Abstract
Rationale
The highly prevalent obstructive sleep apnea syndrome (OSA) with its main component intermittent hypoxia (IH) is a risk factor for cardiovascular mortality. The poor knowledge of its pathophysiology has limited the development of specific treatments, whereas the gold standard treatment, continuous positive airway pressure, may not fully reverse OSA chronic consequences and has limited acceptance in some patients.
Objectives
To examine the contribution of IH-induced inflammation to OSA cardiovascular complications.
Methods
We investigated systemic and vascular inflammatory changes in C57BL6 mice exposed to IH (21–5% FiO2, 60s cycle) or normoxia, 8h/day up to 14 days. Vascular alterations were reassessed in mice treated with a blocking antibody of RANTES/CCL5 signaling pathway, or with the IgG isotype control throughout the IH exposure.
Measurement and Main Results
IH induced systemic inflammation combining increased splenic lymphocyte proliferation and chemokine expression, with early and predominant RANTES/CCL5 alterations, and enhanced splenocyte migration toward RANTES/CCL5. IH also induced structural and inflammatory vascular alterations. Leukocyte-endothelium adhesive interactions were increased, attested by leukocyte rolling and ICAM-1 expression in mesenteric vessels. Aortas had increased intima-media thickness with elastic fiber alterations, mucoid depositions, NFkB-p50 and ICAM-1 overexpression, hypertrophy of smooth-muscle cells overexpressing RANTES/CCL5, and adventitial-periadventitial T-lymphocyte infiltration. RANTES/CCL5 neutralization prevented both intima-media thickening and inflammatory alterations, independently of the IH-associated proatherogenic dyslipidemia.
Conclusions
Inflammation is a determinant mechanism for IH-induced pre-atherosclerotic remodeling, involving RANTES/CCL5, a key chemokine in atherogenesis. Characterization of the inflammatory response could allow identifying at-risk patients for complications, and its pharmacological manipulation may represent a potential complementary treatment of sleep apnea consequences.
Keywords: Animals; Anoxia; Mice, Inbred C57BL; Microscopy; Sleep Apnea Syndromes; Transcription, Genetic; Tunica Intima; Aorta; Atherosclerosis; Chemokine CCL5; Disease Models, Animal; Inflammation; Male; Mesenteric Arteries; Mice
INTRODUCTION
Obstructive sleep apnea (OSA) is a worldwide public-health problem, affecting at least 5% of the general population and characterized by repetitive upper airway collapse during sleep leading to intermittent hypoxia (IH) (1). OSA is recognized as a cardiovascular risk factor leading to systemic arterial hypertension, coronary heart disease, arrhythmias, stroke and death (2,3). Recently, the American Heart Association and American College of Cardiology has jointly highlighted the cardiovascular risks of OSA, and acknowledged the lack of understanding that had limited the development of specific treatments (2,3). The current gold standard treatment, continuous positive airway pressure (CPAP) therapy, may not fully reverse OSA chronic cardiovascular consequences, e.g. hypertension (4,5). In addition, CPAP has poor effective long-term compliance in some individuals (6). OSA-cardiovascular morbidity could result mainly from IH-related inflammation (7), including elevated serum pro-thrombotic and pro-inflammatory factors that are major determinants for atherosclerosis development (8,9). OSA and common atherosclerosis share endothelial dysfunction, increases in leukocyte adhesion and platelet aggregation. Cytokines, chemokines and adhesion molecules expression are also elevated compared to controls (10). Circulating levels of inflammatory mediators parallel atherosclerotic plaque formation (9,11) and correlate with oxygen desaturation in OSA (12). Increased carotid intima-media thickness (IMT) is an early sign of atherosclerosis in OSA patients (13) and also correlates with serum inflammatory markers and oxygen desaturation (14,15). Together, these findings suggest an important promoting role for IH in systemic and vascular inflammation.
The specificity of OSA-related atherogenesis remains unknown whereas this knowledge could be useful for providing alternative treatment to CPAP in preventing OSA cardiovascular complications. At early stages, general mechanisms of atherogenesis include leukocyte activation and recruitment into vascular tissue (8). These processes are partly under the control of chemokines and adhesion molecules, resulting in leukocyte rolling, endothelial adhesion, and transendothelial migration (16). Among leukocytes and chemokines, T-cells and the leukoattractant RANTES/CCL5 (regulated on activation, T-cell expressed, and secreted/chemokine ligand 5) appear to be critically and early involved in the atherogenesis (9,16), with serious prospects for future clinical treatments (17–19). RANTES/CCL5 mediates trafficking and homing of T-lymphocytes, monocytes, and other leukocytes, and has been implicated in arterial injury and atherosclerosis (9), circulating levels being predictive of cardiac events and mortality (20,21). Several studies have provided evidence for T-lymphocyte involvement in the atherosclerosis of OSA-patients (22), however the role of RANTES/CCL5 is still unknown. It is of interest to characterize the role of chemokines in the IH-related inflammation, as they represent potential targets for future pharmacological manipulations.
The aim of the present study was to identify the biological events leading to pre-atherosclerotic remodeling through systemic and vascular inflammatory responses to IH in a murine model of sleep apnea. On the basis of our results, we secondarily focused our investigations on the specific role of the chemokine RANTES/CCL5 in the IH-related vascular remodeling. Some of the results of this study have been previously reported in the form of an abstract (23).
METHODS
Details are provided in the online supplement.
Animals
Male C57BL/6J mice (8 weeks old) were randomized to 5 and 14 days of IH (21-5% FiO2, 60s cycle, 8h/d) or air (N, normoxic), as previously described (24). Blood was collected under anesthesia for hematocrit, chemokine and cholesterol determinations. Tissues were harvested and frozen until analysis. All efforts were made to reduce the number of animals used to an unavoidable minimum.
Assessment of systemic inflammation
Proliferation assay
Splenocytes were isolated, cultured at a concentration of 5x106 cells.ml−1, and stimulated in triplicates with graded concentrations of concanavalin-A (Sigma). Cell proliferation was determined 48h later using a cell proliferation kit (CellTiter 96® AQueous non-radioactive cell proliferation assay, Promega).
Splenocyte chemokine mRNA expression
Total mRNA was extracted from spleen, and chemokine expression was assessed by qRT-PCR and normalized with the 18S ribosomal-RNA level.
Ex vivo transmigration assay
Interferon-gamma (IFN-γ) stimulated and unstimulated splenocytes were assessed for transwell migration toward RANTES/CCL5 (R&D Systems).
Assessment of vascular inflammation and remodeling
Leukocyte rolling
Intravital microscopy was performed on exteriorized mesenteric microvasculature since the technique requires thin transparent tissue. Rolling of rhodamine 6G-stained leukocytes was assessed by two blinded observers.
ICAM-1, alpha-smooth muscle actin (αSMA) and NFkB immunoblotting
Expressions of mesenteric and aortic ICAM-1, aortic αSMA and NFkB were assessed by Western blot. Tissues were homogenized and proteins were separated on 8% SDS-PAGE, immunoblotted for ICAM-1 (R&D systems) or αSMA (Abcam), visualized using enhanced chemoluminescence detection system and quantified by densitometric analysis using Image J® software. For NFkB, nuclear proteins were separated on 10% SDS/PAGE and immunoblotted for NFkB-p50 (Abcam).
Aortic IFNγ mRNA expression
Total mRNA was extracted from aortas, and IFNγ expression was assessed by qRT-PCR and normalized using ubiquitin mRNA levels.
Immunohistochemistry
OCT-embedded aorta sections (10-μm) (Tissue tek®-OCTTM, Sakura) were stained with hematoxylin-eosin, Verhoeff, alcian blue, Oil-red-O and sirius red to assess global tissue morphology, elastic fibers, mucoid degeneration, lipid deposition and collagen content, respectively. Additional sections were immunostained for CD3 (DakoCytomation) and RANTES/CCL5 (R&D systems). Morphometric analysis (up to 30 measurements on 3 non-contiguous midthoracic aorta sections per animal, n=7–10 mice per group) was performed with a light microscope (Nikon Eclipse 80i) and LUCIA-G software V5.0.
RANTES/CCL5 neutralization
To confirm the role of RANTES/CCL5 in IH-induced vascular remodeling, additional mice were treated as previously described (25), using a rat anti-mouse RANTES/CCL5 monoclonal antibody (R&D systems, intraperitoneal injection, 250 μg, 3 times per week) or its rat IgG isotype control (ATCC) throughout the 14-day exposure to IH or air. Mice were assessed for vascular remodeling as described above.
Statistical analysis
Results were expressed as means ± SEM and analyzed using either ANOVA and t-test or Mann-Whitney U-test, according to normality and variance homogeneity. Statistical significance was set at p<0.05.
RESULTS
SYSTEMIC INFLAMMATION
We assessed three indices reflecting systemic T-lymphocyte activation. Spleen-isolated T-cells were analyzed for their proliferative response to concanavalin A, and their capacity to express chemokines and migrate upon a chemokine gradient.
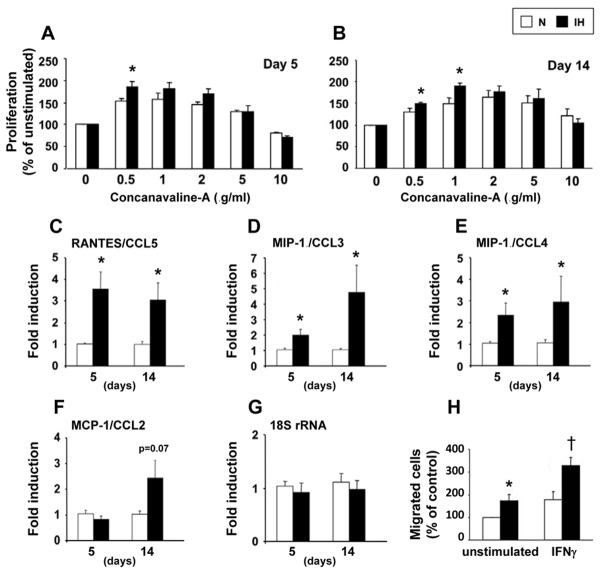
Splenocyte proliferation: No significant difference in the baseline proliferation rate emerged between N and IH. The dose-response relationship resulted in bell-shaped curves, the hypoxic mice showing a significantly higher peak proliferation with 0.5 μg/ml of Con-A at day 5 and 0.5–1 μg/ml at day 14 (Figures 1A and 1B).
Splenocyte expression of leukostimulating and leukoattractant chemokines: IH induced a predominant elevation in RANTES/CCL5 after only 5 days of IH that was still present at 14 days. Expressions of MIP1α/CCL3 and MIP1β/CCL4 increased more progressively, whereas modifications of MCP1/CCL2 did not reach significance (Figures 1C to 1F).
Splenocyte migration: Unstimulated and IFN-γ stimulated splenocytes from IH-mice showed higher migration capacity towards the leukoattractant RANTES/CCL5 (Figure 1H), again confirming that IH induced splenocyte activation.
Figure 1. Intermittent hypoxia induces splenocyte activation.
Splenocyte proliferation in response to concanavalin-A after 5 (A) and 14 (B) days of intermittent hypoxia (IH) or air (N); *p<0.05 vs N (n=6–12 per group). Splenocyte mRNA expression of RANTES/CCL5 (C), MIP-1α/CCL3 (D), MIP-1β/CCL4 (E) and MCP-1/CCL2 (F). Measurements were normalized to the eukaryotic 18S ribosomal-RNA (G) and expressed as fold induction of their baseline values; *p<0.05 vs N (n=6 per group). Splenocyte migration toward RANTES/CCL5 after 14 days of IH or air (H). Splenocytes were tested without stimulation or after 50 ng.ml−1 interferon-gamma (IFN-γ) stimulation; p<0.05 vs unstimulated* or stimulated† splenocytes from N-mice (n=4).
VASCULAR INFLAMMATION
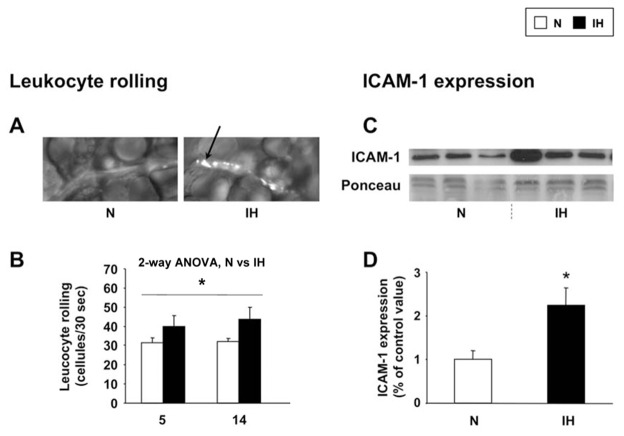
IH increases leukocyte rolling and ICAM-1 expression
To investigate the effect of IH on circulating leukocyte recruitment, we used intravital microscopy on the mesenteric microcirculation. We found an increased number of rolling leukocytes in hypoxic mice (Figures 2A and 2B). Furthermore, whereas leukocyte arrest was not significantly altered, mesenteric ICAM-1 protein was overexpressed after 14 days of IH (Figures 2C and 2D).
Figure 2. Intermittent hypoxia increases leukocyte-endothelium adhesive interactions.
Leukocyte-microvessel interplay was assessed by leukocyte rolling and ICAM-1 expression in mesenteric vessels from mice exposed to intermittent hypoxia (IH) or air (N) for 14 days. (A) Representative photographs showing leukocyte rolling (arrow). (B) Rolling quantification (n=4–5 each). Representative immunoblotting (C) and quantitative analysis (D) of ICAM-1 expression (n=4 each).
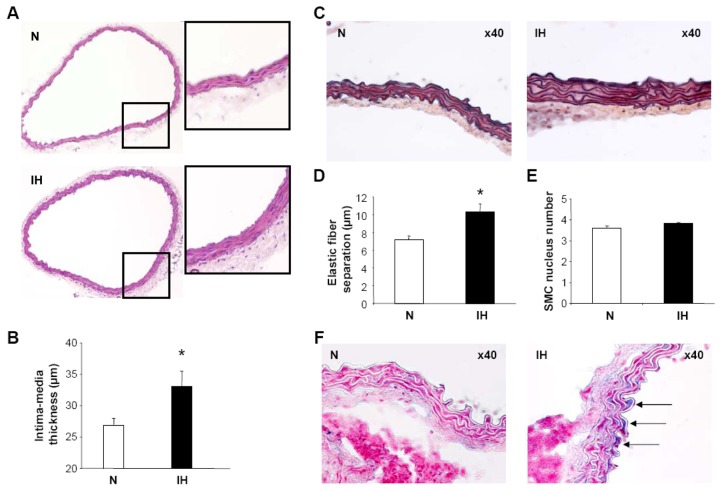
IH induces structural and inflammatory aorta remodeling
Structural remodeling: While the internal perimeter was unaffected (N vs IH, 1942±54 vs 1993±71 μm), IMT was increased after 14 days of IH (Figures 3A and 3B), suggesting an expansive remodeling. The enlarged wall involved the tunica media, in which elastic lamellae were thicker (N vs IH, 1.7±0.1 vs 2.6±0.2 μm, p<0.01) with a less harmonious organization and some discontinuities of the elastic network (Figure 3C). Distance between the elastic lamellae was increased (Figure 3D) due to smooth-muscle cell (SMC) hypertrophy, without an alteration in the number of SMC nuclei in the media (Figure 3E). Alcian blue staining showed some mucoid accumulations between sub-intimal elastic fibers (Figure 3F), that could result from elastoid degeneration and/or mucoid degenerating SMC. In contrast, no lipid deposition or collagen alteration was observed (data not shown).
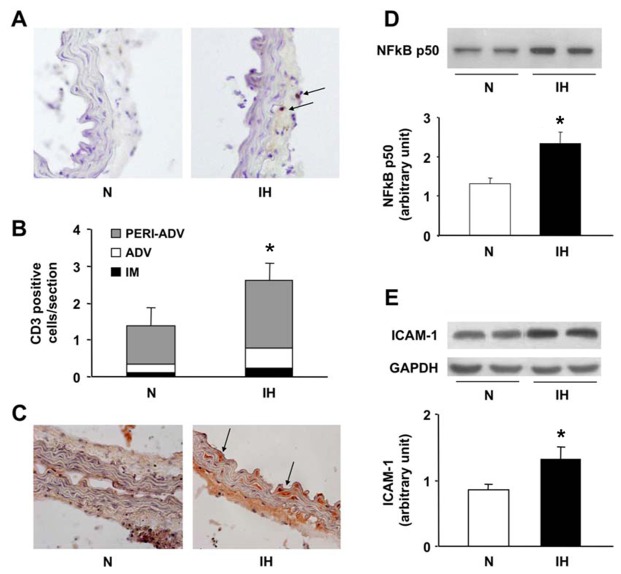
Aorta inflammation: 14 days of IH induced a slight but significant increase in T-cell (CD3 positive cells) infiltration in the aortic wall, almost exclusively located in the adventitia-periadventitia (Figures 4A and 4B). RANTES/CCL5 expression was increased in IH aortas, as shown by immunostaining, either underlining the elastic fibers of the media, or covering the cytoplasm of SMCs. For the latter, there was a characteristic spindle-shaped staining, especially for the hypertrophic SMCs between the two most internal layers of elastic fibers (Figure 4C). IH-aortas also exhibited increased expression of nuclear NFkB-p50 and cytoplasmic ICAM-1 (Figures 4D and 4E).
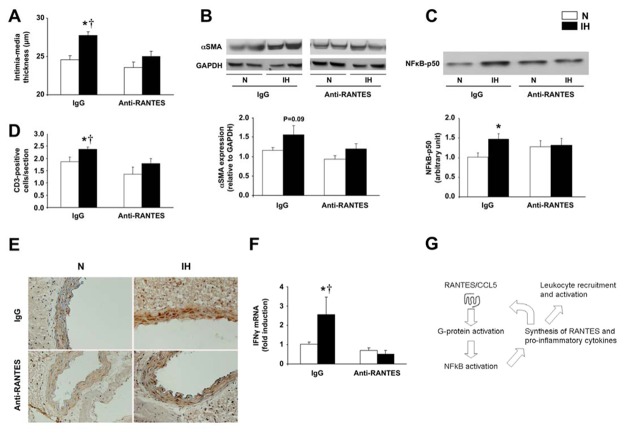
RANTES/CCL5 neutralization prevents IH-induced aorta remodeling The antibody selectively binds to the chemokine RANTES/CCL5 and inhibits the interaction of RANTES/CCL5 with its receptors, thereby neutralizing RANTES/CCL5 activity. RANTES/CCL5 inhibition prevented both structural and inflammatory alterations of the aortic wall due to IH. Indeed, anti-RANTES treatment attenuated the increases in IMT, αSMA, T-cell infiltration and RANTES/CCL5 expression (Figures 5A, 5B, 5D and 5E). This was associated with a global anti-inflammatory effect, as RANTES/CCL5 neutralization also prevented the IH-induced NFkB-p50 and Th1 cytokine IFNγ overexpression (Figures 5C, 5F and 5G). In contrast, RANTES/CCL5 neutralization did not prevent hematocrit (normoxic IgG and anti-RANTES/CCL5 treated mice: 43.5±0.5 vs 42.3±0.6%; hypoxic IgG and anti-RANTES/CCL5 treated mice: 46.6±0.4 vs 46.8±0.6%), cholesterol and weight alterations associated with IH (online Figures E1B to E1D).
Figure 3. Intermittent hypoxia induces structural aorta remodeling.
Vascular remodeling was assessed in mice exposed to intermittent hypoxia (IH) or air (N) for 14 days. (A) Hematoxylin-eosin stainings (10x10 magnification and digitally magnified insets). (B) Histomorphometric analysis of intima-media thickness, n=7 each. (C) Verhoeff coloration showing thicker elastic fibers in IH-mice (10x40 magnification). Elastic fiber separation (D) and smooth-muscle cell (SMC) nuclei (E) in the media (n=7 each). (F) Alcian blue coloration showing mucoid depositions between the elastic fibers in IH-mice (arrows, 10x40 magnification).
Figure 4. Intermittent hypoxia induces aorta inflammation.
Inflammation was assessed in mice exposed to intermittent hypoxia (IH) or air (N) for 14 days. (A) CD3 immunostaining with arrows showing T-cells (10x20 magnification). (B) Quantitative analysis of CD3-positive cell infiltration according to the various tunica of the aortic wall. Note that T-cells predominated in the adventitia-periadventitia tunica (n=9–10 per group). (C) Representative RANTES/CCL5 immunostaining (10x20 magnification). Immunoblottings and quantifications of nuclear NFkB-p50 (D) and cytosolic ICAM-1 (E) (n=4 each).
Figure 5. RANTES/CCL5 neutralization attenuates IH-induced aorta remodeling.
Mice were exposed to intermittent hypoxia (IH) or air (N) for 14 days, and treated either with the anti-RANTES/CCL5 monoclonal antibody or with the control IgG throughout the exposure. (A) Intima-media thickness (n=7–8 each). (B) Cytosolic α-smooth muscle actin (α-SMA) expression with representative immunoblotting and quantitative analysis (n=5–7 each). (C) Nuclear NFkB-p50 expression with representative immunoblotting and quantitative analysis (n=4–7 each). (D) Quantification of T-cell infiltration in the aortic wall (n=7–8 each). (E) Representative RANTES/CCL5 immunostaining (10x20 magnification). (F) IFNγ mRNA expression normalized to ubiquitin (n=4–9 each). *p<0.05 vs N-IgG; †p<0.05 vs anti-RANTES treated IH-mice. (G) Regulation pathway of NFkB activation and subsequent leukocyte recruitment and activation (adapted from Ye et al, (44)).
DISCUSSION
The specific pathophysiology of OSA-induced atherogenesis remains poorly understood. In the current study, we demonstrated in mice that IH, the key hallmark of OSA, induced systemic and vascular inflammation, with pre-atherosclerotic remodeling. Both inflammatory and structural vascular alterations were attenuated with RANTES/CCL5 neutralization. This provides a strong rationale to consider new treatment strategies combined to CPAP when addressing OSA cardiovascular consequences.
Methodological considerations
Mouse strain
As previously published (26), we used C57BL6 mice exposed to 14 days of IH to study pre-atherosclerotic remodeling due to IH, i.e. early stages of vascular changes before any fibrolipid lesions. C57BL6 mice can develop atherosclerosis but after a long IH exposure (12 weeks) with a concomittant atherogenic diet resulting in dyslipidemia (27). Atherosensitive mice such as apolipoprotein-E deficient mice could be potentially interesting, but they spontaneously develop very advanced atherosclerotic lesions with systemic inflammation and severe dyslipidemia, even without IH. Therefore the use of C57BL6 mice without confounders (e.g. atherogenic diet, spontaneous inflammation and dyslipidemia), as performed in this study, allowed assessing the effects of IH per se on the vasculature at early stages.
IH stimulus
The hypoxic stimulus used in this study has been extensively used by our group and others (24). With a nadir arterial oxygen saturation around 60% (26), our experimental model mimics severe sleep apnea, representing less than 10% of patients. In the absence of confounding factors (i.e. obesity…) or genetic susceptibility for complications, IH needs to be severe enough to induce detrimental effects (24), but also leads to weight loss as observed in our study. However despite this limitation, the IH model proved to be useful during the last two decades for investigating the various consequences elicited by sleep apnea (24).
IH induces systemic inflammation
During the inflammatory response, lymphocytes are activated into lymphoid organs such as the spleen where they proliferate. Then, lymphocytes are recruited into non-lymphoid inflamed tissues under the control of chemokines and adhesion molecules, and release inducible chemokines (9). In the present study, we observed splenocyte activation in response to IH, including enhanced proliferative and migratory capacities, as well as increased chemokine expression. Our data are consistent with the literature reporting specific activation of lymphocytes in OSA patients (22). Thus from our experimental data, we can hypothesize that the hypoxic component of OSA plays a major role in lymphocyte activation. Splenic-derived T lymphocytes may be directly activated by hypoxia through HIF-1α and NFkB activation, with complex interactions between these two hypoxia-sensitive transcription factors (28,29). Additionally, lymphocytes may be indirectly activated through the numerous IH-induced changes including oxidative stress (30), sympathetic activation (31) and hormonal alterations including leptin (32). We further specifically assessed four chemokines that are known to be determinant in atherosclerosis (9), and we found an early and predominant RANTES/CCL5 overexpression. This splenic overexpression of chemokines confirmed the IH-induced splenocyte activation. We also found that activated splenocytes had enhanced migration toward RANTES/CCL5 gradient, supporting an important role for this specific chemokine in the IH response.
IH increases leukocyte-endothelium interactions
Leukocyte recruitment is an early stage linking systemic and tissue inflammation, with leukocyte rolling being one of the first step. In the present study, we showed increased adhesive interactions between leukocytes and microvessels in the IH animals. Similar microcirculation alterations, with increased leukocyte rolling and adhesion, have been recently shown after only three hours of experimentally induced obstructive apneas (33). These early alterations may rely on biomechanical activation (34), such as the oscillatory shear stress due to blood pressure fluctuations (26). This mechanism could be particularly relevant to the obstructive apnea condition that also includes respiratory efforts and related hemodynamic changes (33). Whereas leukocyte arrest was not significant in our IH model, we evidenced a mesenteric upregulation of the ICAM1 protein, which is crucial in the adhesion and transmigration steps of leukocyte recruitment (35) and could precede adhesion of leukocytes. This result is in agreement with clinical studies in OSA patients showing elevated circulating adhesion molecules (12).
IH induces structural remodeling of large arteries
IH-mice exhibited an enlarged IMT without vascular dilatation, suggesting an expansive remodeling (34,36). While collagen alterations and lipid depositions were absent, elastic fibers were thicker, disorganized and separated by a larger distance due to SMC hypertrophy. These alterations suggest mechanical adaptations of the arterial wall. Indeed, we previously reported at a similar time point that IH induced blood pressure elevation and enhanced vasoconstriction to norepinephrine due to sympathetic hyperactivity (26). In response to elevated blood pressure, early functional and structural vascular plasticity occurs, including SMC hypertrophy and hyperplasia, elastic fiber thickening and abnormal extracellular matrix turnover (37). In addition to hemodynamic strains, hypoxia itself and the numerous alterations generated by IH can contribute to SMC hypertrophy, through sympatho-adrenergic hyperactivity, endocrine and paracrine factors, as well as oxidative, inflammatory and growth factors (36). We also observed some mucoid depositions in the media which may originate from elastoid degeneration and/or mucoid degenerating SMC.
IH-induced inflammation of large arteries involves RANTES/CCL5
To investigate whether the IH-induced vascular remodeling exhibited an inflammatory component, we studied the nuclear NFkB protein expression and some of its downstream targets. We found a higher NFkB-p50 expression in hypoxic mice, which is in accordance with recent studies showing NFkB activation in cardiovascular tissue from IH-mice (38) and in cells cultured under IH (7). This consistent IH-induced NFkB activation could underlie the inflammatory alterations in apneic patients, including increased adhesion molecules and chemokines (12,39) that play an important role in vascular remodelling (40). Among downstream NFkB targets, we uncovered RANTES/CCL5 overexpression in the media. This RANTES/CCL5 expression seemed to stem essentially from SMC, as suggested by the spindle-shaped staining, and not from T-cells as the latter were located in the adventitia-periadventitia. Another possible source of RANTES/CCL5 could be activated platelets, depositing RANTES/CCL5 on endothelial cells (40).
Chemokines and their receptors have a great impact on initiating and progressing vascular alterations, controlling each step of the remodeling process (40). Therefore, by expressing this leukoattractant chemokine, SMC could have participated in recruiting leukocytes into aortas during IH (41), as suggested by the enhanced ex-vivo splenocyte migration toward RANTES/CCL5. However, other chemokines, cytokines and adhesion molecules, downstream NFkB and produced by vascular cells, may also contribute to inflammatory remodeling (9). Indeed, ICAM-1 overexpression in IH-aortas may have also contributed to T-lymphocyte infiltration, as ICAM-1 is critical in leukocyte recruitment into inflamed tissues (35). The slight aortic T-cell infiltration did not enlarge IMT, as lymphocytes were few and peripherally located. This rather indicates tissue inflammation, and the lymphocyte localization is in line with the recent concept of the “outside-to-inside” signaling (42). Indeed, atherosclerosis has been usually looked at as a vascular process starting at the intima level and progressing to media and adventitia (i.e. inside-out process). In contrast in our study, periadventitial T-cells suggest a role of the periadventitial fat in IH-related vascular inflammation (i.e. outside-in process). The perivascular fat is a specific subset of the white adipose tissue that secretes proatherogenic cytokines and chemokines, such as RANTES/CCL5; this may contribute to the early steps of atherogenesis by attracting inflammatory cells via the periadventitial vasa vasorum rather than from the systemic circulation at the intima level (42).”
The important role of RANTES/CCL5 has already been described in early vascular remodeling (43), as well as in advanced atherosclerotic process (19). Since we found predominant alterations of RANTES/CCL5 in splenocytes from IH mice, we hypothesized that RANTES/CCL5 inhibition could exert a beneficial effect on IH-induced vasculature remodeling. RANTES/CCL5 neutralization attenuated both intima-media thickening and vascular inflammation, without affecting the IH-induced proatherogenic dyslipidemia and HIF-related hematocrit elevation. These results demonstrate the significant contribution of inflammation to the vascular damages due to IH, and support RANTES/CCL5 involvement. Although RANTES/CCL5 expression can result from NFkB activation, RANTES/CCL5 neutralization also reduced IH-induced NFkB activation, likely due to reciprocal interactions (44) (figure 5G). It may result from a global anti-inflammatory effect, as similarly observed when using RANTES/CCL5 antagonist (45), despite HIF activation attested by hematocrit elevation. Indeed, besides preventing T-cell recruitment, RANTES/CCL5 neutralization prevented activation of T-cells and possibly of SMC as suggested by the abolition of IH-induced Th1 cytokine IFNγ expression.
Conclusion
Atherosclerosis is considered as an immuno-inflammatory disease (8), suggesting that targeting inflammation could provide clinical benefit. In view of our results and of the literature, OSA should be considered as an immuno-inflammatory disorder as well. In the present study, we found moderate inflammatory changes, suggesting low-grade inflammation following IH exposure. Besides hemodynamic (26) and metabolic (46) alterations, we showed that the inflammatory response due to severe IH is an early and determinant factor that could contribute to OSA-associated pre-atherosclerotic remodeling.
Emerging therapies aiming at decreasing leukocyte activity and recruitment have led to promising results in atherosclerosis research, either using anti-CD3 antibody (18) or blocking chemokine pathways (19). Orally-administered small molecules to neutralize chemokines are under development and will have clear benefits over antibody treatment in terms of cost and ease of use, but their safety especially for chronic use, will need to be determined.
In this study, we evidenced RANTES/CCL5 involvement in the vascular remodeling initiated by severe IH, with an early involvement in both systemic and vascular inflammatory responses, implicating various cell-types (leukocytes, SMC). This preclinical study suggests that the inflammatory response should be considered in apneic patients, as a potential target for treatment of this disease.
At a Glance Commentary.
Scientific Knowledge on the Subject
Intermittent hypoxia in sleep apnea is a major risk factor for cardiovascular morbidity and mortality. Understanding the development of these outcomes may condition the management of apneic patients at risk for cardiovascular complications.
What This Study Adds to the Field
Intermittent hypoxia induced early systemic inflammation and inflammatory pre-atherosclerotic remodeling in mice, clearly involving the chemokine RANTES/CCL5. These results strengthen the need for early identification of apneic individuals at risk for cardiovascular complications, and suggest new therapeutic options for these patients.
Supplementary Material
Acknowledgments
Support: This study was supported by grants from AGIR@dom to M.D. and C.A., Fondation pour la Recherche Médicale (France) to C.A. and the Swiss National Science Foundation to F.M. (#3200BO-105896).
The authors thank S. Cachot, N. Miguet and S. Jacquard for technical help.
Footnotes
This article has an online data supplement, which is accessible from this issue’s table of content online at www.atsjournals.org
Author contributions
Substantial contributions to conception and design: CA, MD
Acquisition of data: CA, PB, CG, GP, FB, VB, MD
Analysis and interpretation of data: CA, PB, SL, VB, CR, MD
Drafting the article: CA, MD
Revising critically the article for important intellectual content: CA, PB, SL, JLP, CR, FM, PL, MD
Final approval of the version to be published: CA, PB, SL, JLP, CG, GP, FB, VB, CR, JPB, FM, PL, MD
References
- 1.Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165:1217–1239. doi: 10.1164/rccm.2109080. [DOI] [PubMed] [Google Scholar]
- 2.Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, Daniels S, Floras JS, Hunt CE, Olson LJ, Pickering TG, Russell R, Woo M, Young T American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology; American Heart Association Stroke Council; American Heart Association Council on Cardiovascular Nursing; American College of Cardiology Foundation. Sleep apnea and cardiovascular disease: an American Heart Association/American College Of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council On Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health) Circulation. 2008;118:1080–1111. doi: 10.1161/CIRCULATIONAHA.107.189375. [DOI] [PubMed] [Google Scholar]
- 3.Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, Daniels S, Floras JS, Hunt CE, Olson LJ, Pickering TG, Russell R, Woo M, Young T. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. J Am Coll Cardiol. 2008;52:686–717. doi: 10.1016/j.jacc.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 4.Barbé F, Durán-Cantolla J, Capote F, de la Peña M, Chiner E, Masa JF, Gonzalez M, Marín JM, Garcia-Rio F, de Atauri JD, Terán J, Mayos M, Monasterio C, del Campo F, Gomez S, de la Torre MS, Martinez M, Montserrat JM Spanish Sleep and Breathing Group. Long-term effect of continuous positive airway pressure in hypertensive patients with sleep apnea. Am J Respir Crit Care Med. 2010;181:718–726. doi: 10.1164/rccm.200901-0050OC. [DOI] [PubMed] [Google Scholar]
- 5.Pépin JL, Tamisier R, Barone-Rochette G, Launois SH, Lévy P, Baguet JP. Comparison of continuous positive airway pressure and valsartan in hypertensive patients with sleep apnea. Am J Respir Crit Care Med. 2010;182:954–960. doi: 10.1164/rccm.200912-1803OC. [DOI] [PubMed] [Google Scholar]
- 6.Gay P, Weaver T, Loube D, Iber C Positive Airway Pressure Task Force; Standards of Practice Committee; American Academy of Sleep Medicine. Evaluation of positive airway pressure treatment for sleep related breathing disorders in adults. Sleep. 2006;29:381–401. doi: 10.1093/sleep/29.3.381. [DOI] [PubMed] [Google Scholar]
- 7.Ryan S, Taylor CT, McNicholas WT. Selective activation of inflammatory pathways by intermittent hypoxia in obstructive sleep apnea syndrome. Circulation. 2005;112:2660–2667. doi: 10.1161/CIRCULATIONAHA.105.556746. [DOI] [PubMed] [Google Scholar]
- 8.Hansson GK, Libby P. The immune response in atherosclerosis: a double-edged sword. Nat Rev Immunol. 2006;6:508–519. doi: 10.1038/nri1882. [DOI] [PubMed] [Google Scholar]
- 9.Tedgui A, Mallat Z. Cytokines in atherosclerosis: pathogenic and regulatory pathways. Physiol Rev. 2006;86:515–581. doi: 10.1152/physrev.00024.2005. [DOI] [PubMed] [Google Scholar]
- 10.Arnaud C, Dematteis M, Pépin JL, Baguet JP, Lévy P. Obstructive sleep apnea syndrome, immuno-inflammation and atherosclerosis. Semin Immunopathol. 2009;31:113–125. doi: 10.1007/s00281-009-0148-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Charo IF, Taubman MB. Chemokines in the pathogenesis of vascular disease. Circ Res. 2004;95:858–866. doi: 10.1161/01.RES.0000146672.10582.17. [DOI] [PubMed] [Google Scholar]
- 12.Ohga E, Tomita T, Wada H, Yamamoto H, Nagase T, Ouchi Y. Effects of obstructive sleep apnea on circulating ICAM-1, IL-8, and MCP-1. J Appl Physiol. 2003;94:179–184. doi: 10.1152/japplphysiol.00177.2002. [DOI] [PubMed] [Google Scholar]
- 13.Drager LF, Bortolotto LA, Lorenzi MC, Figueiredo AC, Krieger EM, Lorenzi-Filho G. Early signs of atherosclerosis in obstructive sleep apnea. Am J Respir Crit Care Med. 2005;172:613–618. doi: 10.1164/rccm.200503-340OC. [DOI] [PubMed] [Google Scholar]
- 14.Baguet JP, Hammer L, Lévy P, Pierre H, Launois S, Mallion JM, Pépin JL. The severity of oxygen desaturation is predictive of carotid wall thickening and plaque occurrence. Chest. 2005;128:3407–3412. doi: 10.1378/chest.128.5.3407. [DOI] [PubMed] [Google Scholar]
- 15.Minoguchi K, Yokoe T, Tazaki T, Minoguchi H, Tanaka A, Oda N, Okada S, Ohta S, Naito H, Adachi M. Increased carotid intima-media thickness and serum inflammatory markers in obstructive sleep apnea. Am J Respir Crit Care Med. 2005;172:625–630. doi: 10.1164/rccm.200412-1652OC. [DOI] [PubMed] [Google Scholar]
- 16.Braunersreuther V, Mach F. Leukocyte recruitment in atherosclerosis: potential targets for therapeutic approaches? Cell Mol Life Sci. 2006;63:2079–2088. doi: 10.1007/s00018-006-6127-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Veillard NR, Kwak B, Pelli G, Mulhaupt F, James RW, Proudfoot AE, Mach F. Antagonism of RANTES receptors reduces atherosclerotic plaque formation in mice. Circ Res. 2004;94:253–261. doi: 10.1161/01.RES.0000109793.17591.4E. [DOI] [PubMed] [Google Scholar]
- 18.Steffens S, Burger F, Pelli G, Dean Y, Elson G, Kosco-Vilbois M, Chatenoud L, Mach F. Short-term treatment with anti-CD3 antibody reduces the development and progression of atherosclerosis in mice. Circulation. 2006;114:1977–1984. doi: 10.1161/CIRCULATIONAHA.106.627430. [DOI] [PubMed] [Google Scholar]
- 19.Braunersreuther V, Steffens S, Arnaud C, Pelli G, Burger F, Proudfoot A, Mach F. A novel RANTES antagonist prevents progression of established atherosclerotic lesions in mice. Arterioscler Thromb Vasc Biol. 2008;28:1090–1096. doi: 10.1161/ATVBAHA.108.165423. [DOI] [PubMed] [Google Scholar]
- 20.Kraaijeveld AO, de Jager SC, de Jager WJ, Prakken BJ, McColl SR, Haspels I, Putter H, van Berkel TJ, Nagelkerken L, Jukema JW, Biessen EA. CC chemokine ligand-5 (CCL5/RANTES) and CC chemokine ligand-18 (CCL18/PARC) are specific markers of refractory unstable angina pectoris and are transiently raised during severe ischemic symptoms. Circulation. 2007;116:1931–1941. doi: 10.1161/CIRCULATIONAHA.107.706986. [DOI] [PubMed] [Google Scholar]
- 21.Cavusoglu E, Eng C, Chopra V, Clark LT, Pinsky DJ, Marmur JD. Low plasma RANTES levels are an independent predictor of cardiac mortality in patients referred for coronary angiography. Arterioscler Thromb Vasc Biol. 2007;27:929–935. doi: 10.1161/01.ATV.0000258789.21585.76. [DOI] [PubMed] [Google Scholar]
- 22.Dyugovskaya L, Lavie P, Lavie L. Lymphocyte activation as a possible measure of atherosclerotic risk in patients with sleep apnea. Ann N Y Acad Sci. 2005;1051:340–350. doi: 10.1196/annals.1361.076. [DOI] [PubMed] [Google Scholar]
- 23.Arnaud C, Béguin PC, Dematteis M, Pelli G, Miguet N, Burger F, Ribuot C, Mach F, Lévy P. Intermittent hypoxia induces inflammatory vascular remodeling in C57bl6 mice. Am J Resp Crit Care Med. 2008;177:A291. [Google Scholar]
- 24.Dematteis M, Godin-Ribuot D, Arnaud C, Ribuot C, Stanke-Labesque F, Pépin JL, Lévy P. Cardiovascular consequences of sleep-disordered breathing: contribution of animal models to understanding of the human disease. ILAR J. 2009;50:262–281. doi: 10.1093/ilar.50.3.262. [DOI] [PubMed] [Google Scholar]
- 25.Glass WG, Hickey MJ, Hardison JL, Liu MT, Manning JE, Lane TE. Antibody targeting of the CC chemokine ligand 5 results in diminished leukocyte infiltration into the central nervous system and reduced neurologic disease in a viral model of multiple sclerosis. J Immunol. 2004;172:4018–4025. doi: 10.4049/jimmunol.172.7.4018. [DOI] [PubMed] [Google Scholar]
- 26.Dematteis M, Julien C, Guillermet C, Sturm N, Lantuejoul S, Mallaret M, Lévy P, Gozal E. Intermittent hypoxia induces early functional cardiovascular remodeling in mice. Am J Respir Crit Care Med. 2008;177:227–235. doi: 10.1164/rccm.200702-238OC. [DOI] [PubMed] [Google Scholar]
- 27.Savransky V, Nanayakkara A, Li J, Bevans S, Smith PL, Rodriguez A, Polotsky VY. Chronic intermittent hypoxia induces atherosclerosis. Am J Respir Crit Care Med. 2007;175:1290–1297. doi: 10.1164/rccm.200612-1771OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Neumann AK, Yang J, Biju MP, Joseph SK, Johnson RS, Haase VH, Freedman BD, Turka LA. Hypoxia inducible factor 1 alpha regulates T cell receptor signal transduction. Proc Natl Acad Sci U S A. 2005;102:17071–17076. doi: 10.1073/pnas.0506070102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taylor CT. Interdependent roles for hypoxia inducible factor and nuclear factor-kappaB in hypoxic inflammation. J Physiol. 2008;586:4055–4059. doi: 10.1113/jphysiol.2008.157669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Williams MS, Kwon J. T cell receptor stimulation, reactive oxygen species, and cell signaling. Free Radic Biol Med. 2004;37:1144–1151. doi: 10.1016/j.freeradbiomed.2004.05.029. [DOI] [PubMed] [Google Scholar]
- 31.Elenkov IJ, Wilder RL, Chrousos GP, Vizi ES. The sympathetic nerve--an integrative interface between two supersystems: the brain and the immune system. Pharmacol Rev. 2000;52:595–638. [PubMed] [Google Scholar]
- 32.Martín-Romero C, Santos-Alvarez J, Goberna R, Sánchez-Margalet V. Human leptin enhances activation and proliferation of human circulating T lymphocytes. Cell Immunol. 2000;199:15–24. doi: 10.1006/cimm.1999.1594. [DOI] [PubMed] [Google Scholar]
- 33.Nácher M, Serrano-Mollar A, Farré R, Panés J, Seguí J, Montserrat JM. Recurrent obstructive apneas trigger early systemic inflammation in a rat model of sleep apnea. Respir Physiol Neurobiol. 2007;155:93–96. doi: 10.1016/j.resp.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 34.Chatzizisis YS, Coskun AU, Jonas M, Edelman ER, Feldman CL, Stone PH. Role of endothelial shear stress in the natural history of coronary atherosclerosis and vascular remodeling: molecular, cellular, and vascular behavior. J Am Coll Cardiol. 2007;49:2379–2393. doi: 10.1016/j.jacc.2007.02.059. [DOI] [PubMed] [Google Scholar]
- 35.Vestweber D. Adhesion and signaling molecules controlling the transmigration of leukocytes through endothelium. Immunol Rev. 2007;218:178–196. doi: 10.1111/j.1600-065X.2007.00533.x. [DOI] [PubMed] [Google Scholar]
- 36.Berk BC. Vascular smooth muscle growth: autocrine growth mechanisms. Physiol Rev. 2001;81:999–1030. doi: 10.1152/physrev.2001.81.3.999. [DOI] [PubMed] [Google Scholar]
- 37.Hu JJ, Ambrus A, Fossum TW, Miller MW, Humphrey JD, Wilson E. Time courses of growth and remodeling of porcine aortic media during hypertension: a quantitative immunohistochemical examination. J Histochem Cytochem. 2008;56:359–370. doi: 10.1369/jhc.7A7324.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Greenberg H, Ye X, Wilson D, Htoo AK, Hendersen T, Liu SF. Chronic intermittent hypoxia activates nuclear factor-kappaB in cardiovascular tissues in vivo. Biochem Biophys Res Commun. 2006;343:591–596. doi: 10.1016/j.bbrc.2006.03.015. [DOI] [PubMed] [Google Scholar]
- 39.Dyugovskaya L, Lavie P, Lavie L. Increased adhesion molecules expression and production of reactive oxygen species in leukocytes of sleep apnea patients. Am J Respir Crit Care Med. 2002;165:934–939. doi: 10.1164/ajrccm.165.7.2104126. [DOI] [PubMed] [Google Scholar]
- 40.Schober A. Chemokines in vascular dysfunction and remodeling. Arterioscler Thromb Vasc Biol. 2008;28:1950–1959. doi: 10.1161/ATVBAHA.107.161224. [DOI] [PubMed] [Google Scholar]
- 41.Krohn R, Raffetseder U, Bot I, Zernecke A, Shagdarsuren E, Liehn EA, van Santbrink PJ, Nelson PJ, Biessen EA, Mertens PR, Weber C. Y-box binding protein-1 controls CC chemokine ligand-5 (CCL5) expression in smooth muscle cells and contributes to neointima formation in atherosclerosis-prone mice. Circulation. 2007;116:1812–1820. doi: 10.1161/CIRCULATIONAHA.107.708016. [DOI] [PubMed] [Google Scholar]
- 42.Vela D, Buja LM, Madjid M, Burke A, Naghavi M, Willerson JT, Casscells SW, Litovsky S. The role of periadventitial fat in atherosclerosis. Arch Pathol Lab Med. 2007;131:481–487. doi: 10.5858/2007-131-481-TROPFI. [DOI] [PubMed] [Google Scholar]
- 43.Zernecke A, Liehn EA, Gao JL, Kuziel WA, Murphy PM, Weber C. Deficiency in CCR5 but not CCR1 protects against neointima formation in atherosclerosis-prone mice: involvement of IL-10. Blood. 2006;107:4240–4243. doi: 10.1182/blood-2005-09-3922. [DOI] [PubMed] [Google Scholar]
- 44.Ye RD. Regulation of nuclear factor kappaB activation by G-protein-coupled receptors. J Leukoc Biol. 2001;70:839–848. [PubMed] [Google Scholar]
- 45.Braunersreuther V, Pellieux C, Pelli G, Burger F, Steffens S, Montessuit C, Weber C, Proudfoot A, Mach F, Arnaud C. Chemokine CCL5/RANTES inhibition reduces myocardial reperfusion injury in atherosclerotic mice. J Mol Cell Cardiol. 2010;48:789–798. doi: 10.1016/j.yjmcc.2009.07.029. [DOI] [PubMed] [Google Scholar]
- 46.Li J, Thorne LN, Punjabi NM, Sun CK, Schwartz AR, Smith PL, Marino RL, Rodriguez A, Hubbard WC, O’Donnell CP, Polotsky VY. Intermittent hypoxia induces hyperlipidemia in lean mice. Circ Res. 2005;97:698–706. doi: 10.1161/01.RES.0000183879.60089.a9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.