Abstract
Evidence shows that continued smoking by cancer patients leads to adverse treatment outcomes and affects survival. Smoking diminishes treatment effectiveness, exacerbates side effects, and increases the risk of developing additional complications. Patients who continue to smoke also have a higher risk of developing a second primary cancer or experiencing a cancer recurrence, both of which ultimately contribute to poorer quality of life and poorer survival. Here, we present a snapshot of smoking behaviours of current cancer patients compared with the non-cancer patient population in Canada.
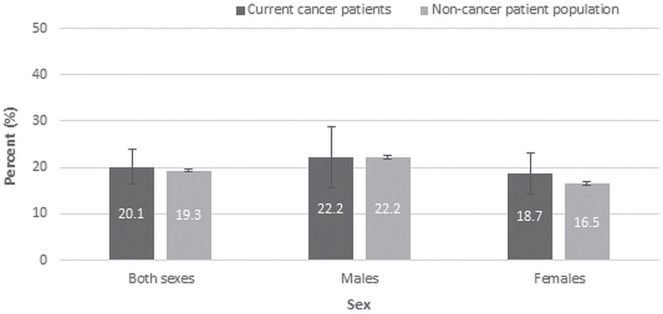
Minimal differences in smoking behaviours were noted between current cancer patients and the rest of the population. Based on 2011–2014 data from the Canadian Community Health Survey, 1 in 5 current cancer patients (20.1%) reported daily or occasional smoking. That estimate is comparable to findings in the surveyed non-cancer patient population, of whom 19.3% reported smoking daily or occasionally. Slightly more male cancer patients than female cancer patients identified as current smokers. A similar distribution was observed in the non-cancer patient population.
There is an urgent need across Canada to better support cancer patients in quitting smoking. As a result, the quality of patient care will improve, as will cancer treatment and survival outcomes, and quality of life for these patients.
Keywords: Smoking, smoking behaviours, cancer patients, adverse outcomes, Canadian Community Health Survey
INTRODUCTION
It is common knowledge that smoking is associated with many types of cancer, including those of lung, head and neck, esophagus, bladder, and cervix1,2. Currently, smoking cessation efforts are largely aimed at the prevention of cancer and other chronic diseases3. Smoking cessation for individuals diagnosed with cancer could be equally as important.
Evidence has shown that continued smoking by cancer patients leads to adverse cancer treatment outcomes and affects survival4–6. Smoking diminishes treatment effectiveness, particularly for radiation therapy and chemotherapy; it also exacerbates side effects, interferes with wound healing, and can be a risk factor for a wide range of pulmonary, cardiovascular, infectious, and wound-related complications3,4,7–9. Patients who smoke also have a higher risk of developing a second primary cancer or experiencing a cancer recurrence. All of those factors ultimately contribute to poorer quality of life and poorer survival10. Such adverse outcomes have been identified both in patients with smoking-related and non-smoking-related cancers3. The 2014 U.S. Surgeon General’s Report concluded that there is sufficient evidence linking smoking with adverse health outcomes in cancer patients and that quitting improves their prognosis6.
Here, we present a snapshot of smoking behaviours of current cancer patients compared with the non-cancer patient population in Canada, information that can be used by clinicians and policymakers to support broader adoption of evidence-based approaches to smoking cessation and to ensure that relapse prevention strategies are delivered to cancer patients.
METHODS
Smoking behaviours in Canadian cancer patients were examined using 4 years of self-reported data (2011–2014 combined) from the Canadian Community Health Survey (cchs), a population-based cross-sectional survey representative of the non-institutionalized Canadian population 12 years of age and older in all provinces and territories, excluding full-time members of the Canadian Forces, residents of First Nations reserves, and select remote areas11. For the purposes of the present study, 4 years of survey data were combined to reduce variability. Cancer patients were defined as respondents 12 years of age and older who answered yes to the “Do you have cancer” question; those who answered no were defined as the non-cancer patient population. Based on the survey weights, we identified 338,450 current cancer patients and 22,468,550 individuals without cancer. Weighted counts are reported using a rounding base of 250. Here, we focused on studying current cancer patients under the assumption that they best represent patients currently receiving treatment (and therefore the population most likely to experience adverse outcomes attributable to continued smoking). The analyses did not differentiate by type of cancer or by province and territory.
Smoking status (that is, daily or occasional) was derived from the subset of the respondents who provided a valid response to smoking-related questions. Estimates were age-standardized to the 2011 Canadian population to account for differences in age distribution across the cancer patient population compared with the non-cancer patient population. The analyses included data from all provinces and territories. All descriptive statistical analyses were conducted using the SAS software application (version 9.3: SAS Institute, Cary, NC, U.S.A.).
RESULTS
Minimal differences were noted in the age-standardized smoking estimates for current cancer patients compared with the non-cancer patient population. Based on 2011–2014 data, 2% of respondents were identified as current cancer patients. Of those cancer patients, 1 in 5 [20.1%; 95% confidence interval (ci): 16.3% to 23.9%] reported daily or occasional smoking (Figure 1). That estimate is comparable to the estimate in the surveyed non-cancer patient population, of whom 19.3% (95% ci: 19.0% to 19.6%) reported smoking daily or occasionally. Daily or occasional smoking was reported by 22.2% of male cancer patients (95% ci: 15.6% to 28.8%) compared with 18.7% of female cancer patients (95% ci: 14.2% to 23.2%), and by 22.2% of the male non-cancer patient population (95% ci: 21.7% to 22.7%) compared with 16.5% of the female non-cancer patient population (95% ci: 16.2% to 16.9%; Figure 1).
FIGURE 1.
Percentage of individuals 12 or more years of age reporting daily or occasional smoking, by sex and cancer status, Canada, age-standardized to the 2011 Canadian population, 2011–2014 reporting years combined. Vertical lines indicate the 95% confidence intervals. Data source: Statistics Canada, Canadian Community Health Survey.
DISCUSSION
Our findings demonstrate that a considerable proportion of smokers did not quit when faced with a cancer diagnosis in Canada. About 20% of current cancer patients in Canada are smokers. Similar conclusions have been reached in other studies showing that 20%–30% of cancer patients continue to smoke after their diagnosis12–14.
There are a number of possible explanations for why cancer patients continue to smoke. One important explanation is that cancer diagnosis and treatment are often unappreciated by health professionals as a teachable moment for smoking cessation3,15,16. Cancer patients might try to quit, but are unable to do so independently or with limited support7,17. In our results, the similarity in smoking rates between current cancer patients and the non-cancer patient population could be attributable to high smoking relapse rates among cancer patients despite attempts to quit immediately after a cancer diagnosis18,19. Alternatively, cancer patients might believe that the damage has already been done and therefore quitting might not help them7,17. The type of cancer diagnosis can also influence a smoker’s decision to quit. For example, patients with lung, head, or neck cancers are more likely to quit smoking after their diagnosis7,12, possibly because physicians discuss smoking more with such patients or because the patients themselves can easily link their smoking habits with their cancer7. Patients with other types of cancer (for example, colorectal, breast, or prostate) might not see the link and might therefore have less motivation to quit7,12. Additional reasons for continued smoking include psychological stress or depression after diagnosis, lack of social support (because smokers might have family members or friends who are also smokers), sex, education, and socioeconomic status17.
Given the harmful consequences of continued smoking after diagnosis, smoking cessation interventions are crucial for cancer patients. More efforts should be aimed at embedding cessation support as a standard of care for patients, regardless of whether their cancer is smoking-related. Effective interventions by health care professionals have been shown to increase smoking abstinence rates among cancer patients20. Because health care professionals often identify lack of experience, time, and resources as the main barriers to providing cessation support5, more action is required to mobilize such knowledge when developing support strategies for patients.
The present analysis had some limitations. One is that we could not compare the smoking status of patients before and after diagnosis, because time-of-diagnosis information is not collected by the cchs. It is possible that pre-diagnosis smoking rates were even higher and declined post-diagnosis to a rate similar to that in the non-cancer patient population. Studies have shown that about one half to two thirds of patients quit smoking after being diagnosed with certain cancers21,22; however, we were unable to reach such a conclusion. Second, patients in remission could also have been misclassified into the non-cancer patient population if they answered no to the “Do you have cancer” question, thus possibly underrepresenting the number of current cancer patients. Third, the cchs does not identify cancer patients by type of cancer, which prevented us from assessing whether the type of cancer (that is, smoking-related vs. non-smoking-related) differentially affects the patient’s motivation to quit and therefore the percentage of current smokers. Because cchs responses are self-reported, the presence of reporting bias could also have underestimated the percentage of cancer patients who are smokers: patient respondents might, because of stigma, have been more reluctant to reveal their post-diagnosis smoking status23,24. Wide confidence intervals for the estimates of current cancer patients are a result of the uncertainty associated with a small sample size. Lastly, it is important to note that adolescents 12–18 years of age were included in our analysis even though the cessation patterns for adolescents and adults can differ25; age standardization was used to minimize the impact on our results.
The present analysis underscores an urgent need across Canada to better support cancer patients in quitting smoking. Such efforts will improve the quality of patient care, including cancer treatment and survival outcomes, and quality of life for patients.
ACKNOWLEDGMENTS
The authors gratefully acknowledge the System Performance Steering Committee and Technical Working Group for providing insights on content related to the manuscript.
CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflicts of interest, and we declare that we have none.
REFERENCES
- 1.Canadian Cancer Society’s Advisory Committee on Cancer Statistics . Canadian Cancer Statistics. Toronto, ON: Canadian Cancer Society; 2015. 2015. [Google Scholar]
- 2.American Cancer Society(acs) Cancer Prevention and Early Detection: Facts and Figures 2015–2016. Atlanta, GA: ACS; 2015. [Google Scholar]
- 3.Gritz ER, Fingeret MC, Vidrine DJ, Lazev AB, Mehta NV, Reece GP. Successes and failures of the teachable moment: smoking cessation in cancer patients. Cancer. 2006;106:17–27. doi: 10.1002/cncr.21598. [DOI] [PubMed] [Google Scholar]
- 4.Warren GW, Sobus S, Gritz ER. The biological and clinical effects of smoking by patients with cancer and strategies to implement evidence-based tobacco cessation support. Lancet Oncol. 2014;15:e568–80. doi: 10.1016/S1470-2045(14)70266-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Warren GW, Dibaj S, Hutson A, Cummings KM, Dresler C, Marshall JR. Identifying targeted strategies to improve smoking cessation support for cancer patients. J Thorac Oncol. 2015;10:1532–7. doi: 10.1097/JTO.0000000000000659. [Erratum in: J Thorac Oncol 2015;10:1702] [DOI] [PubMed] [Google Scholar]
- 6.United States, Department of Health and Human Services . The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- 7.Park ER, Japuntich SJ, Rigotti NA, et al. A snapshot of smokers after lung and colorectal cancer diagnosis. Cancer. 2012;118:3153–64. doi: 10.1002/cncr.26545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burke L, Miller LA, Saad A, Abraham J. Smoking behaviors among cancer survivors: an observational clinical study. J Oncol Pract. 2009;5:6–9. doi: 10.1200/JOP.0912001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moller AM, Pedersen T, Villebro N, Schnaberich A, Haas M, Tonnesen R. A study of the impact of long-term tobacco smoking on postoperative intensive care admission. Anaesthesia. 2003;58:55–9. doi: 10.1046/j.1365-2044.2003.02788_2.x. [DOI] [PubMed] [Google Scholar]
- 10.Parsons A, Daley A, Begh R, Aveyard P. Influence of smoking cessation after diagnosis of early stage lung cancer on prognosis: systematic review of observational studies with meta-analysis. BMJ. 2010;340:b5569. doi: 10.1136/bmj.b5569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Statistics Canada . Canadian Community Health Survey – Annual Component (CCHS) [Web resource] Ottawa, ON: Statistics Canada; 2015. [Available at: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3226; cited 11 February 2016] [Google Scholar]
- 12.Demark-Wahnefried W, Aziz NM, Rowland JH, Pinto BM. Riding the crest of the teachable moment: promoting long-term health after the diagnosis of cancer. J Clin Oncol. 2005;23:5814–30. doi: 10.1200/JCO.2005.01.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garces YI, Yang P, Parkinson J, et al. The relationship between cigarette smoking and quality of life after lung cancer diagnosis. Chest. 2004;126:1733–41. doi: 10.1378/chest.126.6.1733. [DOI] [PubMed] [Google Scholar]
- 14.Tseng TS, Lin HY, Moody-Thomas S, Martin M, Chen T. Who tended to continue smoking after cancer diagnosis: the national health and nutrition examination survey 1999–2008. BMC Public Health. 2012;12:784. doi: 10.1186/1471-2458-12-784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weaver KE, Danhauer SC, Tooze JA, et al. Smoking cessation counseling beliefs and behaviors of outpatient oncology providers. Oncologist. 2012;17:455–62. doi: 10.1634/theoncologist.2011-0350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Simmons VN, Litvin EB, Unrod M, Brandon TH. Oncology healthcare providers’ implementation of the 5A’s model of brief intervention for smoking cessation: patients’ perceptions. Patient Educ Couns. 2012;86:414–19. doi: 10.1016/j.pec.2011.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duffy SA, Louzon SA, Gritz ER. Why do cancer patients smoke and what can providers do about it? Community Oncol. 2012;9:344–52. doi: 10.1016/j.cmonc.2012.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coups EJ, Ostroff JS. A population-based estimate of the prevalence of behavioral risk factors among adult cancer survivors and noncancer controls. Prev Med. 2005;40:702–11. doi: 10.1016/j.ypmed.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 19.Pasichnyk D, Guo B, Harstall C, Tjosvold L. Rapid Review of the Impact of Continued Tobacco Use on Treatment Efficacy in Cancer Patients. Toronto, ON: Canadian Partnership Against Cancer; 2014. [Google Scholar]
- 20.Park ER, Japuntich S, Temel J, et al. A smoking cessation intervention for thoracic surgery and oncology clinics: a pilot trial. J Thorac Oncol. 2011;6:1059–65. doi: 10.1097/JTO.0b013e318215a4dc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gritz ER, Nisenbaum R, Elashoff RE, Holmes EC. Smoking behavior following diagnosis in patients with stage i non-small cell lung cancer. Cancer Causes Control. 1991;2:105–12. doi: 10.1007/BF00053129. [DOI] [PubMed] [Google Scholar]
- 22.Schnoll RA, Zhang B, Rue M, et al. Brief physician-initiated quit-smoking strategies for clinical oncology settings: a trial coordinated by the Eastern Cooperative Oncology Group. J Clin Oncol. 2003;21:355–65. doi: 10.1200/JCO.2003.04.122. [DOI] [PubMed] [Google Scholar]
- 23.Chapple A, Ziebland S, McPherson A. Stigma, shame, and blame experienced by patients with lung cancer: qualitative study. BMJ. 2004;328:1470. doi: 10.1136/bmj.38111.639734.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shin DW, Park JH, Kim SY, et al. Guilt, censure, and concealment of active smoking status among cancer patients and family members after diagnosis: a nationwide study. Psychooncology. 2014;23:585–91. doi: 10.1002/pon.3460. [DOI] [PubMed] [Google Scholar]
- 25.United States, Department of Health and Human Services . Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2012. [Google Scholar]