Abstract
Bereaved family members of cancer patient are at risk of having psychological problems such as anxiety and depression. However, prevalence and associated factors of anxiety and depressive symptoms among this population have not been explored in Korea.
We conducted a nation-wide cross-sectional questionnaire survey of 3522 bereaved family members of cancer patients who died at 44 hospice palliative care unit (HPCU) in Korea in 2012. The questionnaire comprised the Hospital Anxiety and Depression Scale (HADS) and Good Death Inventory (GDI). Deceased patient's age, sex, primary site of cancer, duration of stay at HPCU, awareness of terminal status, bereaved family member's age, sex, and relation to the deceased were collected from Korean Terminal Cancer Patients Information System.
1121 returned questionnaires were analyzed (response rate, 31.8%). Using a cut-off value of 8 for HADS subscale, the prevalence of anxiety and depressive symptoms was 48.0% and 57.6%, respectively. Mean scores for HADS-A and HADS-D were 7.88 ± 4.87 and 8.91 ± 4.82, respectively. Among the bereaved, older age, being a spouse to the deceased, family members of younger patient, and negative score for a few GDI items were significantly associated with an increased risk of having anxiety or depressive symptoms in the multivariate logistic analysis.
In conclusion, we noted the high prevalence of anxiety and depressive symptoms among the bereaved of cancer patients and identified associated factors for these psychological morbidities. Systematic efforts are needed to improve the mental health of the bereaved family members of cancer patients.
INTRODUCTION
Life is never quite the same after losing a loved one. Bereavement happens to almost everyone and can affect one's life deeply. Previous studies have shown that bereaved family members are at an increased risk of mortality and developing new illness or worsening of preexisting disease, compared to nonbereaved counterparts.1 In additional to physical ailments, the bereaved may experience a variety of psychiatric problems, such as anxiety and depression. Although most cases are clinically insignificant, some bereaved family members show serious psychiatric symptoms: reportedly, about 10% to 20% of bereaved individuals exhibit clinical levels of depression, and bereaved parents show an increased prevalence of posttraumatic stress disorder.1
A few factors have been found to be related with psychological states among the bereaved. First, mental health status before a death has been shown to be associated with developing anxiety and depression at 3 to 6 months after the loss.2–4 As well, the circumstances under which deaths occur have also been found to affect psychological adjustment in the bereaved: violentness of the death, family's preparedness for the death, and an unexpected death were shown to be predictive of depression among the bereaved,5,6 Active family coping during caregiving has also been reported to negatively affect mental health outcomes.3 Lastly, a perceived lack of support and lower level of sense of control were also shown to be predictive of having depressive symptoms among the widowed.7
Can quality of end-of-life (EOL) care for the patient influence health status of the bereaved? A few studies have looked into the relationship between EOL care quality and health outcomes in bereaved family members. Christakis and Iwashyna8 found that the mortality of widows whose deceased husbands received hospice care was lower than that of those whose husbands did not seek hospice care, which suggests that EOL care may affect health outcomes among bereaved families. Carr reported that pain suffered by the deceased before their death was positively associated with loss-related anxiety of the spouse.9 Staying less than 3 days in hospice10 and receiving aggressive medical care at the end of life11 have also been shown to increase the risk of major depression among bereaved caregivers. However, Kapari et al3 discovered no significant relationship between a “good death,” as rated by hospital staff, and common mental disorders in bereaved family members.
Since 2005, the Ministry of Health & Welfare for Korea has promoted hospice palliative care by providing subsidies to designated hospice palliative care units (HPCUs). However, this program has been largely focused on the care of the patient while attention for the bereaved family has been relatively insufficient. In this study, we aimed to investigate the prevalence and associated factors of psychological symptoms (anxiety and depression) among bereaved family members of cancer patients who utilized these designated HPCU across Korea.
METHODS
Subjects
We conducted a cross-sectional questionnaire survey of family caregivers of terminal cancer patients who were admitted and passed away at the 44 designated HPCUs during the year 2012. This study was carried out as part of an initiative to evaluate the quality of EOL care offered at designated HPCUs across Korea. This survey was performed from July 2012 to March 2013. This study was approved by the Institutional Review Board of the National Cancer Center, Korea.
The inclusion criteria for participating in the questionnaire survey were as follows: the patient and their family caregivers gave consent to register personal information with the Korean Terminal Cancer Patient Information System (KTCPIS); patient passed away 2 to 6 months before the survey; the patient stayed in the designated HPCU for 72 hours or longer; and the family caregiver was 18-years-old or older. Family caregivers were deemed ineligible for the survey if the patient stayed less than 72 hours in the HPCU as the family caregiver's experience could have been too limited to rate the quality of service. Lastly, family caregivers were excluded from the survey if the patient moved to other facilities.
Eligible family members were telephoned and given a description of the purpose of the survey. Those who agreed to participate were sent a questionnaire by mail, along with a consent form and a return envelope. Questionnaires were to be returned to the secretariat office (Hospice & Palliative Care Branch) of the National Cancer Center, Korea.
A total of 6726 patients were admitted to 1 of 44 designated HPCUs during 2012. Among these, 5644 patients were confirmed as having died at the start of the survey period. After applying inclusion and exclusion criteria, 4465 cases were contacted via telephone, and 943 refused to participate in the survey. Finally, 3522 cases were deemed eligible and surveys were mailed out, and 1121 returned questionnaires were included in the final analysis (response rate of 31.8%).
Data Collection
General characteristics of patient (age, sex, primary site of cancer, marital status, religion, awareness of terminal condition, and duration of admission at HPCU) and family caregiver (age, sex, and relation to the patient) were extracted from KTCPIS. Since 2009, the Ministry of Health and Welfare has required designated HPCUs to submit patient and family data to the KTCPIS via a web-based information system (eVelos System, Velos, Inc., Fremont, CA) for the purpose of policy development. When a patient is admitted to a designated HPCU, the patient and their family members are introduced to the KTCPIS, and personal information is archived in the KTCPIS for those who give consent. Details on the KTCPIS have been explained previously.12
Questionnaire for Anxiety, Depression, and Quality of Death
Symptoms of anxiety and depression among the family caregivers were assessed with the Hospital Anxiety and Depression Scale (HADS). The HADS questionnaire is a self-reporting measurement tool designed for use in medical settings to assess anxiety and depression.13 The scale consists of 14 items and 2 subscales: seven items for anxiety (HADS-A) and 7 for depression (HADS-D). Each subscale is scored from 0 to 21, with higher scores indicating greater distress (0–7: normal, 8–10: mild disorder, 11–14: moderate disorder, and 15–21: severe disorder). This instrument has been validated in the Korean population and demonstrated a sensitivity of 89.2% and specificity of 82.5% when a cut-off level of 8 was used for each subscale.14
Bereaved family members were also invited to rate the quality of death of the deceased using the Korean short version of Good Death Inventory (GDI). The GDI was developed in Japan by Miyashita et al15 and was modified and validated in Korean in 2009.16 The GDI comprises 18 items on comprehensive EOL care outcomes, including constructs and processes of service delivery, physical, psychoexistential, relationships, and dignity domains, all measured on a 7-point Likert scale. Higher scores for each GDI item are interpreted as better EOL care outcomes. The GDI was shown to have sufficient concurrent validity with the Care Evaluation Scale and patient EOL quality.15,16
Statistical Analysis
General characteristics of the family caregivers between those who returned the questionnaire and who did not were compared using Student t test for continuous variables and Chi-square test for categorical variables. General characteristics of the bereaved family caregivers and the deceased were summarized as means and percentages. Scores for the HADS-A and HADS-D were classified according to severity (normal, mild, moderate, severe) and presented as mean values and percentages. Score of 8 or above for HADS-A and HADS-D subscale was used to define cases with anxiety and depressive symptoms, respectively. We performed univariate logistic regression analysis to calculate odds ratios (OR) for having anxiety or depressive symptoms according to the general characteristics of bereaved family members (age, sex, relation to the patient), deceased (age, sex, primary site of cancer, marital status, religion, awareness of terminal condition, duration of admission at HPCU) and GDI scores. For the factors identified as significantly associated with the risk of having anxiety and depressive symptoms in the univariate analysis (P < 0.05), stepwise logistic regression using backward elimination was performed adjusted with age and sex of both bereaved family caregiver and deceased. All analyses were performed using SAS version 9.3 statistical software package (SAS Institute, Cary, NC).
RESULTS
General Characteristics of Participants and Prevalence of Anxiety and Depression
Age, sex, and relationship to the deceased were compared between respondents (n = 1121) and nonrespondents (who declined to participate or did not return the questionnaire, n = 3344). In respondent group, the proportion of female caregiver (60.8% vs 64.9%, P = 0.012) and spouse of the deceased (36.5% vs 42.0%, P < 0.001) was lower than in the nonrespondent group.
The mean duration between the date of patient's death and mailing the questionnaire was 126.5 ± 37.9 days (median 124, ranges from 57 to 211 days) among respondents. The proportion of family caregivers who experienced bereavement 3 months or longer from the point of survey was 81.1%.
General characteristics of family caregiver and deceased and the HADS score of the family caregivers are described in Table 1. The mean age of family caregiver was 50.9 ± 11.5, and 60.2% of them were female. Spouse of the deceased comprised more than a third of the respondents (36.5%).
TABLE 1.
Characteristics of Participants and Prevalence of Anxiety∗ and Depression†
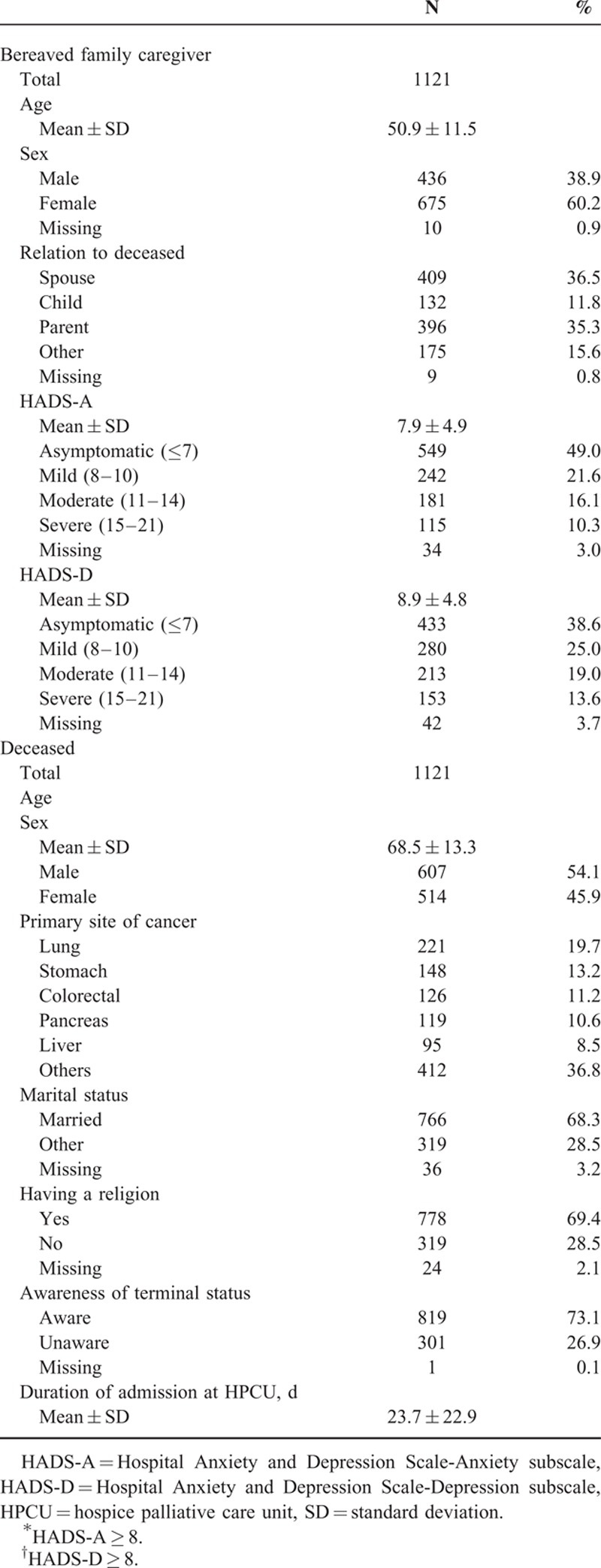
Symptoms of anxiety were present in almost half of the participants (48.0%), and the mean score for the HADS-A was 7.9 ± 4.9. 10.3% of the participants exhibited a severe level of anxiety. Depressive symptoms were observed in 57.6% of the respondents, and 13.6% showed a severe level thereof, with a mean score on the HADS-D of 8.9 ± 4.8.
42.7% of respondent showed both HADS-A and HADS-B as 8 or higher.
The mean age of deceased was 68.5 ± 13.3, and 54.1% thereof were male. The most common primary site of cancer was lung (19.7%). Majority of the deceased was married (68.3%). At the time of admission to the HPCU, 26.9% of the deceased were unaware of their terminal status. The mean duration of stay at the HPCU was 23.7 ± 22.9 days.
Risk of Having Anxiety and Depressive Symptoms According to General Characteristics of Family Caregiver and Deceased
Table 2 presents the result of univariate logistic analysis for having anxiety and depressive symptoms according to the general characteristics of family caregiver and deceased.
TABLE 2.
Risk of Having Anxiety and Depression According to Characteristics of Bereaved Family Caregiver and Deceased
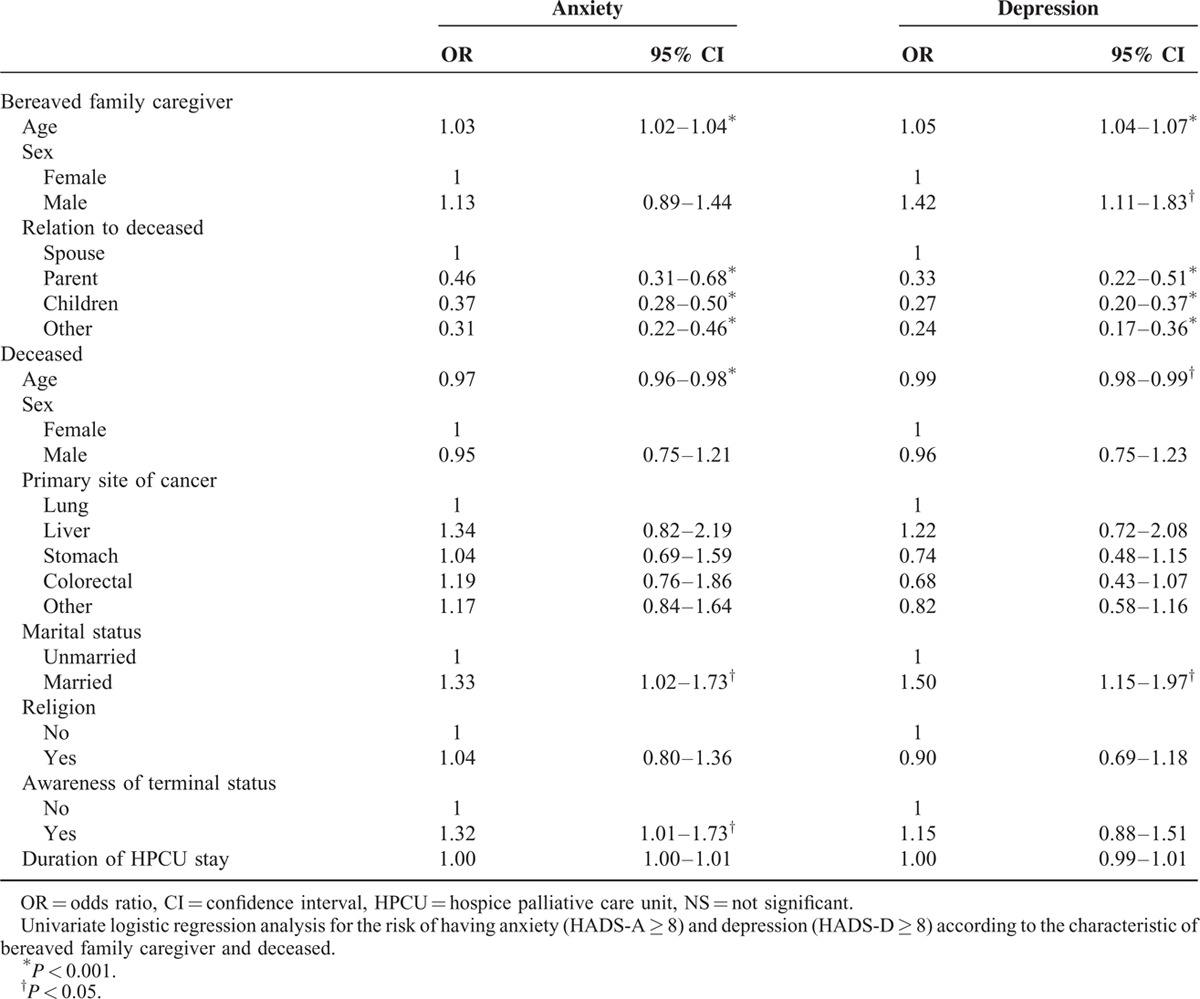
Using a cut-off value of 8 for HADS subscales, family caregiver's being aged and a spouse to the deceased, deceased's being younger and married were significantly related with having both anxiety and depressive symptoms among respondents. Male sex of the family caregiver was associated with and increased risk of having depressive symptoms (OR 1.42, 95% CI = 1.11–1.83), while the deceased's awareness of the terminal status was significantly associated with risk of having anxiety symptoms (OR 1.32, 95% CI = 1.01–1.73) among family caregivers.
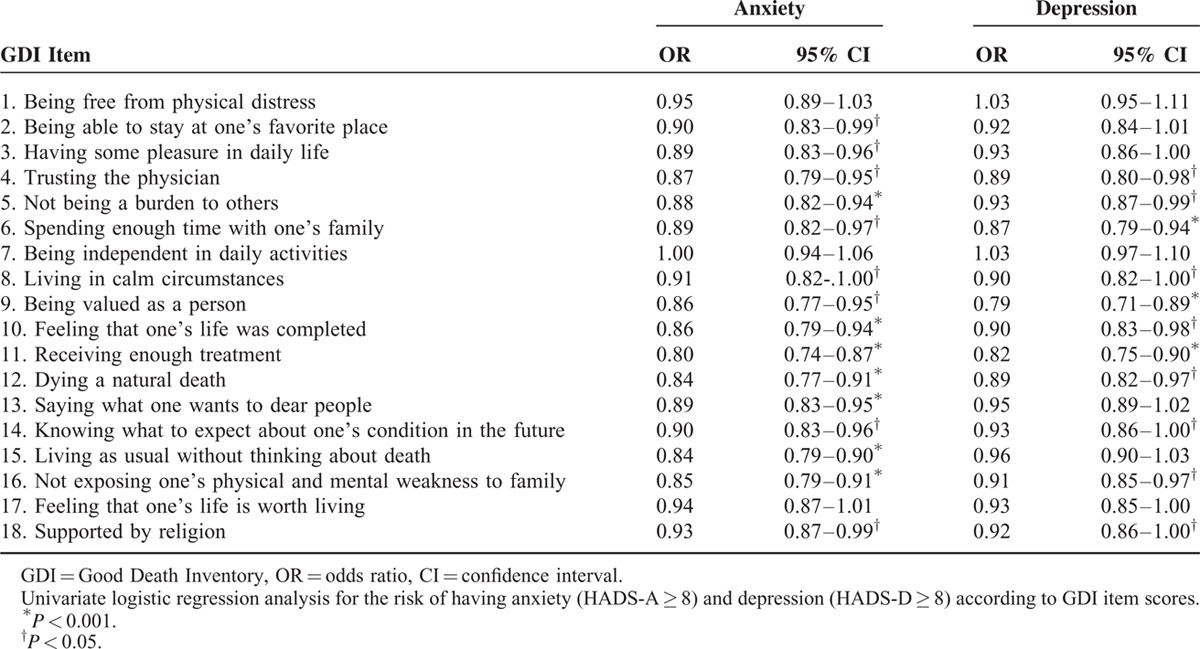
Risk of Having Anxiety or Depressive Symptoms According to Quality of Death Measured With GDI
Table 3 shows the risks of having anxiety or depressive symptoms according to GDI score. For all 18 items, higher GDI scores were related to a lower risk of having anxiety symptoms, and this association was significant in 15 items. Higher GDI scores were also found to be related with a lower risk of having depressive symptoms in 16 items, and the association was significant for 11 items.
TABLE 3.
Risk of Having Anxiety and Depression According to Quality of Death Measured With Good Death Inventory
Factors Associated With Having Anxiety and Depressive Symptoms Among Bereaved Family Caregiver
Table 4 summarizes the result of multivariate logistic analysis for the risk of having anxiety and depressive symptoms. Older age and being spouse to the deceased of family caregiver were significantly associated with having both anxiety and depressive symptoms. Younger age of the deceased was positively associated with increased risk of having anxiety symptoms among family caregivers.
TABLE 4.
Factors Associated With Risk of Having Anxiety and Depression Among Bereaved Family Caregiver
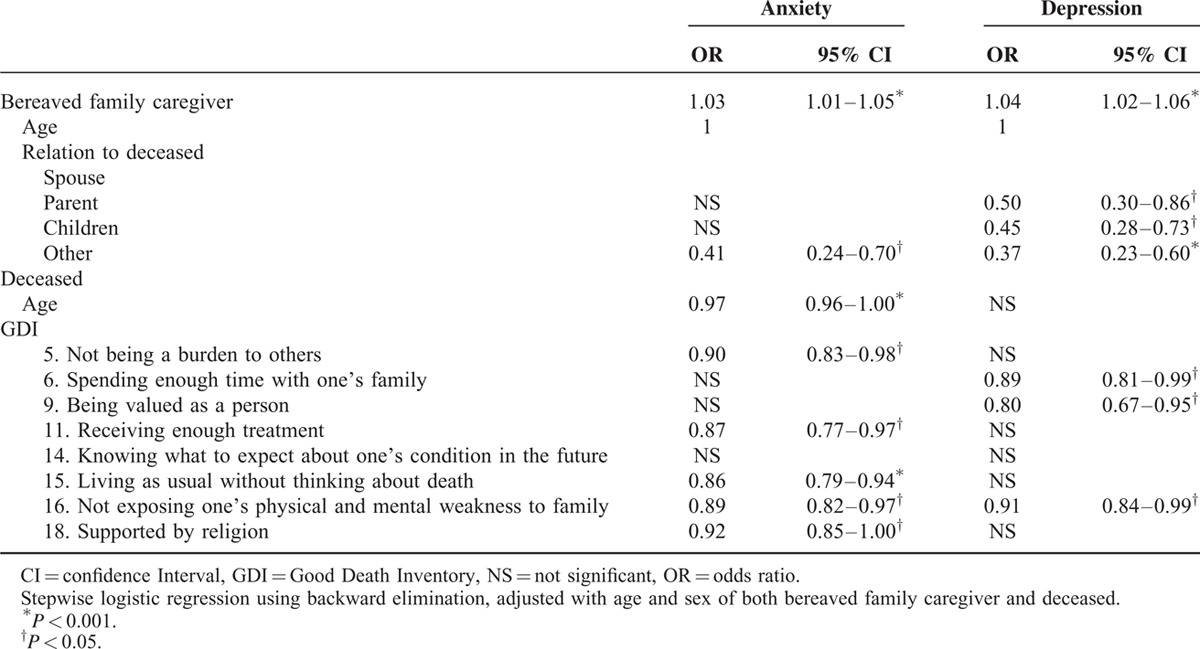
Among GDI items, lower scores for the 5 items of “Not being a burden to others” (OR = 0.90, 95% CI = 0.83–0.98), “Receiving enough treatment” (OR = 0.87, 95% CI = 0.77–0.97), “Living as usual without thinking about death” (OR = 0.86, 95% CI = 0.79–0.94), “Not exposing one's physical and mental weakness to family” (OR = 0.89, 95% CI = 0.82–0.97) and “Supported by religion” (OR = 0.92, 95% CI = 0.85–1.00) were significantly associated with a higher risk of having anxiety symptoms. Meanwhile, lower scores for 3 items of “Spending enough time with one's family” (OR = 0.89, 95% CI = 0.81–0.99), “Being valued as a person” (OR = 0.80, 95% CI = 0.67–0.95), and “Not exposing one's physical and mental weakness to family” (OR = 0.91, 95% CI = 0.84–0.99) were significantly associated with increased risk of having depressive symptoms.
DISCUSSION
To our knowledge, this is the first study to evaluate prevalence and associated factors of anxiety and depressive symptoms among bereaved family members in Korea using national representative population. In the present study, we noted relatively high prevalence of anxiety (48.0%) and depressive symptoms (57.6%) among family caregivers during 2 to 6 months after bereavement. Family caregiver's age, being a spouse to the deceased, and younger age of the deceased were associated with increased risk of having anxiety or depression. As well, negative ratings for a few quality of death items showed significant relationship with higher risk of having anxiety or depressive symptoms.
Previous research reported that 25% to 45% of bereaved people have mild level of depressive symptoms while 10% to 20% exhibit clinical level of symptoms,1 which is comparable to our finding in this study. In addition, the high prevalence of depression and anxiety in our result could be explained by that the survey was done 2 to 6 months after the bereavement. In general, psychological reaction to bereavement is most intense at early bereavement period and decreases over time.1,17,18 In a systematic review, it was suggested that major depressive disorder or anxiety disorders in the widowhood were more prevalent in the first year after the bereavement.19
In the present study, older age of bereaved family caregiver was associated with a higher risk of having anxiety and depressive symptoms. This is in line with a previous study20,21 which showed older age contributes to increased psychological distress during the bereavement period. However, Onrust et al7 suggested that younger widowed individual is more prone to depression among bereaved spouses with aged 55 and older. Meanwhile, it was reported that younger age of caregiver was associated with worse psychosocial outcome at the phase of before loss.22 Thus, the age of caregiver might influence psychological adaptation differently on caregiving and bereavement phase.
It is not surprising that being a spouse and younger age of the deceased were associated with increased risk of depression and anxiety in the present study, which was also revealed in previous study.4 Interestingly, physical distress of the deceased, which was assessed with GDI, was not significantly related with risk of depression and anxiety in the multivariate analysis in our study. This finding contrasts with other studies9,23 which suggested association between physical distress of the deceased and mental health of the bereaved.
Additionally, in the present study, several GDI items including “Not being a burden to others,” “Receiving enough treatment,” “Living as usual without thinking about death,” “Not exposing one's physical and mental weakness to family,” “Supported by religion,” “Spending enough time with one's family,” “Being valued as a person,” and “Knowing what to expect about one's condition in the future” were found to be significantly related with having anxiety or depressive symptoms among bereaved family members. It is noteworthy that these items reflect psychoexistential issues, family relationship, and decision-making domains,15 which mainly focus on psychosocial distress of patient rather than on physical distress or care environment. Specifically, feeling of “Being a burden” among patients with terminal illness was found to be linked with the risk of having adjustment disorder,24 major depression,24 wish to hasten death25 and even committing suicide26 of patients. Patient's emotional distress perceived by family caregiver before death may have influenced the level of anxiety and depression of family caregivers both before death and during bereavement period. A positive relationship between psychological distress of cancer patients and their caregivers was noted in a meta-analysis.27 It was also reported that bereaved widowers have an increased risk of having sleep disorder with anxiety if their spouse had suffered from anxiety during last month.23
Previous studies suggested that quality of EOL influences the psychological adjustment of the bereaved.9–11 Hospice care aims to promote quality EOL care for patients, as well as their family, by providing whole person care. As Christakis suggested, the consequences of care for the patient do not end with the patient's death, rather they continue to affect the health of bereaved family members.8 In this context, care for bereaved families begins not after but before their relative's death.
On the other hand, bereaved family members who may be dealing with anxiety or depression may allocate lower scores for EOL care quality as a reflection of their mental status. Although reports from bereaved family members are often utilized for the monitoring of service quality at hospice units,28,29 recall of the patient's death may change according to their stages of grief.30 Accordingly, a previous study demonstrated that the concordance of proxy reports from the family with reports from the patient tended to be lower after the patient died than while they were living.31 Thus, as the emotional status of the bereaved may distort their recollections of their relative's death,32 bereaved family members coping with anxiety or depression may have responded in the present study with more negative attitudes on the quality of care offered to their relative during their passing.30
These findings from present study highlight areas that warrant development for better EOL care. First, greater attention for reducing anxiety and depression among family caregivers is needed before their relative passes, not only after. Previous studies have shown that baseline statuses of anxiety and depression are significant predictors of the psychological state of bereaved family members after their loss.2,3 According to a previous report, the prevalence of anxiety and depression during the caregiving period ranges from 20% to 40% and 20% to 73%, respectively.33 In a Korean population, Park reported that about 38% of caregivers of cancer patients had anxiety and 82% had depression upon measurement with HADS.34 Nonetheless, screening, diagnosis, and treatment for anxiety and depression in family caregivers have been neglected in both palliative care practice and policies.
Secondly, the quality of EOL care should be improved not only for greater quality of life for patients but also for the psychological state of their families. In Korea, the Ministry of Health & Welfare employs a set of standards for grading the performance of designated HPCUs. These standards dictate the presence of essential facilities, such as a family lounge and patient bathrooms, an adequate ratio of nurses and physicians per patient, fulfillment of a minimum of 60 hours of education for hospice palliative team members, and service evaluation from bereaved families using the GDI and Care Evaluation Scale. However, these indicators are minimum requirements, and assessment of service quality heavily depends on subjective reporting from the bereaved family. Accordingly, we stress that there is an indispensable need to improve the monitoring of service performance with more objective components, with which to better assess and address areas of weakness in hospice palliative care services in Korea.
Our study is subject to a few limitations. First, the response rate for the survey was only about 32%, and the proportion of spouse was lower in the participants than in the nonparticipants. Considering that being a spouse was associated with an increased risk of having depressive or anxiety symptoms, the actual prevalence of these symptoms among bereaved family caregivers could be higher than that of our finding. In addition, family caregivers of patients who passed away within 72 hours after admission to the HPCU were excluded from the survey. Therefore, caution is needed on interpreting the result of our study. Second, the baseline status of anxiety and depression of participant before loss was not available, and anxiety and depressive symptoms were assessed only with HADS. For clinical diagnosis of anxiety and depression, one needs to be assessed by mental health professional with clinical interview. In particular, diagnosing major depression in bereavement period requires to consider the individual history and cultural background,35 which cannot be assessed with HADS alone. Therefore, the notion of depressive or anxiety symptoms in our study should be distinguished from clinical disorder. Lastly, only limited variables regarding the deceased and the family members were included in the analysis.
Nevertheless, our study has strength in that the results were drawn from a large number of participants across 44 HPCU institutions across Korea. In addition, standardized measurement tools such as HADS and GDI were used to assess psychological symptoms and quality of death among the participants. The findings from our study could be utilized as a starting point for further research, policy development, and improving clinical care for the mental health of the bereaved.
CONCLUSIONS
In Korea, the policy on hospice palliative care was more focused on to the care offered to dying patients, while the psychological state of family caregivers has been relatively neglected. Systematic efforts are needed to improve EOL care as a benefit to both patients and their bereaved family members; such efforts must include the development of policies for appropriate quality control of EOL care services. To do so, further research is needed to identify elements affecting the psychological well-being of family caregivers and bereaved family members.
Acknowledgment
The authors would like to thank Anthony Thomas Milliken, ELS (Editing Synthase, Seoul, Korea) for his help with the editing of this manuscript.
Footnotes
Abbreviations: EOL = end of life, GDI = Good Death Inventory, HADS = Hospital Anxiety and Depression Scale, HADS-A = Hospital Anxiety and Depression Scale for Anxiety, HADS-D = Hospital Anxiety and Depression Scale for Depression, HPCUs = hospice palliative care units, KTCPIS = Korean Terminal Cancer Patient Information System.
This work was supported by Grant No. 1310242-3 from the National Cancer Center, Korea.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Stroebe M, Schut H, Stroebe W. Health outcomes of bereavement. Lancet 2007; 370:1960–1973. [DOI] [PubMed] [Google Scholar]
- 2.Garrido MM, Prigerson HG. The end-of-life experience: modifiable predictors of caregivers’ bereavement adjustment. Cancer 2014; 120:918–925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kapari M, Addington-Hall J, Hotopf M. Risk factors for common mental disorder in caregiving and bereavement. J Pain Symptom Manage 2010; 40:844–856. [DOI] [PubMed] [Google Scholar]
- 4.Ling SF, Chen ML, Li CY, et al. Trajectory and influencing factors of depressive symptoms in family caregivers before and after the death of terminally ill patients with cancer. Oncol Nurs Forum 2013; 40:E32–E40. [DOI] [PubMed] [Google Scholar]
- 5.Barry LC, Kasl SV, Prigerson HG. Psychiatric disorders among bereaved persons: the role of perceived circumstances of death and preparedness for death. Am J Geriatr Psychiatry 2002; 10:447–457. [PubMed] [Google Scholar]
- 6.Burton A, Haley W, Small B. Bereavement after caregiving or unexpected death: effects on elderly spouses. Aging Mental Health 2006; 10:319–326. [DOI] [PubMed] [Google Scholar]
- 7.Onrust S, Cuijpers P, Smit F, et al. Predictors of psychological adjustment after bereavement. Int Psychogeriat 2007; 19:921–934. [DOI] [PubMed] [Google Scholar]
- 8.Christakis NA, Iwashyna TJ. The health impact of health care on families: a matched cohort study of hospice use by decedents and mortality outcomes in surviving, widowed spouses. Soc Sci Med 2003; 57:465–475. [DOI] [PubMed] [Google Scholar]
- 9.Carr D. A “good death” for whom? Quality of spouse's death and psychological distress among older widowed persons. J Health Soc Behav 2003; 44:215–232. [PubMed] [Google Scholar]
- 10.Bradley EH, Prigerson H, Carlson MD, et al. Depression among surviving caregivers: does length of hospice enrollment matter? Am J Psychiatry 2004; 161:2257–2262. [DOI] [PubMed] [Google Scholar]
- 11.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. J Am Med Assoc 2008; 300:1665–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baek YJ, Shin DW, Choi JY, et al. Late referral to palliative care services in Korea. J Pain Symptom Manage 2011; 41:692–699. [DOI] [PubMed] [Google Scholar]
- 13.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67:361–370. [DOI] [PubMed] [Google Scholar]
- 14.Oh SM, Min KJ, Park DB. A study on the standardization of the hospital anxiety and depression scale for Koreans: a comparison of normal, depressed and anxious groups. J Korean Neuropsychiatr Assoc 1999; 38:289–296. [Google Scholar]
- 15.Miyashita M, Morita T, Sato K, et al. Good death inventory: a measure for evaluating good death from the bereaved family member's perspective. J Pain Symptom Manage 2008; 35:486–498. [DOI] [PubMed] [Google Scholar]
- 16.Shin DW, Choi J, Miyashita M, et al. Measuring comprehensive outcomes in palliative care: validation of the Korean version of the Good Death Inventory. J Pain Symptom Manage 2011; 42:632–642. [DOI] [PubMed] [Google Scholar]
- 17.Ringdal GI, Jordh⊘y MS, Ringdal K, et al. The first year of grief and bereavement in close family members to individuals who have died of cancer. Palliat Med 2001; 15:91–105. [DOI] [PubMed] [Google Scholar]
- 18.Taylor DH, Jr, Kuchibhatla M, Ostbye T, et al. The effect of spousal caregiving and bereavement on depressive symptoms. Aging Ment Health 2008; 12:100–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Onrust S, Cuijpers P. Mood and anxiety disorders in widowhood: a systematic review. Aging Mental Health 2006; 10:327–334. [DOI] [PubMed] [Google Scholar]
- 20.Ringdal GI, Jordh⊘y MS, Ringdal K, et al. Factors affecting grief reactions in close family members to individuals who have died of cancer. J Pain Symptom Manage 2001; 22:1016–1026. [DOI] [PubMed] [Google Scholar]
- 21.Gilbar O, Ben-Zur H. Bereavement of spouse caregivers of cancer patients. Am J Orthopsychiatry 2002; 72:422–432. [DOI] [PubMed] [Google Scholar]
- 22.Williams A-L, McCorkle R. Cancer family caregivers during the palliative, hospice, and bereavement phases: a review of the descriptive psychosocial literature. Palliat Support Care 2011; 9:315–325. [DOI] [PubMed] [Google Scholar]
- 23.Jonasson JM, Hauksdóttir A, Valdimarsdóttir U, et al. Unrelieved symptoms of female cancer patients during their last months of life and long-term psychological morbidity in their widowers: a nationwide population-based study. Eur J Cancer 2009; 45:1839–1845. [DOI] [PubMed] [Google Scholar]
- 24.Akechi T, Okuyama T, Sugawara Y, et al. Major depression, adjustment disorders, and post-traumatic stress disorder in terminally ill cancer patients: associated and predictive factors. J Clin Oncol 2004; 22:1957–1965. [DOI] [PubMed] [Google Scholar]
- 25.Kelly B, Burnett P, Pelusi D, et al. Factors associated with the wish to hasten death: a study of patients with terminal illness. Psychol Med 2003; 33:75–81. [DOI] [PubMed] [Google Scholar]
- 26.Filiberti A, Ripamonti C, Totis A, et al. Characteristics of terminal cancer patients who committed suicide during a home palliative care program. J Pain Symptom Manage 2001; 22:544–553. [DOI] [PubMed] [Google Scholar]
- 27.Hodges L, Humphris G, Macfarlane G. A meta-analytic investigation of the relationship between the psychological distress of cancer patients and their carers. Soc Sci Med 2005; 60:1–12. [DOI] [PubMed] [Google Scholar]
- 28.Morita T, Hirai K, Sakaguchi Y, et al. Measuring the quality of structure and process in end-of-life care from the bereaved family perspective. J Pain Symptom Manage 2004; 27:492–501. [DOI] [PubMed] [Google Scholar]
- 29.Connor SR, Teno J, Spence C, et al. Family evaluation of hospice care: results from voluntary submission of data via website. J Pain Symptom Manage 2005; 30:9–17. [DOI] [PubMed] [Google Scholar]
- 30.Teno JM. Measuring end-of-life care outcomes retrospectively. J Palliat Med 2005; 8 (Suppl. 1):s-42–s-49. [DOI] [PubMed] [Google Scholar]
- 31.Hinton J. How reliable are relatives’ retrospective reports of terminal illness? Patients’ and relatives’ accounts compared. Soc Sci Med 1996; 43:1229–1236. [DOI] [PubMed] [Google Scholar]
- 32.Addington-Hall J, McPherson C. After-death interviews with surrogates/bereaved family members: some issues of validity. J Pain Symptom Manage 2001; 22:784–790. [DOI] [PubMed] [Google Scholar]
- 33.Fletcher BAS, Dodd MJ, Schumacher KL, et al. Symptom experience of family caregivers of patients with cancer. Oncol Nurs Forum 2008; 35:E23–E44. [DOI] [PubMed] [Google Scholar]
- 34.Park B, Kim SY, Shin J-Y, et al. Prevalence and predictors of anxiety and depression among family caregivers of cancer patients: a nationwide survey of patient–family caregiver dyads in Korea. Support Care Cancer 2013; 21:2799–2807. [DOI] [PubMed] [Google Scholar]
- 35.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Washington, DC: American Psychiatric Association; 2013. [Google Scholar]


