Abstract
Tuberculosis contact investigations are a top priority in TB infection control. The aim is to prevent the spread of infectious disease, identify potential TB sources, and treat individuals who are infected or actively ill. The contact investigation process is quite simple: identify close contacts; examine their symptoms and determine their clinical status; perform a chest X-ray; administer a tuberculin skin test and/or interferon gamma release assay; and evaluate the results. This communication documents a TB contact investigation that was conducted in one family during the months after the initial TB finding. Investigations of close family contacts found active TB in 3 individuals and latent TB in 1 unvaccinated child. This confirms that contact investigations are an easy intervention that results in rapid identification of TB sources. Treatment of these patients reduces the risk of exposure and spread of infection to additional community members [1].
Keywords: Tuberculosis, Contact investigation, Latent tuberculosis infection, Preventive chemotherapy
1. Introduction
At present, tuberculosis (TB) is the most widespread infectious disease in the world. The Czech Republic has one of the lowest annual TB incidence rates in Central Europe. In 2014, a total of 512 cases of TB disease were reported, which represents 5.0 cases per 100,000 inhabitants. 75% of new pulmonary TB disease cases were found while examining patients for health complaints (passive search method). TB contact investigations were conducted in 8% of these cases (active search method). The Mycobacterium tuberculosis complex is the causative agent of TB, the source of which is primarily ill individuals, but also carriers. TB symptoms are not usually overly pronounced; patients suffer fatigue, perspiration, elevated temperatures, coughing, and weight loss.
In 1953, the former Czechoslovakia launched a blanket vaccination campaign against TB. In the 1950s, all infants and older children were vaccinated to facilitate rapid vaccination coverage of the population. From the early 1960s until 2009, vaccinations were administered to infants; older children (at 11 years of age) with negative tuberculin skin test (TST) results, also received vaccinations. In 2010, the Czech Republic discontinued the blanket vaccination campaign for infants; selective TB vaccination is currently designated for children at risk of contracting TB [2]. This communication presents the TB contact investigation of one family.
1.1. Case report no. 1
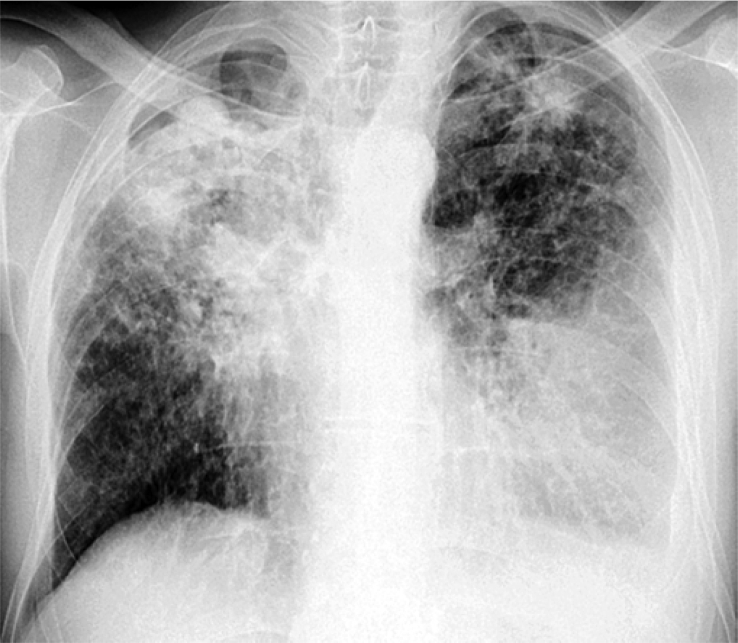
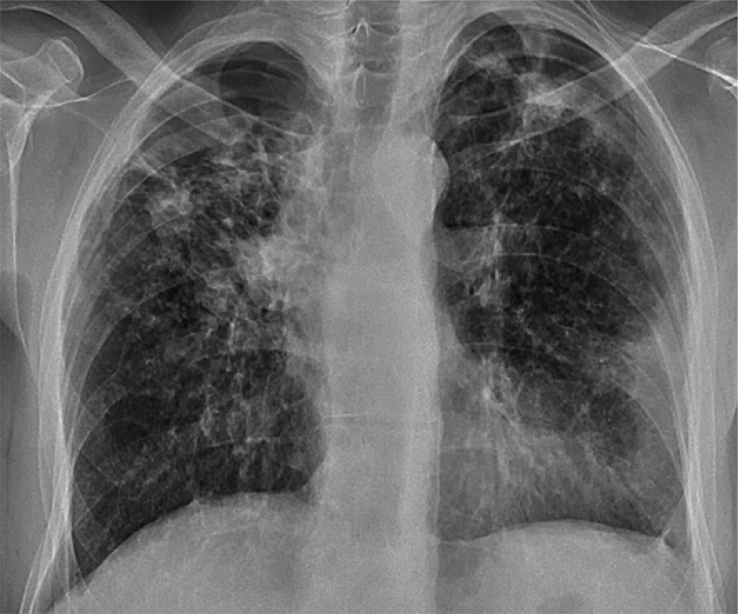
The patient was a 48-year-old male, smoker (30 pack-years), but not yet seriously ill. The patient was vaccinated against TB as a child. He is married and resides in an apartment with his family. The patient arrived at the hospital complaining of sudden hemoptysis. He reported that he had been coughing more than usual during the last month and had been short of breath upon exertion. He was afebrile and had lost 20 kg over the course of 9 months. A posteroanterior chest X-ray showed diffuse bilateral infiltrates (Fig. 1). A sputum examination repeatedly demonstrated massive smear positivity and a finding of acid-fast bacilli, which was followed by culture positivity 3 weeks later. A Bactec MGIT 960 examination produced a positive result on the 8th day and PCR tests results were also positive. The Mantoux TST showed an induration of +15 mm. Typing demonstrated Mycobacterium tuberculosis complex (MTB) with preserved sensitivity to first-line antituberculous medications. HIV test results were negative. First-line antituberculosis treatment (AT) was started immediately with a combination of rifampicin, isoniazid, ethambutol and pyrazinamide. After 2 months, sputum samples were both culture-negative and smear-negative for MTB. Given the extent of the disease, the initial phase of AT treatment was extended to 3 months, with a follow-on phase of bi-therapy with rifampicin and isoniazid for 6 months. Treatment was effective with no adverse effects. Radiograph findings gradually regressed and the patient’s clinical condition improved significantly (Fig. 2).
Fig. 1.
Posteroanterior chest X-ray showed.
Fig. 2.
Regression of bilateral diffuse infitrates diffuse bilateral infiltrates after 3 months AT treatment.
The patient’s wife was examined during the course of a TB contact investigation.
1.2. Case report no. 2
The patient was a 47-year-old female, smoker (31 pack-years), employed as a maid, presenting as not seriously ill. The patient resides in the same household as her husband and was vaccinated against TB as a child. She visited the hospital for the purpose of undergoing a TB contact investigation. No reported pulmonary complaints, apart from a long-standing cough in the mornings. She was afebrile, no reported weight loss, no perspiration. The TST was positive with an induration of +16 mm; HIV test results were negative. A chest X-ray showed infiltrates in the upper right and middle fields on both right and left sides. Sputum tests were repeatedly smear-negative, but culture and Bactec MGIT 960 tests were positive. Genome testing demonstrated a positive finding of the MTB gene. Sensitivity to first-line AT was preserved; the patient started AT treatment with the same combination used for her husband (an initial phase lasting 2 months, and a follow-on phase lasting 4 months).
1.3. Case report no. 3
The third report involves the daughter of the aforementioned married couple: a 23-year-old female, vaccinated against TB as a child, mother of a 4-year-old child, smoker since youth (6 pack-years), presenting as not yet seriously ill. The patient occasionally works as a waitress in a bar and resides with her son and parents in the same apartment. She participated in the TB contact investigation on the basis of being a close contact of her father. During the previous month, the patient noticed a cough and weight loss of 3 kg. She was afebrile, no perspiration, and reportedly felt quite well. TST results showed an induration of +16 mm; HIV test results were negative. A chest X-ray showed findings of pulmonary infiltrates in both lungs with numerous caverns in the right upper lobe (Fig. 3).
Fig. 3.
Pulmonary infiltrates in both lungs with numerous caverns in the right upper lobe.
The patient was hospitalized immediately. Sputum was smear-positive and culture-positive for MTB for a period of 2 months. Mycobacterium testing with the Bactec MGIT 960 was also positive. The patient was started on first-line AT therapy with a combination of rifampicin, isoniazid, ethambutol, and pyrazinamide. Her sputum was smear-positive and culture-positive for MTB for a period of 2 months. Given the extent of the findings, the initial phase was extended to three months, and the follow-on phase involved bi-therapy with rifampicin and isoniazid in a daily regime for 4 months.
1.4. Case report no. 4
The patient was the 4-year-old male, son of the abovementioned 23-year-old patient. The child had never been vaccinated against TB due to the lack of TB risk within the family. He resides in the same household as his mother and grandparents. The family reported no health problems for the child. A posterior-anterior chest X-ray showed no pathology in the lung parenchyma. TST results showed an induration of +16 mm and Interferon gamma release assay (IGRA test) was positive. As a very close family contact, the boy was started on isoniazid chemoprophylaxis at a dose of 5 mg/kg of body weight, which was continued for 6 months as treatment for an identified latent tuberculosis infection.
2. Discussion
Individuals who have had close and frequent contact with persons with bacteriologically proven TB undergo TB contact investigations [3]. These individuals are referred for radiographic and bacteriological examinations and TST and/or IGRA tests are also administered. A TB contact investigation of four individuals in one family found TB disease in three adults and a latent TB infection in a 4-year-old boy (the only family member who had never been vaccinated). None of the adults were aware of having had contact with other individuals who had been diagnosed with TB. In addition, none of these 3 patients had been seriously ill recently. Apart from chronic nicotinism, no other risk factors or severe concomitant diseases were present in any family member. Symptoms were not overt in any of these individuals. Patient 1 was alarmed when he experienced sudden hemoptysis, for which he sought medical attention. Patients 2 and 3 were examined during the month following TB detection in Patient 1. Were it not for initiatives aimed at investigating close contacts, these 2 female TB patients would not have sought medical attention of their own volition – and it can be assumed their TB infections would have spread to other individuals. The range of cavernous X-ray findings was widest in Patient 1, and he had the most severe disease symptoms. This suggests that Patient 1 was the primary TB infection source for the other members of the household. Apart from chronic tobacco use, no other risks that might have triggered TB disease were found in Patient 1. The 2 most serious sources of TB infection in the family were Patients 1 and 3, for whom sputum was repeatedly smear-positive and culture-positive for acid-fast bacilli.
It is clear that the most significant sources of TB infection are patients with smear-positive sputum samples, or those with lung tissue decay. Due to the advanced nature of their disease, these types of patients are believed to be infectious for up to 3 months. Patients with findings of culture-positive sputum pose a risk to those in their surroundings for approximately one month [1]. According to a number of published studies TB disease prevalence is 3.1% in investigated contacts, while latent TB infection prevalence is 51.5%. Similarly, TB prevalence in family contacts is 3.1%. The incidence of TB in contacts is highest in the first year after exposure to TB [4]. In the Czech Republic, 8% of contact investigations conducted each year result in findings of TB [2]. Findings during contact investigations assume an up to 10-times higher detection than the estimated TB prevalence in the general population.
Contact investigations of individuals with respiratory symptoms, as well as familial child contacts, are particularly beneficial [4]. The median incubation period is 6 weeks [1]. TB contact investigation results are influenced by the duration, proximity and intensity of exposure to ill individuals [6]. The 4-year-old child was the only family member who did not have TB disease; but he did have a latent TB infection. At the same time, the boy was the only family member who had never been vaccinated against TB.
A latent TB infection is defined as a putative infection that is identified via a positive TST and/or positive interferon γ release assay (IGRA) with an absence of clinical and x-ray findings [1]. According to the World Health Organization recommendations for infected individuals, preventive therapy with isoniazid prevents progression to TB disease [7]. Preventive treatment of latent tuberculosis infections is a particularly important component of TB control strategies in countries with low TB incidence, such as the Czech Republic [6].
3. Conclusion
TB contact investigations for TB patients are a top priority in TB infection control. Identifying individuals with TB disease and latent TB infections is an important step in locating TB infection sources [3]. From an epidemiologically point of view, the most important TB infection sources are patients with tubercle bacilli in their sputum in a volume that is detectable via microscopic examination. These individuals comprise an important target group that represents a significant infectious source of TB known as “open tuberculosis”. To reduce the spread of tuberculosis infection, it is necessary to search for undiagnosed and untreated TB patient sources who pose a considerable risk to those in their environment. Rapid, reliable and high-quality diagnosis is achieved through clinical, radiologic, and laboratory findings. An investigation of close family contacts is rightly recommended as a strategy for early detection of the disease.1The aim of TB contact investigations is the reduction of TB morbidity, interruption of further TB transmission, and preventive treatment of infected persons to prevent the development of TB disease [1], [7]. Preventive therapy with isoniazid is fully indicated in patients who, due to the intensity of contact, are at high risk for developing TB disease (a risk that exceeds the risk of adverse treatment effects) [5].
This communication demonstrates the importance contact investigations, which can detect TB disease even when symptoms are not obvious.
Conflict of interest
None declared.
References
- 1.Erkens C.G.M., Kamphorst M., Abubakar I. Tuberculosis contact investigation binlow prevalence countries: a European consensus. Eur. Res. J. 2010;36:925–949. doi: 10.1183/09031936.00201609. [DOI] [PubMed] [Google Scholar]
- 2.IHIS CZ. Current information; No. 30/2014.
- 3.Blok L., Sahu S., Creswell J. Comparative meta-analysis of tuberculosis contact investigation interventions in eleven high burden countries. Plos One. 2015;10 doi: 10.1371/journal.pone.0119822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fox G.J., Barry S.E., Britton W.J., Marks G.B. Contact investigation for tuberculosis: a systematic review and meta-analysis. Eur. Respir. J. 2013;41:140–156. doi: 10.1183/09031936.00070812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jerene D., Melese M., Kassie Y. The yield of a tuberculosis household contact investigation in two regions of Ethiopia. Int. J. Tuberc. Lung Dis. 2015;19:898–903. doi: 10.5588/ijtld.14.0978. [DOI] [PubMed] [Google Scholar]
- 6.Sloot R., Schim van der Loeff M.F., Kouw P.M., Borgdorff M.W. Yield of tuberculosis contact investigations in Amsterdam: opportunities for improvement. Eur. Respir. J. 2014;44:714–724. doi: 10.1183/09031936.00009114. [DOI] [PubMed] [Google Scholar]
- 7.Yassin M.A., Petrucci R., Garie K.T. Use of tuberculin skin test, IFN- γ-induced protein-10 to identify children with TB infection. Eur. Respir. J. 2013;2013(41):644–648. doi: 10.1183/09031936.00012212. [DOI] [PubMed] [Google Scholar]