Abstract
Objective Health care proxy (HCP) documentation is suboptimal. To improve rates of proxy selection and documentation, we sought to develop and evaluate a web-based interview to guide patients in their selection, and to capture their choices in their electronic health record (EHR).
Methods We developed and implemented a HCP interview within the patient portal of a large academic health system. We analyzed the experience, together with demographic and clinical factors, of the first 200 patients who used the portal to complete the interview. We invited users to comment about their experience and analyzed their comments using established qualitative methods.
Results From January 20, 2015 to March 13, 2015, 139 of the 200 patients who completed the interview submitted their HCP information for their clinician to review in the EHR. These patients had a median age of 57 years (Inter Quartile Range (IQR) 45–67) and most were healthy. The 99 patients who did not previously have HCP information in their EHR were more likely to complete and then submit their information than the 101 patients who previously had a proxy in their health record (odds ratio 2.4, P = .005). Qualitative analysis identified several ways in which the portal-based interview reminded, encouraged, and facilitated patients to complete their HCP.
Conclusions Patients found our online interview convenient and helpful in facilitating selection and documentation of an HCP. Our study demonstrates that a web-based interview to collect and share a patient’s HCP information is both feasible and useful.
INTRODUCTION
Written advance directives (ADs) in the form of living wills and health care proxies (HCP), allow patients to formalize their wishes for future health care before they reach decisional incapacity. Having an AD in place increases the likelihood of a patient’s wishes being honored, often resulting in less aggressive care, lower cost1 and less likelihood of death in the hospital.2 Though studies have shown an increasing upward trend for patients having ADs,3,4 the rate of implementation is still suboptimal.5
The Patient Self-Determination Act of 19906 and the Joint Commission on Accreditation of Healthcare Organizations have set requirements regarding ADs.7 Despite policy work and clinicians’ understanding of the importance of patients having an AD, clinicians are often unable to spend adequate time with patients to guide them through advance care planning due to time and cost constraints.8 Additionally, all parties may find these conversations uncomfortable, which further impedes their occurrence. A recent study of Medicare beneficiaries showed that <1% of study participants had patient-physician end of life discussions during routine care.9
Prior work has looked into improving the completeness of HCP documentation.10–13 Reminders for patients about advanced care planning, typically through mailings, have been shown to be more effective than reminders to clinicians.7,8 Computers have also been used to help patients navigate the process with good effect.14,15 Online resources do exist to enable patients to document their HCP and ADs and some offer to share this information with patients’ clinicians – many for a fee.12,13 However, we have yet to find a report of a health care system with advance care planning tools that are integrated with an electronic health record (EHR) system.
Computer-based medical interviewing was first reported in 19661 6 and studies over the years have demonstrated the potential of patient-computer dialogue to obtain comprehensive, accurate medical histories that are well received by patients and clinicians.17–21 Studies have also demonstrated that computer-based interviews can sometimes obtain sensitive, even potentially embarrassing information that might not otherwise have been obtained by a clinician interviewer.17,22–26
Patient access to effective and tailored patient education and electronic patient-provider communication tools can lead to improved patient-centered care.27–29 Patient portals, are secure web sites that enable patients to connect with their clinicians and their medical center’s EHR system in a protected manner, and are good platforms for patient engagement tools.30 We report here our study of a HCP interview for use by patients over our patient portal, PatientSite, to assign a proxy for themselves and, when they wish to do so, to submit and thereby share their proxy information with their clinicians who can then integrate this information into the patients’ EHRs.
METHODS
Setting
This study took place at Beth Israel Deaconess Medical Center (BIDMC), a 649 bed urban, academic medical center affiliated with Harvard Medical School. BIDMC has 2353 staff physicians and cared for more than 269 000 patients in 2014 at the main campus in Boston, MA. BIDMC has a rich history in clinical computing, having had one of the early hospital-wide clinical computing systems,31 with a home-grown EHR (webOMR)32 and patient portal (PatientSite).33 BIDMC is also one of the sponsor hospitals supporting the Conversation Project34 with hospital-wide initiative to help patients become “conversation ready” to share their care wishes with their loved ones.
BIDMC has been providing patients, 18 years and older, with access to PatientSite, since 2000. Communication over PatientSite enables patients to exchange messages with their clinicians, schedule appointments, request managed care referrals, refill prescriptions, view laboratory results, and view clinicians’ notes.35,36 In addition, PatientSite has provisions to conduct patient interviews.20 As of February 2015, PatientSite had approximately 85 000 active users, with an average of 3067 patients using it each day. The mean age of PatientSite users is 48.1 years and 62% of the users are women.
Health care proxy documentation process prior to availability of the health care proxy interview
Prior to the availability of the HCP interview, patients at BIDMC provided their HCP information either in person or by mail. During an ambulatory clinic visit, a non-interrupting notification would display to the medical assistant and clinician if the patient was older than 65 years and did not have HCP information in his or her EHR. The medical assistant would typically ask the patient for the information, or provide the patient with an instructional handout along with the form. Completed forms would be witnessed and then filed, and the information would be keyed into the structured field in the electronic record either by the clinician or an administrative staff member. The challenges with the existing process were that HCP packets were inconsistently given to patients, and when given, only a small number of patients would complete and return a signed and witnessed copy of their HCP form.
Development of health care proxy interview
We developed the HCP interview based on our prior experience with computer-based medical histories with advisors from BIDMC’s clinical, information systems, legal, and Conversation Ready teams as well as from patients.16–18,20,36–40 We used our Converse programming language to write, edit, and administer the interview.41 We followed the principle that the interview should present text, offer choices, accept responses, and reply appropriately with succinctness, cogency, and good manners.41 The program follows a branching algorithm dependent on the user’s response to each question, asking details where needed. It also educates the user when the user does not know or understand the question being asked, and allows the team to refine questions that users find unclear. The interview, conducted over PatientSite, is integrated with the patient’s EHR and extracts and utilizes data from the record where appropriate, such as to show patients any information existing previously in the EHR related to their HCP.
Components of the health care proxy interview
The HCP interview consists of four sections:
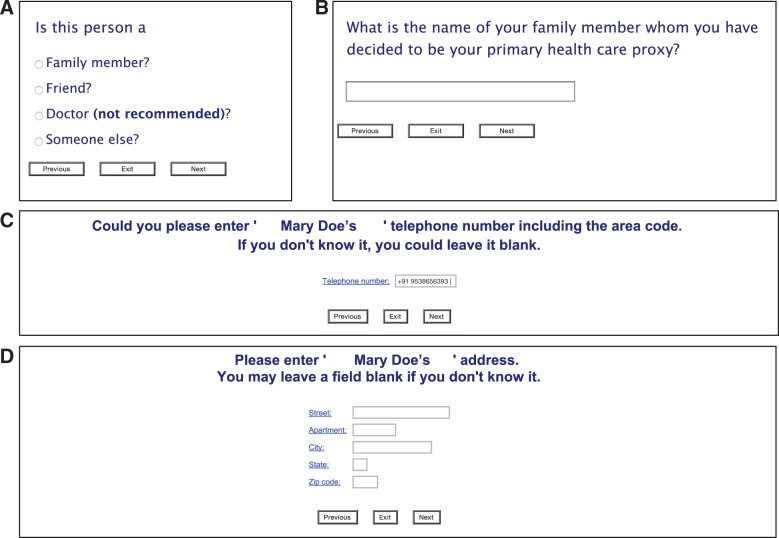
Education: This section informs patients of the importance of a HCP and describes the process of appointing one. (Figure 1) It also provides a link to a section of detailed educational material, should patients choose to view this. In addition, short educational sequences are presented during the interview based on the user’s responses, such as to inform the patient why it is important to have a signed copy of the proxy form.
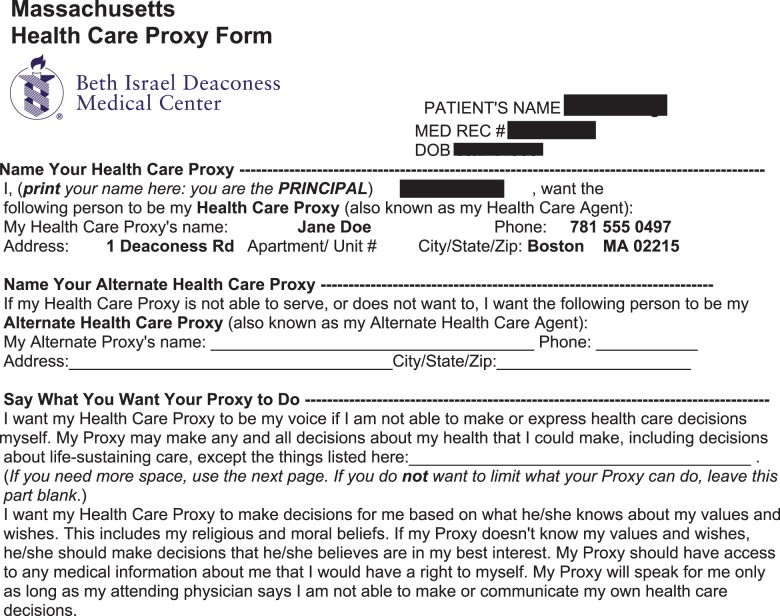
Obtaining the necessary information: The interview asks each patient to record the information necessary for completion of the proxy form, including the proxy’s name, relationship with the patient, telephone number, and contact information (Figure 2). It also enables the patient to designate an alternate HCP if so desired.
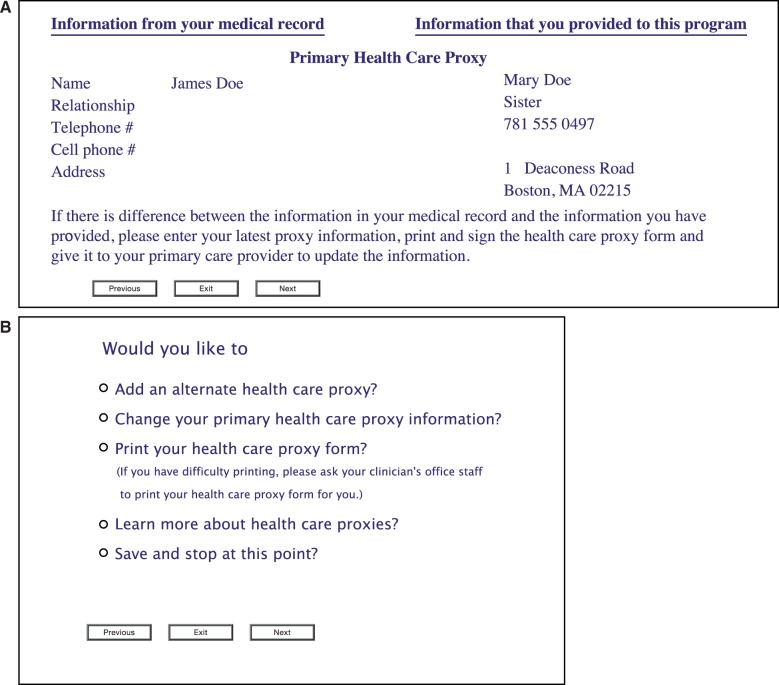
Printing the HCP form: Patients can print an automatically completed HCP form once they provide the necessary information (Figure 3). The proxy form can also be printed by clinicians in the clinic if they choose to do so. Traditional signatures remain required in Massachusetts,42 thus we have not as yet enabled an E-signature for the document.
Submitting the information: The interview enables patients to save their proxy information and return later to provide additional information when needed, thus reserving their HCP information for review until they are satisfied with its readiness to be shared with their clinicians. The interview then enables the patients, if they so wish, to submit their HCP electronically for review by their clinician and subsequent incorporation into their EHR.
Figure 1:
Screenshot from the health care proxy interview, demonstrating the patient education component. All patient data are simulated.
Figure 2:
Screenshots from the health care proxy interview, demonstrating representative fields. (A) Patient’s relation with the HCP. (B) Name of the HCP. (C) Phone number of HCP. (D) Address of HCP.
Figure 3:
At the conclusion of the interview, an auto-populated health care proxy form may be generated for printing.
Integration with the electronic health record
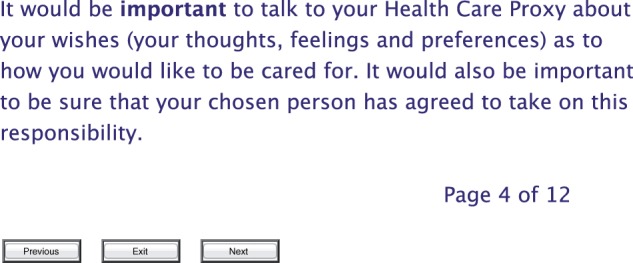
Patients can securely access both the HCP interview and the results of their interview on their computers through their PatientSite portal. With the interview, patients can choose to provide new HCP information, change existing HCP information, print an automatically completed HCP form, view educational information, or stop the interview to be restarted at a later time (Figure 4).
Figure 4:
Screenshots from the health care proxy interview displaying previously captured information from the hospital system. (A) Display of information in the system. (B) Display of patient’s choices.
In considering the impact of this tool on the clinical and administrative workflow, we undertook a user-centered design approach and partnered with staff and members of the hospital’s Health Information Management department. Once a patient has entered the required information, we ask them if they wish to send it to their clinicians. Once completed, a passive alert to the clinician and staff is generated in the patient’s EHR stating the availability of new HCP information through PatientSite (Figure 5). Clinicians can then review this information and use it to update the patient’s EHR. Clinicians can also print a copy of the patient’s HCP form, if not yet signed, so it can then be signed by the patient and the two required witnesses.
Figure 5:
Screenshots from the electronic health record, demonstrating the passive alert of the new health care proxy information from PatientSite, and providing information about reconciliation steps. (A) Passive alert in patient’s EHR. (B) Display of patient entered HCP information with clinician options. (C) Information for clinicians informing the source of new HCP information and steps for reconciliation.
Study Design and Participants
The HCP interview was made available to all PatientSite users. We informed clinicians of this new application through a broadcast email message, but did not make a similar formal announcement to patients. Patients could access the interview through a link on the portal home screen, and patients who accessed the interview were invited to provide comments. Patients were informed at the time of accessing the interview that their data and comments would be analyzed to evaluate and improve upon the interview. For this initial evaluation, we evaluated the usage of the first 200 consecutive patients who completed the interview. The BIDMC Institutional Review Board approved the study.
Data Analysis
We used the Pearson Chi-square statistic with Yates’ continuity correction to compare the difference in the frequency with which HCP information was submitted for review by patients who had at least some HCP information in their EHR and by patients who had no HCP information in their EHR at the time of the interview. We used the Welch two-sample t-test to compare the age distribution of all PatientSite users with the age distribution of the HCP interview users. We used the R software package, version 3.1.2 (http://www.R-project.org/). We evaluated survey data using methods of qualitative analysis described by Crabtree and Miller.43 Two authors inductively coded responses and tracked them with Atlas.ti for Mac (Scientific Software GmbH, Berlin). Initially, investigators (B.C., A.B.) reviewed each of the patients’ comments individually, producing a list of key concepts and assigning codes to them. The investigators then iteratively met to discuss interpretations and compare their codes and then derived themes from the recurrent codes.43,44
RESULTS
Of the first 200 patients to complete the interview, the mean age was 55 years (M = 55.16, SD = 15.16), which was higher than PatientSite users overall (M = 48.1, SD = 15.95), t (199) = 6.47, P ≤ 0.001) (See Supplement figure 1 and 2). Participants were predominantly white (82%); 69.5% of them had a high school degree or higher; their median Charlson Comorbidity Index was 0; and 127(63%) were women.
Ninety-nine (49.5%) of the patients who completed the interview did not have a HCP listed in their EHR and of these, 78 (78.8%) submitted their HCP information for clinician review. One hundred and one out of the 200 patients who completed the interview had at least some information about their HCP in their EHR. Sixty-one of these patients (60.4%) edited their existing HCP information and submitted it for clinician review. Overall, 139 patients submitted their HCP information for their clinician to review and to then update their HCP information in their EHR. Status (presence/absence) of HCP information in a patient’s EHR was significantly associated with submission of HCP information by patients using the HCP interview. Patients who did not have HCP information in their EHR were more likely to submit their HCP information using the HCP interview (Chi square statistic is 7.134 with 1 degree of freedom and P-value of .008).
Patients without HCP information in their EHR were also more likely to submit this information than were those with any existing HCP information in their EHR (odds ratio of 2.4 with 95% CI, 1.3-4.6 and P-value of 0.005). Fifty (36%) of the 139 patients who submitted their proxy information, printed a copy of the prefilled HCP form to be signed by them and their witnesses. Six patients accessed the educational section of the interview.
Analysis of Patient Comment Data
Seventy-four out of 200 patients who completed the HCP interview (37%) entered comments on their experience. Overall, patients were positive about having the HCP interview available to them through PatientSite and to be able to share their HCP information with their clinicians. Upon analysis, the patients’ comments fit into four themes.
First, the interview helped patients become aware of issues surrounding the HCP and to talk about the HCP at home with their families. Patients felt that the interview was easy to use and enlightening; as one user commented “logical, quick and simple process to go through.” They liked being able to stop and return later, which allowed them time to discuss the issues with family members and to come to an agreement before appointing their HCP. As two patients put it: 1) “It is very helpful in making sure patients are informed and prepared in this regard.” 2) “I think that it is one of the excellent choices for me to have the opportunity to assign my Health Care Proxy or Agent to, at least, one of my eight children to make any decision that needs to be made in my behalf after having discussed and harmoniously reached their final judgment.”
Second, seeing a link to the HCP interview reminded patients to take the take time to appoint their HCP, and to submit this information to their clinicians. As three patients noted: 1) “I continually forget to bring this up when I visit my primary care doctor so I am grateful to have this program and get this on file and part of my medical history.” 2) “Useful to have this accessible for patients to complete.” 3) “Very convenient and an easy way to remember to fill the [HCP] form.”
Third, the interview created an opportunity to improve the quality of their HCP information and enabled them to verify their information in their medical record. As one patient stated, “I believe I have a health care proxy on record but am not sure so this gives me a chance to make sure.”
And fourth, the interview on the computer helped patients tackle the sensitive topic of health care proxy. One patient commented, “I think that this is a great way to address a situation that is uncomfortable for many including me. It will now be addressed. I know when we think of illness & death, we don't mention what we should do. This is a great way of handling reality.”
Patients also suggested additional features, such as an easier way to print the HCP form, the ability to make edits directly on the HCP form, a provision to add more than one alternate proxy, the ability to enter foreign addresses, and an option to let their clinicians know of their interest in talking with them further about their advance care wishes. Additionally, patients wondered if electronic submission of HCP information might be able to replace the needs for ink signatures, “Of course, one still needs to have witnesses, etc., to finalize the document -- so that remains an impediment, even with the ease of the computer prompts.”
DISCUSSION
Our study shows that patients are interested in using our online interview to assign their HCP information, and to share it with their clinicians. Two hundred patients completed the interview in <6 weeks from going live, without any formal announcement of its availability. We found that most went on to submit their information for clinician review, and that those without any prior HCP information in their EHR were more likely to proceed and submit their information to the office. This new and corrected information was garnered and added to the EHR by patients alone, and represents a significant way in which patients can help health systems with information entry. Furthermore, our patients’ rate of sharing has been higher than has been reported in studies of computer-based interventions to improve ADs,7,8,10 potentially because our interview addressed an unmet need for an application that is user friendly, educational, and allowing for sharing of HCP information with the EHR. Furthermore, our findings also show that patients are interested in their clinicians having up-to-date information about their HCP and thus, their care wishes.
Interestingly, of the 200 patients who completed the interview, ∼30% of them did not go on and affirmatively submit information for clinician review. One reason may be that these patients did not as yet have all the necessary information. Patients may have also decided to wait to talk with their proxies and their family members before submitting the information for review and incorporation into their medical record. Furthermore, patients who already had HCP information in their electronic record may have considered this to be sufficiently correct or considered their changes to be too minor to be submitted.
The interview users were similar in gender but older than the general population of PatientSite users. The interview users were also predominantly white, healthy, and well educated as well as being more often women, similar to the PatientSite population.45 It seems reasonable that older patients would be more likely to think of end of life, and that well educated patients would be more likely to be sufficiently informed to address issues of the HCP. These findings are in line with a previous study that showed older age, female gender, and white race to be associated with higher rates of AD completion.4 To reach beyond the relatively healthy population, it would be helpful to have special alerts and reminders made available to elders and patients with multiple comorbidity.
Patients found the interview to be a useful tool when available online. It helped them to be better informed about HCPs and gave them a convenient means to establish or to update their proxy and to discuss issues of the proxy with their family members in the privacy of their homes. Interview users’ comments also indicate how the interview primed these patients to have advanced care discussions with their physicians. Discussion about HCP and advance care planning often takes place in a busy clinic visit or not until a patient has been admitted to the hospital. One could argue that these are not the best settings to discuss matters that require time, deep thinking, and careful discussion with loved ones. The online interview addresses these needs. It is worthy to note that some patients felt assignment of a HCP was important, but found the “ink” signatures on the prepopulated print out from the program to be a barrier to completely closing the loop. They perceived a need for a way to provide their signatures online. This has important legal and policy implications as we strive towards greater patient awareness, engagement, and communication of their ADs.
Our educational section to inform patients of the importance of the HCP and the process of appointing a proxy was accessed by six patients. Patients were offered relevant educational phrases en route through the interview, which we hope sufficed for their purposes. It is likely that some of the participants were already well informed about the HCP and its importance, but had delayed creating one until the availability of our program. While evaluation of this requires further use of our program, we believe that the section will continue to serve a useful purpose.
We developed this interview taking legal aspects as well as clinical workflow into consideration and received endorsements from both our legal and clinical stakeholders. The current process for HCP form submission has a low return rate; and with our interview, the ability to print the HCP form both at the patient’s home and after submission by the patient, at the clinician’s office, increases the likelihood of having an official, signed form available for the patient in case of need.
Table 1:
Patient characteristics
| Patient characteristics | N (%) |
|---|---|
| Number of Users | 200 |
| Sex | Female (F ) = 126 (63%), Male (M ) = 74 |
| Age, years | Median 57 (IQR = 45–68) |
| <20 | 1 (5) |
| 20–29 | 12 (6) |
| 30–30 | 26 (13) |
| 40–49 | 28 (14) |
| 50–59 | 49 (24.5) |
| 60–69 | 43 (22) |
| 70+ | 40 (20) |
| Race | |
| White | 164 (82) |
| Black/African American | 12 (6) |
| Hispanic/Latino | 4 (2) |
| Asian | 5 (2.5) |
| Other | 0 |
| Unknown | 15 (7.5) |
| Highest Education | |
| N/A | 5 (2.5) |
| Eighth Grade or less | 0 |
| Some High School | 1 (0.5) |
| Graduated from High School/General Education Development (GED) | 19 (9.5) |
| Some College/Vocational/Tech program | 23 (11.5) |
| Graduated from College, graduate, post graduate school | 97 (48.5) |
| Other | 14 (7) |
| Patient Declined to answer | 20 (10) |
| Patient unavailable to answer | 21 (10.5) |
| Charlson Comorbidity Index | Median = 0 (IQR = 0–2) |
Table 2.
| Health Care Proxy (HCP) information Submitted | HCP information Not submitted | Marginal Column Totals | |
|---|---|---|---|
| HCP in Online Medical Record (OMR) | 61 | 40 | 101 |
| No HCP in OMR | 78 | 21 | 99 |
| Marginal Row Totals | 139 | 61 | 200 |
Our study should be interpreted given its context, conducted as it was in a single health care setting with a homebuilt EHR and patient portal. On the other hand, with health care organizations across the United States working towards achieving meaningful use objectives, patient portals are becoming increasingly available, and commercial EHR vendors are becoming more open to integrating third party applications through Application Programming Interfaces. Given these national trends, we believe that our interview would be useful in multiple settings. We had a small sample size and short study period, and our study sample consisted of self-selected patients. Still, a substantial number of these patients had no HCP to start with and were able to establish one by our interview and that enabled their clinician to incorporate their new HCP into their electronic record. Moreover, our program continues to be used, with approximately 28 patients taking our interview each week as it remains available to patients of BIDMC who have an active portal account. As with other technology-mediated patient processes, the interview will not replace personal communication with clinicians, but may extend clinicians’ reach to patients who are interested and able to complete the process online.
We are currently conducting a prospective study to evaluate the impact of our interview on the rates of HCP documentation in patients’ EHRs. We also plan to further explore the reasons why some patients decide not to submit their HCP information for incorporation into their electronic records, why so few patients availed themselves of the educational section and prevalence of prior physician-patient advanced care discussion among the interview users. This should help us improve our interview. In the future, we also hope to ask patients additional questions to better capture their care preferences.
CONCLUSION
Though substantial work has been done to educate and help patients in advance care planning, gaps remain in closing the communication loop. Our study shows that our HCP interview can be an effective means to help patients to assign and communicate their HCP information. We believe our approach can help to enhance communication between patients and clinicians and be an important assistant to patients as they plan for the future.
FUNDING
This work was funded by National Library of Medicine grant T15LM007092 and Agency for Healthcare Research and Quality grant R01HS021495.
COMPETING INTERESTS
W.S. is on the medical advisory board of Qur, a health IT startup developing a self-driving diagnostic program. C.S. serves as a consultant for Cerner and Allscripts, a member of the physician advisory board of Elsevier, a council member of Health on the Net foundation, and a shareholder and director at Intelligent Medical Objects.
CONTRIBUTORS
A.B., B.C., H.K., C.S., and W.S. designed and developed the interview. A.B., B.C., and H.K. conducted the analysis. All authors contributed to drafting or editing the manuscript.
ACKNOWLEDGEMENTS
The authors would like to thank the Larry Markson, MD, Julie Rockwell and the BIDMC Information Systems team, Lauge Sokol-Hessner, MD, Jennifer Greene, and the Conversation Ready team at BIDMC, David Sontag, JD, Roger Davis, ScD, Margaret Jeddry, Melek Somai, MD, and Christina Cain for their help during this study.
REFERENCES
- 1.Klugman CM, Usatine RP. An Evaluation of 2 Online Advance Directive Programs. Am J Hosp Palliat Med. 2013;30(7):657–663. [DOI] [PubMed] [Google Scholar]
- 2.Silveira MJ, Kim SYH, Langa KM. Advance directives and outcomes of surrogate decision making before death. N Engl J Med. 2010;362(13):1211–1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Silveira MJ, Wiitala W, Piette J. Advance directive completion by elderly Americans: a decade of change. J Am Geriatr Soc. 2014;62(4):706–710. [DOI] [PubMed] [Google Scholar]
- 4.Teno JM, Gruneir A, Schwartz Z, Nanda A, Wetle T. Association between advance directives and quality of end-of-life care: a national study. J Am Geriatr Soc. 2007;55(2):189–194. [DOI] [PubMed] [Google Scholar]
- 5.Ramsaroop SD, Reid MC, Adelman RD. Completing an advance directive in the primary care setting: what do we need for success? J Am Geriatr Soc. 2007;55(2):277–283. [DOI] [PubMed] [Google Scholar]
- 6.H.R.5835 - 101st Congress (1989-1990): Omnibus Budget Reconciliation Act of 1990 | Congress.gov | Library of Congress [Internet]. https://www.congress.gov/bill/101st-congress/house-bill/5835. Accessed February 20, 2015.
- 7.Heiman H, Bates DW, Fairchild D, Shaykevich S, Lehmann LS. Improving completion of advance directives in the primary care setting: a randomized controlled trial. Am J Med. 2004;117(5):318–324. [DOI] [PubMed] [Google Scholar]
- 8.Tung EE, Vickers KS, Lackore K, Cabanela R, Hathaway J, Chaudhry R. Clinical decision support technology to increase advance care planning in the primary care setting. Am J Hosp Palliat Care. 2011;28(4):230–235. [DOI] [PubMed] [Google Scholar]
- 9.Keary S, Moorman SM. Patient-physician end-of-life discussions in the routine care of medicare beneficiaries. J Aging Health. 2015;27(6):983–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dexter PR, Wolinsky FD, Gramelspacher GP, et al. Effectiveness of computer-generated reminders for increasing discussions about advance directives and completion of advance directive forms a randomized, controlled trial. Ann Intern Med. 1998;128(2):102–110. [DOI] [PubMed] [Google Scholar]
- 11.Schubart JR, Levi BH, Camacho F, Whitehead M, Farace E, Green MJ. Reliability of an interactive computer program for advance care planning. J Palliat Med. 2012;15(6):637–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Your Decisions Matter - NHDD is April 16 - Advance Directive Public Resources [Internet]. http://www.nhdd.org/public-resources/. Accessed February 26, 2015.
- 13.Online Advance Medical Directives, Better than a Living Will | MyDirectives [Internet]. https://mydirectives.com/. Accessed February 26, 2015.
- 14.Durbin CR, Fish AF, Bachman JA, Smith KV. Systematic review of educational interventions for improving advance directive completion. J Nurs Scholarsh Off Publ Sigma Theta Tau Int Honor Soc Nurs Sigma Theta Tau. 2010;42(3):234–241. [DOI] [PubMed] [Google Scholar]
- 15.Green MJ, Levi BH. The era of “e”: The use of new technologies in advance care planning. Nurs Outlook. 2012;60(6):376–383.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Slack WV, Hicks GP, Reed CE, Van Cura LJ. A computer-based medical-history system. N Engl J Med. 1966;274(4):194–198. [DOI] [PubMed] [Google Scholar]
- 17.Slack WV, Van Cura LJ. Patient reaction to computer-based medical interviewing. Comput Biomed Res Int J. 1968;1(5):527–531. [DOI] [PubMed] [Google Scholar]
- 18.Slack WV, Slack CW. Patient-computer dialogue. N Engl J Med. 1972;286(24):1304–1309. [DOI] [PubMed] [Google Scholar]
- 19.Slack WV, Safran C, Kowaloff HB, Pearce J, Delbanco TL. Be well!: a computer-based health care interview for hospital personnel. Proc Annu Symp Comput Appl Sic Med Care Symp Comput Appl Med Care. 1993;12–16. [PMC free article] [PubMed] [Google Scholar]
- 20.Slack WV, Kowaloff HB, Davis RB, et al. Evaluation of computer-based medical histories taken by patients at home. JAMIA. 2012;19(4):545–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bachman J. Improving care with an automated patient history. Fam Pract Manag. 2007;14(7):39–43. [PubMed] [Google Scholar]
- 22.Greist JH, Gustafson DH, Stauss FF, Rowse GL, Laughren TP, Chiles JA. A computer interview for suicide-risk prediction. Am J Psychiatry. 1973;130(12):1327–1332. [DOI] [PubMed] [Google Scholar]
- 23.Lucas RW, Card WI, Knill-Jones RP, Watkinson G, Crean GP. Computer interrogation of patients. Br Med J. 1976;2(6036):623–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280(5365):867–873. [DOI] [PubMed] [Google Scholar]
- 25.Kurth AE, Martin DP, Golden MR, et al. A comparison between audio computer-assisted self-interviews and clinician interviews for obtaining the sexual history. Sex Transm Dis. 2004;31(12):719–726. [DOI] [PubMed] [Google Scholar]
- 26.Locke SE, Kowaloff HB, Hoff RG, et al. Computer-based interview for screening blood donors for risk of HIV transmission. JAMA. 1992;268(10):1301–1305. [PubMed] [Google Scholar]
- 27.Otte-Trojel T, de Bont A, Rundall TG, van de Klundert J. How outcomes are achieved through patient portals: a realist review. JAMIA. 2014;21(4):751–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tenforde M, Nowacki A, Jain A, Hickner J. The association between personal health record use and diabetes quality measures. J Gen Intern Med. 2012;27(4):420–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krist AH, Woolf SH. A vision for patient-centered health information systems. JAMA. 2011;305(3):300–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kerns JW, Krist AH, Longo DR, Kuzel AJ, Woolf SH. How patients want to engage with their personal health record: a qualitative study. BMJ Open. 2013;3(7):e002931–e002931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bleich HL, Beckley RF, Horowitz GL, et al. Clinical computing in a teaching hospital. N Engl J Med. 1985;312(12):756–764. [DOI] [PubMed] [Google Scholar]
- 32.Safran C, Sands DZ, Rind DM. Online medical records: a decade of experience. Methods Inf Med. 1999;38(4-5):308–312. [PubMed] [Google Scholar]
- 33.PatientSite: Patient-Centered Communication, Services, and Access to Information. Consumer informatics: Applications and Strategies in Cyber Health Care New York. Springer-Verlag; 2004;20–32. http://link.springer.com/chapter/10.1007%2F978-1-4757-3920-6_2#. [Google Scholar]
- 34.The Conversation Project - Have You Had The Conversation? [Internet]. http://theconversationproject.org/. Accessed February 27, 2015.
- 35.Halamka JD, Mandl KD, Tang PC. Early experiences with personal health records. JAMIA. 2008;15(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Slack WV, Kowaloff HB, Davis RB, Delbanco T, Locke SE, Bleich HL. Test-retest reliability in a computer-based medical history. JAMIA. 2011;18(1):73–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Slack WV. A history of computerized medical interviews. MD Comput Comput Med Pract. 1984;1(5):52–59, 68. [PubMed] [Google Scholar]
- 38.Slack WV. A 67-year-old man who e-mails his physician. JAMA. 2004;292(18):2255–2261. [DOI] [PubMed] [Google Scholar]
- 39.Slack WV. Patient-computer dialogue: a hope for the future. Mayo Clin Proc Mayo Clin. 2010;85(8):701–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Slack WV. Cybermedicine as a patient’s assistant. Cybermedicine: how computing empowers doctors and patients for better health care. Rev edn. San Francisco (Calif): Jossey-Bass Publishers; 2001: 38–43. [Google Scholar]
- 41.Bloom SM, White RJ, Beckley RF, Slack WV. Converse: a means to write, edit, administer, and summarize computer-based dialogue. Comput Biomed Res Int J. 1978;11(2):167–175. [DOI] [PubMed] [Google Scholar]
- 42.General Laws: CHAPTER 201D, Section 2 [Internet]. https://malegislature.gov/Laws/GeneralLaws/PartII/TitleII/Chapter201D/Section2. Accessed February 20, 2015.
- 43.Doing Qualitative Research - Google Books [Internet]. http://books.google.com/books?hl=en&lr=&id=4ebxYPyY5noC&oi=fnd&pg=PR9&dq=doing+qualitative+research+crabtree+and+miller+1999&ots=7z280cXsQE&sig=Hq1vXKz8zhB6RoJXAdhTDzF9YIA#v=onepage&q=doing%20qualitative%20research%20crabtree%20and%20miller%201999&f=false. Accessed February 26, 2015.
- 44.Miller WL CB. Doing Qualitative Research. 2nd ed. Thousand Oaks, CA: Sage Publication; 1999.
- 45.Weingart SN, Rind D, Tofias Z, Sands DZ. Who uses the patient internet portal? The PatientSite experience. JAMIA. 2006;13(1):91–95. [DOI] [PMC free article] [PubMed] [Google Scholar]