Abstract
Bowler’s thumb is a rare perineural fibrosis involving the ulnar digital nerve of the thumb. Affected patients present with pain, neuropathy, and mass lesion. The condition is caused by chronic repetitive impaction of the ulnar soft tissues of the thumb against the thumbhole of a bowling ball. In our case, MRI showed decreased signal intensity on both T1- and T2-weighted images surrounding an enlarged ulnar digital nerve of the thumb. The findings can be confused with giant-cell tumor of the tendon sheath or peripheral-nerve-sheath tumor.
Abbreviations: MRI, magnetic resonance imaging
Case report
A 27-year-old, left-hand-dominant man with a long history of avid bowling presented to the Orthopedic Surgery Clinic complaining of pain, numbness, and a thumb mass. On physical examination, a small, tender, mobile mass was identified at the ulnar aspect of the thumb at the level of the proximal phalanx. Steroid and anesthetic injection did not provide any relief.
An MRI of the thumb was performed. A fusiform mass was identified at the medial aspect of the thumb (Fig. 1), measuring 1.2 × 1.2 × 2.3 cm, that demonstrated intermediate signal on T1-weighted images and very low signal on fat-saturated T2-weighted images. The mass was located in the expected region of the ulnar digital nerve, and the nerve was enlarged. A differential diagnosis of perineural fibrosis, giant-cell tumor of the tendon sheath, and peripheral-nerve-sheath tumor was given at the time of image interpretation.
Figure 1.
A. Axial T1-weighted image of the thumb (TR=500, TE 12) at the level of the proximal phalanx shows an intermediate signal mass in the ulnar soft tissues (arrows). B. T1-weighted axial image through the thumb just distal to the mass shows an enlarged digital nerve (arrowhead) compared to the normal radial digital nerve (open arrow). C. The tubular configuration of the mass (arrows) can be seen on T1-weighted coronal image through the thumb. D. The mass (arrows) is very low in signal on fat-saturated FSE T2-weighted (TR=5500, TEeff=90) axial image.
The patient was taken to surgery because he did not respond to conservative therapy after a clinical diagnosis of Bowler’s Thumb. At surgery, the ulnar digital nerve was markedly enlarged secondary to perineural fibrosis (Fig. 2). Definitive surgical therapy consisted of neurolysis with careful removal of perineural fibrotic tissue. The patient had an uneventful postoperative course and was able to eventually return to bowling.
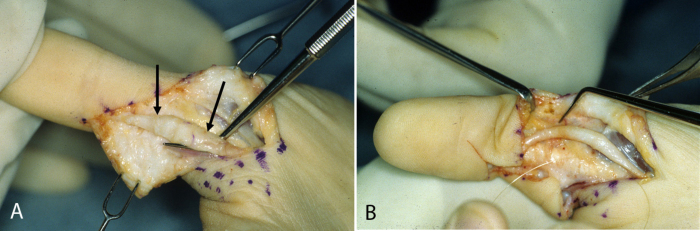
Figure 2.
A. Enlarged ulnar digital nerve (arrows) is surrounded by perineural fibrosis producing irregular rather than normal smooth contour. B. The nerve is smaller and has a smoother contour following neurolysis.
Discussion
Bowler’s thumb was first reported by Siegel in 1965 (1), and it is an uncommon disease given the popularity of bowling. This condition is a neuropathy induced by recurrent compression of the ulnar digital nerve by the thumbhole of a bowling ball in avid bowlers. Chronic excessive pressure on the digital nerve leads to perineural fibrosis, pain, and numbness (2, 3). While this condition is usually related to chronic activity, traumatic injury of the ulnar digital nerve from a single episode of bowling has been described (4).
On presentation, patients with bowler’s thumb may complain of hypesthesia, paresthesia, and numbness. A mass is detectable on clinical examination in almost all cases (2). The mass is usually mobile, and thickening of the digital nerve may also be appreciated. A positive Tinel’s sign, callous formation, or skin atrophy may also be seen. Nerve conduction studies may be abnormal (5).
Very few reports of the MRI appearance of bowler’s thumb exist because it is a clinical diagnosis. It is no surprise that this process shares MRI features with Morton neuroma. Both conditions are pathologically related to perineural fibrosis rather than to true neuromas. The perineural fibrosis in both entities is low to intermediate in signal on T1- and T2-weighted images. In fact, the signal on T2-weighted images is so low that the mass might not be identifiable on fat-suppressed imaging. Although intravenous gadolinium was not used in our case, avid enhancement is predicted. A recent study has suggested that MRI of this condition is clinically useful; the authors feel that preoperative distinction between nodular neuroma and epineural fibrosis forms of the disease is important (6).
A good clinical history and recognition of enlargement of the digital nerve should permit accurate characterization of the perineural fibrosis of bowler’s thumb. The differential diagnosis may include peripheral-nerve-sheath tumor and giant-cell tumor of the tendon sheath. Peripheral-nerve-sheath tumor of a digital nerve is uncommon (7), and these lesions are characteristically higher in signal on T2-weighted images than they are in the case of perineural fibrosis. The masslike presentation and low T2 signal may cause confusion with giant-cell tumor of the tendon sheath, but this process should not cause enlargement of the digital nerve.
Perineural fibrosis of a digital nerve is not isolated to bowlers. It can be seen in any vocation or avocation that exposes the nerve to chronic repetitive pressure and has been described in cherry pickers (8), martial artists (9), and in association with orthopedic splints (8, 10). Treatment of bowler’s thumb is usually conservative. Nonoperative interventions such as avoidance of bowling, beveled holes in the bowling ball, more distant placement of the ball thumbhole (so that only the distal phalanx can enter the ball), and thumb guards have been used with success. Operative interventions are reserved for individuals who fail conservative therapy. Neurolysis (2) and transposition of the nerve (11) are surgical options.
Footnotes
Published: January 31, 2011
References
- 1.Siegel IM. Bowling-thumb neuroma. JAMA. [Letter to editor] 1965;192(3):263. [Google Scholar]
- 2.Dobyns JH, O'Brien ET, Linscheid RL, Farrow GM. Bowler's thumb: diagnosis and treatment. A review of seventeen cases. J Bone Joint Surg Am. 1972;54(4):751–755. [PubMed] [PubMed] [Google Scholar]
- 3.Howell AE, Leach RE. Bowler's thumb. Perineural fibrosis of the digital nerve. J Bone Joint Surg Am. 1970;52(2):379–381. [PubMed] [PubMed] [Google Scholar]
- 4.Ostrovskiy D, Wilbourn A. Acute bowler's thumb. Neurology. 2004;63(5):938. doi: 10.1212/01.wnl.0000137110.18160.9e. [PubMed] [DOI] [PubMed] [Google Scholar]
- 5.Nasr JT, Kaufman MA. Electrophysiologic findings in two patients with digital neuropathy of the thumb. Electromyogr Clin Neurophysiol. 2001;41(6):353–356. [PubMed] [PubMed] [Google Scholar]
- 6.Muramatsu K, Yoshida K, Taguchi T. Two different types of bowler's thumb. Orthopedics. 2009;32(7):525. doi: 10.3928/01477447-20090527-22. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Basheer H, Rabia F, Basheer H, el-Helw K. Neurofibromas of digital nerves. J Hand Surg Br. 1997;22(1):61–63. doi: 10.1016/s0266-7681(97)80019-8. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Viegas SF, Torres FG. Cherry pitter's thumb. Case report and review of the literature. Orthop Rev. 1989;18(3):336–338. [PubMed] [PubMed] [Google Scholar]
- 9.Chiu DT. “Karate kid” finger. Plast Reconstr Surg. 1993;91(2):362–364. [PubMed] [PubMed] [Google Scholar]
- 10.Rayan GM, O'Donoghue DH. Ulnar digital compression neuropathy of the thumb caused by splinting. Clin Orthop Relat Res. May 1983;175:170–172. [PubMed] [PubMed] [Google Scholar]
- 11.De Smet L, Van Ransbeeck H, Fabry G. Bowler's thumb treated by translocation of the digital nerve. Acta Orthop Belg. 1999;65(3):367–368. [PubMed] [PubMed] [Google Scholar]