Abstract
Masked hypertension, defined as non-elevated clinic blood pressure and elevated out-of-clinic blood pressure may be an intermediary stage in the progression from normotension to hypertension. We examined the associations of out-of-clinic blood pressure and masked hypertension using ambulatory blood pressure monitoring with incident clinic hypertension in the Jackson Heart Study, a prospective cohort of African Americans. Analyses included 317 participants with clinic blood pressure <140/90mmHg, complete ABPM, who were not taking antihypertensive medication at baseline in 2000–2004. Masked daytime hypertension was defined as mean daytime blood pressure ≥135/85mmHg; masked nighttime hypertension as mean nighttime blood pressure ≥120/70mmHg; and masked 24-hour hypertension as mean 24-hour blood pressure ≥130/80mmHg. Incident clinic hypertension, assessed at study visits in 2005–2008 and 2009–2012, was defined as the first visit with clinic systolic/diastolic blood pressure ≥140/90mmHg or antihypertensive medication use. During a median follow-up of 8.1 years, there were 187 (59.0%) incident cases of clinic hypertension. Clinic hypertension developed in 79.2% and 42.2% of participants with and without any masked hypertension, 85.7% and 50.4% with and without masked daytime hypertension, 79.9% and 43.7% with and without masked nighttime hypertension and 85.7% and 48.2% with and without masked 24-hour hypertension, respectively. Multivariable-adjusted hazard ratios (95% CI) of incident clinic hypertension for any masked hypertension and masked daytime, nighttime, and 24-hour hypertension were 2.13 (1.51–3.02), 1.79 (1.24–2.60), 2.22 (1.58–3.12), and 1.91 (1.32–2.75), respectively. These findings suggest that ambulatory blood pressure monitoring can identify African Americans at increased risk for developing clinic hypertension.
Keywords: ambulatory blood pressure, hypertension, African Americans, masked hypertension
Introduction
Ambulatory blood pressure (BP) monitoring (ABPM) complements clinic BP by obtaining out-of-clinic BP measurements, typically over a 24-hour period.1 Many individuals without elevated clinic BP have elevated BP on ABPM, a phenomenon termed “masked hypertension”.2 Individuals with masked hypertension have an increased prevalence of subclinical cardiovascular disease (CVD) and risk of CVD events and mortality when compared to individuals with sustained normortension, defined as having non-elevated clinic and ambulatory BP.3–8
Masked hypertension may represent an intermediate phenotype between sustained normotension, defined as having non-elevated clinic and ambulatory BP, and sustained hypertension, defined as having elevated clinic and ambulatory BP.9–11 However, there are few data on the risk for incident hypertension associated with masked hypertension particularly among African Americans (AAs), a population with a high prevalence of masked hypertension4 and also a high risk for incident hypertension.12 Previous studies have shown that lifestyle modification and pharmacological therapy prevent the onset of hypertension.13–17 If masked hypertension is associated with an increased risk of incident hypertension, then these preventive strategies may be appropriate for individuals with masked hypertension.
In the current study, we examined the associations of masked daytime, masked nighttime, and masked 24-hour hypertension with incident clinic hypertension among participants in the Jackson Heart Study (JHS), a cohort study comprised exclusively of African Americans. We also examined the association of mean daytime, nighttime, and 24-hour BP with incident clinic hypertension. Further, we evaluated whether these associations were independent of clinic BP and observed for both participants with prehypertension and normal clinic BP.
Methods
Study Population
The JHS is a population-based prospective cohort study, which was designed to evaluate CVD risk among AAs.18,19 The JHS enrolled 5,301 non-institutionalized AAs, aged ≥21 years, between 2000 and 2004 from the Atherosclerosis Risk in the Community (ARIC) site in Jackson, MS, and a representative sample of urban and rural Jackson, MS metropolitan tri-county (Hinds, Madison and Rankin counties) residents, volunteers, randomly selected individuals, and secondary family members.20 The current analysis was restricted to 1,148 JHS participants who completed ABPM following the baseline study visit (Visit 1). Participants who did not meet the International Database on ABPM in relation to Cardiovascular Outcomes21 (IDACO) criteria for valid ABPM (n=102; described below), or who were missing clinic BP or information on antihypertensive medication use at the baseline visit (n=63) were excluded. Participants whose incident clinic hypertension status could not be determined, including those who did not attend Visit 2 (2005–2008) and Visit 3 (2009–2012) (n=82) or with missing information on BP or antihypertensive medication use at both of these visits (n=10) were also excluded as their incident clinic hypertension status could not be determined. For the current analysis, we further excluded participants with clinic systolic BP (SBP) ≥140 mm Hg or diastolic BP (DBP) ≥90 mmHg or who were on antihypertensive medication during the baseline visit (n=574) leaving 317 participants for the current analysis. The JHS was approved by the institutional review boards of the University of Mississippi Medical Center, Jackson State University, and Tougaloo College. The institutional review boards at Columbia University and University of Alabama at Birmingham approved the use of JHS data for the current analysis. All participants provided written informed consent.
Data Collection & Clinical Covariates
Detailed description of data collection, methodology, specimen collection, and specimen processing from the baseline visit (Visit 1) can be found in the online supplement (Supplemental Methods) and have been previously described.19,22 Briefly, data were collected at baseline during an in-home interview, clinic examination, and ABPM. During the clinic examination, trained technicians measured height, weight and BP, collected blood samples, and conducted 2D echocardiography. Antihypertensive medication use was defined by self-report. Clinic BP was measured following standardized procedures as described below. Left ventricular mass (LVM) and LVM index (LVMI) were derived according to American Society of Echocardiography recommendations.23 Left ventricular hypertrophy (LVH) was defined as LVMI ≥ 89 g/m2 in females and LVMI ≥ 103 g/m2 in males. After the clinical examination, participants completed ABPM.
Clinic BP measurement
At each visit, participants rested for at least 5 minutes in an upright position with their back and arms supported, feet flat on the floor and legs uncrossed prior to having their BP measured. Trained staff conducted two BP measurements in the right arm. One minute elapsed between the two measurements. An appropriate cuff size, determined from an arm circumference measurement, was used. The JHS Coordinating Center conducted quality control by monitoring digit preference for each technician and by comparing mean BP measurements within and between trained technicians. The two clinic-measured BP measurements were averaged for analysis.
Clinic BP was measured using a random zero sphygmomanometer (Hawksley and Sons Ltd., Lancing, UK) at Visits 1 and 2 and a semi-automatic oscillometric device (Omron HEM-907XL, Omron Healthcare Inc., Lake Forest, Il.) at Visit 3. Among the 4,182 JHS participants who attended Visit 2 and had clinic BP measurement, 2,115 were included in a BP comparability substudy for which BP was assessed simultaneously, using a Y connector, by random zero sphygmomanometer and the Omron HEM-907XL device. As described in the Supplemental Methods, the random-zero BP measurements were calibrated to the semi-automated device using robust regression. When available, clinic BP from the semi-automated device was used. In the current analysis, the calibrated BP measurements were used at Visit 1 for the 317 participants, and at Visit 2 for 206 participants who did not have their BP measured using the semi-automatic oscillometric device.
Incident clinic hypertension was defined as the first follow-up study visit (Visits 2 or 3) with clinic SBP ≥ 140 mm Hg, DBP ≥ 90 mm Hg, or antihypertensive medication use.
ABPM
Immediately following the baseline exam, participants were fitted with an ABPM device (Spacelabs 90207, Spacelabs, Redmond, WA) on their non-dominant arm. Ambulatory BP was recorded every 20 minutes. After 24 hours, the device was removed and data were downloaded onto a computer and processed with Medifacts International’s Medicom software (Rockville, MD). IDACO criteria were used to define whether the ABPM measurement was complete. Specifically, participants were considered to have a complete ABPM if they had ≥10 daytime (10:00 to 20:00) and ≥5 nighttime (00:00 to 06:00) SBP and DBP measurements.21 Mean daytime SBP and DBP, mean nighttime SBP and DBP, and mean 24-hour SBP and DBP were calculated by averaging the readings during the daytime, nighttime and the entire ABPM period, respectively.
Daytime hypertension was defined as mean daytime SBP ≥ 135mmHg or mean daytime DBP ≥ 85mmHg, nighttime hypertension was defined as mean nighttime SBP ≥ 120mmHg or mean nighttime DBP ≥ 70mmHg and 24-hour hypertension was defined as mean SBP ≥ 130mmHg or mean DBP ≥ 80mmHg based on all available readings. Since the current analysis was restricted to participants with non-elevated clinic-measured BP (clinic SBP/DBP < 140mmHg/90 mm Hg), participants with daytime, nighttime and 24-hour hypertension had masked daytime, masked nighttime and masked 24-hour hypertension, respectively. Additionally, participants with masked daytime, nighttime or 24-hour hypertension were categorized as having any masked hypertension.
Statistical analyses
Baseline participant characteristics were calculated for the analytical sample as mean ± standard deviation (SD) or percentages. The prevalence of any masked hypertension and masked daytime, nighttime and 24-hour hypertension was calculated. The percentage of participants developing hypertension was calculated by quartile of mean daytime, nighttime, and 24-hour SBP. Since we do not know the exact date participants developed hypertension, only that it developed between two study visits, interval-censored Cox regression24 was used to calculate hazard ratios (HRs) for incident hypertension associated with higher quartiles (quartiles 2, 3 and 4) versus lowest quartile (quartile 1) of mean daytime, nighttime, and, separately, 24-hour SBP. Three models with progressive adjustment were estimated. Models adjusted for age and sex (Model 1), variables in the Framingham hypertension risk prediction score25 including age, sex, BMI, clinic SBP, parental history of hypertension, smoking status, age by clinic DBP interaction (Model 2). A final model included additional adjustment for diabetes, education level less than high school, alcohol consumption, total physical activity score, and reduced estimated glomerular filtration rate (eGFR) (Model 3). The above analyses were repeated for higher quartiles (quartiles 2, 3 and 4) versus the lowest quartile (quartile 1) of mean daytime, nighttime and 24-hour DBP. HRs for incident hypertension associated with SD higher mean daytime, nighttime and 24-hour SBP and DBP were also calculated. The percentage of participants developing hypertension was calculated for those with and without any masked hypertension, and masked daytime, nighttime, and 24-hour hypertension. HRs for incident hypertension associated with any masked hypertension, and masked daytime, nighttime, and 24-hour hypertension were calculated with adjustment for covariates in three models as described above.
As prior studies have demonstrated that prehypertension is associated with a higher risk for incident hypertension compared to normal clinic BP,26–29 and that an overlap exists between masked hypertension and prehypertension,4,30 secondary analyses were performed after stratifying the sample into participants with prehypertension or normal CBP at baseline. Prehypertension was defined as mean clinic SBP 120–139mmHg or mean clinic DBP 80–89mmHg. Normal clinic BP was defined as mean clinic SBP < 120mmHg and mean clinic DBP < 80mmHg. Analyses were performed using SAS Version 9.4 (SAS Institute, Cary NC) and Stata Version13.1 (Stata Inc., College Station, TX).
Results
Baseline Characteristics
The mean ± SD age of participants included in the current analysis was 54.8 ± 11.1 years and 69.1% were female (Table S1). The prevalence of prehypertension was 57.1%. The prevalence of masked daytime hypertension, masked nighttime hypertension, and masked 24-hour hypertension, were 22.3%, 42.3%, and 28.7%, respectively. Overall, 45.4% of participants had any masked hypertension. Compared with JHS participants who were not included in the analyses, those who were included were older, more likely to be female, had higher high-density lipoprotein cholesterol, had a higher LVMI, were more likely to have LVH, were less likely to be a current smoker, and had higher clinic SBP and lower clinic DBP.
Ambulatory BP and Incident Clinic Hypertension
The median time between Visit 1 and Visit 2 and Visit 1 and Visit 3 was 5.0 and 8.1 years, respectively. During follow-up, there were 187 cases (59.0%) of incident clinic hypertension; 124 cases at Visit 2 and an additional 63 cases at Visit 3. Of the 187 cases of incident hypertension, 44 (23.5%) had incident hypertension based on having clinic SBP ≥ 140 mmHg or clinic DBP ≥ 90 mmHg without taking antihypertensive medication and 120 (64.2%) had incident hypertension based on taking antihypertensive medication without having either clinic SBP ≥ 140 mmHg or clinic DBP ≥ 90 mmHg at a follow-up visit. Finally, 23 (12.3%) had incident hypertension based on having clinic SBP ≥ 140 mmHg or clinic DBP ≥ 90 mmHg at a follow-up visit and were also taking antihypertensive medication.
After adjustment for age and sex, higher quartiles of daytime, nighttime and 24-hour SBP were associated with an increased risk of incident hypertension (Model 1, Table 1). These associations remained present after further multivariable adjustment. Higher quartiles of daytime, nighttime and 24-hour DBP were also associated with an increased risk of incident clinic hypertension before and after multivariable adjustment (Table S2). When modeled as continuous variables, higher daytime, nighttime, and 24-hour SBP and DBP were associated with an increased risk of incident clinic hypertension (Table S3).
Table 1.
Hazard ratios for clinic hypertension by quartiles of daytime, nighttime and 24-hour systolic blood pressure on ambulatory blood pressure monitoring among Jackson Heart Study participants.
| Quartiles | Quartile range (mm Hg) | N cases of incident hypertension/N at risk (% with incident hypertension) | Hazard ratio (95% confidence interval) | ||
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |||
|
Quartiles of daytime systolic blood pressure
| |||||
| Quartile 1 | < 116.1 | 21/79 (26.6%) | 1 (ref) | 1 (ref) | 1 (ref) |
| Quartile 2 | ≥ 116.1 and < 124.2 | 41/79 (51.9%) | 2.26 (1.33 – 3.84) | 1.93 (1.12–3.31) | 2.14 (1.22–3.73) |
| Quartile 3 | ≥ 124.5 and < 131.9 | 54/80 (67.5%) | 3.65 (2.18 – 6.10) | 2.66 (1.56–4.53) | 2.89 (1.67–5.01) |
| Quartile 4 | ≥ 131.9 | 71/79 (89.9%) | 7.35 (4.32 – 12.49) | 4.59 (2.59–8.11) | 4.94 (2.72–8.98) |
| P-trend | - | <0.001 | <0.001 | <0.001 | |
|
| |||||
|
Quartiles of nighttime systolic blood pressure
| |||||
| Quartile 1 | < 105.3 | 25/78 (32.1%) | 1 (ref) | 1 (ref) | 1 (ref) |
| Quartile 2 | ≥ 105.3 and < 113.6 | 39/80 (48.8%) | 1.80 (1.08 – 2.99) | 1.54 (0.92–2.59) | 1.57 (0.93–2.63) |
| Quartile 3 | ≥ 113.6 and < 122.4 | 52/80 (65.0%) | 2.81 (1.73 – 4.58) | 2.12 (1.28–3.51) | 2.15 (1.29–3.59) |
| Quartile 4 | ≥ 122.4 | 71/79 (89.9%) | 5.41 (3.32 – 8.81) | 3.52 (2.09–5.91) | 3.59 (2.12–6.08) |
| P-trend | - | <0.001 | <0.001 | <0.001 | |
|
| |||||
|
Quartiles of 24-hour systolic blood pressure
| |||||
| Quartile 1 | < 112.5 | 22/79 (27.8%) | 1 (ref) | 1 (ref) | 1 (ref) |
| Quartile 2 | ≥ 112.4 and < 119.3 | 37/79 (46.8%) | 1.87 (1.10 – 3.19) | 1.53 (0.89–2.63) | 1.55 (0.90–2.68) |
| Quartile 3 | ≥ 119.3 and < 128.3 | 57/80 (71.3%) | 3.95 (2.39 – 6.53) | 2.69 (1.58–4.59) | 2.79 (1.62–4.80) |
| Quartile 4 | ≥ 128.3 | 71/79 (89.9%) | 6.77 (4.03 – 11.35) | 4.26 (2.42–7.49) | 4.25 (2.38–7.59) |
| P-trend | - | <0.001 | <0.001 | <0.001 | |
Model 1 includes adjustment for age and sex.
Model 2 includes Model 1 variables plus additional adjustment for body mass index, clinic systolic blood pressure, parental history of hypertension, smoking status (never/former, current), age by clinic diastolic blood pressure interaction.
Model 3 includes Model 2 variables plus additional adjustment for diabetes, education level less than high school, alcohol consumption (non-drinker, moderate, heavy), total physical activity score, and eGFR < 60 ml/min/1.73m2.
Masked Hypertension and Incident Clinic Hypertension
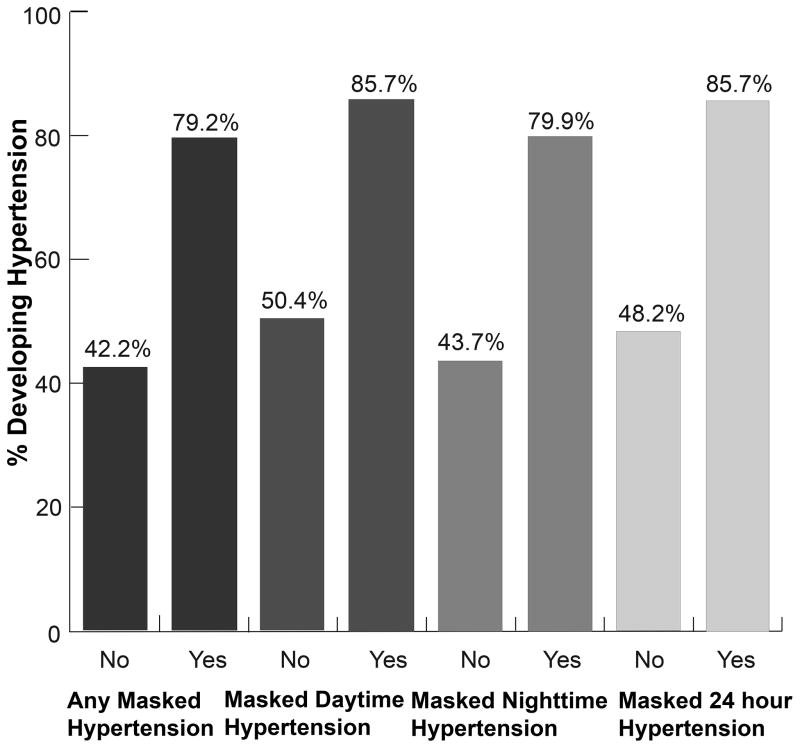
Overall, 79.2% and 42.2% of participants with and without any masked hypertension developed incident clinic hypertension during follow-up (Figure 1). The proportion of participants developing incident clinic hypertension was higher among participants with versus without masked daytime hypertension (85.7% versus 50.4%), masked nighttime hypertension (79.9% versus 43.7%) and masked 24-hour hypertension (85.7% versus 48.2%). After multivariable adjustment, any masked hypertension and masked daytime, nighttime, and 24-hour hypertension were each associated with an increased risk of incident clinic hypertension (Table 2).
Figure 1.
Percent developing clinic hypertension in individuals with and without any masked hypertension, masked daytime hypertension, masked nighttime hypertension, and masked 24-hour hypertension.
Table 2.
Hazard ratios for clinic hypertension associated with any masked hypertension, masked daytime hypertension, masked nighttime hypertension, and masked 24-hour hypertension among Jackson Heart Study participants.
| Type of Masked Hypertension | Hazard ratio (95% confidence interval) | |||
|---|---|---|---|---|
| Any masked hypertension | N cases of incident hypertension/N at risk (% with incident hypertension) | Model 1 | Model 2 | Model 3 |
| No | 73/173 (42.2%) | 1 (ref) | 1 (ref) | 1 (ref) |
| Yes | 114/144 (79.2%) | 2.83 (2.08 – 3.85) | 2.09 (1.49–2.91) | 2.13 (1.51–3.02) |
| Masked daytime hypertension | N cases of incident hypertension/N at risk (% with incident hypertension) | Model 1 | Model 2 | Model 3 |
| No | 121/240 (50.4%) | 1 (ref) | 1 (ref) | 1 (ref) |
| Yes | 66/77 (85.7%) | 2.74 (1.97 – 3.80) | 1.80 (1.25–2.58) | 1.79 (1.24–2.60) |
| Masked nighttime hypertension | N cases of incident hypertension/N at risk (% with incident hypertension) | Model 1 | Model 2 | Model 3 |
| No | 80/183 (43.7%) | 1 (ref) | 1 (ref) | 1 (ref) |
| Yes | 107/134 (79.9%) | 2.72 (2.01 – 3.69) | 2.16 (1.55–2.99) | 2.22 (1.58–3.12) |
| Masked 24-hour hypertension | N cases of incident hypertension/N at risk (% with incident hypertension) | Model 1 | Model 2 | Model 3 |
| No | 109/226 (48.2%) | 1 (ref) | 1 (ref) | 1 (ref) |
| Yes | 78/91(85.7%) | 2.67 (1.96 – 3.65) | 1.86 (1.31–2.63) | 1.91 (1.32–2.75) |
Model 1 includes adjustment for age and sex.
Model 2 includes Model 1 variables plus additional adjustment for body mass index, clinic systolic blood pressure, parental history of hypertension, smoking status (never/former, current), age by clinic diastolic blood pressure interaction.
Model 3 includes Model 2 variables plus additional adjustment for diabetes, education level less than high school, alcohol consumption (non-drinker, moderate, heavy), total physical activity score, and eGFR < 60 ml/min/1.73m2.
Masked Hypertension and the Risk of Incident Clinic Hypertension Stratified by Prehypertension Status
Higher daytime, nighttime, and 24-hour SBP and DBP were each associated with an increased risk of clinic hypertension among participants with prehypertension. (Table S4). Among individuals with normal clinic BP, higher daytime, nighttime, and 24-hour SBP were associated with an increased risk of incident clinic hypertension. Higher nighttime and 24-hour DBP, but not daytime DBP, were associated with incident clinic hypertension in participants with normal CBP. Also, among participants with prehypertension, any masked hypertension, as well as each type of masked hypertension, was associated with an increased risk of clinic hypertension after multivariable adjustment (Table S5). Among participants with normal clinic BP, any masked hypertension and masked nighttime hypertension were associated with an increased risk of incident clinic hypertension. Any masked hypertension and incident hypertension occurred among 51.9% (94/181) of participants with prehypertension and 14.7% (20/136 of participants with normal clinic BP. Among participants with prehypertension, 33.7% (61/181) had masked daytime hypertension and incident hypertension; 48.1% (87/181) had masked nighttime hypertension and incident hypertension; and 39.2% (71/181) had masked 24-hour hypertension and incident hypertension. Among participants with normal clinic BP, these estimates were 3.7% (5/136), 14.7% (20/136) and 5.1% (7/136), respectively.
Discussion
In the current population-based sample of AAs with non-elevated clinic BP at baseline, higher levels of ambulatory BP were associated with an increased risk for incident clinic hypertension. Additionally, having any masked hypertension was associated with an increased risk for incident clinic hypertension as was each type of masked hypertension. Only a few studies, mostly in Whites, have examined the association between masked hypertension and the development of hypertension.7,31–33 In an outpatient sample of 34 Spanish children and adolescents, aged 6 to 18 years old, with masked daytime hypertension, Lurbe et al.31 showed that after a median follow-up of 37 months there were 3 participants (8.8%) who developed sustained hypertension. No participants in the control group of 200 children and adolescents with sustained normotension progressed to sustained hypertension. In the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) Study, which enrolled a population-sample from Monza, Italy32, 47.1% of participants with masked 24-hour hypertension developed sustained hypertension after 10 years of follow-up compared with 18.2% of those with sustained normotension. Also, in a study of 232 Canadian public insurance employees with masked daytime hypertension, sustained hypertension was present in 61 (26.3%) participants after 3 years and 81 (34.9%) participants after 5 years of follow-up.33 In that study, the progression from sustained normotension to sustained hypertension was not reported.
An important limitation of our study is that ABPM was not performed at the follow-up visits. Therefore, the current study was unable to confirm whether participants categorized as having clinic hypertension at follow-up had sustained hypertension or white coat hypertension, defined as elevated clinic BP but non-elevated ambulatory BP. However, prior studies have shown that the progression of masked hypertension to white coat hypertension is uncommon. In the PAMELA study,32 and in a study by Trudel et al.33, only 7.6% and 0.5%, respectively, of participants with masked hypertension at baseline had white coat hypertension during follow-up. Therefore, it is likely that most of the participants in the current study with incident clinic hypertension during follow-up had sustained hypertension. The current study was also unable to determine the percentage of participants with masked hypertension at baseline who continued to have masked hypertension or alternatively had sustained normotension at follow-up. In the PAMELA study, among participants with masked hypertension at baseline and who did not have elevated clinic BP at follow-up, 51.9% and 48.1% had masked hypertension and sustained normotension, respectively, during follow-up.32
In younger adults, clinic BP is, on average, lower than ambulatory BP.9,10,34,35 It has been proposed that during the aging process, some individuals reach a stage where their ambulatory BP exceeds the threshold for a diagnosis of hypertension while their clinic BP is not yet in the hypertensive range;9,10 many of these individuals are likely to have prehypertension. We have previously reported that there is a substantial overlap between masked hypertension and prehypertension.30 Given that prehypertension is associated with an increased risk of incident clinic hypertension compared to normal clinic blood pressure,29 prehypertension may explain the increased risk for clinic hypertension among individuals with masked hypertension. However, in the current study, the association between any masked hypertension and incident clinic hypertension was independent of clinic BP level, and this association was also similar for participants with prehypertension and those with normal clinic BP.
In our study, masked nighttime hypertension, but not masked daytime or masked 24-hour hypertension, was associated with incident clinic hypertension among those with normal clinic BP. Prior studies have shown that compared to Whites, AAs have a higher prevalence of nighttime hypertension.36–38 The underlying mechanisms linking nighttime hypertension to incident clinic hypertension in AAs are unknown. Psychosocial stress, sleep apnea as well as biological factors such as arterial stiffness, inflammation, endothelial dysfunction, and salt sensitivity may be possible mechanisms.39–42 Future studies should examine the factors linking masked nighttime hypertension to incident clinic hypertension among AAs.
Given the substantial morbidity and mortality associated with hypertension, earlier identification of individuals at a high risk for developing hypertension is of paramount importance. The results of our study suggest that the identification of masked hypertension among individuals with non-elevated clinic BP using ABPM may identify those at highest risk for incident clinic hypertension. Previous studies15,16,26,43,44 have demonstrated that lifestyle modification and pharmacological therapy may delay the onset of hypertension among high-risk individuals including those with prehypertension. These preventive strategies may prove to be most effective for not only the subset of individuals with prehypertension who have masked hypertension but also for those individuals with normal CBP and masked hypertension. Furthermore, in the current study, 11.1% of participants had LVH at baseline. Diaz et al.4 previously demonstrated that among JHS participants, masked hypertension was associated with increased LVMI. Given the increased CVD risk associated with LVH45, individuals with masked hypertension and LVH may represent a high-risk group that might benefit from antihypertensive medication initiation prior to the development of clinic hypertension. Randomized trials are needed to determine whether lifestyle modification and pharmacological therapy delay hypertension onset and reverse cardiovascular end-organ damage among individuals with masked hypertension.
There are several strengths of the current study. We used data from a population-based sample comprised entirely of AAs. There have been few prior investigations of ABPM among AAs,4,46 and this population has a high risk for masked hypertension4 and incident clinic hypertension.12 Also, given the broad data collection in the JHS, we were able to control for multiple potential confounders. We were also able to examine several types of masked hypertension including masked daytime, nighttime, and 24-hour hypertension, as well as determine the risk of incident clinic hypertension stratified by prehypertension status. In addition to ABPM not being conducted at a follow-up visit in the JHS, there were also other possible limitations. Only a sub-sample of JHS participants had ABPM performed at the baseline visit. Information regarding napping during the daytime period and awakening during the nighttime period, which may impact estimates of daytime and nighttime BP, was not collected. In addition, the JHS did not conduct home BP monitoring (HBPM), another out-of-clinic approach for measuring BP, which also can be used to determine masked hypertension. Some evidence suggests that many individuals have masked hypertension on either ABPM or HBPM, but not on both.47 Therefore, masked hypertension on ABPM vs. HBPM may represent different out-of-clinic BP phenotypes. We were unable to assess the association of masked hypertension on HBPM and incident hypertension within the JHS.
Perspectives
Among AAs with non-elevated clinic BP and who were not taking antihypertensive medication, masked hypertension was associated with an increased risk for the development of clinic hypertension. The association between any masked hypertension and incident clinic hypertension was present after adjustment for clinic BP, and was similar among participants with prehypertension and normal clinic BP. Also, daytime, nighttime and 24-hour masked hypertension was each associated with incident clinic hypertension. The results of the current study suggest that among AA adults with non-elevated clinic BP, ABPM can identify those who are at increased risk for developing clinic hypertension.
Supplementary Material
Novelty and Significance.
What is New?
We examined the associations of masked hypertension and its subtypes (masked daytime, nighttime, and 24-hour hypertension) with incident clinic hypertension among a population-based cohort of AAs.
We also evaluated whether these associations were independent of clinic BP level and consistent for those with prehypertension and, separately, normal clinic BP.
What is Relevant?
It has been hypothesized that masked hypertension represents an intermediate phenotype between normotension and hypertension.
Few population-based studies have examined the association between masked hypertension and incident hypertension, and none have examined this association in AAs, who have a high prevalence of masked hypertension.
Summary
Among a large population-based cohort study of AAs with non-elevated clinic blood pressure, participants with any masked hypertension had twice the risk of incident clinic hypertension compared to participants without masked hypertension over an 8 year follow up period.
Among participants with either prehypertension or normal clinic BP, masked hypertension was associated with increased risk of incident clinic hypertension.
Acknowledgments
The authors would like to thank the Jackson Heart Study participants, investigators, and staff for their valuable contributions and long-term commitment to the study.
Funding Sources
The Jackson Heart Study is supported and conducted in collaboration with Jackson State University (N01-HC-95170); University of Mississippi Medical Center (N01-HC-95171); and Touglaoo College (N01-HC-95172) and contracts HHSN268201300046C, HHSN268201300047C, HHSN268201300048C, HHSN268201300049C, HHSN268201300050C from the National Heart, Lung, and Blood Institute (NHLBI) and the National Institute on Minority Health and Health Disparities (NIMHD) at the National Institutes of Health (NIH). This work was also supported by the NIH (HL047540, HL117323, HL117323-02S2, K24-HL125704) from the NHLBI, Bethesda, MD.
Footnotes
Disclosures: Dr. Paul Muntner received an institutional grant from Amgen Inc. Other author disclosures: None.
References
- 1.Pickering TG, Shimbo D, Haas D. Ambulatory blood-pressure monitoring. N Engl J Med. 2006;354:2368–2374. doi: 10.1056/NEJMra060433. [DOI] [PubMed] [Google Scholar]
- 2.Pickering TG, Davidson K, Gerin W, Schwartz JE. Masked hypertension. Hypertension. 2002;40:795–796. doi: 10.1161/01.hyp.0000038733.08436.98. [DOI] [PubMed] [Google Scholar]
- 3.Cuspidi C, Sala C, Tadic M, Rescaldani M, Grassi G, Mancia G. Untreated Masked Hypertension and Subclinical Cardiac Damage: A Systematic Review and Meta-analysis. Am J Hypertens. 2015;28:806–813. doi: 10.1093/ajh/hpu231. [DOI] [PubMed] [Google Scholar]
- 4.Diaz KM, Veerabhadrappa P, Brown MD, Whited MC, Dubbert PM, Hickson DA. Prevalence, Determinants, and Clinical Significance of Masked Hypertension in a Population-Based Sample of African Americans: The Jackson Heart Study. Am J Hypertens. 2015;28:900–908. doi: 10.1093/ajh/hpu241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hansen TW, Kikuya M, Thijs L, Björklund-Bodegård K, Kuznetsova T, Ohkubo T, Richart T, Torp-Pedersen C, Lind L, Jeppesen J, Ibsen H, Imai Y, Staessen JA IDACO Investigators. Prognostic superiority of daytime ambulatory over conventional blood pressure in four populations: a meta-analysis of 7,030 individuals. J Hypertens. 2007;25:1554–1564. doi: 10.1097/HJH.0b013e3281c49da5. [DOI] [PubMed] [Google Scholar]
- 6.Ohkubo T, Kikuya M, Metoki H, Asayama K, Obara T, Hashimoto J, Totsune K, Hoshi H, Satoh H, Imai Y. Prognosis of “masked” hypertension and “white-coat” hypertension detected by 24-h ambulatory blood pressure monitoring 10-year follow-up from the Ohasama study. J Am Coll Cardiol. 2005;46:508–515. doi: 10.1016/j.jacc.2005.03.070. [DOI] [PubMed] [Google Scholar]
- 7.Pierdomenico SD, Pannarale G, Rabbia F, Lapenna D, Licitra R, Zito M, Campanella M, Gaudio C, Veglio F, Cuccurullo F. Prognostic relevance of masked hypertension in subjects with prehypertension. Am J Hypertens. 2008;21:879–883. doi: 10.1038/ajh.2008.196. [DOI] [PubMed] [Google Scholar]
- 8.Verberk WJ, Kessels AG, de Leeuw PW. Prevalence, causes, and consequences of masked hypertension: a meta-analysis. Am J Hypertens. 2008;21:969–975. doi: 10.1038/ajh.2008.221. [DOI] [PubMed] [Google Scholar]
- 9.Pickering TG. The natural history of hypertension: prehypertension or masked hypertension? J Clin Hypertens (Greenwich) 2007;9:807–810. doi: 10.1111/j.1751-7176.2007.tb00011.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pickering TG, Gerin W, Schwartz JE, Spruill TM, Davidson KW. Franz Volhard lecture: should doctors still measure blood pressure? The missing patients with masked hypertension. J Hypertens. 2008;26:2259–2267. doi: 10.1097/HJH.0b013e32831313c4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Palatini P, Winnicki M, Santonastaso M, Mos L, Longo D, Zaetta V, Dal Follo M, Biasion T, Pessina AC. Prevalence and clinical significance of isolated ambulatory hypertension in young subjects screened for stage 1 hypertension. Hypertension. 2004;44:170–174. doi: 10.1161/01.HYP.0000135250.57004.19. [DOI] [PubMed] [Google Scholar]
- 12.Muntner P, Woodward M, Mann DM, Shimbo D, Michos ED, Blumenthal RS, Carson AP, Chen H, Arnett DK. Comparison of the Framingham Heart Study hypertension model with blood pressure alone in the prediction of risk of hypertension: the Multi-Ethnic Study of Atherosclerosis. Hypertension. 2010;55:1339–1345. doi: 10.1161/HYPERTENSIONAHA.109.149609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Hypertension Prevention Trial: three-year effects of dietary changes on blood pressure. Hypertension Prevention Trial Research Group. Arch Intern Med. 1990;150:153–162. [PubMed] [Google Scholar]
- 14.Dickey RA, Janick JJ. Lifestyle modifications in the prevention and treatment of hypertension. Endocr Pract. 2001;7:392–399. doi: 10.4158/EP.7.5.392. [DOI] [PubMed] [Google Scholar]
- 15.Julius S, Nesbitt SD, Egan BM, Weber MA, Michelson EL, Kaciroti N, Black HR, Grimm RH, Jr, Messerli FH, Oparil S, Schork MA Trial of Preventing Hypertension (TROPHY) Study Investigators. Feasibility of treating prehypertension with an angiotensin-receptor blocker. N Engl J Med. 2006;354:1685–1697. doi: 10.1056/NEJMoa060838. [DOI] [PubMed] [Google Scholar]
- 16.Luders S, Schrader J, Berger J, Unger T, Zidek W, Böhm M, Middeke M, Motz W, Lübcke C, Gansz A, Brokamp L, Schmieder RE, Trenkwalder P, Haller H, Dominiak P PHARAO Study Group. The PHARAO study: prevention of hypertension with the angiotensin-converting enzyme inhibitor ramipril in patients with high-normal blood pressure: a prospective, randomized, controlled prevention trial of the German Hypertension League. J Hypertens. 2008;26:1487–1496. doi: 10.1097/HJH.0b013e3282ff8864. [DOI] [PubMed] [Google Scholar]
- 17.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, 3rd, Simons-Morton DG, Karanja N, Lin PH DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 18.Taylor HA., Jr The Jackson Heart Study: an overview. Ethn Dis. 2005;15:S6-1-3. [PubMed] [Google Scholar]
- 19.Taylor HA, Jr, Wilson JG, Jones DW, Sarpong DF, Srinivasan A, Garrison RJ, Nelson C, Wyatt SB, Adeyemo A, Zhou J, Taylor HA, Jr, Jaquish C. Toward resolution of cardiovascular health disparities in African Americans: design and methods of the Jackson Heart Study. Ethn Dis. 2005;15:S6-4-17. [PubMed] [Google Scholar]
- 20.Wilson JG, Rotimi CN, Ekunwe L, Royal CD, Crump ME, Wyatt SB, Steffes MW. Study design for genetic analysis in the Jackson Heart Study. Ethn Dis. 2005;15:S6-30-37. [PubMed] [Google Scholar]
- 21.Thijs L, Hansen TW, Kikuya M, et al. The International Database of Ambulatory Blood Pressure in relation to Cardiovascular Outcome (IDACO): protocol and research perspectives. Blood Press Monit. 2007;12:255–262. doi: 10.1097/mbp.0b013e3280f813bc. [DOI] [PubMed] [Google Scholar]
- 22.Carpenter MA, Crow R, Steffes M, Rock W, Heilbraun J, Evans G, Skelton T, Jensen R, Sarpong D. Laboratory, reading center, and coordinating center data management methods in the Jackson Heart Study. Am J Med Sci. 2004;328:131–144. doi: 10.1097/00000441-200409000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the american society of echocardiography and the European association of cardiovascular imaging. J Am Soc Echocardiogr. 2015;28:1–39. e14. doi: 10.1016/j.echo.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 24.Finkelstein DM. A proportional hazards model for interval-censored failure time data. Biometrics. 1986;42:845–854. [PubMed] [Google Scholar]
- 25.Parikh NI, Pencina MJ, Wang TJ, Benjamin EJ, Lanier KJ, Levy D, D’Agostino RB, Sr, Kannel WB, Vasan RS. A risk score for predicting near-term incidence of hypertension: the Framingham Heart Study. Ann Intern Med. 2008;148:102–110. doi: 10.7326/0003-4819-148-2-200801150-00005. [DOI] [PubMed] [Google Scholar]
- 26.Egan BM, Stevens-Fabry S. Prehypertension--prevalence, health risks, and management strategies. Nat Rev Cardiol. 2015;12:289–300. doi: 10.1038/nrcardio.2015.17. [DOI] [PubMed] [Google Scholar]
- 27.Leitschuh M, Cupples LA, Kannel W, Gagnon D, Chobanian A. High-normal blood pressure progression to hypertension in the Framingham Heart Study. Hypertension. 1991;17:22–27. doi: 10.1161/01.hyp.17.1.22. [DOI] [PubMed] [Google Scholar]
- 28.Selassie A, Wagner CS, Laken ML, Ferguson ML, Ferdinand KC, Egan BM. Progression is accelerated from prehypertension to hypertension in blacks. Hypertension. 2011;58:579–587. doi: 10.1161/HYPERTENSIONAHA.111.177410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet. 2001;358:1682–1686. doi: 10.1016/S0140-6736(01)06710-1. [DOI] [PubMed] [Google Scholar]
- 30.Shimbo D, Newman JD, Schwartz JE. Masked hypertension and prehypertension: diagnostic overlap and interrelationships with left ventricular mass: the Masked Hypertension Study. Am J Hypertens. 2012;25:664–671. doi: 10.1038/ajh.2012.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lurbe E, Torro I, Alvarez V, Nawrot T, Paya R, Redon J, Staessen JA. Prevalence, persistence, and clinical significance of masked hypertension in youth. Hypertension. 2005;45:493–498. doi: 10.1161/01.HYP.0000160320.39303.ab. [DOI] [PubMed] [Google Scholar]
- 32.Mancia G, Bombelli M, Facchetti R, Madotto F, Quarti-Trevano F, Polo Friz H, Grassi G, Sega R. Long-term risk of sustained hypertension in white-coat or masked hypertension. Hypertension. 2009;54:226–232. doi: 10.1161/HYPERTENSIONAHA.109.129882. [DOI] [PubMed] [Google Scholar]
- 33.Trudel X, Milot A, Brisson C. Persistence and progression of masked hypertension: a 5-year prospective study. Int J Hypertens. 2013;2013:836387. doi: 10.1155/2013/836387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ishikawa J, Ishikawa Y, Edmondson D, Pickering TG, Schwartz JE. Age and the difference between awake ambulatory blood pressure and office blood pressure: a meta-analysis. Blood Press Monit. 2011;16:159–167. doi: 10.1097/MBP.0b013e328346d603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Brien E, Murphy J, Tyndall A, Atkins N, Mee F, McCarthy G, Staessen J, Cox J, O’Malley K. Twenty-four-hour ambulatory blood pressure in men and women aged 17 to 80 years: the Allied Irish Bank Study. J Hypertens. 1991;9:355–360. doi: 10.1097/00004872-199104000-00007. [DOI] [PubMed] [Google Scholar]
- 36.Muntner P, Lewis CE, Diaz KM, Carson AP, Kim Y, Calhoun D, Yano Y, Viera AJ, Shimbo D. Racial differences in abnormal ambulatory blood pressure monitoring measures: Results from the Coronary Artery Risk Development in Young Adults (CARDIA) study. Am J Hypertens. 2015;28:640–648. doi: 10.1093/ajh/hpu193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Profant J, Dimsdale JE. Race and diurnal blood pressure patterns. A review and meta-analysis. Hypertension. 1999;33:1099–1104. doi: 10.1161/01.hyp.33.5.1099. [DOI] [PubMed] [Google Scholar]
- 38.Wang X, Poole JC, Treiber FA, Harshfield GA, Hanevold CD, Snieder H. Ethnic and gender differences in ambulatory blood pressure trajectories: results from a 15-year longitudinal study in youth and young adults. Circulation. 2006;114:2780–2787. doi: 10.1161/CIRCULATIONAHA.106.643940. [DOI] [PubMed] [Google Scholar]
- 39.Harshfield GA, Pulliam DA, Alpert BS, Stapleton FB, Willey ES, Somes GW. Ambulatory blood pressure patterns in children and adolescents: influence of renin-sodium profiles. Pediatrics. 1991;87:94–100. [PubMed] [Google Scholar]
- 40.Reimann M, Hamer M, Schlaich MP, Malan NT, Ruediger H, Ziemssen T, Malan L. Greater cardiovascular reactivity to a cold stimulus is due to higher cold pain perception in black Africans: the Sympathetic Activity and Ambulatory Blood Pressure in Africans (SABPA) study. J Hypertens. 2012;30:2416–2424. doi: 10.1097/HJH.0b013e328358faf7. [DOI] [PubMed] [Google Scholar]
- 41.van Lill L, Malan L, van Rooyen J, Steyn F, Reimann M, Ziemssen T. Baroreceptor sensitivity, cardiovascular responses and ECG left ventricular hypertrophy in men: the SABPA study. Blood Press. 2011;20:355–361. doi: 10.3109/08037051.2011.580529. [DOI] [PubMed] [Google Scholar]
- 42.Wilson DK, Sica DA, Miller SB. Ambulatory blood pressure nondipping status in salt-sensitive and salt-resistant black adolescents. Am J Hypertens. 1999;12:159–165. doi: 10.1016/s0895-7061(98)00234-9. [DOI] [PubMed] [Google Scholar]
- 43.Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure. The Trials of Hypertension Prevention, phase II. The Trials of Hypertension Prevention Collaborative Research Group. Arch Intern Med. 1997;157:657–667. [PubMed] [Google Scholar]
- 44.Stevens VJ, Corrigan SA, Obarzanek E, Bernauer E, Cook NR, Hebert P, Mattfeldt-Beman M, Oberman A, Sugars C, Dalcin AT, Whelton PK. Weight loss intervention in phase 1 of the Trials of Hypertension Prevention. The TOHP Collaborative Research Group. Arch Intern Med. 1993;153:849–858. [PubMed] [Google Scholar]
- 45.Bombelli M, Facchetti R, Carugo S, Madotto F, Arenare F, Quarti-Trevano F, Capra A, Giannattasio C, Dell’Oro R, Grassi G, Sega R, Mancia G. Left ventricular hypertrophy increases cardiovascular risk independently of in-office and out-of-office blood pressure values. J Hypertens. 2009;27:2458–2464. doi: 10.1097/HJH.0b013e328330b845. [DOI] [PubMed] [Google Scholar]
- 46.Larsen TR, Gelaye A, Waanbah B, Assad H, Daloul Y, Williams F, Williams M, Steigerwalt S. Prevalence of masked hypertension in African Americans. J Clin Hypertens (Greenwich) 2014;16:801–804. doi: 10.1111/jch.12418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stergiou GS, Salgami EV, Tzamouranis DG, Roussias LG. Masked hypertension assessed by ambulatory blood pressure versus home blood pressure monitoring: is it the same phenomenon? Am J Hypertens. 2005;18:772–778. doi: 10.1016/j.amjhyper.2005.01.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.