Abstract
Pretransplant alpha-fetoprotein (AFP) is a useful tumor marker predicting recurrence of hepatocellular carcinoma (HCC). Little is known, however, about the relationship between changes in AFP concentration and prognosis. This study investigated the clinical significance of change in peri-transplant AFP level as a predictor of HCC recurrence. Data from 125 HCC patients with elevated pretransplant AFP level who underwent liver transplantation (LT) between February 2000 and December 2010 were retrospectively reviewed. Patients with AFP normalization within 1 month after LT were classified into the rapid normalization group (n = 97), with all other patients classified into the non-rapid normalization group (n = 28). Tumor recurrence was observed in 17 of the 97 patients (17.5%) with rapid normalization; of these, 11 patients had high AFP levels and six had normal levels at recurrence. In contrast, tumor recurrence was observed in 24 of the 28 patients (85.7%) without rapid normalization, with all 24 having high AFP levels at recurrence. Multivariate analysis showed that non-rapid normalization (harzard ratio [HR], 4.41, P < 0.001), sex (HR, 3.26, P = 0.03), tumor size (HR, 1.15, P = 0.001), and microvascular invasion (HR, 2.65, P = 0.005) were independent risk factors for recurrence. In conclusion, rapid normalization of post-LT AFP level at 1 month is a useful clinical marker for HCC recurrence. Therefore, an adjuvant strategy and/or intensive screening are needed for patients who do not show rapid normalization.
Keywords: Alpha-Fetoprotein, Tumor Marker, Liver Cancer, Hepatocellular Carcinoma, Liver Transplantation
INTRODUCTION
Alpha-fetoprotein (AFP) is a serum tumor marker for hepatocellular carcinoma (HCC) and can also be used to monitor HCC recurrence after liver transplantation (LT). Although AFP can be slightly elevated in several other conditions, such as chronic hepatitis and liver cirrhosis (1,2), high preoperative levels of AFP are associated with poorer outcomes following liver transplantation for HCC (3,4,5). Recently, the significance of AFP decline after curative resection for HCC has been reported as a predictor of tumor recurrence (6,7). Nobuoka et al. (7) emphasized that a positive level of AFP within 4 months after resection was a strong predictor of post-operative tumor recurrence. Little is known, however, about the relationship between peri-operative change in AFP level and tumor recurrence or the clinical usefulness of peri-operative change as an early marker of HCC recurrence. Based on the studies in resection, we hypothesized that a rapid decline in AFP may be associated with better recurrence-free survival (RFS) in patients who have undergone LT.
This study, therefore, evaluated the clinical significance of change in peri-transplant serum AFP level as a predictor of tumor recurrence in HCC patients who underwent liver transplantation.
MATERIALS AND METHODS
Patients
Data were retrospectively collected from 242 patients with pathologically diagnosed HCC who underwent liver transplantation between February 2000 and December 2010 at Seoul National University Hospital, Seoul, Korea. Of these 242 patients, 136 (56.1%) had elevated AFP levels (> 20 ng/mL) before liver transplantation, but 11 were excluded because of lack of peri-operative AFP data. Thus, 125 patients were enrolled in this study. Immunosuppression consisted of basilixmab induction and maintenance of calcineurin inhibitor and steroid. Mycophenolate mofetil was employed in cases of side effects from calcineurin inhibitors or renal impairment. The corticosteroid was tapered to discontinuation by 6 months after LT.
AFP measurement
Serum AFP concentrations were measured using an enzyme-linked immunoassay, with normal AFP concentration defined as below 20 ng/mL. AFP concentrations were measured within one month before liver transplantation; every month after LT (1-6 months); and at the time of tumor recurrence.
Grouping based on AFP changes after LT
The 125 patients with elevated pre-transplant AFP were stratified into two groups based on the lowest post-transplant AFP concentration: a normalization group and a persistently elevated group. Patients in the normalization group were divided into two subgroups, a rapid normalization group (Group R), defined as those with normalized AFP within 1 month after LT, and a slow normalization group, defined as those with normalized AFP within 1-3 months. Since recurrence outcomes were comparable in patients with persistently elevated AFP and those with slow normalization, these two groups were combined into a non-rapid normalization group (Group NR).
Follow-up protocol and definition of recurrence
After discharge, AFP was measured monthly. Imaging workup (liver CT ± chest CT and bone scan) was performed every 3-6 months, depending on the risk of recurrence, for 3 years and annually thereafter. Recurrence was defined as the appearance of a new HCC lesion on radiological examination.
Statistical analysis
Recurrenc-free survival was calculated using the Kaplan-Meier method, with between group comparisons using log-rank analysis. Multivariate Cox’s proportional hazard regression with forward stepwise technique was used to determine the effect of all potential variables. Demographics and clinicopathologic characteristics of the patients were compared between groups using Student’s t test for continuous variables and contingency table analysis (χ2 test or Fisher exact test, as appropriate) for categorical variables. All statistical analyses were performed using SPSS version 18 for Windows (SPSS Inc., Chicago, IL, USA). All tests were two sided, with a P value < 0.05 considered statistically significant.
Ethics statement
This study was approved by the institutional review board of Seoul National University Hospital (IRB No. 1409-042-608). Informed consent was waived by the board.
RESULTS
Distribution of patients and RFS according to peri-transplant changes in AFP
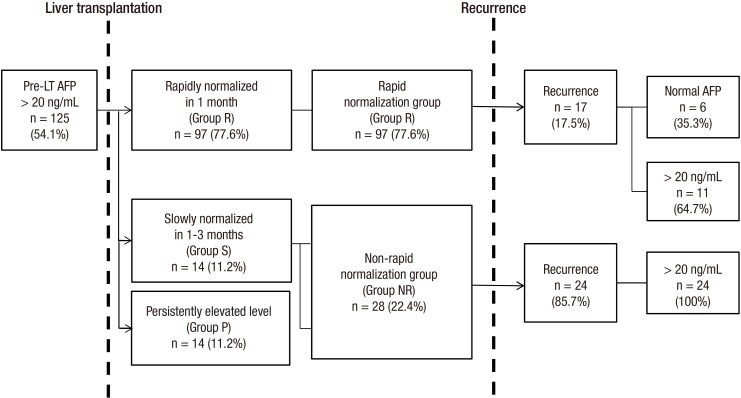
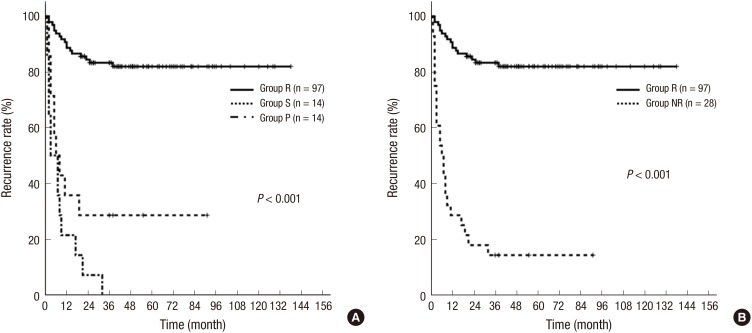
Fig. 1 shows the patient distribution according to peri-transplant AFP levels. Of the 125 patients with elevated pre-LT AFP concentrations, 111 (88.8%) had normalized post-LT AFP, whereas 14 (11.2%) had elevated post-LT AFP. Patients with normalized post-LT AFP had significantly higher 2-year RFS rates than patients with persistently elevated post-transplant AFP (89.6% vs. 20.8%, P < 0.001). Of the 111 patients who showed normalization of AFP, 97 showed rapid normalization and 14 showed slow normalization. The 2-year RFS rate was significantly higher in patients with rapid than slow normalization (83.3% vs. 30%, P < 0.001) (Fig. 2A). Since the slow normalization subgroup and patients with persistently elevated AFP had similar 2-year RFS rates, they were combined into Group NR. The two-year RFS rate was significantly greater in Group R than Group NR (83.3% vs. 13.4%, P < 0.001) (Fig. 2B). Analysis of AFP in the 41 patients with tumor recurrence showed that six (14.7%) had normal AFP at recurrence.
Fig. 1.
Patient distribution according to peri-transplant AFP concentrations in HCC patients with elevated pre-transplant AFP level. (n = 125)
Fig. 2.
Recurrence-free survival according to change in post-transplant AFP level in HCC patients with elevated pre-transplant AFP levels. (A) RFS rates are higher in patients with rapid normalization of AFP within 1 month (Group R) than in patients with slow normalization of AFP within 1-3 months (Group S) or in patients with persistently elevated AFP level (Group P). (B) RFS rates were higher in Group R than in patients with non-rapid normalization of AFP level (Group R).
Demographics
Of the 125 patients, 97 (77.6%) were men and 28 (22.4%) were women; their mean age was 54.3 years (range, 27–82 years). The most common underlying diseases were virus-related cirrhosis (HBV, 74.5%; HCV, 2.3%). According to the Child-Pugh classification of cirrhosis, 27 (21.6%), 66 (52.8%) and 32 (24.6%) patients were Child-Pugh classes C, B, and A, respectively. Table 1 shows the demographic and clinical characteristics in patients with rapid and non-rapid normalization of AFP. Comparisons showed that pre-LT AFP concentration (P < 0.001), tumor size (P = 0.006), tumor number (P < 0.001), Edmondson-Steiner grade (P = 0.07), and microvascular invasion (P < 0.001) differed significantly between these two groups.
Table 1. Clinicopathological factors in HCC patients with elevated pre-transplant AFP levels and rapid or non-rapid normalization of post-LT AFP.
| Factors | Subgroups | Rapid normalization (n = 97) | Non-rapid normalization (n = 28) | P value |
|---|---|---|---|---|
| Sex | Male/Female | 75/22 | 22/6 | 0.78 |
| Age, yr (Mean) | 54.2 | 54.4 | 0.85 | |
| Cause of cirrhosis | Virus/Others | 85/12 | 11/3 | 0.34 |
| Child | A/B/C | 26/52/19 | 6/14/8 | 0.11 |
| MELD score (Mean) | 16.9 | 17 | 0.62 | |
| AFP before LT, ng/mL (Mean) | 298 | 459 | < 0.001 | |
| Pretreatment | No treatment | 17 | 10 | 0.21 |
| Locoregional treatment | 80 | 18 | 0.22 | |
| Size, cm (Mean) | 3.4 | 5.5 | 0.006 | |
| No. (Mean) | 2.7 | 3.3 | 0.001 | |
| Edmonson-Steiner grade | (I, II)/(III, IV) | 41/56 | 5/23 | 0.07 |
| Microvascular invasion (No.) | (+) | 21 | 16 | < 0.001 |
MELD, model for End-stage liver disease.
Risk factors for HCC recurrence after LT
Univariate analysis showed that sex, pre-LT AFP (> 200 ng/mL), non-rapid AFP normalization, tumor size, tumor number, Edmonson-Steiner grade and the presence of microvascular invasion were risk factors for HCC recurrence (Table 2). Multivariate analysis showed that non-rapid AFP normalization (hazard ratio [HR], 4.41; 95% Confidence intervals [95% CI], 2.01-6.72, P < 0.001), male sex (HR, 3.26; 95% CI, 1.12-9.57, P = 0.03), tumor size > 7 cm (HR, 1.15; 95% CI, 1.04-1.26, P = 0.001), and the presence of microvascular invasion (HR, 2.65; 95% CI, 1.33-5.26, P = 0.005) were significant independent risk factors for HCC recurrence (Table 2).
Table 2. Risk factors in HCC patients with elevated pre-transplant AFP levels in univariate and multivariate analysis.
| Factors | Subgroups | No. | HR (95% CI) | P value (Univariate) | P value (Multivariate) |
|---|---|---|---|---|---|
| Sex | Male | 97 | 3.26 (1.12-9.57) | 0.01 | 0.03 |
| Female | 28 | Ref. | |||
| Age, yr | > 50 | 43 | 0.34 | ||
| ≤ 50 | 82 | ||||
| Cause of cirrhosis | Virus | 112 | 0.95 | ||
| Others | 13 | ||||
| Child | A/B | 94 | 0.32 | ||
| C | 31 | ||||
| MELD | > 20 | 39 | 0.25 | ||
| ≤ 20 | 96 | ||||
| Pre-transplant AFP, ng/mL | > 200 | 49 | 0.01 | ||
| ≤ 200 | 76 | ||||
| Post-transplant AFP, ng/mL | Non-rapid normalization | 28 | 4.41 (2.01-6.72) | < 0.001 | < 0.001 |
| Rapid normalization | 97 | Ref. | |||
| Pretreatment (Locoregional treatment) | (+) | 98 | 0.25 | ||
| (-) | 27 | ||||
| Tumor size, cm | > 7 | 111 | 1.15 (1.04-1.26) | 0.001 | 0.001 |
| ≤ 7 | 14 | Ref. | |||
| Tumor No. | > 5 | 12 | 0.001 | ||
| ≤ 5 | 113 | ||||
| Edmonson-Steiner grade | III, IV | 79 | < 0.001 | ||
| I, II | 46 | ||||
| Microvascular invasion | (+) | 37 | 2.65 (1.33-5.26) | < 0.001 | 0.005 |
| (-) | 88 | Ref. |
MELD, model for End-stage liver disease.
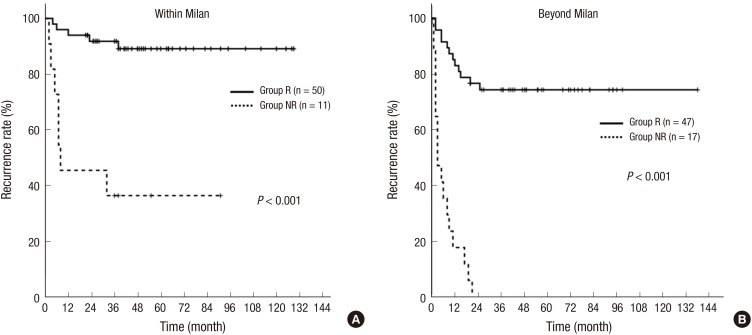
Recurrences in patients with and without rapid AFP normalization according to the Milan criteria
The significance of post-LT AFP concentration was further evaluated in patients with and without rapid AFP normalization by comparing RFS rate in these two groups according to the Milan criteria (Fig. 3). Even in patients who fulfilled the Milan criteria, those without rapid normalization had relatively poor outcomes, with a 2-year RFS rate of 45.5% (Fig. 3A). In comparison, patients with rapid normalization of AFP who exceeded the Milan criteria, but had acceptable outcomes, had a 2-year RFS rate of 74.3% (Fig. 3B).
Fig. 3.
Recurrence-free survival according to post-transplant AFP levels in HCC patients within (A) or beyond (B) the Milan criteria. (Group R; patients with rapid normalization of AFP level within 1 month after LT; Group NR, patients with non-rapid normalization of AFP)
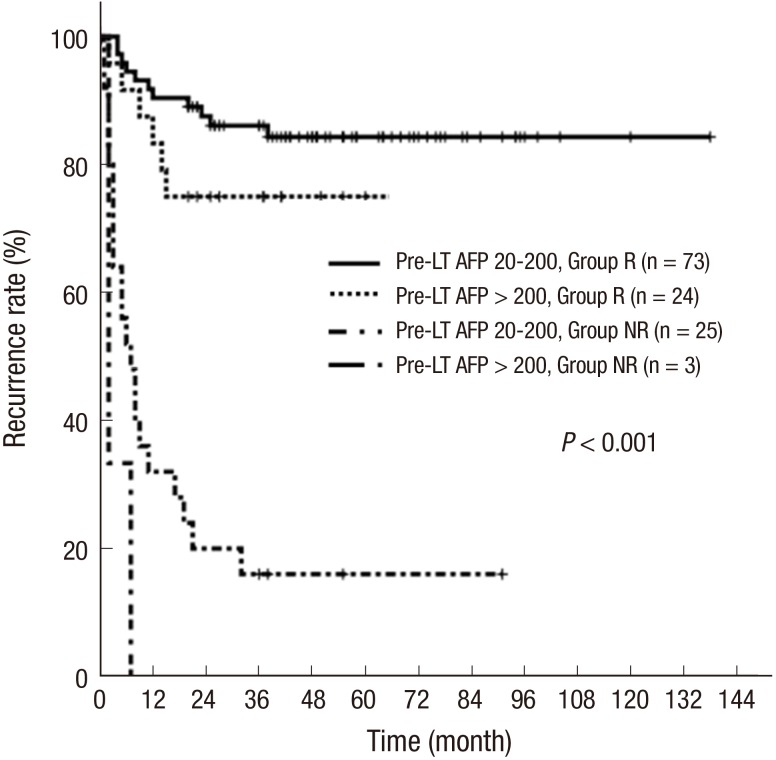
Recurrence based on pre-LT AFP level
Because the degree of pre-LT AFP level itself can affect recurrence, patients were further divided into two groups, those with highly (> 200 ng/mL) and moderately (< 200 ng/mL) elevated pre-LT AFP concentration, with each subdivided by their peri-transplant changes in AFP (Fig. 4). A comparison of RFS rates in these four groups showed that RFS rate was highest in patients with moderately elevated pre-transplant AFP and rapid post-transplant normalization, although patients with high elevated pre-transplant and rapid transplant normalization had similarly good outcomes. Patients with non-rapid normalization showed poor outcomes, regardless of the degree of elevation of pre-LT AFP.
Fig. 4.
Recurrence-free survival according to the combination of degree of pre-transplant AFP level and peri-transplant AFP changes. RFS rates were highest in patients with rapid normalization of post-transplant AFP and moderately elevated pre-LT AFP, although outcomes were also good in patients with rapid normalization of post-transplant AFP and highly elevated pre-LT AFP. Patients without rapid normalization of post-LT AFP showed poor outcomes, regardless of the degree of pre-LT AFP. (Group R, patients with rapid normalization of AFP level within 1 month; Group NR, patients with non-rapid normalization of AFP)
DISCUSSION
Liver transplantation has been shown to be the best therapeutic option in selected patients with HCC. Although transplants are usually performed in patients who meet the Milan criteria, a substantial subset of patients who do not meet these criteria have the potential for good outcomes after liver transplantation, leading to the proposal of several new criteria (3,8). These latter criteria emphasize the importance of the inclusion of new markers of biological behavior, along with morphological tumor size and number, in formulating new sets of criteria that can better predict the risk of recurrence. AFP is one of strong biological markers and used for early diagnosis of HCC and for recurrence after LT. Numerous study groups have emphasized that high preoperative levels of AFP are associated with poorer outcomes from liver transplantation for HCC (6,7). To date, however, few studies have assessed the significance of peri-operative changes in AFP in patients who have undergone LT for HCC (9).
Several studies have analyzed the significance of AFP increase after curative resection for HCC as a predictor of tumor recurrence. For example, one study evaluating minimum postoperative AFP concentration within four months in 165 HCC patients who had undergone hepatectomy found that, among patients with high preoperative AFP, those without normalized postoperative AFP were more likely to experience tumor recurrence (48/60, 80.0% vs. 4/23, 17.4%, P < 0.001) (7). In addition, a study of three tumor markers (AFP, AFP-L3, and DCP) before and after HCC resection found decreased levels after surgery to be a strong predictor of overall survival and increased levels to be connected with higher rates of tumor recurrence (6).
Based on these findings in patients resected for HCC, we hypothesized that a rapid decline in AFP may be associated with better RFS in patients who have undergone LT. In this study, we found that AFP changing pattern was similarly important to predict the HCC recurrence in LT setting. Pre-LT high AFP is an important risk factor for HCC recurrence and has therefore been included in the selection criteria for resection of HCC (10,11,12). However, we found that rapid normalization of AFP within one month was associated with good prognosis, even in patients with very high pre-LT AFP. Rapid normalization of AFP regardless of the degree of pre-transplant AFP level was important feature to predict low recurrence rate after LT. Even though the pre-transplant AFP level was high, which has been known as strong predictor of recurrence after LT, if AFP became normalized until 1 month, low recurrence can be expected. On the contrary, if AFP level was not normalized until 1 month, there was high chance of recurrence regardless of degree of pre-transplant level. Although pre-LT AFP concentration is an important factor in the preoperative assessment of risk of recurrence, the speed of AFP reduction is more important in assessing the risk of recurrence after LT. Therefore, if AFP level was not normalized until 1 month, adjuvant strategy such as m-TOR inhibitor or adjuvant chemotherapy and intensive screening should be considered regardless of pre-LT AFP level.
The similar conclusion was reported in a previous study, although that study found that normalization within two months was predictive of RFS (9). That study measured AFP concentrations at two post-LT time points, two weeks and two months, whereas our study measured AFP at several time points, ranging from one to six months. Moreover, using these values, the sensitivity and specificity of AFP was assessed by receiver operating characteristic (ROC) curve. The areas under the receiver operating characteristic curve (AUROC) was for AFP was 0.79 (95% CI, 0.76–0.81) and the optimal cutoff point of sensitivity and specificity was the time at 1 month after LT.
In this study, we found that the 2-year RFS rate was only 61% in the 102 patients who showed normalization of AFP within two months after LT, but was 83.3% in the 97 patients who showed normalization of AFP within one month after LT. Therefore, these findings suggest that the one month time point is an important cut off for prediction of recurrence after LT. There can be concerns that considering the 5-7 days of half-life of AFP (13), one month may be short to be normalized, especially in cases with high pre-transplant AFP level. However, we found that AFP higher than 200 ng/mL became normalized in most cases (24/27) within 1 month even in cases with very high AFP level.
This study had several limitations, including its retrospective design and the relatively long period of patient inclusion (11 years). Due to advances in surgical techniques and chemotherapy, there may be an element of lead time bias, in that patients treated more recently may have better survival and recurrence rates due to greater experience, better prior therapy and better supportive care.
In conclusion, change in peri-transplant AFP (rapid vs. non-rapid normalization) is significantly prognostic of tumor recurrence after liver transplantation for HCC in patients with elevated pre-LT AFP level. Rapid normalization within 1 month after LT was associated with a significantly higher RFS rate, regardless of pre-LT AFP level. An adjuvant strategy and/or intensive screening may be necessary, however, if AFP does not return to normal within one month after LT.
Footnotes
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Substantial contributions to the conception or design of the work: Yoo T, Lee KW. Acquisition, analysis, or interpretation of data for the work: Yoo T, Lee KW, Choi YR, Kim H, Suh SW, Jeong JH, Lee JM. Drafting the work or revising it critically for important intellectual content: Yi NJ, Suh KS. Agreement to be accountable for all aspects of the work and submission of manuscript: all authors.
References
- 1.Debruyne EN, Delanghe JR. Diagnosing and monitoring hepatocellular carcinoma with alpha-fetoprotein: new aspects and applications. Clin Chim Acta. 2008;395:19–26. doi: 10.1016/j.cca.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 2.Trevisani F, D’Intino PE, Morselli-Labate AM, Mazzella G, Accogli E, Caraceni P, Domenicali M, De Notariis S, Roda E, Bernardi M. Serum alpha-fetoprotein for diagnosis of hepatocellular carcinoma in patients with chronic liver disease: influence of HBsAg and anti-HCV status. J Hepatol. 2001;34:570–575. doi: 10.1016/s0168-8278(00)00053-2. [DOI] [PubMed] [Google Scholar]
- 3.Yao FY, Ferrell L, Bass NM, Watson JJ, Bacchetti P, Venook A, Ascher NL, Roberts JP. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology. 2001;33:1394–1403. doi: 10.1053/jhep.2001.24563. [DOI] [PubMed] [Google Scholar]
- 4.Zou WL, Zang YJ, Chen XG, Shen ZY. Risk factors for fatal recurrence of hepatocellular carcinoma and their role in selecting candidates for liver transplantation. Hepatobiliary Pancreat Dis Int. 2008;7:145–151. [PubMed] [Google Scholar]
- 5.Wang ZX, Song SH, Teng F, Wang GH, Guo WY, Shi XM, Ma J, Wu YM, Ding GS, Fu ZR. A single-center retrospective analysis of liver transplantation on 255 patients with hepatocellular carcinoma. Clin Transplant. 2010;24:752–757. doi: 10.1111/j.1399-0012.2009.01172.x. [DOI] [PubMed] [Google Scholar]
- 6.Toyoda H, Kumada T, Tada T, Niinomi T, Ito T, Kaneoka Y, Maeda A. Prognostic significance of a combination of pre- and post-treatment tumor markers for hepatocellular carcinoma curatively treated with hepatectomy. J Hepatol. 2012;57:1251–1257. doi: 10.1016/j.jhep.2012.07.018. [DOI] [PubMed] [Google Scholar]
- 7.Nobuoka D, Kato Y, Gotohda N, Takahashi S, Nakagohri T, Konishi M, Kinoshita T, Nakatsura T. Postoperative serum alpha-fetoprotein level is a useful predictor of recurrence after hepatectomy for hepatocellular carcinoma. Oncol Rep. 2010;24:521–528. doi: 10.3892/or_00000888. [DOI] [PubMed] [Google Scholar]
- 8.Sugawara Y, Tamura S, Makuuchi M. Living donor liver transplantation for hepatocellular carcinoma: Tokyo University series. Dig Dis. 2007;25:310–312. doi: 10.1159/000106910. [DOI] [PubMed] [Google Scholar]
- 9.Xu X, Ke QH, Shao ZX, Wu J, Chen J, Zhou L, Zheng SS. The value of serum alpha-fetoprotein in predicting tumor recurrence after liver transplantation for hepatocellular carcinoma. Dig Dis Sci. 2009;54:385–388. doi: 10.1007/s10620-008-0349-0. [DOI] [PubMed] [Google Scholar]
- 10.Hameed B, Mehta N, Sapisochin G, Roberts JP, Yao FY. Alpha-fetoprotein level > 1000 ng/mL as an exclusion criterion for liver transplantation in patients with hepatocellular carcinoma meeting the Milan criteria. Liver Transpl. 2014;20:945–951. doi: 10.1002/lt.23904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee KW, Yi NJ, Suh KS. Section 5. Further expanding the criteria for HCC in living donor liver transplantation: when not to transplant: SNUH experience. Transplantation. 2014;97(Suppl 8):S20–3. doi: 10.1097/01.tp.0000446269.20934.d3. [DOI] [PubMed] [Google Scholar]
- 12.Yang SH, Suh KS, Lee HW, Cho EH, Cho JY, Cho YB, Kim IH, Yi NJ, Lee KU. A revised scoring system utilizing serum alphafetoprotein levels to expand candidates for living donor transplantation in hepatocellular carcinoma. Surgery. 2007;141:598–609. doi: 10.1016/j.surg.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 13.Duvoux C, Roudot-Thoraval F, Decaens T, Pessione F, Badran H, Piardi T, Francoz C, Compagnon P, Vanlemmens C, Dumortier J, et al. Liver transplantation for hepatocellular carcinoma: a model including α-fetoprotein improves the performance of Milan criteria. Gastroenterology. 2012;143:986–994.e3. doi: 10.1053/j.gastro.2012.05.052. [DOI] [PubMed] [Google Scholar]