Abstract
Clients of female sex workers (CFSWs) are a bridge population for the spread of HIV and syphilis to low or average risk heterosexuals. Most studies have examined the point prevalence of these infections in CFSWs. Limited evidence suggests that older age CFSWs are at a higher risk of acquiring sexually transmitted diseases compared with younger clients. Thus, we sought to describe long-term trends in HIV, syphilis, and hepatitis C (HCV) to better understand how these infections differ by sex worker classification and client age. We also examined trends in HIV, syphilis, and HCV among categories of female sex workers (FSWs).
We conducted serial cross-sectional studies from 2010 to 2015 in Guangxi autonomous region, China. We collected demographic and behavior variables. FSWs and their clients were tested for HIV, syphilis, and HCV antibodies. Positive HIV and syphilis serologies were confirmed by Western blot and rapid plasma regain, respectively. Clients were categorized as middle age (40–49 years) and older clients (≥50 years). FSWs were categorized as high-tier, middle-tier, or low-tier based on the payment amount charged for sex and their work venue. Chi-square test for trends was used for testing changes in prevalence over time.
By 2015, low-tier FSWs (LTFSWs) accounted for almost half of all FSWs; and they had the highest HIV prevalence at 1.4%. HIV prevalence declined significantly for FSWs (high-tier FSW, P = 0.003; middle-tier FSWs; P = 0.021; LTFSWs, P < 0.001). Syphilis infections significantly declined for FSWs (P < 0.001) but only to 7.3% for LTFSWs. HCV and intravenous drug use were uncommon in FSWs. HIV prevalence increased for older age clients (1.3%–2.0%, P = 0.159) while syphilis prevalence remained stable. HCV infections were halved among older clients in 3 years (1.7%–0.8%, P < 0.001). Condom use during the last sexual encounter increased for FSWs and CFSWs. Few clients reported sex with men or intravenous drug use. Clients preferred LTFSWs, especially older clients (81.9%).
Our results suggest that HIV and syphilis infections are increasing in older clients who prefer LTFSWs. HIV and syphilis are likely increasing in Guangxi Province through heterosexual transmission.
INTRODUCTION
In 2014, heterosexual transmission contributing to 66.4% of HIV cases.1 Female sex workers (FSWs) are a key bridging population for the spread of HIV to the heterosexual population through their clients.2 Trends point to a decline in the national prevalence of HIV, syphilis, and HCV among FSWs, which is likely driven by their increased use of preventive services and consistent condom use.3,4 The burden of STDs, however, has declined unevenly among FSWs: a meta-analysis estimated the pooled prevalence of HIV in high, middle, and low-tier FSWs (LTFSWs) as 0.59%, 0.92%, and 1.10%, respectively.3 LTFSWs are solicited on the street or at outdoor public places and charge a low fee for their services. The HIV and syphilis prevalence among LTFSWs has been estimated as 1.1% and 3.9%.3,4 LTFSWs use condoms inconsistently compared with other types of FSWs.5
Solicitation of prostitutes by men in China is relatively common. According to Pan et al,2 7.0% of urban men and 1.8 % of rural men visited FSWs in the last year. The typical Chinese client has a regular noncommercial partner.6 Clients of FSWs are at high risk for sexually transmitted diseases (STDs). They tend to have insufficient knowledge regarding STD transmission routes, perceive a low risk of acquiring STDs, and they use condoms inconsistently.7–11 McLaughlin et al6 estimated that clients of FSWs are at 12 times the risk of acquiring HIV compared with the general population. Clients of FSWs use condoms more frequently with FSWs than their noncommercial partners, which may explain their important role as vectors of STDs to low to average risk heterosexuals.12,13
Guangxi, in southern China, accounts for approximately 10% of reported HIV cases in China.14 Ninety-three percent of persons living with HIV/AIDS in Guangxi Province acquire HIV through heterosexual practices.14 FSWs share a high burden of STDs. HIV prevalence among LTFSWs was reported as 2.2% in 2014.15 Older men are particularly at risk for STDs due to their frequent visits to FSWs. In 2014, 46% of all HIV cases occurred in men over 50 years of age.14
Although the prevalence of HIV, syphilis, and HCV for individual years has been measured,16 the true burden of disease and the effectiveness of control measures over the long-term is unknown. Therefore, there we explore how HIV, syphilis, and HCV prevalence differ by sex worker classification and client age over 6 years. The findings from our study will better inform STD control measures for female sex workers and their male clients.
METHODS
Study Design and Study Participants
Serial cross-sectional studies were conducted yearly for surveillance purposes from 2010 to 2015, in all 14 prefectures and 64 city or county regions in Guangxi, China. The number of surveillance sites increased from 55 in 2010 to 84 by the end of 2015. Our sampling strategy included dedicating a site for surveying FSWs at every city or county region whereas 30% of cities or county regions were selected for surveying clients. The study protocol was developed by the Guangxi Center for Disease Control and Prevention (CDC) in accordance with national guidelines.17 Study participants included FSWs and their male clients. Eligibility criteria required FSWs to be at least 18 years old and clients to be 40 years of age. To be eligible, participants had to provide informed consent. History of sex work or solicitation of FSWs was by self-report. Sex work venues at each surveillance site were systematically mapped by an experienced outreach worker. The outreach worker subsequently recruited male clients to participate through providing study brochures and verbal encouragement. Outreach workers also invited clients, FSWs, and brothel managers to refer other male clients to the study. Those who met the screening criteria then completed an interview questionnaire and received HIV pretest counseling. Data quality was assured by assigning a noninterviewing staff member to examine questionnaires for errors, blanks, or inconsistent data. Participants were also given HIV post-test counseling when they returned for their HIV test results. The detailed study protocol is described elsewhere.17–19
Data Collection
Study participants were assigned a unique identifier number to collected data confidentially. Demographic variables collected included age, sex, ethnicity, marital status, and education. Behavioral variables were collected on unprotected sex with male clients or FSWs and prior sex with men. Variables on drug and IV drug use were also collected. Data on HCV infections among male clients was only available from 2013 to 2015. FSWs were categorized as high, middle, and low-tier FSWs according to the sex work venues where they solicit their clients. High-tier FSWs were from karaoke bars, bathhouses, or hotels; middle-tier FSWs were from hair salons, barbershops, massage parlors, foot bathing shops, roadside shops, guesthouses, or roadside restaurants; and LTFSWs were street based or worked in public outdoor places. Clients were categorized as middle age (40–49 years) and older clients (≥50 years).
Laboratory Methods
Blood samples were collected from all participants for serologic testing for HIV, syphilis, and HCV. Blood samples were tested for HIV antibodies with an enzyme-linked immunosorbent assay (ELISA). Western blot testing was conducted to confirm positive HIV ELISA results. For syphilis, all specimens were tested with ELISA and rapid plasma reagin testing in parallel. Patients with positive results on both tests were considered to have syphilis. Samples were tested for HCV antibodies by ELISA.
Statistical Analysis
Questionnaires and laboratory testing data were double entered and validated with EpiData software (EpiData 3.0 for Windows; The EpiData Association Odense, Denmark). Data were then transferred into SPSS software (version 17.0; SPSS Inc, Chicago, IL). Univariate proportions and means were calculated for categorical and continuous variables, respectively. The descriptive and Chi-square test for trends were used for categorical and continuous variables, respectively. P < 0.05 was considered statistically significant, and all tests were two sided.
Ethics Statement
The institutional review board of the Guangxi CDC approved this study of secondary surveillance data analysis.
RESULTS
Female Sex Workers
Table 1 shows the characteristics of FSWs surveyed (N = 120,049). The majority of sex workers were <35 years of age, married/cohabiting, of Han ethnicity, and with >6 years of education. The number of FSWs increased over 2010 to 2015. LTFSWs increased from 5095 to 10686; by the end of 2015, they comprised the majority of FSWs.
TABLE 1.
Demographic and Behavioral Characteristics by Survey Year Among FSWs in Guangxi, China, 2010 to 2015 (N = 120,049)
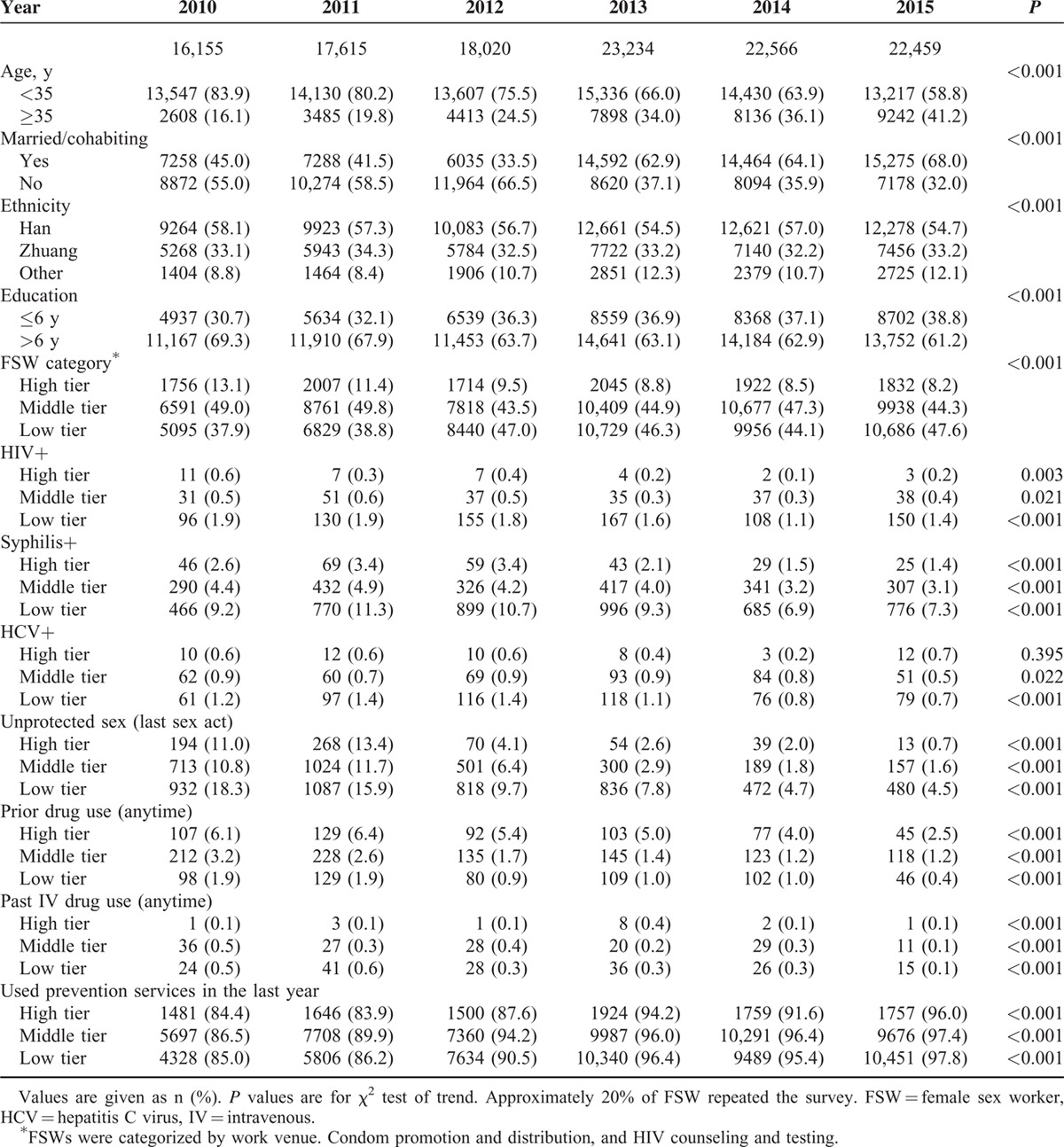
The prevalence of HIV in FSWs ranged from 1.9% for LTFSW in 2010 to 0.1% for high tier FSWs in 2014. Among FSWs, LTFSWs had the highest prevalence of HIV (Figure 1). HIV prevalence declined among LTFSWs over 2010 to 2013 (P < 0.001) but slightly increased by 0.3% from 2014 to 2015. Syphilis prevalence decreased across all categories of FSWs (P < 0.001) but began to increase slightly for LTFSWs starting in 2014 (Figure 1). The prevalence of syphilis peaked at 11.3% in 2011 for LTFSWs. HCV prevalence decreased among middle tier and LTFSWs (P = 0.02, P < 0.001, respectively). From 2010 to 2015, there was a substantial and significant increase in protected sex among all FSW tiers (P < 0.001). Consistent condom use by LTFSWs increased by 13.8% in 6 years; at the end of 2015, only 4.5% of LTFSWs reported using condoms inconsistently. Use of preventive services such as HIV testing also rose for all categories of FSWs during this time and was above 80% for all years (P < 0.001). Non-IV drug use among FSWs decreased from 2010 to 2015 (P < 0.001). IV drug use was essentially unchanged over the 6 years of the survey and remained <1% for all FSWs (Table 1).
FIGURE 1.
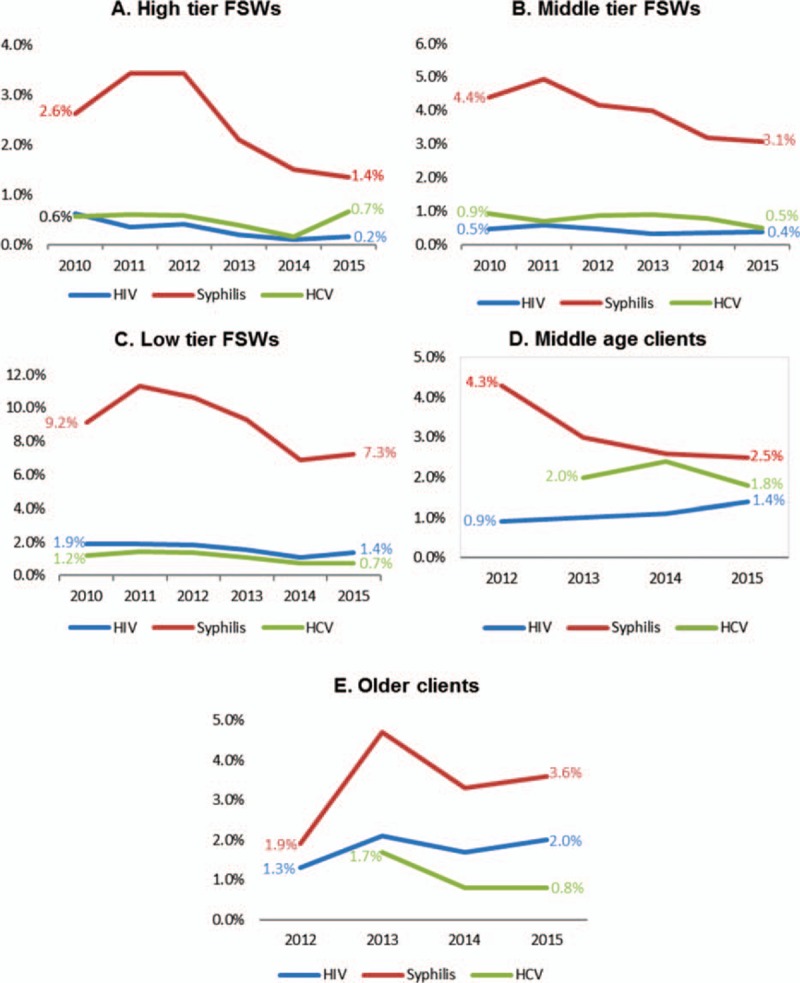
Prevalence of HIV, syphilis, and hepatitis C over time for FSWs and their clients taken from serial surveys, Guangix, China, 2010–2015. FSWs were categorized according to the sex work venues where they solicit their clients. Clients were categorized as middle age (40–49 years) and older clients (≥50 years). Data on HCV prevalence was only available for clients of FSWs from 2013–2015. FSWs = female sex workers, HCV = hepatitis C virus.
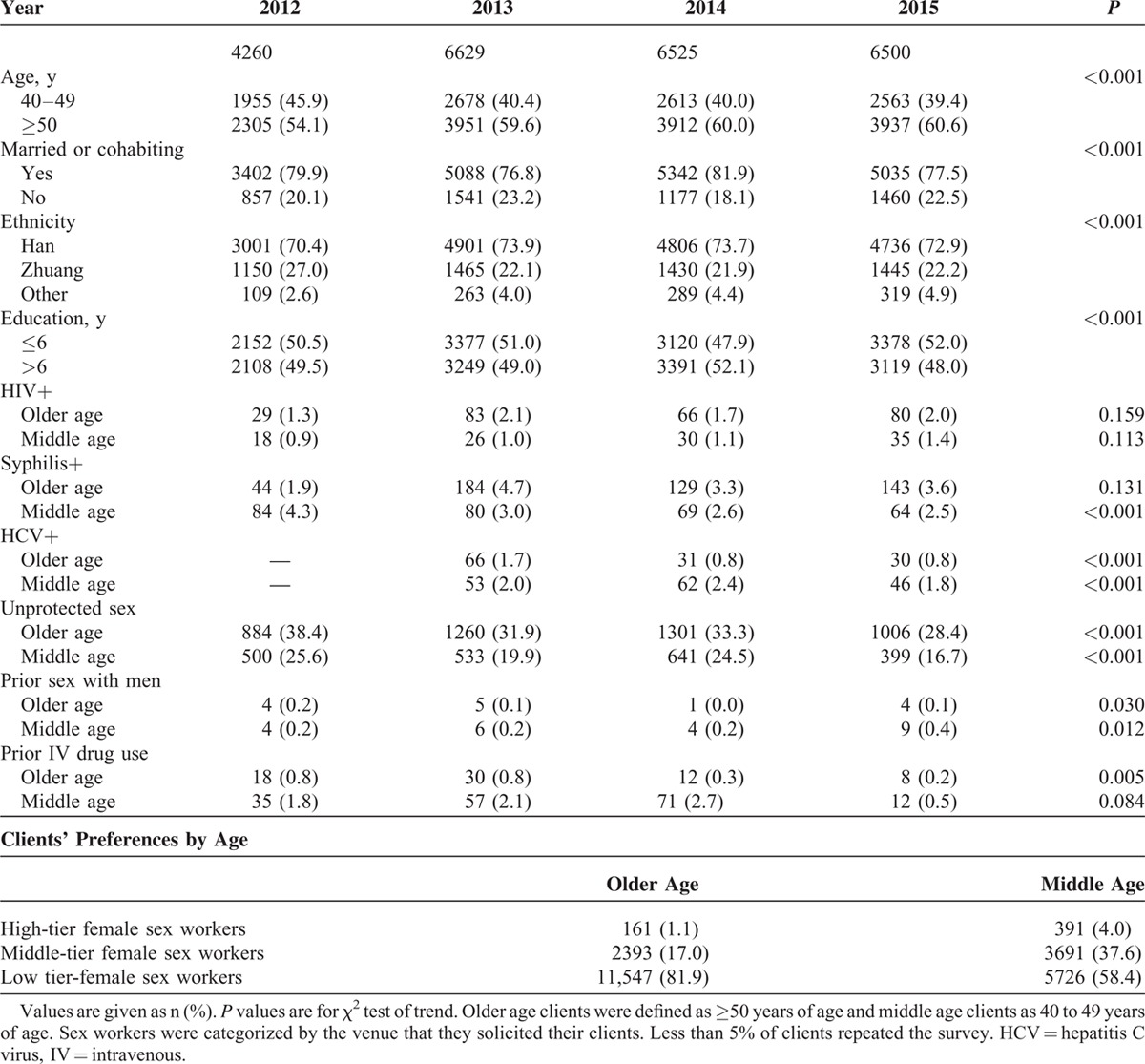
Clients of Female Sex Workers
Table 2 shows the characteristics of clients of FSWs (N = 23,914). The majority of clients were classified as older. Most were married, of Han ethnicity, and had 6 years of education or less. The prevalence of HIV fluctuated in older clients: in 2012 it was 1.3%, peaked at 2.1% in 2013, decreased to 1.7% in 2014, and increased to 2.0% in 2015 (Figure 1) (P = 0.159). Although not statistically significant, there was a small and steady increase in HIV prevalence in middle age clients. Except for 2012, the majority of syphilis infections occurred among older clients. Trends pointed to a decrease in syphilis among middle age clients by 1.3% over 2012 to 2013 and slower declines in subsequent years (P < 0.001). From 201 to 2015, the prevalence of HCV was more than halved among older clients (P < 0.001) and slightly declined for middle age clients (P < 0.001). Protected sex increased (P < 0.001), especially for older clients who improved their condom use by 10% over the study period. Less than 1% of clients reported having sex with men or intravenous drug use. Clients preferred LTFSWs. Older clients preferred LTFSWs more so than middle age clients (81.9% vs 58.4%, respectively) (Table 2).
TABLE 2.
Demographic and Behavioral Characteristics by Survey Year Among Clients of FSWs in Guangxi, China, 2010 to 2015 (N = 23,914)
DISCUSSION
Our research suggests that important gains in the control of HIV, syphilis, and HCV were made for FSWs from 2010 to 2015 in Guangxi Province, which is likely a result of increased use of condoms and preventive services. Notably, inconsistent condom use decreased in LTFSWs from 18.3% in 2010 to 4.5% in 2015. For comparison, a 2012 study by Zhang et al5 reported that around 34% of LTFSWs used condoms during their last paid sex act. Radio, television, and newspaper advertisements have helped to raise awareness on HIV prevention for women of reproductive age, which has likely improved consistent condom use.20,21 Perhaps, increased exposure to media sources or outreach programs fostered a greater awareness on the importance of using condoms consistently to prevent HIV among FSW in our sample. Other factors, however, may explain the decline in HIV and syphilis we observed, such as increased availability of treatment.
We found that the frequency of protected sex increased by 10% for older clients and 8.9% for middle age clients. At the end of 2015, 28.4% of older clients and 16.7% of middle age clients reported using a condom at their last paid sex encounter. For comparison, a 2010 study found that 33.7% of clients in Yunnan Province reported using a condom during their prior paid sex act.8
Surprisingly, over only 4 years, the prevalence of HIV increased by 0.5% for middle age clients and by 0.7% for older clients. Few studies report on long-term trends in HIV or syphilis prevalence in clients of FSWs in China. Thus, we compare our results for individual years to other studies to provide a benchmark. A study of clients of FSWs from a rural county of Guangxi Province in 2011 found that most clients were older (mean age 61.8 years) and that the prevalence of HIV and syphilis were 1.9% and 18.4%, respectively.22 The 2012 HIV prevalence in older clients in our sample (1.3%) was lower than that reported by Wu et al23 (2.9%). The prevalence of syphilis decreased among middle age clients but increased among older clients. The prevalence of syphilis among older clients in Guangxi Province in our sample was similar to that found by Lu et al16 (3.3% vs 3.4%) from 2012 to 2013. Of note, older clients in the Lu et al study were defined as 60 years and older whereas in our study we defined an older client as 50 years and above. These studies used different sampling strategies as well as choice of locations. These differences may explain the higher prevalence of HIV found in our study. In our study the rates of HIV and syphilis among clients >60 years ranged from 1.9% to 2.7% and 4.2% to 8.1%, respectively.
We anticipated a decline in HIV among clients of FSMs. The fall of intravenous drug use by clients, their increased condom use, as well as increased protective sex by FSM should have contributed to declining rates. Further, we also expected these positive behavior changes to decrease syphilis rates among older clients of FSMs. One possibility that HIV and syphilis rates did not decline as anticipated is that clients have changed their preferences for LTFSWs. Many older clients are from rural areas and may have relocated to cities for economic reasons. These migrants may prefer LTFSWs because of their low cost. In addition, China has increasingly cracked down on the illegal sex trade. Perhaps, clients have changed their preferences to LTFSWs workers because they perceive a lower risk for arrest outside compared with enclosed spaces such as karaoke bars. Further, we observed that the number of LTFSWs more than doubled over the survey period, which could reflect that we added survey sites each year. In addition, increased awareness about free preventive services may have drawn LTFSWs to the survey sites. Men who visit LTFSWs are less likely to practice safe sex than those who visit high tier FSWs.24,25 Increasing visits to LTFSWs may have increased clients’ susceptibility to STDs given that LTFSWs have a high burden of STDs relative to other tiers of FSWs. That older clients had a greater preference for LTFSWs and higher rates of HIV and syphilis than middle age clients lends support to our hypothesis. Finally, older clients may be at greater risk than younger clients because of use of aphrodisiacs, which were found to be a risk factor for inconsistent condom use and HIV infection in Guangxi.26 Further studies are needed to understand the increase in HIV infections among clients and the parallel decrease in LTFSWs. To better understand the role that clients of FSWs play as a bridging population, research is needed on their risk behaviors, preferences for FSWs, motivation for buying sex, and substance abuse.
Our study faced the following limitations. First, we were unable to calculate incidence and thus the risk of HIV, syphilis, or HCV over time. Second, it is possible that we underestimated the true prevalence of HIV among FSWs as they are a highly mobile population who may exit sex work to pursue other occupations. Third, serial surveys inquired only about intravenous drug use in clients: Knowledge on alcohol and noninjectable illicit drugs would have allowed us to better characterize substance abuse among clients of FSWs. Fourth, we did not inquire about client preferences. Therefore, we could not adequately explain why older clients overwhelmingly preferred LTFSM. Fifth, relying on surveillance data and increasing the number of surveillance sites may have overestimated the prevalence of HIV in clients through detection bias. Nevertheless, surveillance data show a steady increase in HIV among older men.27 Finally, we were not able to make any firm conclusions regarding trends in HCV prevalence for clients because they were only tested over 3 years.
In conclusion, we found increased condom use among FSWs and their clients. Compared with FSWs, clients used condoms less frequently. This may reflect that there are fewer targeted HIV outreach efforts for clients compared with FSWs. Although HIV rates declined among FSWs, there was an unexpected increase in HIV among clients. The prevalence of syphilis decreased among all groups surveyed except older clients. Possibilities for these observations may include increased susceptibility to STDs mediated through greater reliance on relatively higher risk LTFSWs workers. Further research should focus on ways to increase condom use among clients of FSWs.
Footnotes
Abbreviations: CDC = Chinese Centers for Disease Control and Prevention, FSWs = female sex workers, HCV = hepatitis C, HIV = human immunodeficiency virus, LTFSWs = low-tier female sex workers.
YC and SAB contributed equally to this work.
This study was supported by grants from the National Natural Science Foundation of China (81502862), Guangxi Bagui Honor Scholars, Chinese State Key Laboratory of Infectious Disease Development Grant, and the International Development Research Center of Canada (grant #104519–010). SAB contributed to this work during his fellowship, which was supported by National Institutes of Health (NIH) Research Training Grant R25 TW009337, funded by Fogarty International Center, the NIH Office of the Director, and the National institute of Mental Health.
The authors report no conflicts of interest.
REFERENCES
- 1.NCAIDS, NCSTD. Update on the AIDS/STD epidemic in China and main response in control and prevention in December, 2014. Chin J AIDS STD 2014; 3:145–146. [Google Scholar]
- 2.Pan S, Parish WL, Huang Y. Clients of female sex workers: a population-based survey of China. J Infect Dis 2011; 204 Suppl 5:S1211–S1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang L, Chow E, Su S, et al. A systematic review and meta-analysis of the prevalence, trends, and geographical distribution of HIV among Chinese female sex wokers (2000-2011): implications for preventing sexually transmitted HIV. Int J Infect Dis 2015; 39:76–86. [DOI] [PubMed] [Google Scholar]
- 4.Yang Z, Su J, Peng X, et al. A decline in HIV and syphilis epidemics in Chinese female sex workers (2000-2011): a systematic review and meta-analysis. PloS One 2013; 8:e82451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang C, Li X, Hong Y, et al. Unprotected sex with their clients among low-paying female sex workers in southwest China. AIDS Care 2013; 25:503–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McLaughlin MM, Chow EPF, Wang C, et al. Sexually transmitted infections among heterosexual male clients of female sex workers in China: a systematic review and meta-analysis. PloS One 2013; 8:e71394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang C, Li X, Su S, et al. Prevalence of HIV, syphilis, and HCV infection and associated risk factors among male clients of low-paying female sex workers in a rural county of Guangxi, China: a cross-sectional study. Sex Transm Infect 2014; 90:230–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reilly KH, Wang J, Zhu Z, et al. HIV and associated risk factors among male clients of female sex workers in a Chinese border region. Sex Transm Dis 2012; 39:750–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang C, Latkin C, Luan R, et al. Condom use with female sex workers among male clients in Sichuan Province, China: the role of interpersonal and venue-level factors. J Urban Health Bull N Y Acad Med 2010; 87:292–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang C, Latkin C, Luan R, et al. HIV, syphilis, hepatitis C and risk behaviours among commercial sex male clients in Sichuan province, China. Sex Transm Infect 2010; 86:559–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang C, Latkin CA, Liu P, et al. A qualitative study on commercial sex behaviors among male clients in Sichuan Province, China. AIDS Care 2010; 22:246–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sabidó M, Lahuerta M, Montoliu A, et al. Human immunodeficiency virus, sexually transmitted infections, and risk behaviors among clients of sex workers in Guatemala: are they a bridge in human immunodeficiency virus transmission? Sex Transm Dis 2011; 38:735–742. [DOI] [PubMed] [Google Scholar]
- 13.Niccolai LM, Odinokova VA, Safiullina LZ, et al. Clients of street-based female sex workers and potential bridging of HIV/STI in Russia: results of a pilot study. AIDS Care 2012; 24:665–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guangxi CDC. Prevention: Analysis of HIV/STD Epidemic in 2014. Nanning, China; 2014. [Google Scholar]
- 15.Li J, Zhang H, Shen Z, et al. Screening for acute HIV infections and estimating HIV incidence among female sex workers from low-grade venues in Guangxi, China. PloS One 2014; 9:e99522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lu H, Zhu Y, Wu X, et al. Study on the characteristics of commercial sexual behavior and the risk factors analysis of HIV infection among the old male clients, in Guangxi. Zhonghua Liu Xing Bing Xue Za Zhi 2015; 36:31–34. [PubMed] [Google Scholar]
- 17.Sun X, Wang N, Li D, et al. The development of HIV/AIDS surveillance in China. AIDS Lond Engl 2007; 21 Suppl 8:S33–S38. [DOI] [PubMed] [Google Scholar]
- 18.Chen Y, Shen Z, Morano JP, et al. Bridging the epidemic: a comprehensive analysis of prevalence and correlates of HIV, hepatitis C, and syphilis, and infection among female sex workers in Guangxi Province, China. PloS One 2015; 10:e0115311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang X, Lan G, Shen Z, et al. HIV and syphilis prevalence trends among men who have sex with men in Guangxi, China: yearly cross-sectional surveys, 2008–2012. BMC Infect Dis 2014; 14:367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maslovskaya O, Brown JJ, Smith PWF, et al. HIV awareness in China among women of reproductive age (1997-2005): a decomposition analysis. J Biosoc Sci 2014; 46:178–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xiao Z, Li X, Lin D, et al. Mass media and HIV/AIDS prevention among female sex workers in Beijing, China. J Health Commun 2015; 20:1095–1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang C, Li X, Su S, et al. Prevalence of HIV, syphilis, and HCV infection and associated risk factors among male clients of low-paying female sex workers in a rural county of Guangxi, China: a cross-sectional study. Sex Transm Infect 2014; 90:230–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Infection among Male Clients over 50 years old in low-cost commercial sex venues of Guangxi,China—ClinicalKey. Available at: https://www-clinicalkey-com.proxy.library.vanderbilt.edu/#!/content/journal/1-s2.0-S1098301515014849 Accessed December 15, 2015. [Google Scholar]
- 24.Lau JTF, Wan SP, Yu XN, et al. Changes in condom use behaviours among clients of female sex workers in China. Sex Transm Infect 2009; 85:376–382. [DOI] [PubMed] [Google Scholar]
- 25.Huang Y, Maman S, Pan S. Understanding the diversity of male clients of sex workers in China and the implications for HIV prevention programmes. Glob Public Health 2012; 7:509–521. [DOI] [PubMed] [Google Scholar]
- 26.Tang Z, Wu X, Li G, et al. Aphrodisiac use associated with HIV infection in elderly male clients of low-cost commercial sex venues in Guangxi, China: a matched case-control study. PloS One 2014; 9:e109452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guangxi CDC. Guangxi Center for Disease Control and Prevention: Analysis of HIV/STD epidemic in 2014. 2014. [Google Scholar]


