Abstract
Gallium-67 citrate has long been used for imaging of infection and inflammation. Although gallium-67 uptake due to silicone implants and silicone injections has been previously reported in the literature, very few cases are documented. We report a case of increased gallium-67 uptake in the buttocks in a patient who previously received silicone injections in the buttocks, to reemphasize silicone augmentation as a potential source of gallium-67 uptake. In addition, we present a F-18-fluorodeoxyglucose (FDG) PET/CT scan from the same patient to demonstrate mild diffuse FDG uptake in the buttocks in the region of previous silicone injection. Although FDG is well known to accumulate in areas of inflammation such as prior sites of silicone injection or silicone implantation in the breast, FDG uptake in the buttocks due to silicone injections has not been previously reported or correlated with a gallium scan.
Abbreviations: CT, computed tomography; 18F-FDG PET/CT, fusion fluorine-18 fluorodeoxyglucose positron-emission tomography and computed tomography
Case report
A 48-year-old HIV-positive male underwent FDG PET/CT due to elevated lactate dehydrogenase and suspected malignancy. The PET/CT scan demonstrated no evidence of active neoplastic process; however, there was mild diffuse FDG uptake in the gluteal area with a maximum standardized uptake value (SUV) of 2.2 (Figure 1A, Figure 1B, Figure 1C). Five months later, the patient presented with shortness of breath and recurrent fever. Chest X-ray demonstrated no evidence of infection (Fig. 2). A subsequent gallium scan showed no evidence of pneumocystis carinii pneumonia (PCP) or other source of infection. Transient focal gallium-67 concentration seen in the left pelvis was consistent with physiologic excretion of tracer in the bowel (Figure 3, Figure 4). Incidentally noted was moderate diffuse gallium-67 concentration in the gluteal area bilaterally. Upon questioning, the patient revealed that he had received subcutaneous silicone injections in the buttocks ten years prior. The patient denied any current local symptoms such as pain or swelling in the buttocks.
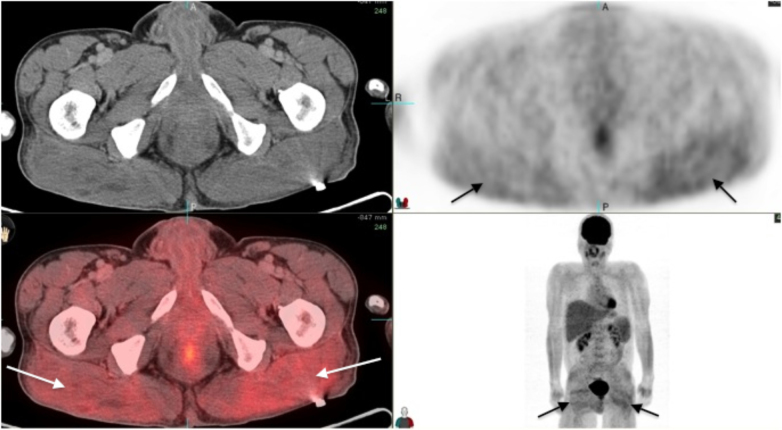
Figure 1A.
48-year-old HIV-positive male with silicone granulomas. Axial PET/CT images. PET (upper right), CT (upper left), fused PET/CT (lower left), and maximum-intensity projection (lower right) images demonstrate diffuse mild FDG uptake in the gluteal area (arrows) with maximum SUV of 2.2.
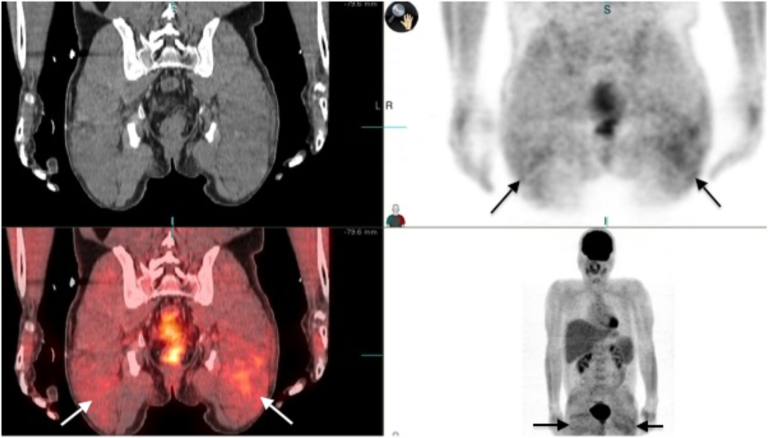
Figure 1B.
48-year-old HIV-positive male with silicone granulomas. Coronal PET/CT images. PET (upper right), CT (upper left), fused PET/CT (lower left), and maximum-intensity projection (lower right) images demonstrate diffuse mild FDG uptake in the gluteal area (arrows) with maximum SUV of 2.2.
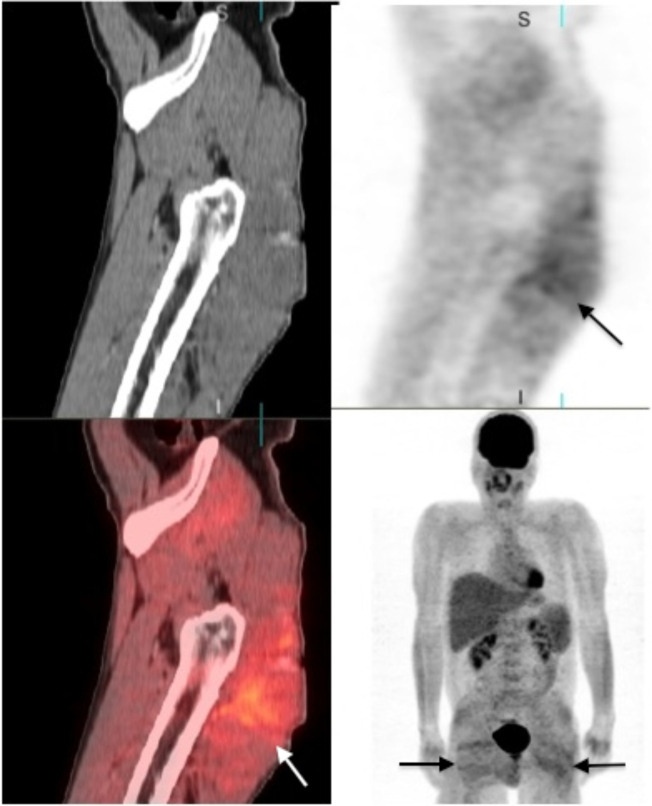
Figure 1C.
48-year-old HIV-positive male with silicone granulomas. Sagittal PET/CT images. PET (upper right), CT (upper left), fused PET/CT (lower left), and maximum-intensity projection (lower right) images demonstrate diffuse mild FDG uptake in the gluteal area (arrows) with maximum SUV of 2.2.
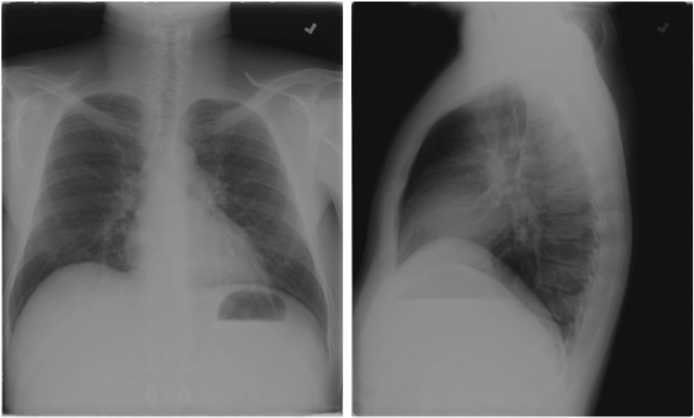
Figure 2.
48-year-old HIV-positive male with silicone granulomas. PA (left ) and lateral (right) chest X-rays demonstrate clear lungs with no evidence of pleural effusion.
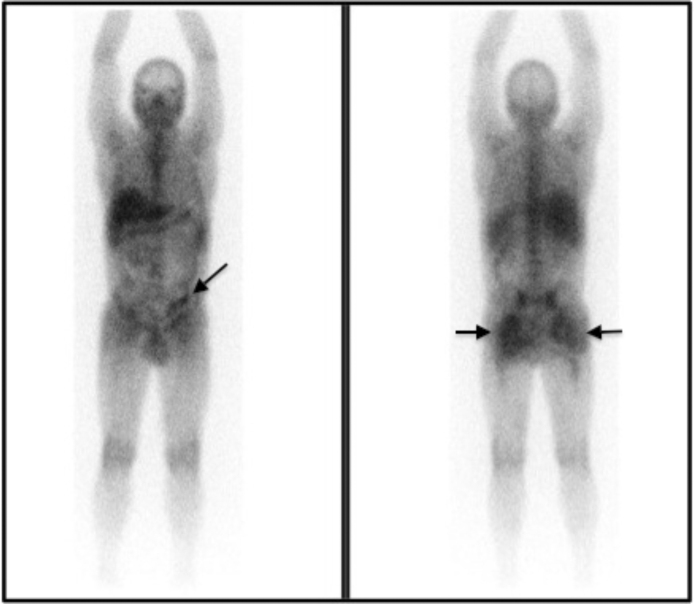
Figure 3.
48-year-old HIV-positive male with silicone granulomas. Anterior (left) and posterior (right) projections from gallium scan acquired 48 hours after the intravenous administration of 6.1 mCi of gallium-67 citrate demonstrate physiologic tracer uptake in the chest without evidence of PCP. In addition, there is moderate diffuse tracer uptake in the gluteal area bilaterally (arrows). Focal tracer concentration in the left pelvis that resolved on followup imaging (Fig. 4) is consistent with physiologic excretion of tracer in the bowel (arrow).
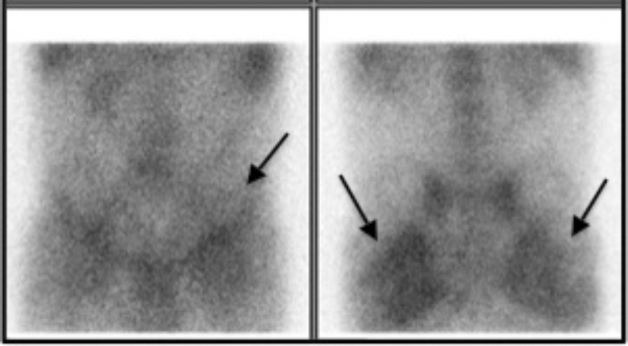
Figure 4.
48-year-old HIV-positive male with silicone granulomas. Anterior (left) and posterior (right) spot images from gallium scan acquired 72 hours after the intravenous administration of 6.1 mCi of gallium-67 citrate demonstrate clearance of tracer from the left pelvis (arrow), consistent with physiologic bowel excretion of tracer. In addition, there is persistent bilateral soft-tissue tracer uptake in the gluteal region bilaterally (arrows).
Discussion
Prior to its ban by the FDA in 1992, silicone was used with much success to treat wrinkles and to enhance the lips, cheekbones, chin, breasts, hips, and buttocks (1, 2). Although the FDA recognized and warned of the side effects of silicone injection at that time, it was still practiced on the black market and in plastic surgeons' offices (3, 4). Although the ban on silicone was removed by the FDA in 2006, its safety remains controversial (1). The most notable side effects of silicone injection include granulomatous, inflammatory responses (the so-called “siliconoma”), silicone migration, excessive collagen formation, necrosis, and silicone embolism (3, 4, 5, 6, 7). As a radiologist or nuclear medicine physician, one must be aware of these potential effects of silicone to prevent misinterpretation of gallium scans or FDG PET/CT scans.
Gallium-67 uptake at the site of prior silicone implants and silicone injections has been previously reported in the literature (8, 9). This case demonstrates increased gallium uptake in the buttocks of a patient with prior silicone injections in this region, to re-emphasize silicone injections and silicone implants as a potential cause of increased gallium-67 uptake. In addition, we correlate our patient’s gallium scan with a F-18-fluorodeoxyglucose (FDG) PET/CT to emphasize that increased FDG uptake may also be seen in the setting of prior silicone injections in the buttocks or elsewhere in the body. Because previous case reports demonstrating Ga-67 uptake due to silicone injections in the buttocks were published before the clinical use of PET/CT, correlation with PET/CT was not available at that time (8, 9, 10).
Gallium-67 citrate has long been used for imaging of infection and inflammation. The mechanism of gallium uptake at the inflammatory site of prior silicone injections is well understood. Although potential causes of inflammation are numerous, the mechanism of gallium localization to sites of inflammation usually relies on locally increased blood flow and increased vascular permeability at sites of inflammation, regardless of the cause. An additional factor that promotes Ga-67 localization to regions of inflammation is its ferric-ion-like properties. Ga-67 has a high affinity for and binds to lactoferrin, which is released by leukocytes at inflammatory sites (11, 12).
In our patient, the diffuse, bilateral Ga-67 uptake in the gluteal area led us to suspect silicone injections as a cause of Ga-67 uptake. In addition, absence of local signs such as erythema or pain argued against an acute infectious process such as phlegmon or abscess formation. Other causes of increased gallium uptake such as lymphoma were also unlikely due to the location and diffuse, symmetric tracer uptake (11, 12).
In addition to causing increased tracer uptake on gallium scan, it is well known that the inflammatory granulomatous response following silicone injections can cause increased FDG uptake on PET/CT (10, 11, 12). Previous studies have shown that SUVs may vary greatly in the setting of inflammation and can be very high (5, 11, 12). The most important concept for physicians to recognize is that focally increased FDG uptake at the site of prior silicone injections may cause false-positive results by mimicking tumor (10). This is particularly important in the breast (10). FDG uptake in the breast after silicone implant or injection may mimic a new primary breast tumor, recurrent breast tumor in a patient with previous disease, or positive lymph nodes (10, 13). Migration of silicone into the lymphatics after injection can also cause false-positive interpretation at sites that are remote from the initial silicone injection site (10, 13, 14). With regard to subcutaneous silicone injection in the buttocks, diffuse symmetric FDG uptake in the gluteal area has to be differentiated from exercise- or insulin-related muscle uptake, which usually involves multiple muscle groups. In addition, focally increased FDG uptake in the buttocks may be mistaken for sarcoma, connective-tissue tumor, or abscess (11, 12).
An additional point is the patient population where silicone injections in the hips and in the gluteal area have previously been reported. Some of the previous reports of silicone injection for breast, hip, or gluteal augmentation were in transgender patients undergoing male-to-female sex change (7). Focused patient history related to the scan findings may explain causes of increased radiotracer uptake on gallium scan or FDG PET/CT. Frequently, the patients may be reluctant to reveal this history (15).
Lastly, we would like to address the persistence of increased tracer uptake on gallium and FDG PET/CT scan for many years after silicone injection. Our case report and prior case reports have demonstrated increased Ga-67 uptake up to ten years following silicone injections (8, 9). As per Ho et al., granulomatous reactions may occur from three weeks to twenty years after silicone injection (10). Therefore we can conclude that the increased Ga-67 and FDG uptake due to silicone injections can be visualized for at least ten years and perhaps longer (8).
In conclusion, we report this case to emphasize that silicone injections are a potential cause of increased radiotracer uptake on gallium scans and FDG PET/CT. Such knowledge will prevent false-positive and false-negative scan interpretation (5). In addition, we stress that silicone injections are frequently seen in transsexual patients as well in other patients who have sought to augment their physical appearance (3). Lastly, we reiterate that diffuse and/or symmetrical radiotracer uptake on gallium or PET/CT without clinical evidence of infection favors a granulomatous response (“siliconoma”) in the presence of a history of silicone injection.
Footnotes
Published: March 29, 2011
References
- 1.Hajdu S.D., Agmon-Levin N., Shoenfeld Y. Silicone and autoimmunity. Eur J Clin Invest. 2010 doi: 10.1111/j.1365-2362.2010.02389.x. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Spear S.L., Jespersen M.R. Breast implants: saline or silicone? Aesthet Surg J. 2010;30(4):557–570. doi: 10.1177/1090820X10380401. [PubMed] [DOI] [PubMed] [Google Scholar]
- 3.Bruner T.W., Roberts T.L., 3rd, Nguyen K. Complications of buttocks augmentation: diagnosis, management, and prevention. Clin Plast Surg. 2006;33(3):449–466. doi: 10.1016/j.cps.2006.04.005. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Price E.A., Schueler H., Perper J.A. Massive systemic silicone embolism: a case report and review of literature. Am J Forensic Med Pathol. 2006;27(2):97–102. doi: 10.1097/01.paf.0000188072.04746.d5. [PubMed] [DOI] [PubMed] [Google Scholar]
- 5.Chen C.J. A false positive F-FDG PET/CT scan caused by breast silicone injection. Korean J Radiol. 2009;10(2):194–196. doi: 10.3348/kjr.2009.10.2.194. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clark R.F. Subcutaneous silicone injection leading to multi-system organ failure. Clin Toxicol (Phila) 2008;46(9):834–837. doi: 10.1080/15563650701850025. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Schmid A. Silicone embolism syndrome: a case report, review of the literature, and comparison with fat embolism syndrome. Chest. 2005;127(6):2276–2281. doi: 10.1378/chest.127.6.2276. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Decorato D., Derogatis A.J. Prominent gallium uptake associated with silicone implants in an asymptomatic patient. Clin Nucl Med. 1994;19(12):1107–1108. doi: 10.1097/00003072-199419120-00018. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.Palestro C.J., Chau P., Goldsmith S.J. Gallium-67 uptake after breast and hip augmentation with silicone. Clin Nucl Med. 1992;17(11):897–898. doi: 10.1097/00003072-199211000-00015. [PubMed] [DOI] [PubMed] [Google Scholar]
- 10.Ho L., Wassef H., Seto J. FDG PET/CT imaging in granulomatous changes secondary to breast silicone injection. Clin Radiol. 2010;65(8):659–661. doi: 10.1016/j.crad.2010.02.011. [PubMed] [DOI] [PubMed] [Google Scholar]
- 11.Ziessman H.A., O'Malley J.P., Thrall J.H. Nuclear medicine: the requisites. Requisites in radiology. 3rd ed. Mosby Elsevier; Philadelphia: 2006. p. 580. xii. [Google Scholar]
- 12.Mettler F.A., Guiberteau M.J. Essentials of nuclear medicine imaging. 5th ed. Saunders/Elsevier; Philadelphia, Pa.: 2006. p. 577. xi. [Google Scholar]
- 13.Patel C.N., Macpherson R.E., Bradley K.M. False-positive axillary lymphadenopathy due to silicone granuloma on FDG PET/CT. Eur J Nucl Med Mol Imaging. 2010 doi: 10.1007/s00259-010-1607-x. [PubMed] [DOI] [PubMed] [Google Scholar]
- 14.Altmeyer M.D., Anderson L.L., Wang A.R. Silicone migration and granuloma formation. J Cosmet Dermatol. 2009;8(2):92–97. doi: 10.1111/j.1473-2165.2009.00436.x. [PubMed] [DOI] [PubMed] [Google Scholar]
- 15.Schwartzfarb E.M. Foreign body granuloma formation secondary to silicone injection. Dermatol Online J. 2008;14(7):20. [PubMed] [PubMed] [Google Scholar]