Abstract
Pregnant women are prioritized to receive influenza vaccination. However, the maternal influenza vaccination rate has been low in Korea. To identify potential barriers for the vaccination of pregnant women against influenza, a survey using a questionnaire on the perceptions and attitudes about maternal influenza vaccination was applied to Korean obstetricians between May and August of 2014. A total of 473 respondents participated in the survey. Most respondents (94.8%, 442/466) recognized that influenza vaccination was required for pregnant women. In addition, 92.8% (410/442) respondents knew that the incidence of adverse events following influenza vaccination is not different between pregnant and non-pregnant women. However, 26.5% (124/468) obstetricians strongly recommended influenza vaccination to pregnant women. The concern about adverse events following influenza vaccination was considered as a major barrier for the promotion of maternal influenza vaccination by healthcare providers. Providing professional information and education about maternal influenza vaccination will enhance the perception of obstetricians about influenza vaccination to pregnant women and will be helpful to improve maternal influenza vaccination coverage in Korea.
Keywords: Influenza Vaccines, Maternal Welfare, Pregnant Women
Graphical Abstract
INTRODUCTION
Pregnant women are at great risk for severe influenza and influenza-related complications and mortality (1,2,3). In November 2012, the World Health Organization recommended that pregnant women should have the highest priority for seasonal influenza vaccination and that they should be vaccinated with trivalent influenza vaccine at any trimester of pregnancy (4). However, the maternal influenza vaccination rate in Korea was only 4% according to a survey conducted in 2007 and 16.4% according to a study conducted in 2012 (5,6). In addition, influenza vaccine uptake among pregnant women is still low compared with that among the elderly and patients with chronic diseases.
To increase maternal influenza vaccination rate, not only the awareness about influenza vaccination in childbearing women but also the perception of its importance among obstetricians plays a key role. A previous study reported that the antenatal care provider’s recommendation to receive influenza vaccine was an important determinant associated with vaccination in pregnant women (7). The lack of recommendation by healthcare providers was a major reason for women not receiving influenza vaccination during pregnancy (5,6). In this study, the perception and attitudes of Korean obstetricians about maternal influenza vaccination were investigated. This study aimed to identify the potential barriers in maternal healthcare providers and to promote influenza vaccination coverage of pregnant women.
MATERIALS AND METHODS
A questionnaire survey of obstetricians who are members of the Korean Association of Obstetricians & Gynecologists (KAOG) was conducted between May and August 2014. The survey was performed using same questionnaire via fax mailing, information posting on the KAOG website, and a spot survey at a conference venue held by KAOG. The participation in the survey was voluntary and no incentives were provided to the respondents.
The questionnaire inquired about demographic characteristics of the participants, and their experience and practice of influenza vaccination to pregnant women. To the obstetricians who answered that they do not strongly recommend influenza vaccination to pregnant women, three major reasons for those practices were asked. Information about influenza and influenza vaccination in pregnant women were sequentially presented with references (8,9). ‘Influenza-related hospitalization risk was higher among pregnant women than among non-pregnant women’, ‘Maternal influenza vaccination decreased the rate of febrile respiratory illnesses in mothers and the rate of influenza in infants up to 6 months of age’, and ‘Adverse events following influenza vaccination did not differ between pregnant and non-pregnant women and influenza vaccination during pregnancy did not affect perinatal outcome’ were shown. The willingness to recommend maternal influenza vaccination in the future was evaluated after this information was provided sequentially. The reasons for not recommending influenza vaccination to pregnant women were inquired from the respondents who answered that they were not willing to recommend maternal influenza vaccination. In addition, the common sources of getting information about maternal influenza vaccination were inquired.
The frequency of responses was calculated and nonresponses were excluded from the denominator. For statistical analysis of change of willingness to recommend maternal influenza vaccination according to provided information, McNemar test was performed.
Ethics statement
This study was approved by the institutional review Board of Korea University Guro Hospital (approval number: KUGH14139). Study was conducted without written documentation of informed consent.
RESULTS
A total of 473 questionnaires were eligible to be analyzed. Questionnaires were collected via fax mailing (19.0%, 90/473), KAOG website (19.2%, 91/473), and a spot survey (61.7%, 292/473). Among the respondents, 62.8% were male (Table 1). The most frequent age group was 50-59 years (39.4%, 185/469) followed by the age group 40-49 years (35.6%, 167/469). Most of the participants (71.5%, 331/463) worked at local clinics. Influenza vaccination rate during the 2013-2014 influenza season was 81.4% (302/371) in obstetricians.
Table 1. Demographic characteristics of Korean obstetricians who participated in the survey.
| Characteristics | Value (%) |
|---|---|
| Sex (male) | 292/465 (62.8) |
| Age group, yr | |
| 20-29 | 1/469 (0.2) |
| 30-39 | 63/469 (13.4) |
| 40-49 | 167/469 (35.6) |
| 50-59 | 185/469 (39.4) |
| ≥ 60 | 53/469 (11.3) |
| Employment | |
| Local clinics | 331/463 (71.5) |
| Multispecialty hospital | 130/463 (28.1) |
| University hospital | 1/463 (0.2) |
| Resident in teaching hospital | 1/463 (0.2) |
| Influenza vaccination (2013-2014 season) | |
| Vaccinated | 302/371 (81.4) |
Nonresponses were excluded from the denominator.
Perception and practices about influenza vaccination of pregnant women
More than 90% of the respondents knew of the not different incidence of adverse events following influenza vaccination between pregnant and non-pregnant women (92.8%, 410/442), priority of pregnant women for influenza vaccination (92.7%, 417/450), and the increased risk of influenza-related complications during pregnancy (90.9%, 411/452) (Table 2). However, 78.8% (319/405) obstetricians were aware that pregnant women could be vaccinated against influenza during any trimester of pregnancy and 82.0% (338/412) knew that influenza during pregnancy increased the risk of poor birth outcomes.
Table 2. Perception and attitudes about influenza vaccination of pregnant women.
| Perception and attitudes | Value (%) |
|---|---|
| Perception | |
| Pregnant women are at increased risk of influenza-related complications compared with non-pregnant women. | 411/452 (90.9)* |
| Pregnant women infected with influenza have high risk of poor birth outcomes. | 338/412 (82.0)* |
| Pregnant women have a priority for seasonal influenza vaccination. | 417/450 (92.7)* |
| Pregnant women at any stage of pregnancy can get influenza vaccine. | 319/405 (78.8)* |
| Adverse events following influenza vaccination do not differ between pregnant and non-pregnant women. | 410/442 (92.8)* |
| Attitudes | |
| Having an experience giving influenza vaccines to pregnant women | |
| Yes | 395/473 (83.5) |
| No | 78/473 (16.5) |
| Frequency providing influenza vaccine to pregnant women (per ten patients) | |
| < 1 | 56/419 (13.4) |
| 1-2 | 103/419 (24.6) |
| 3-4 | 52/419 (12.4) |
| 5-6 | 72/419 (17.2) |
| 7-8 | 76/419 (18.1) |
| 9-10 | 60/419 (14.3) |
| Requirement to vaccinate pregnant women against influenza | |
| Required | 442/466 (94.8) |
| Not required | 24/466 (5.2) |
| Level of recommendation and practice of influenza vaccination to pregnant women | |
| Not recommend and vaccinate influenza vaccine to pregnant women | 30/468 (6.4) |
| Vaccinate pregnant women against influenza when they ask to be vaccinated | 122/468 (26.1) |
| Recommend influenza vaccination to pregnant women | 192/468 (41.0) |
| Strongly recommend influenza vaccination to pregnant women | 124/468 (26.5) |
Nonresponses were excluded from the denominator.
*answered ‘yes’.
Most of respondents (94.8%, 442/466) recognized that influenza vaccination was necessary for pregnant women. However, 83.5% (395/473) respondents vaccinated pregnant women against influenza and 32.5% (136/419) vaccinated pregnant women against influenza at a rate of ≥ 70% on average. Moreover, only 26.5% (124/468) of obstetricians have strongly recommended influenza vaccination to pregnant women.
Reasons for not strongly recommending influenza vaccination to pregnant women
For 344 respondents who answered that they do not strongly recommend influenza vaccination to pregnant women, the three major reasons for not doing so were asked and 690 answers were obtained. Concerns about adverse events following influenza vaccination (56.5%, 161/285), difficulty and unease to explain the need for influenza vaccination to pregnant women (56.1%, 160/285), and lack of pregnant women’s request to be vaccinated against influenza (45.5%, 121/285) were major reasons for not strongly recommending influenza vaccination to pregnant women. By a survey of the single reason for not strongly recommending influenza vaccination to pregnant women, the neglect of recommendation of influenza vaccination to pregnant women (24.4%, 62/254) was the dominant reason followed by difficulty and troublesomeness to explain the need for influenza vaccination to pregnant women (18.1%, 46/254) and concerns about adverse events following influenza vaccination (17.3%, 44/254) (Table 3).
Table 3. Reasons for not strongly recommending influenza vaccination to pregnant women.
| Reasons | Single response, No. (%) | Multiple responses, No. (%) |
|---|---|---|
| Concern for adverse events following influenza vaccination in pregnant women | 44/254 (17.3) | 161/285 (56.5) |
| Difficulty and troublesomeness to explain a need for influenza vaccination to pregnant women | 46/254 (18.1) | 160/285 (56.1) |
| Lack of request for influenza vaccine by pregnant women | 29/254 (11.4) | 121/285 (45.5) |
| Neglect of recommendation of influenza vaccination to pregnant women | 62/254 (24.4) | 109/285 (38.2) |
| Lack of knowledge about influenza vaccine effectiveness or safety in pregnant women | 44/254 (17.3) | 75/285 (26.3) |
| Cost | 3/254 (1.2) | 33/285 (11.6) |
| Low influenza vaccine effectiveness in pregnant women | 10/254 (3.9) | 18/285 (6.3) |
| Lack of interest in vaccination against influenza | 6/254 (2.4) | 13/285 (4.6) |
Nonresponses were excluded from the denominator.
Willingness to recommend influenza vaccination to pregnant women
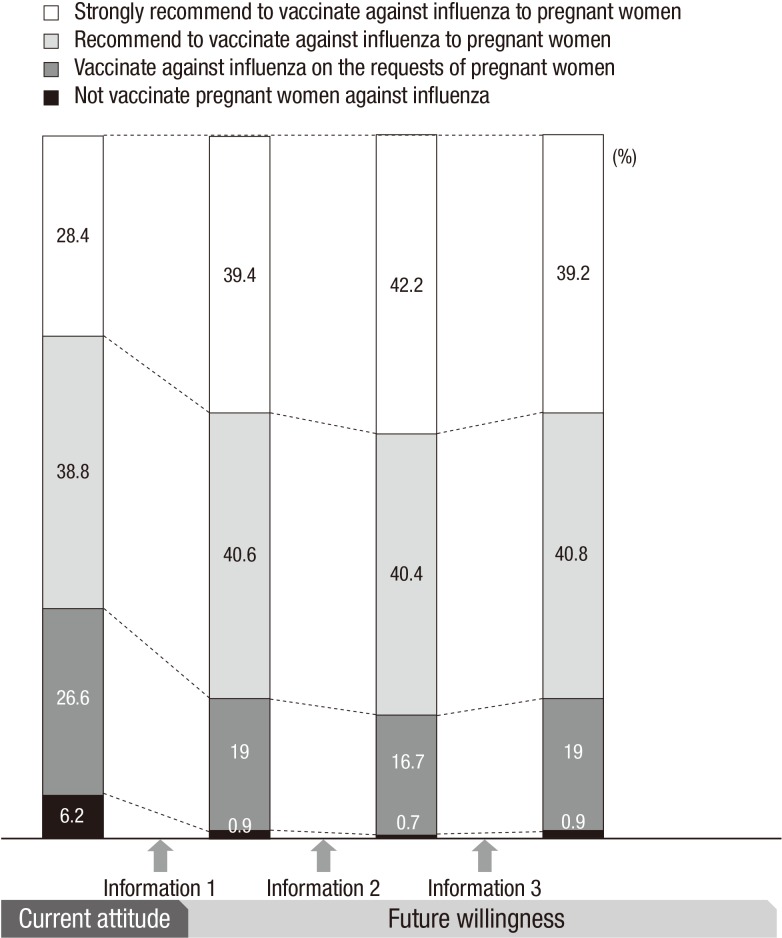
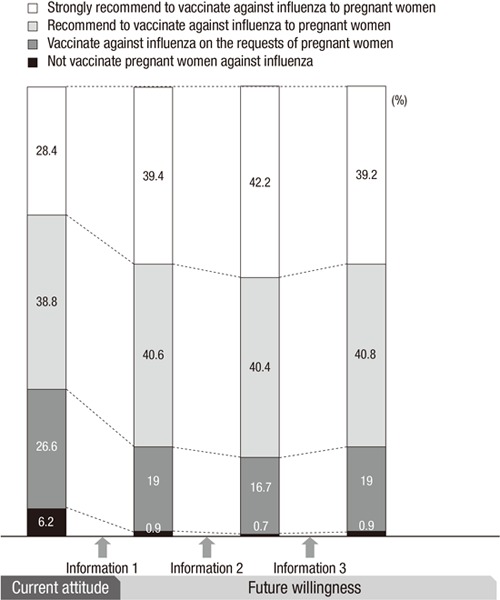
A total of 436 participants answered to the serial questions about current practice and willingness to recommend maternal influenza vaccination in the future (Fig. 1). Among the 436 respondents, 124 (28.4%) answered that they strongly recommend to vaccinate against influenza to pregnant women currently. After the information about ‘the increased hospitalization risk in pregnant women with influenza’ was provided, 39.4% (172/436) of respondents answered that they would strongly recommend influenza vaccination to pregnant women (P < 0.001). When the information about ‘the effect of maternal influenza vaccination on the prevention of febrile episodes in pregnant women and influenza in infants’ was presented in sequence, 42.2% (184/436) answered that they would strongly recommend influenza vaccination to pregnant women in the future (P=0.023). However, the rate of willingness to strongly recommend maternal influenza vaccination reduced to 39.2% (171/436) when the information about ‘the safety of maternal influenza vaccination to pregnant women and the perinatal outcomes’ was provided (P=0.011).
Fig. 1.
Current attitudes and consecutive willingness of obstetricians to recommend influenza vaccination to pregnant women were presented. Information about influenza and influenza vaccination in pregnant women was sequentially provided: information 1, increased severity in pregnant women with influenza; information 2, influenza vaccine effectiveness in pregnant women and infants up to 6 months of age; information 3, safety of influenza vaccination in pregnant women.
Furthermore, 4.5% (20/441) of respondents answered that they would not recommend to vaccinate against influenza to pregnant women (Table 4). The analysis of multiple responses indicated that the major reason was the concern over the safety of influenza vaccination during pregnancy (85.0%, 17/20).
Table 4. Willingness to recommend influenza vaccination to pregnant women in the future and reasons for not recommending influenza vaccination to pregnant women.
| Willingness and reasons | Value (%) |
|---|---|
| Recommend | 421/441 (95.5) |
| Do not recommend | 20/441 (4.5) |
| Concern about the safety of influenza vaccine | 17/20 (85.0) |
| Concern about the effectiveness of influenza vaccine | 9/20 (45.0) |
| Lack of forceful advice by government | 8/20 (40.0) |
| Cost of influenza vaccine | 5/20 (25.0) |
| Belief that the severity of influenza is negligible | 3/20 (15.0) |
Nonresponses were excluded from the denominator.
Sources of information about maternal influenza vaccination
To the question about major routes by which the obstetricians obtain information about maternal influenza vaccination, a total of 511 answers were collected from 460 participants. The most common source of getting information about influenza vaccination in pregnant women was academic meetings (61.7%, 284/460) such as conferences, symposium and seminars. Other sources included media (22.2%, 102/460), scientific journals (11.7%, 54/460), promotional materials (9.6%, 44/460), and governmental guidance (5.9%, 27/460).
DISCUSSION
Maternal influenza vaccination protects both pregnant women and infants from influenza (10,11). The safety of maternal influenza vaccination on both maternal and fetal outcomes during pregnancy has been shown in several studies (12,13,14). However, influenza vaccination coverage among pregnant women is still lower than that among the elderly (up to 80%) and among individuals with underlying medical diseases (50%-60%) in Korea (15,16,17). In general, obstetricians are the principal healthcare providers to pregnant women. Thus, they play a key role in maternal influenza vaccination. Recommendation and offer for influenza vaccination by healthcare providers of pregnant women have an influence on the acceptance of influenza vaccination of pregnant women (18).
In this study, most respondents had the appropriate perception about influenza and influenza vaccination during pregnancy, whereas 21.2% obstetricians were not aware that pregnant women could be vaccinated against influenza regardless of the trimester of pregnancy. Since 2004, the Advisory Committee on Immunization Practices (ACIP) has recommended that all pregnant women at any trimester and women who will be pregnant during the influenza season should be vaccinated (19). However, still some healthcare providers offer influenza vaccination only during the second or third trimester of pregnancy (20).
Most respondents perceived the need for maternal influenza vaccination and not increased risk of adverse events following influenza vaccination in pregnant women compared with non-pregnant women. However, there were substantial discrepancies between their perceptions and practices. The concern over the potential of harmful effects of influenza vaccination to the fetus and the anticipated pressure about succeeding measures following the occurrence of adverse events following influenza vaccination in pregnant women would be responsible for these discrepancies among obstetricians. In addition, the concern for the safety of influenza vaccination in pregnant women and following psychological resistance to maternal influenza vaccination may lead to neglect of explanation the need for influenza vaccination and strong recommendation of influenza vaccination to pregnant women.
The results of providing information and serial questions on the willingness to recommend influenza vaccination to pregnant women revealed the negative attitude of obstetricians on the basis of concerns for the safety of influenza vaccine to pregnant women. When the information about ‘the safety’ of influenza vaccination during pregnancy regarding maternal and perinatal outcomes was provided, the willingness to strongly recommend influenza vaccination to pregnant women significantly decreased from 42.2% to 39.2%. This result suggests that the potential concern and pressure about safety of maternal influenza vaccination made the obstetricians feel uneasy even though information on the safety of influenza vaccination during pregnancy was provided.
In the Unites States, the Healthy People 2020 established a target of the percentage of pregnant women who are vaccinated against seasonal influenza as 80% (21). Despite the highest priority for seasonal influenza vaccination of pregnant women provided by WHO, pregnant women do not have the highest priority for influenza vaccination in Korea. Pregnant women just belonged to priority group for influenza vaccination and maternal influenza vaccination has not been incorporated into the National Immunization Program (NIP) in Korea. The revision of the NIP including influenza vaccination in pregnant women might be helpful to lessen the concern of obstetricians about the safety of maternal influenza vaccination and to improve the maternal influenza vaccination rate.
This study has some limitations. Most of respondents are primary care obstetricians, thus, our results do not sufficiently reflect perception and attitudes about maternal influenza vaccination of healthcare workers in tertiary care hospitals. There is a possibility that respondents are more aware of the importance of influenza vaccination in pregnant women. Missing responses in the questionnaire could suggest lack of knowledge about influenza vaccination in pregnant women. Also, participants could show more positive attitude for maternal influenza vaccination as the survey progress forward. Overall response rate could not be estimated from the study. However, this study might be valuable to evaluate major barrier for the promotion of maternal influenza vaccination by healthcare providers.
This study indicates that the obstetricians are sufficiently aware of the need, effectiveness, and safety of influenza vaccination in pregnant women. However, the concern about the potential harmful effects of influenza vaccine on maternal and fetal health make them not strongly recommend influenza vaccination to pregnant women in practice. Providing professional information and education in scientific meetings about maternal influenza vaccination will enhance the perception of obstetricians about influenza vaccination to pregnant women. In addition, the revision of governmental policies for influenza vaccination of high-risk groups could be considered to support maternal influenza vaccination and to improve influenza vaccination coverage of pregnant women in Korea.
ACKNOWLEDGMENT
Authors wish to thank Hyun-Ok An in the Korean Association of Obstetricians and Gynecologists for supporting the survey.
Footnotes
Funding: This study was supported by a grant of the TEPIK (Transgovernmental Enterprise for Pandemic Influenza in Korea) which is a part of Korea Healthcare Technology R&D Project by Ministry of Health and Welfare‚ Republic of Korea (Grant No. A103001).
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conception and design: Noh JY, Seo YB, Song JY, Choi WS, Lee J, Lee JS, Cheong HJ, Kim WJ. Acquisition of data: Noh JY, Jung E, Kang S, Choi MJ, Jun J, Yoon JG, Lee SN, Hyun H, Cheong H, Cheong HJ. Analysis and interpretation of data: Noh JY, Seo YB, Song JY, Choi WS, Lee J, Lee JS, Cheong HJ. Manuscript preparation: Noh JY, Cheong HJ. Manuscript approval: all authors.
References
- 1.Kourtis AP, Read JS, Jamieson DJ. Pregnancy and infection. N Engl J Med. 2014;370:2211–2218. doi: 10.1056/NEJMra1213566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jamieson DJ, Honein MA, Rasmussen SA, Williams JL, Swerdlow DL, Biggerstaff MS, Lindstrom S, Louie JK, Christ CM, Bohm SR, et al. H1N1 2009 influenza virus infection during pregnancy in the USA. Lancet. 2009;374:451–458. doi: 10.1016/S0140-6736(09)61304-0. [DOI] [PubMed] [Google Scholar]
- 3.Siston AM, Rasmussen SA, Honein MA, Fry AM, Seib K, Callaghan WM, Louie J, Doyle TJ, Crockett M, Lynfield R, et al. Pandemic 2009 influenza A(H1N1) virus illness among pregnant women in the United States. JAMA. 2010;303:1517–1525. doi: 10.1001/jama.2010.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vaccines against influenza WHO position paper - November 2012. Wkly Epidemiol Rec. 2012;87:461–476. [PubMed] [Google Scholar]
- 5.Kim MJ, Lee SY, Lee KS, Kim A, Son D, Chung MH, Park SG, Park JH, Lee BI, Lee JS. Influenza vaccine coverage rate and related factors on pregnant women. Infect Chemother. 2009;41:349–354. [Google Scholar]
- 6.Kim IS, Seo YB, Hong KW, Noh JY, Choi WS, Song JY, Cho GJ, Oh MJ, Kim HJ, Hong SC, et al. Perception on influenza vaccination in Korean women of childbearing age. Clin Exp Vaccine Res. 2012;1:88–94. doi: 10.7774/cevr.2012.1.1.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mak DB, Regan AK, Joyce S, Gibbs R, Effler PV. Antenatal care provider’s advice is the key determinant of influenza vaccination uptake in pregnant women. Aust N Z J Obstet Gynaecol. 2015;55:131–137. doi: 10.1111/ajo.12292. [DOI] [PubMed] [Google Scholar]
- 8.Mertz D, Kim TH, Johnstone J, Lam PP, Science M, Kuster SP, Fadel SA, Tran D, Fernandez E, Bhatnagar N, et al. Populations at risk for severe or complicated influenza illness: systematic review and meta-analysis. BMJ. 2013;347:f5061. doi: 10.1136/bmj.f5061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zaman K, Roy E, Arifeen SE, Rahman M, Raqib R, Wilson E, Omer SB, Shahid NS, Breiman RF, Steinhoff MC. Effectiveness of maternal influenza immunization in mothers and infants. N Engl J Med. 2008;359:1555–1564. doi: 10.1056/NEJMoa0708630. [DOI] [PubMed] [Google Scholar]
- 10.Madhi SA, Cutland CL, Kuwanda L, Weinberg A, Hugo A, Jones S, Adrian PV, van Niekerk N, Treurnicht F, Ortiz JR, et al. Influenza vaccination of pregnant women and protection of their infants. N Engl J Med. 2014;371:918–931. doi: 10.1056/NEJMoa1401480. [DOI] [PubMed] [Google Scholar]
- 11.Blanchard-Rohner G, Siegrist CA. Vaccination during pregnancy to protect infants against influenza: why and why not? Vaccine. 2011;29:7542–7550. doi: 10.1016/j.vaccine.2011.08.013. [DOI] [PubMed] [Google Scholar]
- 12.Bratton KN, Wardle MT, Orenstein WA, Omer SB. Maternal influenza immunization and birth outcomes of stillbirth and spontaneous abortion: a systematic review and meta-analysis. Clin Infect Dis. 2015;60:e11–9. doi: 10.1093/cid/ciu915. [DOI] [PubMed] [Google Scholar]
- 13.Chambers CD, Johnson D, Xu R, Luo Y, Louik C, Mitchell AA, Schatz M, Jones KL, OTIS Collaborative Research Group Risks and safety of pandemic H1N1 influenza vaccine in pregnancy: birth defects, spontaneous abortion, preterm delivery, and small for gestational age infants. Vaccine. 2013;31:5026–5032. doi: 10.1016/j.vaccine.2013.08.097. [DOI] [PubMed] [Google Scholar]
- 14.Takeda S, Hisano M, Komano J, Yamamoto H, Sago H, Yamaguchi K. Influenza vaccination during pregnancy and its usefulness to mothers and their young infants. J Infect Chemother. 2015;21:238–246. doi: 10.1016/j.jiac.2015.01.015. [DOI] [PubMed] [Google Scholar]
- 15.Kee SY, Lee JS, Cheong HJ, Chun BC, Song JY, Choi WS, Jo YM, Seo YB, Kim WJ. Influenza vaccine coverage rates and perceptions on vaccination in South Korea. J Infect. 2007;55:273–281. doi: 10.1016/j.jinf.2007.04.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seo YB, Choi WS, Baek JH, Lee J, Song JY, Lee JS, Cheong HJ, Kim WJ. Effectiveness of the influenza vaccine at preventing hospitalization due to acute exacerbation of cardiopulmonary disease in Korea from 2011 to 2012. Hum Vaccin Immunother. 2014;10:423–427. doi: 10.4161/hv.26858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Seo YB, Hong KW, Kim IS, Choi WS, Baek JH, Lee J, Song JY, Lee JS, Cheong HJ, Kim WJ. Effectiveness of the influenza vaccine at preventing hospitalization due to acute lower respiratory infection and exacerbation of chronic cardiopulmonary disease in Korea during 2010-2011. Vaccine. 2013;31:1426–1430. doi: 10.1016/j.vaccine.2012.10.024. [DOI] [PubMed] [Google Scholar]
- 18.Kennedy ED, Ahluwalia IB, Ding H, Lu PJ, Singleton JA, Bridges CB. Monitoring seasonal influenza vaccination coverage among pregnant women in the United States. Am J Obstet Gynecol. 2012;207(Suppl):S9–16. doi: 10.1016/j.ajog.2012.06.069. [DOI] [PubMed] [Google Scholar]
- 19.Harper SA, Fukuda K, Uyeki TM, Cox NJ, Bridges CB, Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP) Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2004;53:1–40. [PubMed] [Google Scholar]
- 20.Kissin DM, Power ML, Kahn EB, Williams JL, Jamieson DJ, MacFarlane K, Schulkin J, Zhang Y, Callaghan WM. Attitudes and practices of obstetrician-gynecologists regarding influenza vaccination in pregnancy. Obstet Gynecol. 2011;118:1074–1080. doi: 10.1097/AOG.0b013e3182329681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.The Office of Disease Prevention and Health Promotion (US) Healthy People 2020 [Internet] [accessed on 11 March 2015]. Available at http://www.healthypeople.gov/node/3527/data-details.