Abstract
Objective
Sleep disturbances, including trouble falling and remaining asleep and recurrent nightmares, are symptoms of posttraumatic stress. A growing body of literature indicates that sleep disturbance may also convey vulnerability for the continuation of other symptoms of posttraumatic stress including fear, anxiety, and heightened arousal. However, longitudinal research, which could help understand how these relationships unfold over time, has been limited.
Method
The longitudinal relationships between sleep disturbance and posttraumatic stress were investigated in 779 Palestinian adults randomly selected and interviewed twice during the period of April, 2008 to November, 2008 amidst ongoing violent political turmoil. The recruitment method produced a representative sample and excellent retention. Cross-panel structural equation modeling was used to examine relationships between sleep and distress across two study periods.
Results
Results indicated that initial sleep problems were associated with increased PTSD, depression, and intrapersonal resource loss at follow-up 6 months later, but initial PTSD, depression, and intrapersonal resource loss were not associated with increased sleep problems at follow-up.
Conclusions
Sleep problems may confer vulnerability to longer-term distress in the presence of ongoing political violence. Future research should examine whether interventions targeting trauma-related sleep problems may improve prevention and treatment for PTSD and related disorders.
Keywords: Trauma, Sleep Disturbance, Longitudinal Design
Disruptions in sleep have long been part of our diagnostic criteria for a variety of psychological disorders. However, only recently have researchers begun to examine the complex interactions between sleep and specific pathology. Sleep is an energetic resource (Zohar, Tzischinsky, Epstein, & Lavie, 2005) that is thought to have enabled our evolutionary ancestors to preserve energy, avoid nighttime predation, maximize learning from ontogenic contingencies, and ultimately survive and reproduce (Rechtstaffen, 1998). Deprivation of this energetic resource results in an array of detrimental biopsychosocial consequences (Orzeł-Gryglewska, 2010). At the biochemical level, sleep disruption alters the normal sleep-induced surge of ATP needed for biosynthesis in the brain (Dworak, McCarley, Kim, Kalinchuck & Basheer, 2010) and triggers patterns of altered immune activation (Orzeł-Gryglewska, 2010). At the psychological level, persons deprived of sleep report increased pain and discomfort (Lentz, Landis, Rothermel & Shaver, 1999), evidence mood dysregulation (Walker & van Der Helm, 2009) and exhibit neurocognitive impairments in attention and memory (Durmer & Dinges, 2005). Therefore, disruptions in sleep lead to considerable biological and psychological dysfunction.
Sleep disruption is a significant challenge to individuals suffering from posttraumatic stress disorder (PTSD), a disorder marked by exposure to trauma and subsequent re-experiencing of the traumatic event, heightened arousal, and avoidance of trauma-related stimuli (American Psychiatric Association, 2000; Lamarche and De Koninck, 2007). This is reflected in the diagnostic criteria such that nightmares are included as a symptom of reexperiencing and insomnia is reflected in the hyperarousal cluster. Additionally, a high prevalence of sleep problems are reported among persons exposed to an array of traumatic experiences including sexual abuse (Steine et al., 2011), motor vehicle accidents (Kobayashi et al., 2008), political violence (Palmieri, Chipman, Canetti, Johnson & Hobfoll, 2010), and war (Peterson, Goodie, Satterfield & Brim, 2008). Given the high prevalence of these sleep problems among traumatized populations, some have argued that sleep disturbance is a core feature of PTSD (Spoormaker & Montgomery, 2008; Ross, Ball, Sullivan & Caroff, 1989).
Sleep problems tend to evoke and exacerbate general discomfort and dysphoria (Lentz, Landis, Rothermel & Shaver, 1999; Walker & Van de Helm, 2009), suggesting that negative emotionality in PTSD and other psychological disorders is amplified in the absence of sleep. Individuals with PTSD also report greater fear and anxiety about sleeping due to trauma related nightmares, exhibit conditioned avoidance of sleep and sleep related stimuli, and report higher levels of substance use which interfere with sleep (Lamarche and De Koninck, 2007). In addition to behavioral manifestations of sleep problems, individuals with PTSD demonstrate differences in their sleep architecture (Kobayahsi, Boarts, Delahanty, 2007) which may interfere with normal processes of fear extinction such that habituation to feared stimuli is not retained in memory (Mellman, Pigeon, Nowell & Nolan, 2007; Spoormaker et al., 2010). What is less clear is the critical question of causality, whether sleep disruption is exacerbating PTSD symptoms or vice versa.
Despite clinical and epidemiological evidence linking sleep problems to PTSD, only a few longitudinal studies have evaluated the relationship between sleep problems and PTSD over time (Babson & Feldner, 2010; Kobayashi et al., 2008; Mellman, Bustamente, Fins, Pigeon & Nolan, 2002; Steine et al., 2011; Wright et al., 2011). In a small study of patients admitted to the hospital for traumatic injuries related to motor vehicle accidents, industrial accidents, and gunshots, fragmented REM sleep predicted PTSD six weeks later (Mellman et al., 2002). Conversely, a study of motor vehicle accident survivors found that PTSD and nightmares were shown to predict later sleep problems (Kobayashi et al., 2008). In a two-wave study of U.S. veterans, initial insomnia was significantly associated with increased PTSD and depression eight months later, but PTSD and depression were not associated with later insomnia (Wright et al. 2011). Thus, the literature remains mixed whether sleep problems lead to later psychological problems or whether psychological problems lead to later sleep difficulties. We attempt to help answer this question in the current study.
In the current study, the longitudinal relationships between sleep and PTSD, depression, and intrapersonal resource loss were investigated in a large national random sample of adults living in the Palestinian Authority during 2008. Since the start of the Al Aqsa Intifada, or Second Intifada, in September 2000, to the time of the current study, thousands of Palestinians have been killed in acts of political violence (B'Tselem, 2012). The Israeli-Palestinian conflict occurring during 2008 was greatest during Israel's “Operation Hot Winter” in the early months of that year. Although a truce between Israel and the Palestinian Authority was reached on June 19, 2008 and lasted until December, it is estimated that 455 Palestinians were killed by Israeli forces in the period from January 1 through December 26, 2008 (B'Tselem, 2008). There was also active violence between Palestinian factions during this time. Previous studies demonstrated that ongoing political violence in this region is a source of significant posttraumatic stress and resource loss (Canetti, Galea, Hall, Johnson, Palmieri, & Hobfoll, 2010; Gelkopf, Berger, Bleich, & Silver, 2012; Heath, Hall, Russ, Canetti, & Hobfoll, 2012; Hobfoll, Hall, & Canetti, 2012; Hobfoll, Mancini, Hall, Canetti & Bonanno, 2012). Prior cross-sectional work conducted in neighboring Israel indicated that political violence is a source of markedly high levels of sleep disturbance and psychological distress (Palmieri et al., 2010). The current study extends this work by examining the relationship between sleep problems, each of the PTSD symptom clusters, depression, and intrapersonal resource loss using a more powerful prospective design.
Based on the literature that sleep serves multiple core survival functions, sleep problems were conceptualized as a loss of an energetic resource (Zohar et al., 2005) which broadly impairs the ability to cope with ongoing adversity and trauma (Hobfoll & Lilly, 1993; Hobfoll, 2002). That is, if individuals’ sleep patterns are markedly disrupted, they are expected to have less energy to deal with problems and cope; this in turn may contribute to the loss of intrapersonal resources such as feelings of self-efficacy. As such, the first hypothesis was that sleep problems would have a broad impact on psychological distress, predicting increased symptoms of re-experiencing, avoidance, and hyperarousal, depression, and intrapersonal resource loss.
It is also possible that sleep problems may worsen as a function of earlier PTSD. For instance, individuals may become increasingly anxious and agitated as PTSD transitions to a chronic phase. As emotion regulation resources erode, individuals may struggle to manage symptoms, become increasingly hyperaroused, and evince greater sleep problems. As such, the second hypothesis was that psychological distress would predict later sleep problems. Thus, a reciprocal process in which sleep problems predict greater distress, and greater distress predicts later sleep problems was anticipated. An initial cross-panel model included overall PTSD and sleep problems, nightmares, and depression. A second cross-panel model included PTSD symptom clusters, depression, intrapersonal resource loss, sleep problems, and nightmares.
Method
Participants
The study sample included 889 Palestinians adults living in the Palestinian Authority who participated in a longitudinal population-based cohort study. The sample was averaged 36 years old (SD 13 years), and 53% female. Thirty-two percent had completed high school, 11% completed some college, and 22 % held a university degree or higher. Seventy percent of the sample was married. Of the initial sample, 785 participants (89%) responded to a follow-up survey approximately six months later, with 779 providing complete data. Analysis indicated that data were missing completely at random. The demographic characteristics of the 779 analyzed cases were highly similar to the overall sample.
Procedure
The authors’ institutional review boards approved this study. Data were obtained from a stratified three-stage cluster random sample of Palestinians living in the West Bank, Gaza Strip, and East Jerusalem. Face-to-face interviews were conducted at the participants’ homes in 60 sampling points chosen randomly according to population. Households were randomly selected, and Kish tables were used to randomly select participants within selected households. Each household was visited on at least three occasions to maximize response rates. All interviewers were same-gender Palestinians and trained in interviewing. The interviews were conducted between April 24, 2008 and May 17, 2008, and again between October 15, 2008 and November 1, 2008.
Measures
Trauma exposure
Trauma exposure was measured by the number of times individuals were directly or indirectly exposed to political violence. Sample questions included, “Have you witnessed Israeli attacks or violence among Palestinian factions or been present at a site where there were injuries or fatalities?”, “Have you experienced a death of a family member or a friend as a result of Israeli attacks or violence among Palestinian factions?”, and “Have you experienced an injury of yourself, a family member or a friend in as a result of Israeli attacks or violence among Palestinian factions?” If exposure to political violence was endorsed, the exposure was further characterized with follow up questions such as “If there was more than one person among your family or friends who was killed, can you tell us how many were killed?” and “What is your relationship to the person who was killed?”. The trauma exposures were summed to derive a total score that represented the total number of traumas the participant experienced. Because exposure to one trauma does not necessarily portend exposure to another, internal consistency was not tabulated. The variable was treated as a manifest variable in the structural model.
Sleep problems
Sleep problems were assessed with the following two items: “how many nights have you experienced difficulty sleeping in the past two weeks?” and “on average, how many hours have you slept each night in the past two weeks?” The number of hours slept is a component of sleep assessed by standardized sleep measures (Hayes & Stuart, 1992; Buysse, Reynolds, Monk, Berman & Kupfer, 1988). Results from two samples demonstrated that a single-item sleep quality scale demonstrated adequate test-retest reliability, and showed convergent validity with a lengthier sleep scale (Cappelleri, Bushmakin, McDermott, Sadosky, Petrie & Martin (2009). The correlations between these two items in the current study were r =−.36 at time 1, and r = −.20 at time 2, indicated they comprise two separate facets of sleep. These two items were modeled as a latent variable in the structural equation model and provided good fit to the underlying data. The variable was scaled based on nights with trouble sleeping such that a higher level of the latent variable indicated more sleep problems.
Post-traumatic Stress Disorder (PTSD) symptom severity
PTSD symptom severity occurring during the past month was measured using the PTSD Symptom Scale (PSS; Foa, Riggs, Dancu, & Rothbaum, 1993). Respondents rated the severity of PTS symptoms on a 4-point Likert scale from 0 (not at all) to 3 (very much) associated with exposure to political violence (i.e., the target criterion). This scale has been used previously in non-Western, low income regions (Johnson & Thompson, 2008) and within the Palestinian population (e.g., Hobfoll et al., 2010; Heath et al., 2012). Following the example of Wright et al. (2011) the nightmare and insomnia items were removed. Items were summed to create three scales corresponding to the DSM IV PTSD symptom clusters of re-experiencing, avoidance, and hyperarousal. These scales were entered as manifest variables in the structural model. Internal consistency for the 15-item scale was good at time 1 (α=.84), and time 2 (α=.87). Likewise, internal consistency for each of subscales the scales was good at time one (α=.71 to α=.73), and time two (α=.65 to α=.79).
Nightmares
The single PTSD item pertaining to nightmares was used to measure trauma-related nightmares.
Depression symptoms
Depression symptoms were measured using the Patient Health Questionnaire - 9 (PDQ-9; Kroenke, Spitzer, & Williams, 2001). Participants respond to the nine-item measure by rating the frequency of a depression symptom from 1 (not at all) to 4 (nearly every day) for the two weeks prior to the administration of the measure. Example items are “Little interest or pleasure in doing things” and “Feeling low, depressed or hopeless.” As was done for the PTSD measure, one item measuring insomnia was removed. Internal consistency for the eight-item was good at time 1 (α=.87) and time 2 (α=.89).
Intrapersonal resource loss
Intrapersonal resource loss was measured using 5 items from the COR-E questionnaire (Hobfoll & Lilly, 1993). Example items asked participants to indicate the extent that they had lost: “the feeling that you are a successful person,” “sense of control in your life,” and “hope.” For all items, participants indicated the degree of their resource loss on a 4-point scale, with item responses ranging from 1 (did not lose at all) to 4 (lost very much). Internal consistency was good at time 1 (α=.86) and time 2 (α=.89).
Analyses
Basic descriptive statistics were computed with SPSS version 19 and correlation matrices are included as an online supplement. The cross-panel structural equation model was computed using AMOS version 20. Because 11 percent of the sample was lost to follow up, multiple imputation was used to replace missing data. Missing items were missing completely at random (MCAR) as measured by Little's MCAR χ2(34, N = 889) = 34.93, p > .05. This tests supports a complete cases analysis as the smaller sample is not expected to differ from the overall sample with missing data. Therefore, missing data were removed via listwise deletion. Path analysis was performed using the current guidelines of the American Psychological Association (APA; McArdle, Ferrer, & Grimm, 2011). Model goodness of fit was assessed using the residual mean squared error of approximation (RMSEA) with values below .08 and a lower bound of the 90% confidence interval less than .05 indicating adequate fit (Browne & Cudeck, 1993), and the Comparative Fit Index (CFI; Bentler, 1990), with values greater than .95 indicating good fit.
Results
Respondents reported on average three exposures to political violence (median=2, SD=5, range=0 to 60). Of the total sample, 50 percent reported witnessing political violence, 39 percent reported having at least one family member or friend injured, 48 percent reported having at least one family member or friend killed, and 7 percent reported being directly injured. Taken together, 68 percent of the sample reported at least one exposure to political violence. Results indicated that on average this sample experienced sleep difficulty, and high levels of PTSD symptom severity at both study points. During both time periods participants reported approximately 5 nights with difficulty sleeping in the prior two weeks. The initial mean reported hours slept was 6.54 (SD 1.91), and the mean reported hours slept at follow up was 6.43 (SD 2.01). The average PTSD scores of 20.84 and 18.74 fell above a suggested clinical cut-off of 14 for the PSS-SR (Coffey, 2006). Depression scores of 9.86 at time one and 8.51 at time two suggested participants on average endorsed mild levels of depression. A meta-analysis suggests that the measure is an acceptable screen for major depression disorder when cut-offs between 8 and 11 are used (Manea, Gilbody, McMillan, 2011). Thus, on average, participants reported clinical levels of PTSD and Depression symptoms.
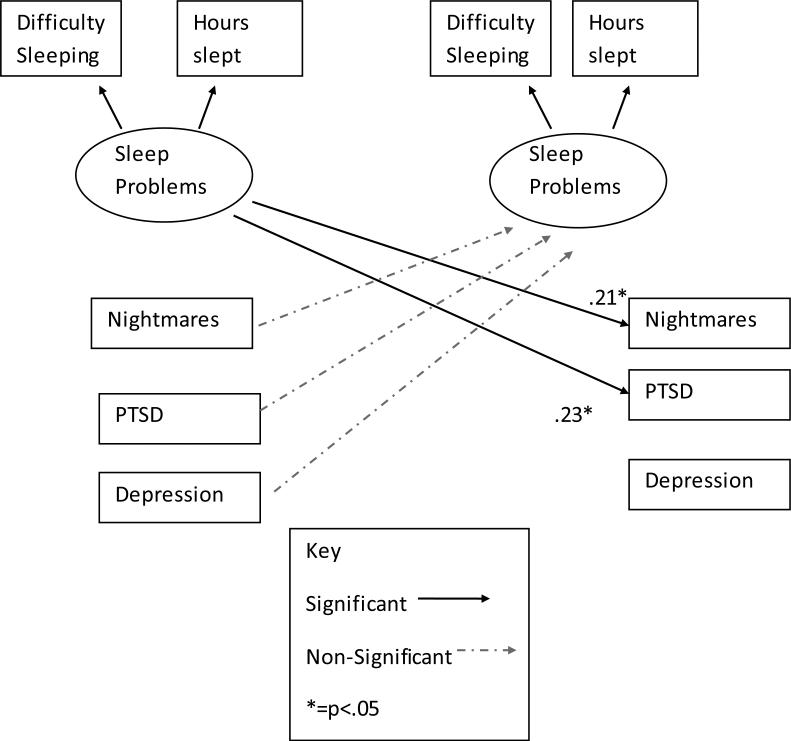
The correlation matrix of variables entered in the first model is available as an online supplement. The unconstrained measurement model provided adequate fit to the data to permit further analysis χ2 (16) = 60.53, p <.01, CFI = .98; RMSEA= .06 (90% CI = .04 - .08). Next we imposed constraints in our hypothesized cross-panel structural equation model (see Figure 1.) The cross-panel structural equation model fit the underlying data well χ2(17) = 61.10, p <.01, CFI = .98; RMSEA= .06 (90% CI = .04 - .08).
Figure 1.
Cross panel SEM of sleep and posttraumatic stress
Table 1 reports standardized regression weights for the structural equation model. All autoregressive paths were significant such that initial sleep problems were associated with later sleep problems, initial nightmares were associated with later nightmares, initial PTSD symptoms were associated with later PTSD symptoms, and initial depression symptoms were associated with later depression suggesting a moderate degree of stability in sleep disturbance and distress across the study period. Sleep problems were significantly correlated with, nightmares (β = .22, p <.05), PTSD (r = .37, p <.05) and Depression (r = .47, p <.05) at time one. Trauma exposure was significantly related to PTSD at time one (β = .14, p <.01) and time two (β = .07, p <.05), and depression at time one (β = .13, p <.01). Trauma exposure was also significantly related to sleep problems at time one (β = .17, p <.01) and time two (β = .10, p <.05). As a test of our first hypothesis, after controlling for the effect of initial PTSD, initial sleep problems were significantly associated with later PTSD symptom severity (β = .23, p <.01). Sleep problems trended toward a relationship with later depression symptom severity (β = .09, p <.10). In a test of our second hypothesis, PTSD was not significantly associated with later sleep problems.
Table 1.
Standardized Regression Weights in Model 1.
| T1 Exposure | T1 Sleep Problems | T1 Nightmares | T1 PTSD | T1 Depression | |
|---|---|---|---|---|---|
| T1 Exposure | .17* | .08* | .14* | .13* | |
| T2 Sleep Problems | .10* | .61* | .07 | −.08 | .04 |
| T2 Nightmares | .03 | .21* | .24* | .07 | −.03 |
| T2 PTSD | .09* | .23* | .10* | .31* | |
| T2 Depression | .04 | .09 | .10* | .38* |
Note.
=p <.05, bolded values pertain to study hypotheses.
In the same model, and in parallel to the finding that sleep problems predict later PTSD but not vice versa, nightmares independently predicted later PTSD (β = .10, p <.05) and depression two (β = .10, p <.05). Initial depression and PTSD did not predict later nightmares. Taken together these findings suggest that sleep disturbances in the form of nightmares and general sleep difficulty (e.g. trouble sleeping, and short sleep duration) each uniquely contribute to the prediction of later trauma–related distress.
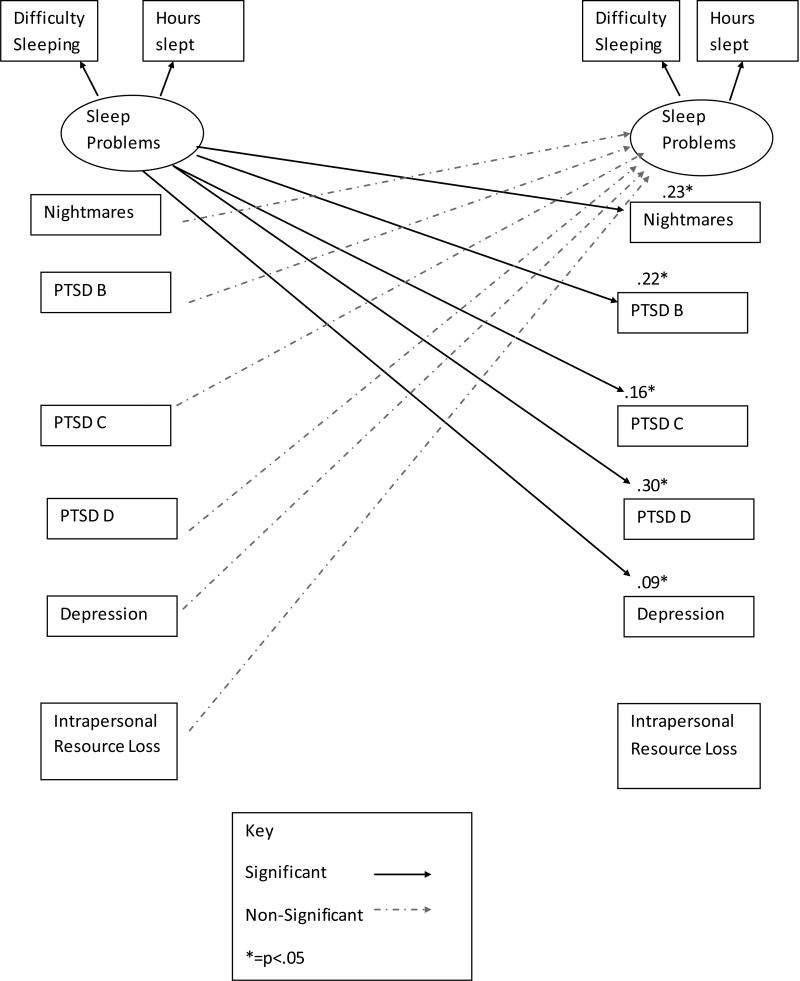
PTSD Symptom Clusters, Depression, and Intrapersonal Loss
The initial model was followed-up by a second that separated PTSD symptom severity into the three diagnostic clusters, intrusive recollection, avoidance/numbing, and hyper-arousal, and also added intrapersonal resource loss to the cross-panel structural model. The correlation matrix of variables included in the second model is available as an online supplement. As above, sleep symptoms were removed from the severity ratings of PTSD and depression. The cross-panel structural equation model fit the underlying data well χ2(47) = 158.17, p <.01, CFI = .98; RMSEA= .06 (90% CI = .05 - .07).
Table 2 reports standardized regression weights from the second model. Review of standardized regression weights revealed a similar pattern to model one. Autoregressive paths for sleep problems, PTSD symptom clusters, depression, and intrapersonal resource loss were significant. Exposure to trauma at time one was significantly associated with sleep problems (β = .17, p <.01), nightmares (β = .08, p <.01), re-experiencing (β = .12, p <.01), avoidance (β = .10, p <.01), hyperarousal (β = .12, p <.01), depression (β = .13, p <.01), and intrapersonal resource loss (β = .12, p <.01) at time one. Exposure to trauma at time one remained significantly associated with sleep problems (β = .10, p <.05), re-experiencing (β = .09, p <.01), and intrapersonal resource loss (β = .07, p <.05) at time two.
Table 2.
Standardized Regression Weights in Model 2.
| T1 Exposure | T1 Sleep Problems | T1 Nightmares | T1 PTSD B | T1 PTSD C | T1 PTSD D | T1 Depression | T1 IntraLoss | |
|---|---|---|---|---|---|---|---|---|
| T1 Exposure | .17* | .08 | .12* | .10* | .12* | .13* | .12* | |
| T2 Sleep Problems | .10* | .63* | .07 | −.02 | −.05 | −.02 | .03 | −.05 |
| T2 Nightmares | .03 | .23* | .24* | .08 | −.01 | −.04 | −.01 | .01 |
| T2 PTSD B | .09* | .22* | .13* | .24* | ||||
| T2 PTSD C | .06 | .16* | .07 | .29* | ||||
| T2 PTSD D | .05 | .30* | .13* | .21* | ||||
| T2 Depression | .04 | .09* | .11* | .34* | ||||
| T2 IntraLoss | .08 | .06 | .09* | .39* |
Note.
=p <.05, bolded values pertain to study hypotheses.
As a test of our first hypothesis, sleep problems were associated with later PTSD symptom clusters including re-experiencing (β = .21, p <.01), avoidance (β = .16, p <.01), and hyper-arousal (β = .30, p <.01). Sleep problems were also associated with later depression (β = .09, p <.05). As a test of our second hypothesis, nightmares, PTSD symptom clusters, depression, and intrapersonal resource loss were not associated with later sleep disturbance, all ps >.18. Follow-up contrasts indicated that the effect of sleep on later PTSD hyperarousal symptoms trended toward being greater than the effect of sleep on later depression symptoms, Z=1.92, p<.10. No other contrasts between PTSD symptoms and depression trended toward significance, Zs =.33 – 1.24, ps>.10. The lack of difference offered further support for the hypothesis that sleep disturbance in the context of political violence confers a general vulnerability to later emotional distress.
In parallel to the finding that sleep problems predict later distress but not vice versa, in the same model nightmares predicted later re-experiencing two (β = .13, p <.05), hyperarousal two (β = .10, p <.05), depression two (β = .11, p <.05), and intrapersonal resource loss two (β = .09, p <.05). Initial re-experiening, hyperarousal, depression, and intrapersonal resource loss did not predict later nightmares. Similar to model one, these findings suggest that sleep disturbances in the form of nightmares and general sleep problems (e.g. trouble sleeping, and short sleep duration) each uniquely contribute to the prediction of later trauma–related distress.
Discussion
This study explored the longitudinal relationship between trauma exposure, sleep problems, PTSD, depression symptom severity, and intrapersonal resource loss in a large national sample of trauma-exposed Palestinians. Trauma exposure was associated with later sleep problems, PTSD symptom severity, depression symptom severity, and intrapersonal resource loss. In support of our first hypothesis, the common trauma-related sleep problems of insomnia-like sleep problems and nightmares were each independently related to later psychological distress. In contrast to our second hypothesis, initial psychological distress was not related later to either of these sleep problems after accounting for the relationships between earlier sleep problems. Moreover, the finding that this pattern of results held across the three symptom clusters of PTSD, depression, and intrapersonal resource loss suggests that sleep problems are associated with a general increase in later trauma-associated emotional distress, but these symptoms do not contribute to later changes in sleep problems.
These findings build upon previous research on sleep, PTSD, and depression (Wright et al., 2011; Mellman, Bustamente, Fins, Pigeon & Nolan, 2002; Mellman, Pigeon, Nowell & Nolan, 2007) by studying these problems in a large randomized sample. The models supported our first hypothesis by replicating the relationship between sleep problems and later PTSD and depression in a national sample of highly traumatized civilians. Whereas mobility within the Wright et al. (2011) study of U.S. veteran population resulted in a follow-up rate of 34%, the current sampling method yielded follow up rate of 89%. In addition the sample included a higher ratio of female participants (52 % female vs. 4% female), thus making the findings more likely to be generalizable to women.
The study findings also build upon the sleep and distress literature by anchoring the relationship between sleep problems and psychological distress within the broader literature on stress and coping (Hobfoll, 1998; Zohar et al., 2005). Conservation of Resources Theory maintains that persons are highly motivated to maintain and preserve valued resources, and that stress increases as these resources are depleted (Hobfoll, 1988; 2001; 2002). A key corollary is that loss of resources has a more potent impact than gain of resources. As persons struggle to preserve a dwindling resource, in this case sleep, the potential for loss spirals ensues (e.g., Health et al., 2012). In the current study, PTSD, and depression increased as a function of sleep problems while intrapersonal resources such as hope, and self-efficacy were diminished by nightmares.
Contrary to our second hypothesis, initial PTSD, depression, and intrapersonal loss were not significantly related to sleep problems at follow-up. One possibility is that psychological distress may have interfered with participants’ sleep habits prior to the study period, and that these sleep problems have simply stabilized (Lamarche and De Koninck, 2007). Future research should assess whether the influence of traumatic stress, sleep hygiene, and other factors shift as trauma exposure transitions from an acute to chronic situation. For example, symptoms may have led to depleted sleep problems initially, before the study period, and these problems remained unchanged as sleep problems lead to exacerbated symptoms of psychological distress. Alternatively, the sleep problems in our current study were pervasive such that the participants may have reached the low-point related to their sleep problems and that further declines in sleep were limited.
Limitations
The current findings are qualified by several limitations. We relied on participant self-reported sleep problems that could be biased by recall. Actigraphic or ambulatory sleep monitoring could offer more objective evaluation of sleep problems in future studies. Furthermore, a major limitation of this study is that our sleep measure was necessarily short owing to the space limitations inherent in conducting such a large-scale longitudinal study. That said, brief sleep scales converge with more comprehensive sleep measures (Cappelleri et al., 2009), and we utilized two items that were face valid, readily reportable by participants, and similar in content to items from lengthier sleep assessments. Although difficulty sleeping and sleep duration are face valid indicators of common sleep problems such as insomnia, research is needed to clarify specific sources of sleep problems such as primary-insomnia, restless leg syndrome, and sleep apnea.
Although a more thorough sleep evaluation would provide a more valid assessment of sleep problems, this concern is partially mitigated by several findings that support the construct validity of our latent sleep problems variable. First, our initial measurement model demonstrated adequate fit. Second, the latent variable demonstrated considerable test-retest reliability over the six-month study period (r =.61 to .62). Finally, the latent variable demonstrated convergence via a small but significant correlation with nightmares, suggesting that these sleep problems and nightmares are related, but distinct, sleep disturbances that may each independently exacerbate later trauma-related distress. Future studies should include more comprehensive sleep scales such as the Medical Outcomes Study Sleep Scale (Hayes & Stuart, 1992) and the Pittsburg Sleep Quality Inventory (Buysse et al., 1988). Medical record reviews may also provide important information about objectively diagnosed sleep disorders.
Conclusions
Our findings indicate that the relationship between sleep problems and PTSD occurs within a broader context of mood disturbance, and diminished intrapersonal resources. The link between sleep problems and diminished coping in the face of traumatic stress is further supported by findings that sleep problems are also associated with trauma-related dissociative symptoms (van der Kloet, Merkelbach & Giesbrecht, 2012). In addition to PTSD and mood disturbance, future longitudinal studies of trauma-related sleep problems should examine other forms of distress such as paranoia, hostility, and obsessive-compulsive symptoms that are potentially exacerbated by trauma and resource loss. Studies should also examine how depletion of coping resources such as acceptance, and psychological flexibility may mediate the relationship between sleep and general trauma-related distress (Bond et al., 2011; Tull, Barrett, McMillian & Roemer, 2007).
The current investigation suggests that sleep problems led to further symptoms of PTSD and therefore suggests that if left untreated, sleep disturbance could lead to the maintenance, exacerbation or new onset of PTSD. Indeed, sleep problems can be treatment-refractory symptoms that remain problematic even following empirically supported front line treatments for PTSD such as prolonged exposure therapy (Belleville, Guay & Marchand, 2011). Clinical interventions that address trauma-related sleep problems directly may be beneficial in lessening prolonged PTSD reactions, enhancing mood, and bolstering coping. Our findings also lend support for interventions targeting early sleep problems in the prevention of later PTSD and trauma-related distress. These findings echo the call by Nappi, Drummond, and Hall (2012) for a more thoroughgoing examination of behavioral and pharmacological interventions for trauma-related sleep disorders that incorporate randomized trials and standardized sleep measures, and exploration of acceptance-based therapies for trauma-related sleep problems that remain difficult to treat (see Hayes, Follette & Linehan, 2004).
Supplementary Material
Figure 2.
Cross-Panel SEM of Sleep Problems, PTSD Clusters, Depression, and Resource Loss
Acknowledgments
This research was made possible in part by a grant from the National Institute of Mental Health (RO1MH073687). National Institute of Mental Health Psychiatric Epidemiology Training Program T32MH014592-35 supported Dr. Hall's contribution to this work (PI: P. Zandi).
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed., text rev. Author; Washington, DC: 2000. [Google Scholar]
- Babson KA, Feldner MT. Temporal relations between sleep problems and both traumatic event exposure and PTSD; a critical review of the empirical literature. Journal of Anxiety Disorders. 2010;24(1):1–15. doi: 10.1016/j.janxdis.2009.08.002. doi:10.1016/j.janxdis.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belleville G, Guay S, Marchand A. Persistence of sleep disturbances following cognitive-behavior therapy for posttraumatic stress disorder. Journal of Psychosomatic Research. 2011;70(4):318–327. doi: 10.1016/j.jpsychores.2010.09.022. doi:10.1016/j.jpsychores.2010.09.022. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Sage; Newbury Park, CA: 1993. pp. 136–162. [Google Scholar]
- B'Tselem Human rights in the occupied territories: 2008 Annual report. 2008 Retrieved from: http://www.btselem.org/download/200812_annual_report_eng.pdf.
- B'Tselem Statistics: Fatalities. 2012 Retrieved from: http://old.btselem.org/statistics/english/Casualties.asp.
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry research. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Canetti D, Galea S, Hall BJ, Johnson RJ, Palmieri P, Hobfoll SE. Exposure to Prolonged socio-political conflict and the risk of PTSD and depression among Palestinians. Psychiatry. 2010;73:219–231. doi: 10.1521/psyc.2010.73.3.219. [DOI] [PubMed] [Google Scholar]
- Cappelleri JC, Bushmakin AG, McDermott AM, Sadosky AB, Petrie CD, Martin S. Psychometric properties of a single-item scale to assess sleep quality among individuals with fibromyalgia. Health and Quality of Life Outcomes. 2009;7(1):54. doi: 10.1186/1477-7525-7-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey SR, Gudmundsdottir B, Beck JG, Palyo SA, Miller L. Screening for PTSD in motor vehicle accident survivors using the PSS-SR and IES. Journal of Traumatic Stress. 2006;19(1):119–128. doi: 10.1002/jts.20106. doi:10.1002/jts.20106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durmer JS, Dinges DF. Neurocognitive consequences of sleep deprivation. Seminars in neurology. 2005;25(1):117–125. doi: 10.1055/s-2005-867080. [DOI] [PubMed] [Google Scholar]
- Dworak M, McCarley RW, Kim T, Kalinchuk AV, Basheer R. Sleep and brain energy levels: ATP changes during sleep. The Journal of Neuroscience. 2010;30(26):9007–9016. doi: 10.1523/JNEUROSCI.1423-10.2010. doi:10.1523/JNEUROSCI.1423-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress. 1993;6(4):459–473. doi:10.1002/jts.2490060405. [Google Scholar]
- Gelkopf M, Berger R, Bleich A, Silver RC. Protective factors and predictors of vulnerability to chronic stress: A comparative study of 4 communities after 7 years of continuous rocket fire. Social Science & Medicine. 2012;74(5):757–766. doi: 10.1016/j.socscimed.2011.10.022. doi:10.1016/j.socscimed.2011.10.022. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Folette VM, Linehan MM. Mindfulness and acceptance; expanding the cognitive behavioral tradition. Guilford; New York: 2004. [Google Scholar]
- Hays RD, Stewart AL. Sleep measures. In: Stewart AL, Ware JE, editors. Measuring functioning and well-being: The Medical Outcomes Study approach. Duke University Press; Durham, NC: 1992. pp. 235–259. [Google Scholar]
- Heath N, Hall BJ, Russ EU, Canetti D, Hobfoll SE. Reciprocal relationships between resource loss and psychological distress following exposure to political violence: an empirical investigation of COR theory's loss spirals. Anxiety, Stress, and Coping. doi: 10.1080/10615806.2011.628988. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heath NM, Hall BJ, Canetti D, Hobfoll SE. Exposure to political violence, psychological distress, resource loss, and benefit finding as predictors of domestic violence among palestinians. Psychological Trauma: Theory, Research. 2012 doi:10.1037/a0028367. [Google Scholar]
- Hobfoll SE. The ecology of stress. Hemisphere Publishing Corp.; Washington, DC, US: 1988. [Google Scholar]
- Hobfoll SE. The influence of culture, community, and the nested-self in the stress process: Advancing conservation of resources theory. Applied Psychology: An International Review. 2001;50(3):337–370. doi:10.1111/1464-0597.00062. [Google Scholar]
- Hobfoll SE. Social and psychological resources and adaptation. Review of General Psychology. 2002;6(4):307–324. doi:10.1037/1089-2680.6.4.307. [Google Scholar]
- Hobfoll SE, Hall BJ, Canetti D. Political violence, psychological distress, and perceived health: A longitudinal investigation in the Palestinian Authority. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4:9–21. doi: 10.1037/a0018743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobfoll SE, Lilly RS. Resource conservation as a strategy for community psychology. Journal of Community Psychology. 1993;21(2):128–148. doi:10.1002/1520-6629(199304)21:2<128::AID-JCOP2290210206>3.0.CO;2-5. [Google Scholar]
- Hobfoll SE, Mancini A, Hall BJ, Canetti D, Bonanno G. The limits of Resilience: Distress following chronic political violence in the Palestinian Authority. Social Science and Medicine. 2011;72:1400–1408. doi: 10.1016/j.socscimed.2011.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson H, Thompson AR. The development and maintenance of post-traumatic stress disorder (PTSD) in civilian adult survivors of war trauma and torture: A review. Clinical Psychology Review. 2008;28(1):36–47. doi: 10.1016/j.cpr.2007.01.017. doi:10.1016/j.cpr.2007.01.017. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. doi:10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamarche LJ, De Koninck J. Sleep disturbance in adults with posttraumatic stress disorder: A review. Journal of Clinical Psychiatry. 2007;68(8):1257–1270. doi: 10.4088/jcp.v68n0813. doi:10.4088/JCP.v68n0813. [DOI] [PubMed] [Google Scholar]
- Lentz MJ, Landis CA, Rothermal J, Shaver JL. Effects of selective slow wave sleep disruption on musculoskeletal pain and fatigue in middle aged women. Journal of Rheumatology. 1999;26(7):1586–1592. [PubMed] [Google Scholar]
- Kobayashi I, Boarts JM, Delahanty DL. Polysomnographically measured sleep abnormalities in PTSD: A meta-analytic review. Psychophysiology. 2007;44(4):660–669. doi: 10.1111/j.1469-8986.2007.537.x. [DOI] [PubMed] [Google Scholar]
- Kobayashi I, Sledjeski EM, Spoonster E, Fallon WF, Delahanty DL. Effects of early nightmares on the development of sleep disturbances in motor vehicle accident victims. Journal of Traumatic Stress. 2008;21(6):548–555. doi: 10.1002/jts.20368. doi:10.1002/jts.20368. [DOI] [PubMed] [Google Scholar]
- Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the patient health questionnaire (PHQ-9): A meta-analysis. CMAJ. 2012;184(3):E191–E196. doi: 10.1503/cmaj.110829. Retrieved from www.scopus.com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McArdle JJ, Ferrer E, Grimm KJ. Handbook on data analysis in longitudinal research: Advanced Training Institute on structural equation modeling. University of California; American Psychological Association; Davis: 2011. [Google Scholar]
- Mellman TA, Bustamante V, Fins AI, Pigeon WR, Nolan B. REM sleep and the early development of posttraumatic stress disorder. The American Journal of Psychiatry. 2002;159(10):1696–1701. doi: 10.1176/appi.ajp.159.10.1696. doi:10.1176/appi.ajp.159.10.1696. [DOI] [PubMed] [Google Scholar]
- Mellman TA, Pigeon WR, Nowell PD, Nolan B. Relationships between REM sleep findings and PTSD symptoms during the early aftermath of trauma. Journal of Traumatic Stress. 2007;20(5):893–901. doi: 10.1002/jts.20246. doi:10.1002/jts.20246. [DOI] [PubMed] [Google Scholar]
- Orzeł-Gryglewska J. Consequences of sleep deprivation. International Journal of Occupational Medicine and Environmental Health. 2010;23(1):95–114. doi: 10.2478/v10001-010-0004-9. doi:10.2478/v10001-010-0004-9. [DOI] [PubMed] [Google Scholar]
- Palmieri PA, Chipman KJ, Canetti D, Johnson RJ, Hobfoll SE. Prevalence and correlates of sleep problems in adult israeli Jews exposed to actual or threatened terrorist or rocket attacks. Journal of Clinical Sleep Medicine. 2010 Dec 15;6(6) Retrieved from www.csa.com. [PMC free article] [PubMed] [Google Scholar]
- Peterson AL, Goodie JL, Satterfield WA, Brim WL. Sleep disturbance during military deployment. Military Medicine. 2008;173(3):230–235. doi: 10.7205/milmed.173.3.230. Retrieved from www.csa.com. [DOI] [PubMed] [Google Scholar]
- Pigeon WR, Cerulli C, Richards H, He H, Perlis M, Caine E. Sleep disturbances and their association with mental health among women exposed to intimate partner violence. Journal of Women's Health. 2011;20(12):1923–1929. doi: 10.1089/jwh.2011.2781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rechtschaffen A. Current perspectives on the function of sleep. Perspectives in Biological Medicine. 1998;41:359–390. doi: 10.1353/pbm.1998.0051. [DOI] [PubMed] [Google Scholar]
- Ross RJ, Ball WA, Sullivan KA, Caroff SN. Sleep disturbance as the hallmark of posttraumatic stress disorder. The American Journal of Psychiatry. 1989;146(6):697–707. doi: 10.1176/ajp.146.6.697. Retrieved from www.csa.com. [DOI] [PubMed] [Google Scholar]
- Spoormaker VI, Montgomery P. Disturbed sleep in post-traumatic stress disorder: Secondary symptom or core feature? Sleep Medicine Reviews. 2008;12(3):169–184. doi: 10.1016/j.smrv.2007.08.008. doi:10.1016/j.smrv.2007.08.008. [DOI] [PubMed] [Google Scholar]
- Spoormaker VI, Sturm A, Andrade KC, Schröter MS, Goya-Maldonado R, Holsboer F, Czisch M. The neural correlates and temporal sequence of the relationship between shock exposure, disturbed sleep and impaired consolidation of fear extinction. Journal of Psychiatric Research. 2010;44(16):1121–1128. doi: 10.1016/j.jpsychires.2010.04.017. doi:10.1016/j.jpsychires.2010.04.017. [DOI] [PubMed] [Google Scholar]
- Steine IM, Harvey AG, Krystal JH, Milde AM, Grønli J, Bjorvatn B, Pallesen S. Sleep disturbances in sexual abuse victims: A systematic review. Sleep Medicine Reviews. 2012;16(1):15–25. doi: 10.1016/j.smrv.2011.01.006. Retrieved from www.scopus.com. [DOI] [PubMed] [Google Scholar]
- Tull MT, Barrett HM, McMillan ES, Roemer L. A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behavior Therapy. 2007;38:303–313. doi: 10.1016/j.beth.2006.10.001. doi:10.1016/j.beth.2006.10.001. [DOI] [PubMed] [Google Scholar]
- van der Kloet D, Merckelbach H, Giesbrecht T, Lynn SJ. Fragmented sleep, fragmented mind: The role of sleep in dissociative symptoms. Perspectives on Psychological Science. 2012;7(2):159–175. doi: 10.1177/1745691612437597. Retrieved from www.scopus.com. [DOI] [PubMed] [Google Scholar]
- Walker MP, van der Helm E. Overnight therapy? the role of sleep in emotional brain processing. Psychological Bulletin. 2009;135(5):731–748. doi: 10.1037/a0016570. doi:10.1037/a0016570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright KM, Britt TW, Bliese PD, Adler AB. Insomnia severity, combat exposure and mental health outcomes. Stress and Health: Journal of the International Society for the Investigation of Stress. 2011;27(4):325–333. doi:10.1002/smi.1373. [Google Scholar]
- Wright KM, Britt TW, Bliese PD, Adler AB, Picchioni D, Moore D. Insomnia as predictor versus outcome of PTSD and depression among iraq combat veterans. Journal of Clinical Psychology. 2011;67(12):1240–1258. doi: 10.1002/jclp.20845. doi:10.1002/jclp.20845. [DOI] [PubMed] [Google Scholar]
- Zohar D, Tzischinsky O, Epstein R, Lavie P. The effects of sleep loss on medical residents' emotional reactions to work events: A cognitive-energy model. Sleep: Journal of Sleep and Sleep Disorders Research. 2005;28(1):47–54. doi: 10.1093/sleep/28.1.47. Retrieved from www.csa.com. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.