Abstract
Education has been known to essential for management of chronic airway diseases. However the real benefits remain unclear. We evaluated the effectiveness of an organized educational intervention for chronic airway diseases directed at primary care physicians and patients. The intervention was a 1-month education program of three visits, during which subjects were taught about their disease, an action plan in acute exacerbation and inhaler technique. Asthma control tests (ACT) for asthma and, chronic obstructive pulmonary disease (COPD) assessment tests (CAT) for COPD subjects were compared before and after education as an index of quality of life. Educational effectiveness was also measured associated with improvement of their knowledge for chronic airway disease itself, proper use of inhaler technique, and satisfaction of the subjects and clinicians before and after education. Among the 285 participants, 60.7% (n = 173) were men and the mean age was 62.2 ± 14.7. ACT for asthma and CAT in COPD patients were significantly improved by 49.7% (n = 79) and 51.2% (n = 65) more than MCID respectively after education (P < 0.05). In all individual items, knowledge about their disease, inhaler use and satisfaction of the patients and clinicians were also improved after education (P < 0.05). This study demonstrates the well-organized education program for primary care physicians and patients is a crucial process for management of chronic airway diseases.
Keywords: Education; Inhaler; Asthma; Pulmonary Disease, Chronic Obstructive; Physicians, Primary Care
Graphical Abstract
INTRODUCTION
Asthma and COPD are the major disease categories in chronic airway disease, and their prevalence has been increasing worldwide (1,2). Additionally, the World Health Organization (WHO) predicts that COPD will become the fourth leading cause of death worldwide in 2030 (3). In Korea, by the Korea National Health and Nutrition Examination Survey (KNHANES) data, the prevalence of COPD and asthma were around 13.4% and 3.9%, each (4,5). However, similar to other countries, patients usually visit physicians only when their symptom worsen due to the lack of awareness about their disease. Additionally, the inhaler prescription rate has still been reported low even though the Global Initiative for Chronic Obstructive Lung Disease (GOLD) and Global Initiative for Asthma (GINA) document has suggested the inhaler as the first line therapy (6,7,8). And even after an appropriate prescription, treatment effect could be varied from person to person according to adherence to medication. In Korea, Quality Assessment of the Asthma has been conducted which was led by the Health Insurance Review and Assessment Service (HIRA) since 2013 (9). According to this, only 17% of primary clinics implemented spirometry, and 16% of them prescribed an inhaler such as inhaled corticosteroid (ICS) or ICS with long-acting beta-2 agonist (LABA) (9). Quality Assessment of COPD is also under way, and the result may be similar to asthma.
In contrast with oral medication, inhaler use requires education no matter what. Besides non-adherence to medication, improper use also can cause failure to control chronic airway disease. Improper use may decrease the effectiveness of the medication; decrease the compliance due to the side effect like oral candidiasis. One study showed that the regular use of low-dose inhaled corticosteroids is associated with a decreased risk of hospitalization and death from asthma (10). However, patient compliance with the steroid inhaler counted as 50% or less (11). COPD subjects also had similar compliance issues (1). However, up to the present, there has been scarce research attempting to identify what can improve inhaler techniques and patient education and understanding about chronic airway disease, both asthma and COPD.
In this study, assuming that organized education for patients who had chronic airway disease could be associated with improving compliance and treatment in primary clinic settings, we observed changes in disease understanding, quality of life, inhaler technique, and satisfaction with education.
MATERIALS AND METHODS
Inclusion and exclusion criteria
Subjects aged over 20 years who were diagnosed with asthma or COPD by their physicians were recruited from 43 primary clinics. Patients who were given informed consent and agreed with participation in this study are included. Patients were diagnosed with asthma or COPD based on the primary physician's clinical judgment. Subjects with malignant cancer, severe kidney or heart disease, transplanted organ for any lesion, bronchiectasis, sequele of tuberculosis and pregnant women were excluded.
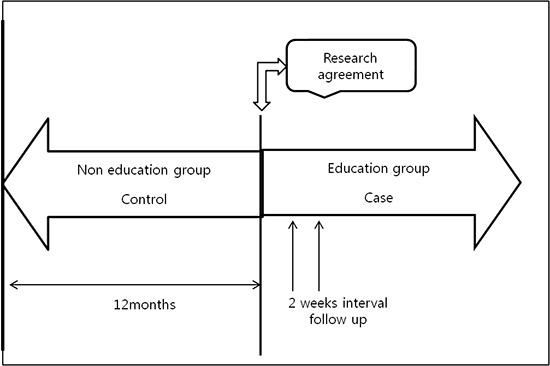
Study design
The present study is a prospective study comparing the outcomes of pre and post-intervention, a one-month education program. We selected four to five primary clinics from each province of Korea (Seoul, Chungcheongbuk-do, Chungcheongnam-do Gyeonggi-do, Gangwon-do, Jeollabuk-do, Jeollanam-do, Jeju-do). Subjects who had been visiting each primary clinic over one year or more were enrolled as an education group from the point of receiving informed consent, three educational visits were conducted and comparing the alteration before and after education. Follow-up visits were held every two weeks in the primary care setting. At the first visit, we obtained the informed consent from each subject, conducted knowledge assessment about their chronic airway disease, and tested their inhaler use technique before the patients received the educational program. Thereafter, we conducted education about disease and inhaler use, and showed educational videos, on these topics. At the second visit, they were taught about an action plan for acute exacerbation and inhaler technique, and received associated video education. At the third visit, the educational contents were refreshed. Thereafter, we investigated the change of each topic: knowledge about their disease, quality of life (ACT in asthma, CAT in COPD patients), inhaler use technique, patients and physicians satisfaction with the education program. Measurement items of each topic were composed of six (knowledge), five (ACT), eight (CAT), seven (inhaler usage), three (satisfaction of the patients), and five items (satisfaction of the physicians). Each item has a 4 grade scale such as “strongly disagree, somewhat disagree, somewhat agree, strongly agree”. And Minimum Clinically Important Difference (MCID) for objective evaluation of quality of life improvement was defined as 3 points in ACT score (12) and 4 points in CAT score (13).
Statistical methods
The results for each variable were shown as the mean with standard deviation, in the case of continuous variables; and the number of cases per category and frequency of responses in the case of categorical variables. For the comparison of quality of life between before and after education, we used paired t-test with the significance level of 0.05. For the comparisons of degree of knowledge and assessment of usage of inhaler by physician before and after education, χ2 test was used. We used SPSS 21.0 (SPSS Inc., Chicago, IL, USA) for statistical analysis.
Ethics statement
The study protocol was reviewed and approved by the Inje University institutional review board (# IIT-2014-283). A written informed consent, describing the purpose of the study was signed by all of the participants.
RESULTS
Baseline characteristics of the study population
After excluding registration error (n = 11) and new patients (n = 19), 285 subjects were finally analyzed. Of the total who completed the survey, 158 (55.4%) had asthma and 127 (44.6%) had COPD. The baseline characteristics are shown in Table 1. The investigated subjects were 62.2 ± 14.7 years and a large portion of the asthma group were women (n = 98, 62.0%), and most of the COPD group were men (n = 113, 89.0%) (Table 1). Hypertension was the most common comorbidity (n = 121, 42.5%) (Table 1).
Table 1. Baseline characteristics according to the asthma and COPD.
| Variables | No. (%) of patients | ||
|---|---|---|---|
| Asthma (n = 158) | COPD (n = 127) | Total (n = 285) | |
| Gender | |||
| Male | 60 (38.0) | 113 (89.0) | 173 (60.7) |
| Female | 98 (62.0) | 14 (11.0) | 112 (39.3) |
| Age, yr | |||
| Mean ± SD | 57.7 ± 16.2 | 67.8 ± 10.1 | 62.2 ± 14.7 |
| 20-29 | 13 (8.2) | 0 (0.0) | 13 (4.6) |
| 30-39 | 13 (8.2) | 1 (0.8) | 14 (4.9) |
| 40-49 | 23 (14.6) | 4 (3.1) | 27 (9.5) |
| 50-59 | 31 (19.6) | 18 (14.2) | 49 (17.2) |
| 60-69 | 30 (19.0) | 39 (30.7) | 69 (24.2) |
| ≥ 70 | 48 (30.4) | 65 (51.2) | 113 (39.6) |
| Total | 158 (100) | 127 (100) | 285 (100) |
| Comorbidities | |||
| Hypertension | 64 (40.5) | 57 (44.9) | 121 (42.5) |
| Cardiovascular disorder (Angina pectoris, MI) | 2 (1.3) | 6 (4.7) | 8 (2.8) |
| Heart failure | 1 (0.6) | 5 (3.9) | 6 (2.1) |
| Arrhythmia | 4 (2.5) | 4 (3.7) | 8 (2.8) |
| Diabetes mellitus | 25 (15.8) | 16 (12.6) | 41 (14.4) |
| Hyperlipidemia | 39 (24.7) | 11 (8.7) | 50 (17.5) |
| Osteoporosis | 10 (6.3) | 3 (2.4) | 13 (4.6) |
| Depression | 0 (0.0) | 7 (5.5) | 7 (2.5) |
| Anemia | 1 (0.6) | 2 (1.6) | 3 (1.1) |
| Others | 13 (8.2) | 14 (11.0) | 27 (9.5) |
| Total | 89 (56.3) | 80 (63.0) | 169 (59.3) |
| Patient's basic knowledge for chronic airway disease | |||
| Education about their disease previous 1 year before visit | |||
| Never | 91 (58.0) | 76 (60.3) | 167 (59.0) |
| Intermittent (1-2 times) | 35 (22.3) | 27 (21.4) | 62 (21.9) |
| Frequently (≥ 3 times) | 7 (4.5) | 7 (5.6) | 14 (4.9) |
| Every time | 24 (15.3) | 16 (12.7) | 40 (14.1) |
COPD, chronic obstructive pulmonary disease; SD, standard deviation; MI, myocardial ischemia.
Changes of quality of life before and after implementing education
ACT total score was increased significantly, and CAT score decreased significantly (P < 0.05) (Table 2). Quality of life improvement more than MCID was 49.7% (79/159) in asthma and 51.2% (65/127) in COPD.
Table 2. Quality of life before and after education.
| Disease | Before education | After education | After-before | P value | Improving more than MCID, No. (%) | |
|---|---|---|---|---|---|---|
| ACT* for asthma subjects | N | 158 | 158 | 158 | ||
| Mean ± SD | 16.6 ± 4.6 | 19.8 ± 4.1 | 3.2 ± 4.6 | < 0.01 | 79 (49.7) | |
| CAT* for COPD subjects | N | 127 | 127 | 127 | ||
| Mean ± SD | 19.9 ± 9.7 | 15.4 ± 9.2 | - 4.4 ± 9.6 | < 0.01 | 65 (51.2) | |
MICD, minimum clinically important difference; ACT, asthma control test; SD, standard deviation; CAT, COPD assessment test; COPD, chronic obstructive pulmonary disease.
*ACT and CAT total score.
Assessment of the chronic airway disease patients' knowledge about the disease before and after implementing education
When analyzing the patients' knowledge before and after implementing the education program, knowledge improvement was observed, since the number of positive answers for each topic containing questions about their chronic airway disease increased. Values were statistically significant for every topic (P < 0.05) (Table 3).
Table 3. The change of knowledge before and after education.
| Items | Positive answer | P value | Improvement, No. (%) | |
|---|---|---|---|---|
| Before education | After education | |||
| I am aware of my disease. | 145 (51.0) | 257 (90.5) | < 0.01 | 161 (56.5) |
| My disease should be treated consistently | 223 (78.5) | 277 (97.5) | < 0.01 | 114 (40.0) |
| I know about how to act at the time of aggravation of my respiratory symptoms. | 130 (45.8) | 247 (87.2) | < 0.01 | 167 (57.6) |
| The most important drug in the treatment of my disease is inhaler. | 200 (70.5) | 274 (96.5) | < 0.01 | 139 (48.8) |
| I know about the method of inhaler use. | 208 (73.5) | 279 (98.2) | < 0.01 | 117 (41.1) |
| I used inhaler regularly according to the prescription. | 201 (71.0) | 265 (93.7) | < 0.01 | 118 (41.4) |
Data are number (percentage); χ2 test for statistical analysis.
Change in usage of inhaler
The usage of inhaler was assessed stage by stage from opening to rinsing the mouth after inhaler use. Every step showed statistically significant changes (P < 0.01). Especially enough breathing out before inhalation (71.4%) and holding their breath after inhalation (70.7%) were the first two higher improving items (Table 4).
Table 4. The improvement in usage of inhaler assessed by physicians before and after education.
| Items | Positive answer | P value | Improvement, No. (%) | |
|---|---|---|---|---|
| Before education | After education | |||
| Open the lid correctly | 224 (79.7) | 280 (99.2) | < 0.01 | 134 (47.9) |
| Hold the inhalator correctly | 192 (68.3) | 275 (97.5) | < 0.01 | 156 (55.7) |
| Enough breathing out before inhalation | 100 (35.6) | 251 (89.0) | < 0.01 | 200 (71.4) |
| Good understanding of the manner of inhalation | 130 (46.3) | 269 (95.4) | < 0.01 | 187 (66.8) |
| Hold his/her breath for 5 seconds after inhalation | 115 (40.9) | 265 (94.0) | < 0.01 | 198 (70.7) |
| Breathe out after removing the inhalator at the end of the inhalation | 156 (55.5) | 266 (94.7) | < 0.01 | 178 (63.8) |
| Rinsing his mouth after inhalator use | 175 (68.6) | 250 (97.2) | < 0.01 | 144 (58.1) |
Data are number (percentage); χ2 test for statistical analysis.
Satisfaction for education of the chronic airway disease patients and clinicians
All items for patients and physicians showed more positive answers than negative answers (Table 5).
Table 5. Degree of satisfaction of patients and physicians after the education.
| Questionannaire items | Strongly disagree | Somewhat disagree | Somewhat agree | Strongly agree |
|---|---|---|---|---|
| Items for patients | ||||
| I know much about the disease after the education provided by the hospital. | 0 (0.0) | 8 (2.8) | 164 (57.7) | 112 (39.4) |
| I think education from the hospital is needed. | 0 (0.0) | 10 (3.5) | 154 (54.2) | 120 (42.3) |
| If I have a chance to education, I will receive an education with additional cost. | 5 (1.8) | 40 (14.1) | 151(53.2) | 88 (31.0) |
| Items for physicians | ||||
| My perception for patient education was changed after the program. | 0 (0.0) | 1 (3.4) | 16 (55.2) | 10 (34.5) |
| My knowledge level was changed after the education program. | 0 (0.0) | 4 (13.8) | 16 (55.2) | 7 (24.1) |
| Patient's compliance was improved after the education. | 0 (0.0) | 0 (0.0) | 19 (65.5) | 8 (27.6) |
| Treatment effect was improved after the education. | 0 (0.0) | 0 (0.0) | 24 (82.8) | 3 (10.3) |
| Education program is positively necessary for treating patients. | 0 (0.0) | 0 (0.0) | 12 (41.4) | 15 (51.7) |
Data are number (percentage).
DISCUSSION
In this study, we identified that education for chronic airway disease patients could be associated with the knowledge about the disease and inhaler use improvement and these could be connected to the quality of life improvement and satisfaction of the patients and physicians in a primary care setting. There have been many studies associated with educational effect in chronic airway disease using diverse items, however, we got the maximum efficiency with minimum effort for both patients and physicians through the education program, spending only five minutes or less and using video demonstrations in the waiting room.
Comparing the knowledge before and after education, all of the items showed significant improvements. When diagnosing the chronic airway disease, patients think that nothing can be done about their disease. Sometimes, when they get breathlessness, they think this means they will suffocate. Even with a flood of information, many of the patients do not visit the physician until an exacerbation develop, which frequently cannot be treated in a primary clinic, and has been known to be as a major cause of hospitalization (14,15). Based on the KNHANES IV, the total number of people with COPD in 2009 was 3,033,560, but only 6.3% of those subjects actually used medical facilities (4,14). As our data showed, cognitive restructuring by education could be expected to improve this low rate of hospital visits and that would also be associated with actively participating in treatment and better prognosis.
By early detection and experiencing improvement after the education and medication, patient's quality of life also can be positively changed as our data showed. In the general population, forced expiratory volume in one seconds (FEV1) declines annually about 25 to 50 mL (6). But in a COPD patient this is commonly observed as an 80 to 150 mL annual decline (16,17). We used MCID to rule out this natural decline effect and have a more objective understanding of the changes comparing both COPD and asthma. Percentage of improvement identified significantly more than MCID in both asthma and COPD. Although we did not evaluate the change of the lung function, ACT in asthma and CAT in COPD has been well correlated with lung function decline. So, enhancement of self-management and cognitive reconstruction, self-confidence in inhaler technique through education, might be associated with the possibility of minimizing lung function decline.
In the Asthma Insights and Reality in Asia-Pacific Phase (AIRIAP) study, which surveyed over 2,300 asthma patients in 8 areas of ASIA including South Korea, showed that only 13.3% of the total participants used ICS and a remarkably low rate in Korea (1.3%) (18). However, Korea has seen an increasing rate of ICS use even though most patients still use a quick reliever only when they experience an attack (5). It might be the result of the change of physician's efforts to treat their asthma patients based on the GINA guideline, combined with the improvement of basic disease knowledge amongst patients over the last couple of decades. However, still a lot of asthma patients are treated inadequately. That means that even thought the fact that inhaled corticosteroid are considered the cornerstone of asthma management, both patients and physicians still prefer the quick reliever and oral medication rather than controller, especially in Korea.
Considering steroid inhaler use, previous introduction and education about their disease could be very important for sustained rapport formation and successful management (19). Additionally, older people with a long history of chronic airway disease may have confidence in using their inhaler in their own way regardless of demonstration and coaching. One study suggested that a patient-centered approach for prescribing inhaler device in primary care and another visit for device technique education is very important for improved outcomes (20). And another randomized controlled trial suggested that passive education alone fails to achieve any improvement in device technique (21). One-on-on technique coaching, including observation, verbal instruction and physical demonstration is needed for improvement. In line with our study, patients had more chance to improve with active education and its association with satisfaction of the patients and clinicians.
Among the improvement of inhaler technique, the “Enough breathing out before inhalation” item showed a highly positive change rate after education. Previous studies also showed that failure to exhale before inhalation is one of the most frequent errors associated with inhaler use (22,23), which means that it is the most important point for teaching techniques especially for dry powder inhalers (DPI) as well as metered dose inhaler (MDI). Even more simple and easier to use compared with MDI, exhaling over a DPI causes excess moisture develop and is associated with a decrease in the delivery of given fixed doses (24). In this study, we verified that the need for education was very high. Most strikingly, patients wanted to be educated even though they pay their cost. Clinicians also experienced that patients' compliance improved after the education by improvement in their disease knowledge and treatment effect. That is, satisfaction both of the patients and clinicians resulted from a well organized educational program like that used in our study, would be undoubtedly necessary to both of them.
The first strength of our study is improving perception about chronic airway disease with minimal effort by a well-organized education program using video-assisted education during waiting time, which eventually took maximal effect of education. Few studies have addressed the effect of patients' and primary clinicians' education, including the whole area of our country (19,25,26,27). Also, no studies existed to our knowledge containing both asthma and COPD. An additional strength is that it is possible to generalize our results. One study showed that, the number of health care use per person was higher in those attending primary and secondary facilities compared to tertiary hospitals (14). As we studied for chronic airway disease patients who visit primary clinics, it could be more objective for showing the effect of education.
The limitation of this study is that no control group existed. We are planning a prospective study and expect to see more clearly the effect of education, if we can get control data. We did not enroll a non-educating control group, because it might cause ethical problems. But, there was no problem in this study design because it compared pre and post knowledge in the same patients. Due to the possibility of observer effect, we cannot completely rule out the possibility of exaggeration of our results (28,29). Another limitation is that no spirometry result was obtained for diagnosing COPD and asthma. But the purpose of this study was to survey the effect of education for chronic airway disease, not for correct diagnosis of COPD and asthma itself. We expect that this study could form the basis of other large population studies for further development of patients' and clinicians' education especially in chronic airway disease which had been regarded as an incurable disease. Also, the present study demonstrates some potentially important changes as a result of a well-organized education program for primary care physicians and patients in dealing with their chronic airway disease.
Footnotes
Funding: This work was conducted with support from AstraZeneca Korea Ltd.
DISCLOSURE: The authors have no potential conflicts of interest to declare.
AUTHOR CONTRIBUTION: Study concept, design, and data collection: Lee JY, Yoo KH, Kim DK, Kim SH, Kim TE, Kim TH. Rhee CK, Park YB, Yoon HK, Yum HK. Writing and revision: Lee JY, Yoo KH, Kim DK, Kim SH, Kim TE, Kim TH. Rhee CK, Park YB, Yoon HK, Yum HK. Review and revision: Lee JY, Yoo KH, Yum HK, Park YB. Accept final version of the manuscript: all authors.
References
- 1.Restrepo RD, Alvarez MT, Wittnebel LD, Sorenson H, Wettstein R, Vines DL, Sikkema-Ortiz J, Gardner DD, Wilkins RL. Medication adherence issues in patients treated for COPD. Int J Chron Obstruct Pulmon Dis. 2008;3:371–384. doi: 10.2147/copd.s3036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The Global Asthma Network. The global asthma report 2014 [Internet] [accessed on July 2014]. Available at http://www.globalasthmareport.org/resources/Global_Asthma_Report_2014.pdf.
- 3.World Health Organization. Chronic respiratory diseases [Internet] [accessed on 26 February 2008]. Available at http://www.who.int/gard/publications/chronic_respiratory_diseases.pdf.
- 4.Yoo KH, Kim YS, Sheen SS, Park JH, Hwang YI, Kim SH, Yoon HI, Lim SC, Park JY, Park SJ, et al. Prevalence of chronic obstructive pulmonary disease in Korea: the fourth Korean National Health and Nutrition Examination Survey, 2008. Respirology. 2011;16:659–665. doi: 10.1111/j.1440-1843.2011.01951.x. [DOI] [PubMed] [Google Scholar]
- 5.Cho SH, Park HW, Rosenberg DM. The current status of asthma in Korea. J Korean Med Sci. 2006;21:181–187. doi: 10.3346/jkms.2006.21.2.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Global Initiative for Asthma. Global strategy for asthma management and prevention [Internet] [accessed on 19 May 2015]. Available at http://www.ginasthma.com.
- 7.Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease [Internet] [accessed on 21 February 2011]. Available at http://www.goldcopd.org.
- 8.Hartert TV, Togias A, Mellen BG, Mitchel EF, Snowden MS, Griffin MR. Underutilization of controller and rescue medications among older adults with asthma requiring hospital care. J Am Geriatr Soc. 2000;48:651–657. doi: 10.1111/j.1532-5415.2000.tb04723.x. [DOI] [PubMed] [Google Scholar]
- 9.Health Insurance Review and Assessment Service [Internet] [accessed on 3 May 2015]. Available at http://www.hira.or.kr.
- 10.Suissa S, Ernst P, Benayoun S, Baltzan M, Cai B. Low-dose inhaled corticosteroids and the prevention of death from asthma. N Engl J Med. 2000;343:332–336. doi: 10.1056/NEJM200008033430504. [DOI] [PubMed] [Google Scholar]
- 11.Cochrane MG, Bala MV, Downs KE, Mauskopf J, Ben-Joseph RH. Inhaled corticosteroids for asthma therapy: patient compliance, devices, and inhalation technique. Chest. 2000;117:542–550. doi: 10.1378/chest.117.2.542. [DOI] [PubMed] [Google Scholar]
- 12.Cloutier MM, Schatz M, Castro M, Clark N, Kelly HW, Mangione-Smith R, Sheller J, Sorkness C, Stoloff S, Gergen P. Asthma outcomes: composite scores of asthma control. J Allergy Clin Immunol. 2012;129:S24–33. doi: 10.1016/j.jaci.2011.12.980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kon SS, Canavan JL, Jones SE, Nolan CM, Clark AL, Dickson MJ, Haselden BM, Polkey MI, Man WD. Minimum clinically important difference for the COPD assessment test: a prospective analysis. Lancet Respir Med. 2014;2:195–203. doi: 10.1016/S2213-2600(14)70001-3. [DOI] [PubMed] [Google Scholar]
- 14.Kim C, Yoo KH, Rhee CK, Yoon HK, Kim YS, Lee SW, Oh YM, Lee SD, Lee JH, Kim KJ, et al. Health care use and economic burden of patients with diagnosed chronic obstructive pulmonary disease in Korea. Int J Tuberc Lung Dis. 2014;18:737–743. doi: 10.5588/ijtld.13.0634. [DOI] [PubMed] [Google Scholar]
- 15.Hoogendoorn M, Feenstra TL, Hoogenveen RT, Al M, Mölken MR. Association between lung function and exacerbation frequency in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2010;5:435–444. doi: 10.2147/COPD.S13826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.James AL, Palmer LJ, Kicic E, Maxwell PS, Lagan SE, Ryan GF, Musk AW. Decline in lung function in the Busselton Health Study: the effects of asthma and cigarette smoking. Am J Respir Crit Care Med. 2005;171:109–114. doi: 10.1164/rccm.200402-230OC. [DOI] [PubMed] [Google Scholar]
- 17.Vestbo J, Edwards LD, Scanlon PD, Yates JC, Agusti A, Bakke P, Calverley PM, Celli B, Coxson HO, Crim C, et al. Changes in forced expiratory volume in 1 second over time in COPD. N Engl J Med. 2011;365:1184–1192. doi: 10.1056/NEJMoa1105482. [DOI] [PubMed] [Google Scholar]
- 18.Zainudin BM, Lai CK, Soriano JB, Jia-Horng W, De Guia TS, Asthma I, Asthma Insights and Reality in Asia-Pacific (AIRIAP) Steering Committee Asthma control in adults in Asia-Pacific. Respirology. 2005;10:579–586. doi: 10.1111/j.1440-1843.2005.00753.x. [DOI] [PubMed] [Google Scholar]
- 19.Chan-Yeung M, Aït-Khaled N, White N, Ip MS, Tan WC. The burden and impact of COPD in Asia and Africa. Int J Tuberc Lung Dis. 2004;8:2–14. [PubMed] [Google Scholar]
- 20.Dekhuijzen PN, Vincken W, Virchow JC, Roche N, Agusti A, Lavorini F, van Aalderen WM, Price D. Prescription of inhalers in asthma and COPD: towards a rational, rapid and effective approach. Respir Med. 2013;107:1817–1821. doi: 10.1016/j.rmed.2013.09.013. [DOI] [PubMed] [Google Scholar]
- 21.Crane MA, Jenkins CR, Goeman DP, Douglass JA. Inhaler device technique can be improved in older adults through tailored education: findings from a randomised controlled trial. NPJ Prim Care Respir Med. 2014;24:14034. doi: 10.1038/npjpcrm.2014.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lavorini F, Magnan A, Dubus JC, Voshaar T, Corbetta L, Broeders M, Dekhuijzen R, Sanchis J, Viejo JL, Barnes P, et al. Effect of incorrect use of dry powder inhalers on management of patients with asthma and COPD. Respir Med. 2008;102:593–604. doi: 10.1016/j.rmed.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 23.Molimard M, Raherison C, Lignot S, Depont F, Abouelfath A, Moore N. Assessment of handling of inhaler devices in real life: an observational study in 3811 patients in primary care. J Aerosol Med. 2003;16:249–254. doi: 10.1089/089426803769017613. [DOI] [PubMed] [Google Scholar]
- 24.Newman SP. Dry powder inhalers for optimal drug delivery. Expert Opin Biol Ther. 2004;4:23–33. doi: 10.1517/14712598.4.1.23. [DOI] [PubMed] [Google Scholar]
- 25.Lee JK, Yang YH. Evaluation of an education program for patients with asthma who use inhalers. J Korean Acad Nurs. 2010;40:202–212. doi: 10.4040/jkan.2010.40.2.202. [DOI] [PubMed] [Google Scholar]
- 26.Kim SH, Cho SH. Educational and decision-support tools for asthma-management guideline implementation. Asia Pac Allergy. 2012;2:26–34. doi: 10.5415/apallergy.2012.2.1.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Choi JY, Cho Chung HI. Effect of an individualised education programme on asthma control, inhaler use skill, asthma knowledge and health-related quality of life among poorly compliant Korean adult patients with asthma. J Clin Nurs. 2011;20:119–126. doi: 10.1111/j.1365-2702.2010.03420.x. [DOI] [PubMed] [Google Scholar]
- 28.McCarney R, Warner J, Iliffe S, van Haselen R, Griffin M, Fisher P. The Hawthorne effect: a randomised, controlled trial. BMC Med Res Methodol. 2007;7:30. doi: 10.1186/1471-2288-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fox NS, Brennan JS, Chasen ST. Clinical estimation of fetal weight and the Hawthorne effect. Eur J Obstet Gynecol Reprod Biol. 2008;141:111–114. doi: 10.1016/j.ejogrb.2008.07.023. [DOI] [PubMed] [Google Scholar]


