Abstract
Extraskeletal para-articular osteochondromas are rather unusual tumors that arise in the soft tissues adjacent to the joint with no bony or joint continuity. We report a 25-year-old female who presented with a two-year history of right knee mass. Diagnostic imaging revealed a calcifying mass in the Hoffa’s fat pad of the knee. Roentgenographic, magnetic resonance imaging, and histopathologic features are presented.
Abbreviations: MRI, magnetic resonance imaging
Case report
A 25-year-old female presented with a two-year history of right knee mass. She noticed that it was gradually enlarging over the first year; however, there was no change in size during the previous year. She denied any history of trauma to her knee. She also noted that the pain that she felt was localized over the mass and was primarily activity-related. However, she reported occasional night pain that was relieved with anti-inflammatory medications. Physical examination revealed a 3 × 5-cm firm mass in the anterolateral aspect of the proximal tibia that was nonpainful to palpation. Ligamentous knee exam was negative, with stable varus and valgus stress at 0 and 30 degrees, as well as an anterior drawer test. There were no wounds or abrasions about the knee.
Radiographs of the right knee revealed an ovoid calcified mass in the Hoffa’s fat pad. There was no joint effusion, and no evidence of bony attachment to the patella, tibia, or femur (Fig. 1). Magnetic resonance imaging (MRI) of the knee was performed. The T1-weighted coronal image demonstrated an ovoid mass in the Hoffa’s fat pad between the medial femoral condyle and the medial tibial plateau. The mass showed iso-signal intensity to the muscle peripherally, and a lobulated central osseous lesion showed similar signal intensity to the bone, with a surrounding low-signal-intensity component. A T2-weighted sagittal image demonstrated slightly heterogeneous, diffuse, high-signal intensity, with the central lesion showing a low-signal-intensity rim. An axial, precontrast, gradient-echo (GRE) image showed iso-signal intensity of the lesion, with the central portion showing slightly lower signal intensity than the periphery (Fig. 2). Axial and sagittal postcontrast GRE images demonstrated mainly rim enhancement of the mass, with a scattered nodular-enhancing portion internally, and the central portion showed bright diffuse contrast enhancement (Fig. 3).
Fig. 1.
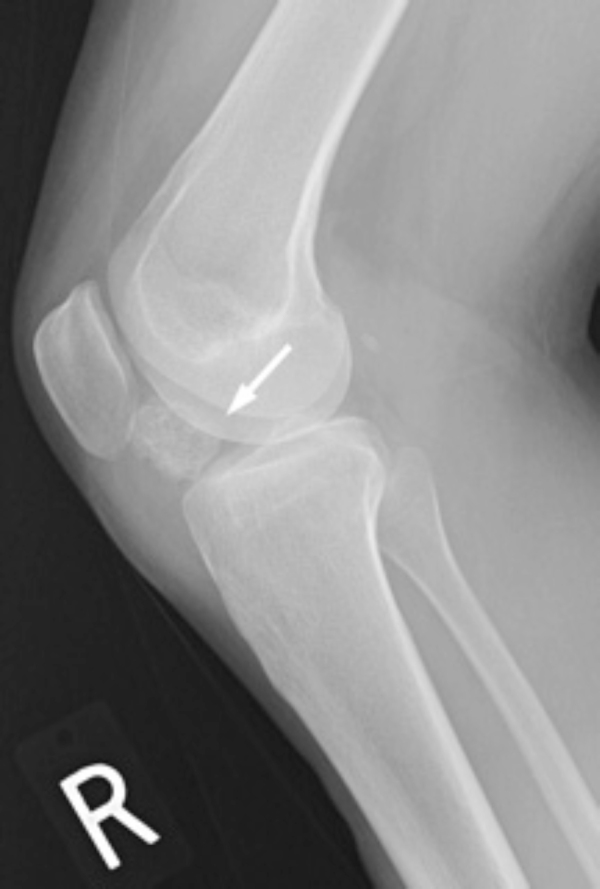
25-year-old woman with an extraskeletal para-articular osteochondroma. Lateral radiograph of the right knee demonstrates an ovoid calcified mass in the Hoffa’s fat pad (arrow).
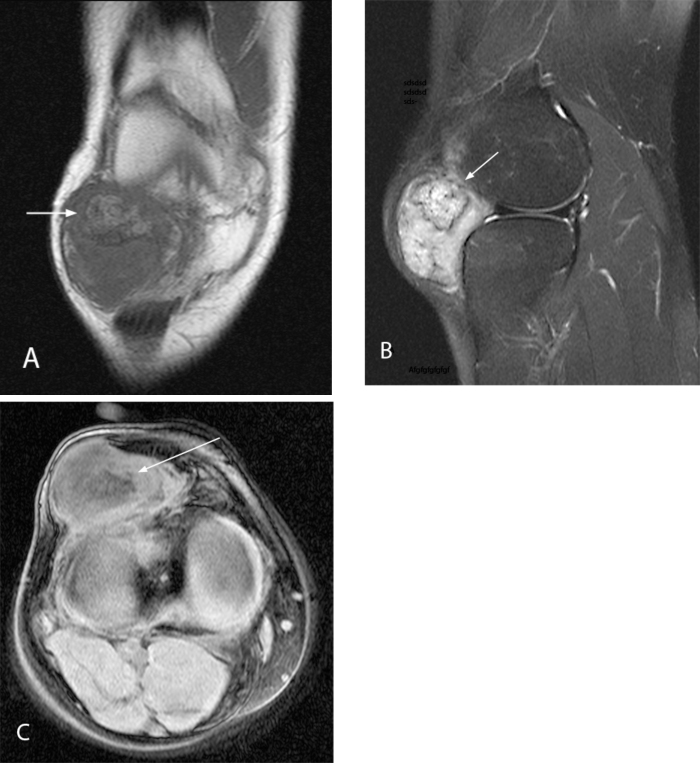
Fig. 2A, B, C.
25-year-old woman with an extraskeletal para-articular osteochondroma. Precontrast coronal T1-weighted (A), sagittal T2-weighted (B), and axial gradient-echo (C) MRI images of the right knee. There is an ovoid mass in the Hoffa’s fat pad. The mass shows iso-signal intensity to the muscle peripherally, and there is a lobulated central osseous lesion that shows similar signal intensity to the bone on T1-weighted image (arrow in A). It shows slightly heterogeneous, diffuse, high signal intensity, with the central lesion showing a low signal intensity rim on T2-weighted image (arrow in B). Axial precontrast gradient-echo (GRE) image shows iso-signal intensity of the lesion, with the central portion showing slightly lower signal intensity than the periphery (arrow in C).
Fig. 3A & B.
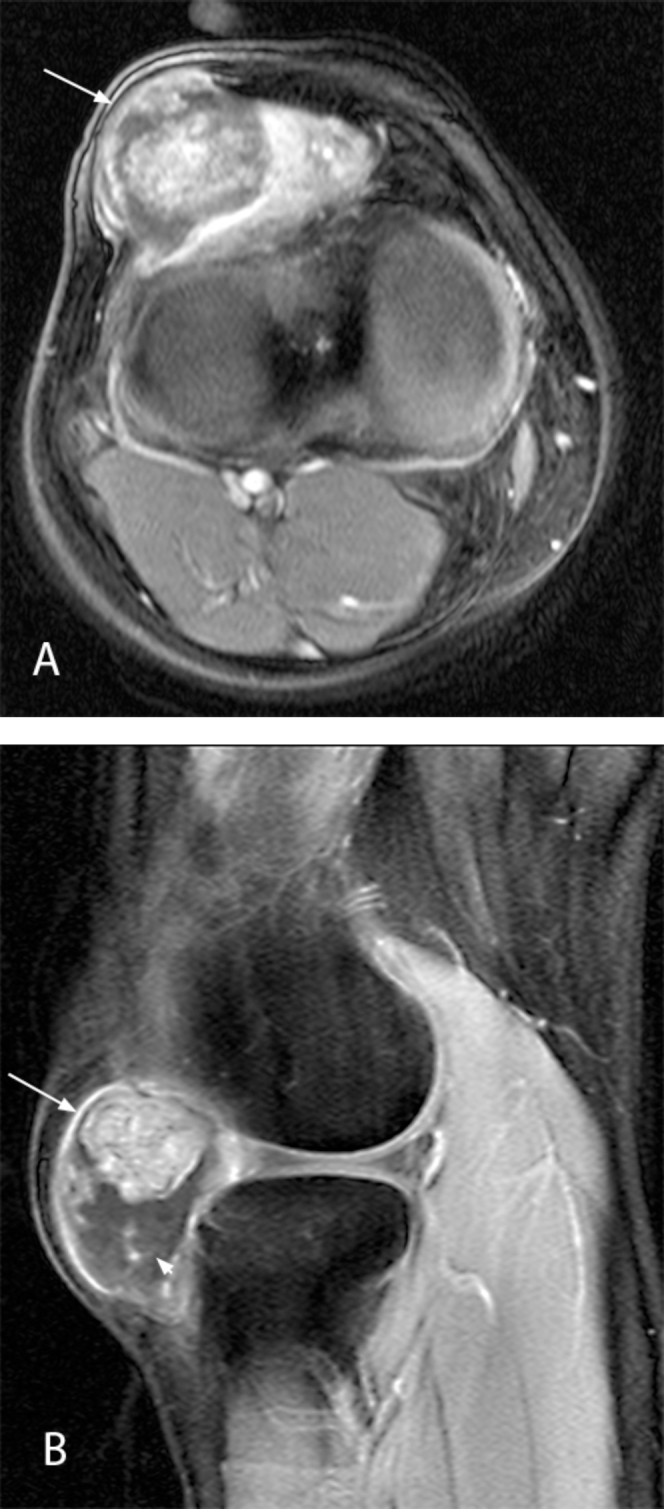
25-year-old woman with an extraskeletal paraarticular osteochondroma. Post-contrast axial (A) and sagittal (B) gradient-echo images of the right knee. The mass shows mainly rim enhancement (arrow in A and B) with scattered nodular enhancing portion (arrowhead in B) internally, and the central portion shows bright diffuse contrast enhancement.
Marginal excision was performed. The mass was quite large and firm at approximately 6 cm, and it had extensive displacement of soft tissues anterior to the right knee capsule. There was a dense attachment to the tissues immediately adjacent to the tibial plateau and the coronary ligament of the meniscus. The knee joint was not invaded by the lesion. Macroscopic examination revealed a 5.5 × 4.5 × 3.0-cm tan, fibrous, centrally indurated mass. When sectioned, the specimen showed white, cartilaginous, edematous cut surfaces with a central portion of trabeculated, cancellous, congested bone, 2.4 cm in greatest dimension. On microscopic examination, the lesion was composed of a nodular rim of cartilaginous matrix ranging from myxoid to hyaline cartilage. Some areas also had the appearance of fibrocartilage. There was extensive endochondral ossification of the cartilage to mature-appearing trabecular bone (Fig. 4). The intertrabecular space was composed of reactive fibrovascular stroma and mature fatty marrow. In addition, there was focal osteonecrosis of the trabecular bone. The pathological features were diagnostic of extraskeletal para-articular osteochondroma.
Fig. 4A & B.
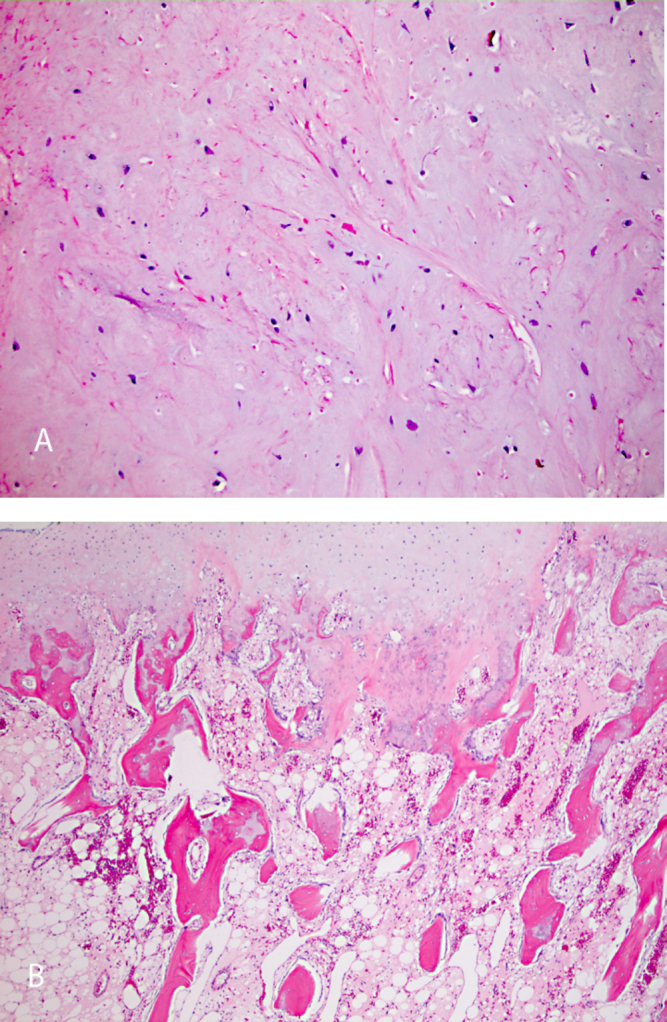
25-year-old woman with an extraskeletal paraarticular osteochondroma. The cartilage matrix of the lesion was composed of hyaline cartilage or fibrocartilage as evidenced by eosinophilic collagen fibers within the matrix. Some areas had poorly formed myxoid cartilage (A). Endochondral ossification of the peripheral rim of cartilage (top) to mature trabecular bone with fatty marrow is characteristic of para-articular osteochondroma (B).
Discussion
Osteochondromas represent the most common bone tumors and are considered hyperplastic–dysplastic developmental lesions of the growth plate rather than true neoplasms. They constitute 20% to 50% of all benign bone tumors and 10% to 15% of all bone tumors (1). However, extraskeletal osteochondromas are uncommon; most arise from synovial tissues in joints, tendon sheaths, or bursae in the hands and feet. The paratenon has characteristics of, and is often considered equivalent to, synovial tissue (tenosynovium) (2). The fact that a cartilage proliferation undergoing endochondral ossification has common pathological features results in similar, and often confusing, descriptive terminology. However, extraskeletal osteochondromas represent a separate osteochondromatous tumor that is clinicopathologically and biologically distinct from skeletal osteochondromas.
Intracapsular and para-articular chondromas have been named capsular osteomas, osteochondromas, or chondromas, depending on the relative proportions of bone and cartilage (3). Para-articular chondromas, also known as intracapsular chondromas, are one of the three variants of extraskeletal chondromatous proliferations: soft-tissue chondromas, synovial chondromatosis, and para-articular chondromas (4). They arise from the capsule and/or connective tissue adjacent to the capsule and are due to cartilaginous metaplasia. If the metaplasia progresses to ossification, the term para-articular osteochondroma may be used (3). The most frequently involved joint is the knee (4).
The concept of para-articular osteochondroma was first introduced in 1958 by Jaffe, who used the synonymous terms para-articular chondromas and intracapsular chondromas to describe osteochondral metaplasia occurring in fibrous joint capsule or soft tissue adjacent to the joint (5). However, it was Milgram et al. who first used the term para-articular osteochondroma and differentiated these lesions from synovial osteochondromatosis (6, 7). In a subsequent publication, Milgram et al. justified the use of the term para-articualar osteochondroma, as opposed to Jaffe’s term para-articular chondroma, noting that the former term more appropriately describes the overall morphologic features of the lesion (7). Reith et al. proposed the following criteria for a lesion to be diagnosed as para-articular osteochondroma in 1997: (A) the lesion presents as a single, dominant mass, both radiographically and grossly; (B) the mass consists histopathologically of both bone and cartilage, organized in a manner similar to conventional osteochondromas; and (C) the lesion is not intra-articular, that is, it does not arise within the synovial lining of a joint (8).
The pathogenesis of these lesions is unclear. Metaplasia from mesenchymal cells may be considered their origin (2). Pathologic examination of para-articular osteochondromas is quite characteristic. Grossly, these tumors are characterized by a solitary mass composed of multiple osteochondral nodules. Histologically, the peripheral portion of each nodule contains the cartilaginous areas, whereas the central portion contains lamellar, trabecular bone. Endochondral ossification usually is evident at the interface between the cartilage and bone. The overall configuration of each nodule is very similar to a conventional osteochondroma (8). However, the quality of the cartilaginous matrix seems to vary more than in conventional osteochrondroma, which has a pure hyaline cartilage cap.
The plain radiographs demonstrate a large soft-tissue mass with a wide central radiodensity due to central ossification. On MRI, this central ossified area shows radiological features of fatty tissue due to the presence of a high proportion of fatty bone marrow among the bone trabeculae. Areas of low signal intensity on T1-weighted images and of high signal intensity on T2-weighted images with contrast enhancement correspond to the hyaline cartilaginous tumor tissue (4).
The infrapatellar (Hoffa’s) fat pad (IFP) is an intracapsular extrasynovial structure. It is bordered by the inferior pole of the patella superiorly, the joint capsule and patellar tendon anteriorly, the proximal tibia and deep infrapatellar bursa inferiorly, and the synovium-lined joint cavity posteriorly. The fat pad is tethered to the intercondylar notch superiorly by the infrapatellar synovial fold or plica ligamentum mucosum (9). It also is attached directly to the periosteum of the tibia (9). The interface between the posterior aspect of the fat pad and the adjacent joint space consists of several synovial recesses separated by fat projections (10). It is not surprising, therefore, that synovial-based pathology may occur de novo within Hoffa’s fat pad and does not always represent an extension from the synovial-lined knee joint (11).
Radiologically, para-articular osteochondromas must be considered in the differential diagnosis of radiological calcified/ossified soft-tissue lesions about the Hoffa’s fat pad, such as old hematomas, calcifying bursitis, tumoral calcinosis, myositis ossificans, crystal deposition disease, calcified synovial sarcomas, primary synovial chondromatosis, and synovial chondrosarcoma.
Para-articular osteochondromas have a characteristic morphology but may be easily confused with other osteochondral lesions if care is not taken to correlate the histologic and radiologic findings. Because marginal excision is adequate management (12), it is important to distinguish the para-articular osteochondroma from other lesions such as chondrosarcoma and synovial chondromatosis.
Footnotes
Published: November 26, 2010
References
- 1.Murphey MD, Choi JJ, Kransdorf MJ, Flemming DJ, Gannon FH. Imaging of osteochondroma: variants and complications with radiologic-pathologic correlation. Radiographics. 2000;20:1407–1434. doi: 10.1148/radiographics.20.5.g00se171407. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Maheshwari AV, Jain AK, Dhammi IK. Extraskeletal paraarticular osteochondroma of the knee–a case report and tumor overview. Knee. 2006;13:411–414. doi: 10.1016/j.knee.2006.05.008. [PubMed] [DOI] [PubMed] [Google Scholar]
- 3.Sakai H, Tamai K, Iwamoto A, Saotome K. Para-articular chondroma and osteochondroma of the infrapatellar fat pad: a report of three cases. Int Orthop. 1999;23:114–117. doi: 10.1007/s002640050322. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gonzalez-Lois C, Garcia-de-la-Torre P, SantosBriz-Terron A, Vila J, Manrique-Chico J, Martinez-Tello J. Intracapsular and para-articular chondroma adjacent to large joints: report of three cases and review of the literature. Skeletal Radiol. 2001;30:672–676. doi: 10.1007/s002560100398. [PubMed] [DOI] [PubMed] [Google Scholar]
- 5.Jaffe H. Tumors and tumorous conditions of the bones and joints. Lea & Febiger; Philadelphia: 1958. pp. 567–569. [Google Scholar]
- 6.Milgram JW, Dunn EJ. Para-articular chondromas and osteochondromas: a report of three cases. Clin Orthop Relat Res. 1980:147–151. [PubMed] [PubMed] [Google Scholar]
- 7.Milgram JW, Jasty M. Case report 238: para-articular osteochondroma of the knee. Skeletal Radiol. 1983;10:121–125. doi: 10.1007/BF00360797. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Reith JD, Bauer TW, Joyce MJ. Paraarticular osteochondroma of the knee: report of 2 cases and review of the literature. Clin Orthop Relat Res. 1997:225–232. [PubMed] [PubMed] [Google Scholar]
- 9.Hoffa A. The influence of adipose tissue with regard to the pathology of the knee joint. J Am Med Assoc. 1904;43:795–796. [Google Scholar]
- 10.Jacobson JA, Lenchik L, Ruhoy MK, Schweitzer ME, Resnick D. MR imaging of the infrapatellar fat pad of Hoffa. Radiographics. 1997;17:675–691. doi: 10.1148/radiographics.17.3.9153705. [PubMed] [DOI] [PubMed] [Google Scholar]
- 11.Saddik D, McNally EG, Richardson M. MRI of Hoffa's fat pad. Skeletal Radiol. 2004;33:433–444. doi: 10.1007/s00256-003-0724-z. [PubMed] [DOI] [PubMed] [Google Scholar]
- 12.Mosher JF, Jr., Kettelkamp DB, Campbell CJ. Intracapsular or para-articular chondroma. A report of three cases. J Bone Joint Surg Am. 1966;48:1561–1569. [PubMed] [PubMed] [Google Scholar]