—gaps in knowledge and practice among healthcare workers in Lagos, August 2014. Trop Med Int Health. 2015;20:1162–1170. doi: 10.1111/tmi.12528. [DOI] [PubMed] [Google Scholar]
- 5.Brewer N.T., Chapman G.B., Gibbons F.X., Gerrard M., McCaul K.D., Weinstein N.D. Meta-analysis of the relationship between risk perception and health behavior: the example of vaccination. Health Psychol. 2007;26:136–145. doi: 10.1037/0278-6133.26.2.136. [DOI] [PubMed] [Google Scholar]
- 6.Langer E.J., Roth J. Heads I win, tails it's chance: the illusion of control as a function of the sequence of outcomes in a purely chance task. J Personality Soc Psychol. 1975;32:951–955. [Google Scholar]
- 7.Weinstein N.D. Unrealistic optimism about future life events. J Personality Soc Psychol. 1980;39:806–820. [Google Scholar]
- 8.Shepperd J.A., Klein W.M.P., Walters E.A., Weinstein N.D. Taking stock of unrealistic optimism. Perspect Psychol Sci. 2013;8:395. doi: 10.1177/1745691613485247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schneider S.L. In search of realistic optimism: meaning, knowledge and warm fuzziness. Am Psychologist. 2001;56:250–263. doi: 10.1037//0003-066x.56.3.250. [DOI] [PubMed] [Google Scholar]
- 10.Preacher K.J., Curran P.J., Bauer D.J. Computational tools for probing interaction effects in multiple linear regression, multilevel modeling, and latent curve analysis. J Educ Behav Stat. 2006;31:448. [Google Scholar]
- 11.Alqahtani A.S., Wiley K.E., Willaby H.W., BinDhim N.F., Tashani M., Heywood A.E. Australian Hajj pilgrims' knowledge, attitude and perception about Ebola, November 2014 to February 2015. Euro Surveill. 2016 doi: 10.2807/1560-7917.es2015.20.12.21072. In press. [DOI] [PubMed] [Google Scholar]
- 12.Rübsamen N., Castell S., Horn J., Karch A., Ott J.J., Raupach-Rosin H. Ebola risk perception in Germany, 2014. Emerg Infect Dis. 2014;21:1012–1018. doi: 10.3201/eid2106.150013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gesser-Edelsburg A., Shir-Raz Y., Hayek S., Sassoni-Bar Lev O. What does the public know about Ebola? The public's risk perceptions regarding the current Ebola outbreak in an as-yet unaffected country. Am J Infect Control. 2015;43:669–675. doi: 10.1016/j.ajic.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 14.Gidado S., Ladimeji A.M., Roberts A.A., Nguku P., Nwangwu I.G., Waziri N.E. Public knowledge, perception and source of information on Ebola virus disease—Lagos, Nigeria; September, 2014. PLoS Curr. 2015;7 doi: 10.1371/currents.outbreaks.0b805cac244d700a47d6a3713ef2d6db. pii:ecurrents.outbreaks.0b805cac244d700a47d6a3713ef2d6db. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rolinson J.J., Hanoch Y. Knowledge and risk perceptions of the Ebola virus in the United States. Prev Med Rep. 2015;2:262–264. doi: 10.1016/j.pmedr.2015.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Davidson K., Prkachin K. Optimism and unrealistic optimism have an interacting impact on health-promoting behavior and knowledge changes. Pers Soc Psychol Bull. 1997;23:617–625. [Google Scholar]
- 17.Peterson C., Stunkard A.J. Personal control and health promotion. Soc Sci Med. 1989;28:819–828. doi: 10.1016/0277-9536(89)90111-1. [DOI] [PubMed] [Google Scholar]
- 18.Ziff M.A., Conrad P., Lachman M.E. The relative effects of perceived personal control and responsibility on health and health-related behaviors in young and middle-aged adults. Health Educ Q. 1995;22:127–142. doi: 10.1177/109019819502200111. [DOI] [PubMed] [Google Scholar]
- 19.Renner B., Schwarzer R. Social–cognitive factors in health behavior change. In: Suls J., Wallston K.A., editors. Social psychological foundations of health and illness. Blackwell Publishers; Malden, MA: 2008. pp. 169–191. [Google Scholar]
- 20.Rose J.P. Debiasing comparative optimism and increasing worry for health outcomes. J Health Psychol. 2011;17:1121–1131. doi: 10.1177/1359105311434051. [DOI] [PubMed] [Google Scholar]
- 21.Kreuter M.W., Strecher V.J. Changing inaccurate perceptions of health risk: results from a randomized trial. Health Psychol. 1995;14:56–63. doi: 10.1037//0278-6133.14.1.56. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.