Abstract
Acute flare up of hepatitis B in noncirrhotic liver with rapid liver function deterioration is a critical condition. This flare up of hepatitis B may be subsided under medical treatments, otherwise urgent liver transplantation is needed. However, the necessity of urgent liver transplantation is hard to decide. In this institute, the indications of urgent liver transplantation for acute flare up of hepatitis B in noncirrhotic liver were settled according to the model for end-stage liver disease (MELD) scores: once upon MELD scores ≥35 (criterion 1) or MELD score < 35 at beginning and increased in the subsequent 1 to 2 weeks (criterion 2). This study was to examine whether MELD score criteria for liver transplantation were valid in such an urgent condition. Eighty-three patients having acute flare up of hepatitis B virus with total bilirubin ≥17.5 mg/dL were included in this study. Among 83 patients, 20 patients met criterion 1. Five patients were transplanted and 15 patients died of liver failure with a median survival of 17 days. Fifty-one patients met criterion 2. Nineteen were transplanted, 30 patients died of liver failure with a median survival of 23.5 days, and 2 patients recovered from this critical condition. The other 12 patients did not meet criteria 1 and 2, and urgent liver transplantation was spared although 5 patients needed liver transplantation in subsequent 2 to 3 months. Therefore, the sensitivity of MELD score criteria for urgent liver transplantation was 100% and specificity was 85.7%. In conclusion, determination of urgent liver transplantation for hepatitis B with acute liver failure is crucial. MELD score criteria are valid to make a decision of urgent liver transplantation for hepatitis B patients with acute flare up and liver failure.
INTRODUCTION
Hepatitis B virus (HBV) infection is a common viral hepatitis in South-East Asia. The natural course of HBV infection includes immune tolerant phase, immune clearance phase, and inactive residual phase.1 During immune clearance phase, HBV viral hepatitis may flare up repeatedly and result in cirrhosis.1,2 When liver function in cirrhotic liver proceeds into decompensated, it is no doubt that liver transplantation is the only effective way to save patients’ lives. However, some patients may be beyond this expected natural course of HBV infection.3 In their immune clearance phase, the provoked strong immune reaction in the 1st flare up may cause severe hepatitis with marked elevation of aspartate aminotransferase (AST) and alanine aminotransferase (ALT) and leads to acute liver failure.4 In such a circumstance, urgent liver transplantation is crucial to rescue lives.5
Acute hepatitis B flare up is defined as an abrupt elevation of ALT more than 5 folds of upper normal limit.6 This flare-up may progress to deteriorate liver function and result in acute liver failure which is defined as acute liver insult manifesting as jaundice and coagulopathy complicated with ascites and/or encephalopathy within 4 weeks.7 Acute liver failure may recover spontaneously or needs liver transplantation to save lives.8 If the patients have the chance to recover by medical treatment, liver transplantation is not only unnecessary but also endangers the patients to expose to transplant surgery and immunosuppressive agents. Nevertheless, if the decision of liver transplantation is made too late, the patients may be too sick to have liver transplantation and die of liver failure. Therefore, to decide the timing and necessity of liver transplantation for acute liver failure resulted from HBV flare up in noncirrhotic liver is not easy. To solve this dilemma, we settled criteria of urgent liver transplantation according to the model of end-stage liver disease (MELD) score for noncirrhotic patients with acute HBV flare up and liver failure before.9 Based on King College's criteria,10 the evaluation of liver transplantation necessity is initiated when the level of serum total bilirubin is ≥17.5 mg/dL. The indication of urgent liver transplantation is once upon MELD scores ≥35 or MELD score <35 at beginning and increased in the subsequent 1 to 2 weeks.9
The indication of urgent liver transplantation for the patients with acute HBV flare up and liver failure in noncirrhotic livers is based on this MELD score criteria at our institute since 2008. In this study, we collected the data of HBV patients with acute flare up and liver failure to examine the validation of MELD score criteria as indicators of urgent liver transplantation for HBV patients with acute flare up in noncirrhotic liver.
MATERIALS AND METHODS
Patients
Eighty-three noncirrhotic patients having acute flare up of HBV and liver failure from 2008 to 2014 were included in this study. The criteria of the patients included in this study were whose serum total bilirubin was ≥17.5 mg/dL, no history of acute hepatitis attacked before and imaging studies showed the liver was noncirrhotic. These patients were all evaluated for necessity of liver transplantation. The clinical characteristics, laboratory data, and survival time were all collected. Eleven patients referred for assessment of liver transplantation but their total bilirubin <17.5 mg/dL were not included in this study and their clinical data were collected only for a reference. This study was approved by local Ethic Committee of Chang-Gung Memorial Hospital.
MELD Score Calculation
The 1st MELD score was calculated when serum total bilirubin was ≥17.5 mg/mL. Subsequent MELD scores were calculated twice a week to help making a decision of liver transplantation.
Indications of Listing Patients for Liver Transplantation
The decision of urgent liver transplantation was determined by MELD score which was described in our previous study.9 The 1st criterion of urgent liver transplantation was MELD ≥35 (criterion 1). The 2nd criterion was MELD <35 initially, but MELD increased in subsequent 1 to 2 weeks (criterion 2). If the patients did not meet 2 criteria, they would be treated by antiviral agents continuously and followed up closely.
Liver Transplantation
All the patients meeting criteria 1 and 2 were listed for liver transplantation and registered in Taiwan Network of Organ Sharing to wait deceased liver allografts. However, organ donation was always short in Taiwan. Living donor liver transplantation would be sincerely considered due to urgent condition of the patients. If members of the family were willing to donate part of the liver, donor evaluation would be proceed immediately including social and psychiatric evaluation, laboratory tests, liver size, vascular, and biliary anatomy. When donor evaluation was complete and liver donation was approved by the Ethic Committee of Chang-Gung Memorial Hospital, living donor liver transplantation was undergone.
Biostatistics
Paired Student t test was used to analyze continuous variables. Categorical variables were analyzed by either Chi-squared test or Fisher exact test. All pairwise multiple comparisons were done by Holm–Sidak method. Meanwhile, the survival rates were calculated using the Kaplan–Meier method and compared between groups using the log-rank test. The statistical analyses were all performed with SigmaPlot 12.3 software for Windows (Systat Softwave, Inc., San Jose, CA). P < 0.05 was considered statistically significant.
RESULTS
Patients
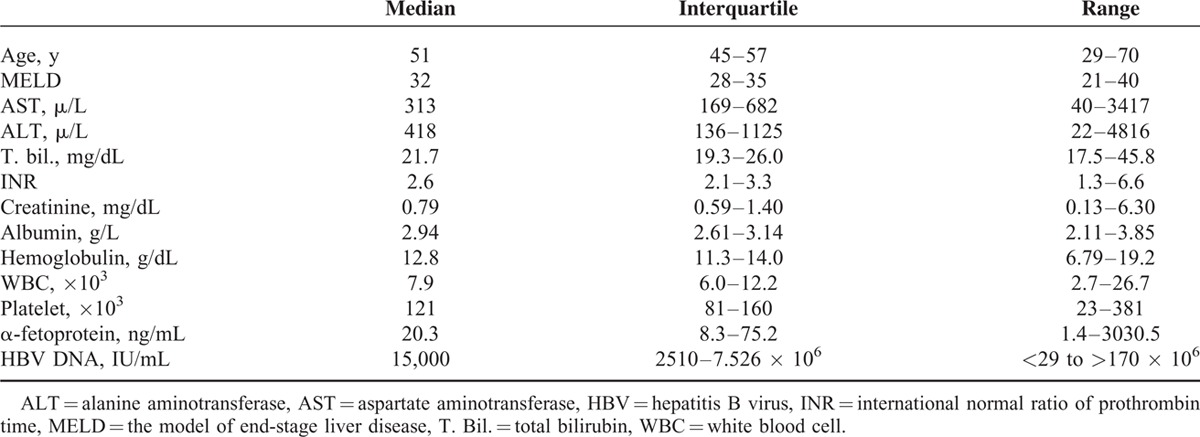
From 2008 to 2014, 83 noncirrhotic patients (75 males and 8 females) with acute flare up of HBV and liver failure were included in this study. No patients had the history of chemotherapy for cancers. Median (interquartile) age of these patients was 51 (45–57) years with a range from 29 to 70 years. At initiation of liver transplantation evaluation, median (interquartile) serum level of total bilirubin was 21.7 (19.3–26.0) mg/dL with a range from 17.5 to 45.8 mg/dL. The median (interquartile) MELD score in the 1st evaluation was 32 (28–35) with a range from 21 to 40. The serum values of AST and ALT varied greatly because the patients might visit our emergency room when they felt sick or were admitted at other hospital for 1 to 2 weeks and referred to our department for liver transplantation (Table 1). All patients were treated with antiviral agents including entecavir for 51 patients, lamivudine for 16 patients, tenofovir for 13 patients, and telbivudine for 3 patients. The viral load varied greatly. The median HBV DNA level was 0.015 × 106 IU/mL with a range from undetectable to more than 170 × 106 IU/mL (Table 1). HBe Ag and anti-HBe were measured in 70 patients and the results showed 15 (21.4%) patients were positive for HBe Ag and 63 (90%) patients were positive for anti-HBe.
TABLE 1.
Characteristics of 83 Patients at the Beginning of Evaluation for Liver Transplantation
Patient Grouping According to MELD Score
Among 83 patients, 20 patients met criterion 1 with MELD ≥35 in their 1st MELD score calculation. Liver transplantation was recommended immediately and all the patients were listed for transplantation. At this time, 11 (55%) patients had hepatic encephalopathy. Endoscopic examination was performed in 15 patients and 9 (60%) patients had mild esophageal varices. Finally, 5 patients were transplanted (4 deceased and 1 living donor) and the other 15 patients died of liver failure without transplantation because liver grafts were not available.
Another 51 patients met criterion 2. The initial calculated MELD score was 29.6 ± 3.1. In the subsequent week, the MELD score was increased to 32.2 ± 5.2 (P < 0.001). Liver transplantation was recommended and all these patients were listed for liver transplantation. At this time, 20 (39.2%) patients had hepatic encephalopathy. Endoscopic examination was performed in 37 patients and 23 (62.2%) patients had mild esophageal varices. Finally, 19 patients had liver transplantation including 8 deceased and 11 living donor liver transplantations. For the other 32 patients, 30 patients expired because liver allografts were not available and 2 patients recovered from this urgent condition.
In this study, the other 12 patients did not meet criteria 1 and 2. Their initial MELD score was 27.9 ± 4.2. In the subsequent week, MELD score decreased to 26.1 ± 3.2 (P = 0.174 in paired T-test). Urgent liver transplantation was not recommended, but the patients were followed up closely. Among the patients, only 1 (8.3%) patient had hepatic encephalopathy. Endoscopic examination was performed in 5 patients and 3 (60%) patients had mild esophageal varices. In the subsequent 2 to 3 months, 5 patients had persisted abnormal liver function which proceed into Child–Pugh C liver cirrhosis and 7 patients fully recovered with normal liver function. Finally, among the 5 patients in Child–Pugh C liver function, 1 patient was transplanted and 4 patients died of liver failure (Figure 1).
FIGURE 1.
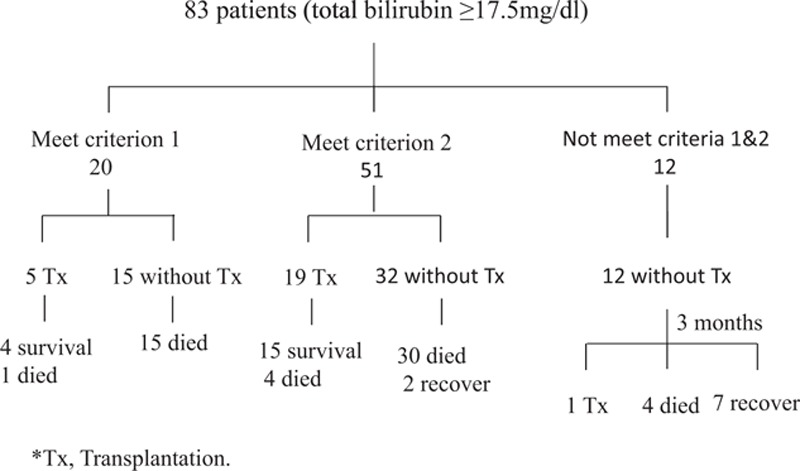
Flow chart of managements for 83 patients with acute flare up of hepatitis B and total bilirubin ≥17.5 mg/dL. Tx = liver transplantation.
For the 11 patients excluded in this study because the level of total bilirubin did not reach 17.5 mg/dL, all patients survived without liver transplantation.
Survival Rates for the Patients Meeting Criteria 1 and 2
Seventy-one patients of the 83 patients (85.5%) meeting criteria 1 and 2 were recommended and listed for urgent liver transplantation. Finally, 24 patients (33.8%) were transplanted. The MELD score at transplantation was 37.1 ± 3.1. The explant livers were shrunken with a median (interquartile) volume reduction to 64.8% (58.6–75.1%) of standard liver volume.11 The 3-month, 1-year, and 3-year survival rates were 82.4%, 73.2%, and 67.1%, respectively. For the patients without liver transplantation, 1-, 2-, and 3-month survival rates were 28.3%, 8.7%, and 4.4%, respectively (P < 0.001, Figure 2). Among 24 patients having liver transplantation, 12 patients had deceased donor liver transplantation and the other 12 had living donor liver transplantation. The survival rates between deceased liver and living donor liver transplantation were not different. The 1-, 2-, and 3-year survival rates were 64.8%, 64.8%, and 64.8%, respectively, for the patients with deceased liver transplantation and 75.0%, 62.5%, and 62.5%, respectively, for the patients with living donor liver transplantation (P = 0.938, Figure 3).
FIGURE 2.
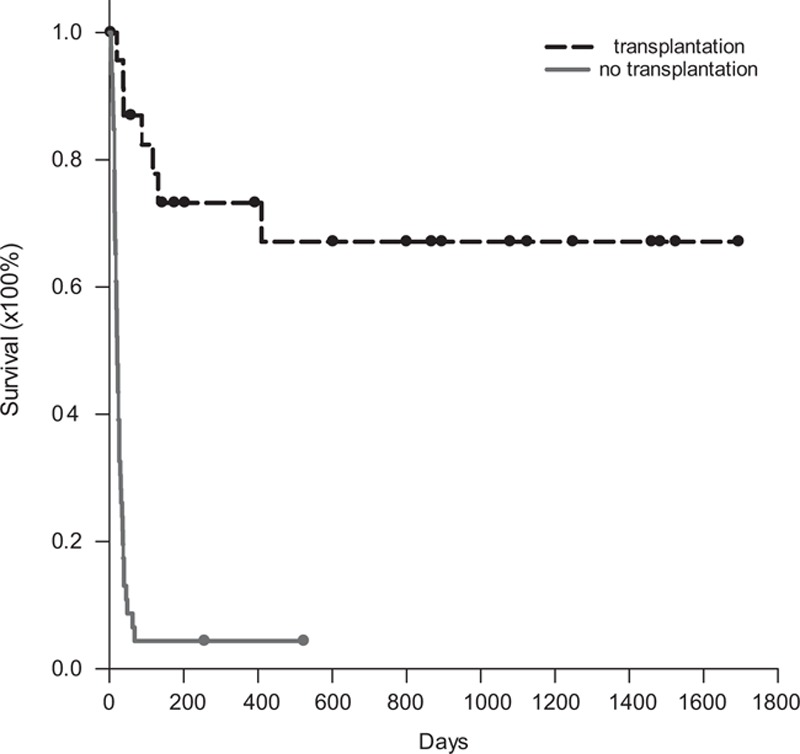
Survival rates for the patients meeting urgent transplant criteria. Seventy-one patients met criteria 1 and 2 and were listed for urgent liver transplantation. Finally, 24 patients (33.8%) were transplanted. The 1-, 2-, and 3-year survival rates were 73.2%, 67.1%, and 67.1%, respectively. For the 47 patients without liver transplantation, 1-, 2-, and 3-month survival rates were 28.3%, 8.7%, and 4.4%, respectively (P < 0.001).
FIGURE 3.
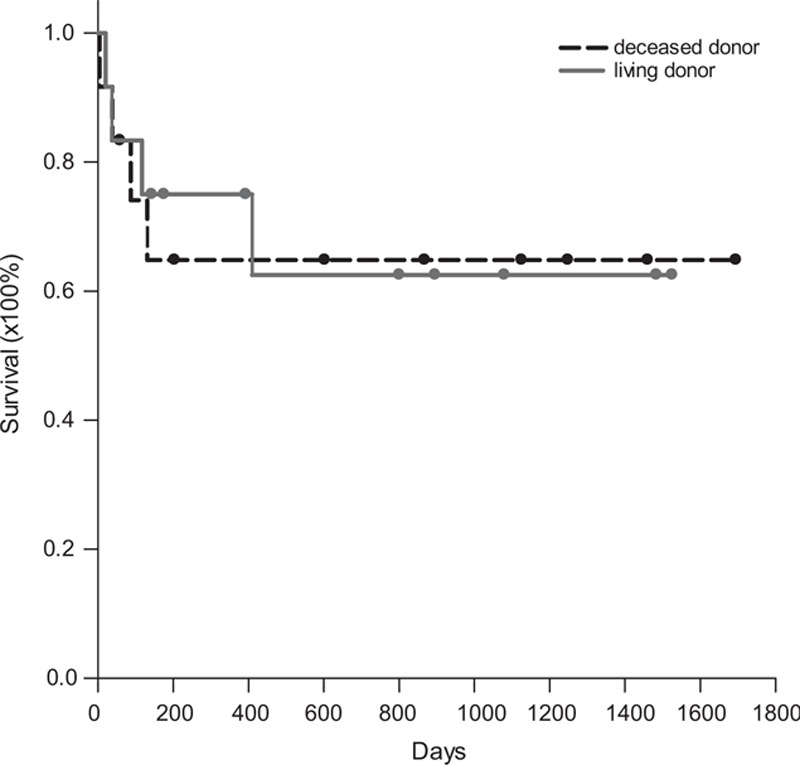
Survival rates of the patients with deceased or living donor liver transplantation. Among 24 patients having liver transplantation, 12 patients had deceased donor liver transplantation and the other 12 patients had living donor liver transplantation. The 1-, 2-, and 3-year survival rates were 64.8%, 64.8%, and 64.8%, respectively, for the patients with deceased liver transplantation and 75.0%, 62.5%, and 62.5%, respectively, for the patients with living donor liver transplantation (P = 0.938).
Life Span Without Liver Transplantation
Because clinical courses of the patient with acute HBV flare up and liver failure deteriorated quickly, liver transplantation must be performed in time to save the patients. We calculated the life span of the patients who did not have liver transplantation and died of liver failure. For the 15 patients who met criterion 1 and did not have transplantation, median (interquartile) survival time was 17 (13–24) days with a range from 4 to 36 days. The 1-, 2-, and 3-month survival rates were 20%, 0%, and 0%, respectively. For the 32 patients who met criterion 2 and did not have transplantation, median (interquartile) survival time was 23.5 (14.5–38.5) days with a range from 5 to 68 days for the 30 patients died of liver failure. The 1-, 2-, and 3-month survival rates were 31.3%, 12.5%, and 6.25%, respectively. For the patients who did not meet criteria 1 and 2, 4 patients died of liver failure. The median (range) life span was 70 (56–105) days for these 4 patients. The 1-, 2-, and 3-month survival rates were 91.7%, 83.3%, and 66.7%, respectively (P < 0.001, Figure 4).
FIGURE 4.
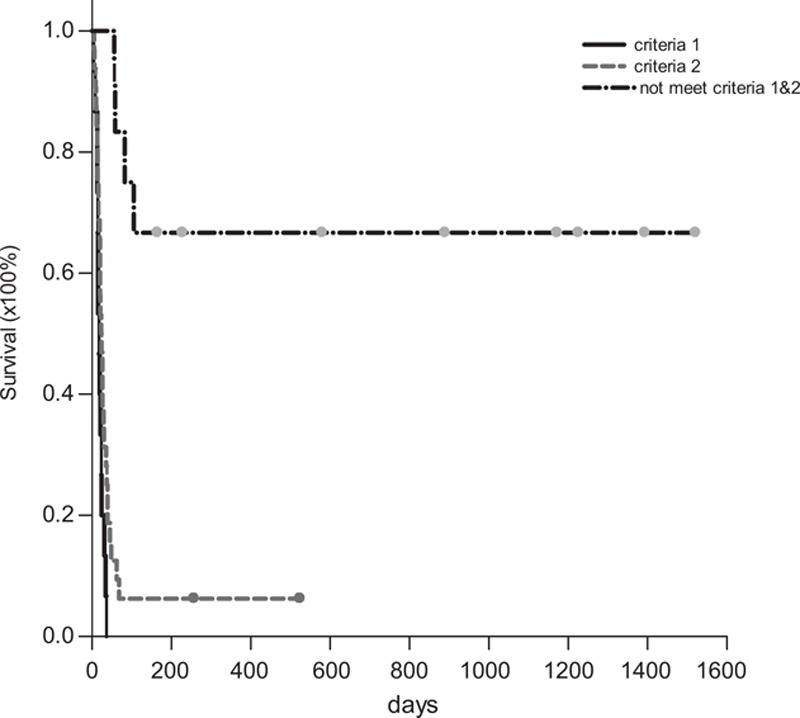
Life span and survival rates of the patients without liver transplantation. For 15 patients meeting criterion 1, median (interquartile) life span was 17 (13–24) d. For the 32 patients meeting criterion 2, median (interquartile) life span was 23.5 (14.5–38.5) d for the 30 patients died of liver failure and survival rate was 6.25%. For the 12 patients who did not meet criteria 1 and 2, the median (range) life span was 70 (56–105) d for the 4 patients died of liver failure and survival rate was 66.7% (P < 0.001).
Sensitivity and Specificity of MELD Score Criteria
To determine the validation of MELD score criteria of urgent liver transplantation for HBV patients with acute flare up and liver failure in noncirrhotic liver, the sensitivity and specificity in this series of patients were calculated. Among 83 patients, 71 patients met criterion 1 or 2, only 2 recovered with medical treatment without transplantation. For other 12 patients outside the criteria, all recovered from acute liver failure without urgent liver transplantation although 5 patients became cirrhosis in Child–Pugh C stage and listed for liver transplantation subsequently. Therefore, sensitivity was 100% and specificity was 85.7% for urgent liver transplantation in this study.
DISCUSSION
Acute liver failure is a critical condition with life threatening. Liver transplantation is the only effective treatment to save lives if the liver function is recognized irreversible. Therefore, when acute liver failure patients are encountered, 2 major concerns are raised. The first concern is whether the liver function can recover spontaneously, otherwise liver transplantation is needed. The other concern is when is the optimal time to carry out liver transplantation to avoid too sick to be transplanted if liver transplantation is indeed needed.5 In the literature, King's College criteria are a well-known reference to perform liver transplantation for acute liver failure.10 Based on the concept of King's College criteria, we began to assess the necessity of liver transplantation for HBV with acute flare up and liver failure in noncirrhotic patients if serum total bilirubin level ≥17.5 mg/dL. The indications of liver transplantation are according to MELD score criteria: MELD ≥ 35 or MELD < 35 with increased MELD in a subsequent week.9 In this study, we reevaluated the validation of MELD score criteria of liver transplantation in noncirrhotic HBV patients with acute flare up and liver failure.
MELD score criteria were valid to determine liver transplantation for noncirrhotic HBV patients with acute flare up and liver failure. In this study, the determination of urgent liver transplantation was according to MELD score criteria and yielded 100% of sensitivity and 87.5% of specificity. Acute flare up of HBV is the nature courses of HBV infection. Most of time, acute flare up of HBV will be subsided by antiviral agents and medical care. However, a small portion of the patients may encounter acute life failure and loss their lives in their 1st flare up. In Lai et al study using entecavir or lamivudine to treat HBV patients with acute-on-chronic liver failure, the mortality was >90% if MELD was >30 and mortality was 41% to 48% if MELD was 23 to 30.12 In acute liver failure, it is very difficult to decide the necessity of urgent liver transplantation according to the markedly elevated AST, ALT, bilirubin, or prolonged prothrombin time. Hepatic encephalopathy was a sign of liver failure, but it was not an independent factor to indicate liver transplantation when calculated with MELD score in our previous study.9 Therefore, we settled MELD score criteria to indicate urgent liver transplantation for noncirrhotic HBV patients with acute flare up and liver failure in our previous study. In this study, we prospectively followed up the clinical courses of the patients according to the MELD score criteria. The occurrence of hepatic encephalopathy was also recorded. The results proved that MELD score criteria were valid for HBV with acute flare up in noncirrhotic livers. Hepatic encephalopathy only occurred in 31 (43.7%) of 71 patients who needed urgent transplantation and could not be accurately employed as an indicator of liver transplantation.
The median survival time of HBV patients with acute flare up and liver failure was correlated to MELD score criteria if the patients did not receive liver transplantation. In this study, the results clearly showed that the median survival time was only 17 days if criterion 1 was met and 23.5 days if criterion 2 was met. This correlation between MELD score criteria and survival time helped us to be aware of how urgent the liver transplantation was needed. In the literature, several papers mentioned the determination of liver transplantation for acute liver failure. However, how urgent the liver transplantation was needed was not cleared showed.5,13,14 This study showed that how urgent of liver transplantation could be determined by MELD score criteria.
Partial liver graft liver transplantation achieved an accept graft and patient survival rates for acute liver failure in this study. It is well-known that the result of urgent liver transplantation for the patients with high MELD score is inferior to nonurgent liver transplantation.15–18 However, deceased liver grafts are always short in Taiwan. Even in urgent situation, liver allografts are not available. In this study, 12 patients had living donor liver transplantation. The graft and patient survival was almost the same as those of deceased whole liver transplantation, or even better in the 1st year. Park et al19 also reported that 1-year survival rate for the patients with urgent adult living donor liver transplantation was 85%. Therefore, partial graft or living donor liver transplantation for acute liver failure was indicated and could achieve acceptable results.
Closed following up of the HBV patient with acute flare up was essential even if the patients did not meet the criteria of urgent liver transplantation. In this study, 12 patients did not meet the criteria of urgent liver transplantation initially. However, 5 (41.7%) of them needed liver transplantation within 3 months after acute flare up of HBV. The MELD scores of these 5 patients hanged on high levels in the subsequent 1 to 2 months. For the other 7 patients, MELD scores dropped quickly within 1 month and the patients recovered fully. Therefore, even MELD score did not meet the criteria of urgent liver transplantation, subsequent MELD score calculation could distinguish the patients who needed liver transplantation and who could recover fully.
There were some limitations in this study. All these patients were managed by different hepatologists outsides this hospital before the patients were referred to liver transplant team for liver transplantation assessment. The incidence of the HBe Ag might be underestimated due to the timing of HBe Ag measurement. In the patients meeting criterion 1 with MELD score ≥35, the calculated median survival days might not exactly correct because some patients were referred for liver transplantation too late. However, it reflected the real world. The survival time still could be used as a reference for transplant teams to recognize how urgent the liver transplantation was.
In conclusion, acute flare up is common in the natural course of HBV in immune clearance phase. Most of the patients will recover spontaneously; however, some patients may have acute liver failure in their 1st experience and need liver transplantation. This study proved the validation that MELD score criteria could be employed to determine the necessity and urgency of liver transplantation for noncirrhotic HBV patients with acute flare up and liver failure.
Footnotes
Abbreviations: ALT = alanine aminotransferase, AST = aspartate aminotransferase, HBV = hepatitis B virus, MELD = model of end-stage liver disease.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Liaw Y-F, Chu C-M. Hepatitis B virus infection. Lancet 2009; 373:582–592. [DOI] [PubMed] [Google Scholar]
- 2.Mutimer DJ, Oo YH. Hepatitis B. Medicine 2011; 39:545–549. [Google Scholar]
- 3.Jayakumar S, Chowdhury R, Ye C, et al. Fulminant viral hepatitis. Crit Care Clin 2013; 29:677–697. [DOI] [PubMed] [Google Scholar]
- 4.Perrillo RP. Acute flares in chronic hepatitis B: the natural and unnatural history of an immunologically mediated liver disease. Gastroenterology 2001; 120:1009–1022. [DOI] [PubMed] [Google Scholar]
- 5.Tillmann HL, Patel K. Therapy of acute and fulminant hepatitis B. Intervirology 2014; 57:181–188. [DOI] [PubMed] [Google Scholar]
- 6.Chang ML, Liaw YF. Hepatitis B flares in chronic hepatitis B: pathogenesis, natural course, and management. J Hepatol 2014; 61:1407–1417. [DOI] [PubMed] [Google Scholar]
- 7.Seto WK, Lai CL, Yuen MF. Acute-on-chronic liver failure in chronic hepatitis B. J Gastroenterol Hepatol 2012; 27:662–669. [DOI] [PubMed] [Google Scholar]
- 8.Shiffman ML. Management of acute hepatitis B. Clin Liver Dis 2010; 14:75–91.viii–ix. [DOI] [PubMed] [Google Scholar]
- 9.Lee WC, Chou HS, Wu TJ, et al. Indicators and outcome of liver transplantation in acute liver decompensation after flares of hepatitis B. J Viral Hepat 2011; 18:193–199. [DOI] [PubMed] [Google Scholar]
- 10.O’Grady JG, Alexander GJM, Hayllar KM, et al. Early indicators of prognosis in fulminant hepatic failure. Gastroenterology 1989; 97:439–445. [DOI] [PubMed] [Google Scholar]
- 11.Urata K, Kawasaki S, Matsunami H, et al. Calculation of child and adult standard liver volume for liver transplantation. Hepatology 1995; 21:1317–1321. [PubMed] [Google Scholar]
- 12.Lai J, Yan Y, Mai L, et al. Short-term entecavir versus lamivudine therapy for HBeAg-negative patients with acute-on-chronic hepatitis B liver failure. Hepatob Pancreat Dis Int 2013; 12:154–159. [DOI] [PubMed] [Google Scholar]
- 13.Polson J, Lee WM. AASLD position paper: the management of acute liver failure. Hepatology 2005; 41:1179–1197. [DOI] [PubMed] [Google Scholar]
- 14.Bernal W, Hyyrylainen A, Gera A, et al. Lessons from look-back in acute liver failure? A single centre experience of 3300 patients. J Hepatol 2013; 59:74–80. [DOI] [PubMed] [Google Scholar]
- 15.Burra P, Freeman R. Trends in liver transplantation 2011. J Hepatol 2012; 56:S101–S111. [DOI] [PubMed] [Google Scholar]
- 16.Rana A, Hardy MA, Halazun KJ, et al. Survival outcomes following liver transplantation (SOFT) score: a novel method to predict patient survival following liver transplantation. Am J Transplant 2008; 8:2537–2546. [DOI] [PubMed] [Google Scholar]
- 17.Katoonizadeh A, Decaestecker J, Wilmer A, et al. MELD score to predict outcome in adult patients with non-acetaminophen-induced acute liver failure. Liver Int 2007; 27:329–334. [DOI] [PubMed] [Google Scholar]
- 18.Wong CS, Lee WC, Jenq CC, et al. Scoring short-term mortality after liver transplantation. Liver Transplant 2010; 16:138–146. [DOI] [PubMed] [Google Scholar]
- 19.Park SJ, Lim YS, Hwang S, et al. Emergency adult-to-adult living-donor liver transplantation for acute liver failure in a hepatitis B virus endemic area. Hepatology 2010; 51:903–911. [DOI] [PubMed] [Google Scholar]


