Abstract
Purpose
While obesity disparities between racial and socioeconomic groups have been well characterized, those based on gender and geography have not been as thoroughly documented. This study describes obesity prevalence by state, gender, and race/ethnicity to (1) characterize obesity gender inequality, (2) determine if the geographic distribution of inequality is spatially clustered and (3) contrast the spatial clustering patterns of obesity gender inequality with overall obesity prevalence.
Methods
Data from the Centers for Disease Control and Prevention’s 2013 Behavioral Risk Factor Surveillance System (BRFSS) were used to calculate state-specific obesity prevalence and gender inequality measures. Global and Local Moran’s Indices were calculated to determine spatial autocorrelation.
Results
Age-adjusted, state-specific obesity prevalence difference and ratio measures show spatial autocorrelation (z-score=4.89, p-value <0.001). Local Moran’s Indices indicate the spatial distributions of obesity prevalence and obesity gender inequalities are not the same. High and low values of obesity prevalence and gender inequalities cluster in different areas of the U.S.
Conclusion
Clustering of gender inequality suggests that spatial processes operating at the state level, such as occupational or physical activity policies or social norms, are involved in the etiology of the inequality and necessitate further attention to the determinates of obesity gender inequality.
MeSH Keywords: Behavioral Risk Factor Surveillance, Continental Population Groups, Environment, Ethnic Groups, Female, Male, Obesity, Social Environment, Spatial Analysis, United States
INTRODUCTION
Obesity is a preventable cause of premature death among US adults (1) that does not impact social groups equally. While obesity prevalence growth among US adults has slowed or leveled off in recent years (2), monitoring of obesity prevalence among different social groups will continue to be important in designing, targeting and evaluating potential intervention strategies that address obesity disparities (3).
While obesity differences among racial/ethnic groups, socio-economic divides, and geographic regions have been thoroughly documented (4–7), gender inequalities have not been adequately characterized. In the work that has been done, there is little difference in obesity prevalence between men and women overall; however, once stratified by race, non-Hispanic Black women have a 19.5-percentage point higher obesity prevalence than non-Hispanic Black males (8). This finding has persisted across samples, as multiple studies have shown large obesity gender inequality in non-Hispanic Blacks but not in non-Hispanic Whites (9–12).
It is unclear what mechanisms cause gender inequalities in obesity, though differential responses to environmental or neighborhood contexts have been proposed (13). Recently, deprived residential environments have been found to contribute to the gender inequality (14). Little work has been done to further explore the distribution of gender inequality using spatial units larger than neighborhoods, though geographic inequalities in overall obesity prevalence have been well documented at larger geographies (4, 15). Together this evidence indicates that spatially influenced processes (e.g. policies, societal norms, etc.) may be operating at several geographic levels to influence obesity prevalence, and, potentially gender inequality. Spatially describing gender obesity inequalities at the state level is appropriate because health and economic policies implemented at this geography are potentially influential.
This study uses obesity prevalence by state, gender, and race/ethnicity in order to 1) characterize obesity gender inequality, 2) determine whether the geographic distribution of inequality is spatially clustered throughout the contiguous US, and 3) contrast spatial clustering of gender obesity inequality versus spatial clustering of overall obesity prevalence.
MATERIALS & METHODS
Data Source
We used data from the 2013 Behavioral Risk Factor Surveillance System (BRFSS), a Centers for Disease Control and Prevention (CDC) annual telephone survey that provides state-level prevalence estimates for the leading causes of premature mortality and morbidity among non-institutionalized adults ages 18 and older (n=491,773). Data for this analysis were collected in 2013 and excluded US territories, the District of Columbia, Alaska and Hawaii.
Statistical Weights and Adjustment
BRFSS data are weighted to account for 1) the probability that a respondent would be selected to participate and 2) demographic factors assigned using iterative proportional fitting (16). Obesity prevalence measures for each state were age-standardized using direct standardization, according to the US Census 2000 projected population. Prevalence and difference measures for the four non-White race/ethnicity groups (NH Black, Hispanic, NH Multiracial, NH Other, with other including: Asian, Native American, Alaskan Native and Pacific Islander) were estimated using pooled data from 2011 to 2013.
Obesity Prevalence and Gender Inequality Measures
The outcome of interest was obesity gender inequality and the covariates were age, state of residence, and race/ethnicity. Obesity was defined as body mass index (BMI) of 30.0 kg/m2 or higher, calculated as self-reported weight (kilograms) divided by height (meters squared). In 2013, 25,475 participants (5.4%) were missing BMI data and were excluded from analyses. Overall obesity prevalence, and prevalence stratified by interviewer-identified gender and self-reported race/ethnicity, were calculated for the 48 contiguous US states. To provide both an absolute and relative comparison of obesity prevalence, differences and ratios were calculated with males as the referent group. Prevalence, inequality measures, and standard errors were calculated using SAS software, version 9.4. Variance estimates accounted for the complex BRFSS survey design and weights by using Taylor Series Linearization through SAS PROC SURVEYREG software.
Exploratory Spatial Analysis and Maps
Global Moran’s Indices (GMI), a tool of spatial exploratory data analysis, were calculated to determine spatial autocorrelation of prevalence and inequality values among the entire sample (i.e., all race/ethnicities combined) and also once stratified by race/ethnicity. The GMI describes, in a single measure, the overall spatial pattern of an attribute over a defined geography, in this case prevalence differences and ratios across the contiguous United States (US) (17). The GMI statistic provides a test of the null hypothesis that there is complete randomness in the spatial distribution of the study attribute (i.e. that the attribute value at one location does not depend on the values of neighboring locations). GMI were converted to normalized z-scores with associated p-values ≤0.05 considered statistically significant (Supplemental Table 1). Statistically significant positive z-scores suggest positive spatial autocorrelation (i.e. clustering) and negative z-scores suggest negative spatial autocorrelation (i.e. dispersion). Non-significant values are consistent with the null hypothesis of random spatial patterning. The neighbor definition used to create the row-standardized spatial weights matrix was first-order queen contiguity (neighboring states are all those states sharing an immediate border or corner). Sensitivity analysis using both the rook neighbor definition (immediate neighboring states sharing a border but not a corner) and the eight-nearest-neighbors definition (the eight closest neighboring states, measured by distance between centroids) did not substantially alter GMI values (results not shown).
In the presence of statistically significant global spatial autocorrelation, Local Moran’s Indices (LMI) decompose the GMI into the contributions made by each individual state. Thus, LMI statistics allow us to locate and characterize specific spatial clusters of states with similar obesity prevalence and gender inequality values (18). Locations of spatial clustering are indicated as high-high (high value state surrounded by high valued states) and low-low (low value state surrounded by low valued states), while spatial outliers are indicated by high-low (high value state surrounded by low value states) and low-high (Figure 1). Pseudo p-values for LMI were calculated (alpha ≤ 0.01 to account for multiple comparisons) using permutation inference (999 permutations). States with (nmen + nwomen) < 200 after pooling were excluded from spatial analyses. Sensitivity analysis indicated that inclusion of these states did not substantively alter GMI values (results not shown). Spatial analyses were performed using GeoDa version 1.6.6 and maps were produced using QGIS version 2.4.0.
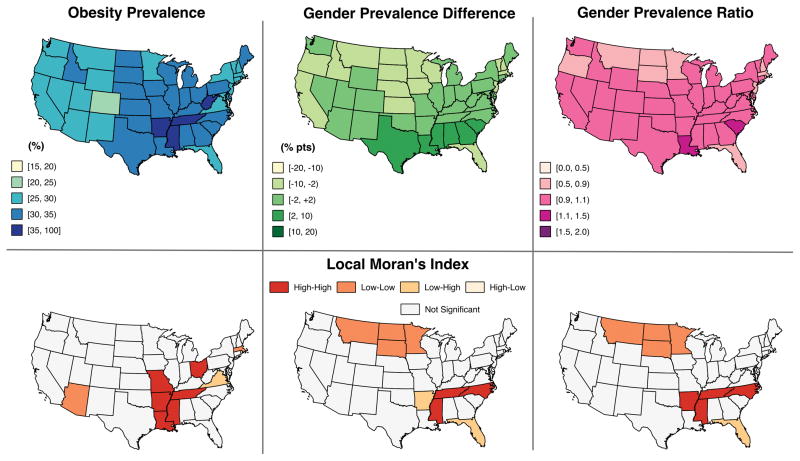
Figure 1. Age-adjusted US obesity prevalence, obesity gender difference and ratio, & corresponding local moran’s indices.
Data source: 2013 Behavioral Risk Factor Surveillance System. Data were age-standardized to US 2000 projected population. Obesity prevalence, gender prevalence difference and gender prevalence ratio show global spatial autocorrelation (z-score = 5.10, 4.89, 4.72 respectively (p-values < 0.001)). Bottom row represents Local Moran’s Indices (LMI) (p-value ≤ 0.01) with ‘high-high’ indicating states with high values near other states with high values, ‘low-low’ indicating states with low values near other states with low values, ‘low-high’ and ‘high-low’ indicating spatial outliers, with all other states having non-significant LMI. The cluster of states with higher female obesity prevalence (high-high) includes Mississippi, Tennessee, and N. Carolina. The cluster of states with higher male obesity prevalence (low-low) includes Montana, North Dakota, South Dakota, and Minnesota. Florida and Arkansas are spatial outliers.
RESULTS
Overall Obesity Prevalence
Nationally, measures of age-adjusted obesity prevalence did not vary by gender (28.2% vs. 28.3%) (Table 1). Global spatial autocorrelation statistics indicated spatial clustering for state-specific overall obesity prevalence with both genders combined (z-score=5.10, p-value <0.001) and among females (z-score=5.82, p-value <0.001) and males (z-score=3.60, p-value <0.001). In race/ethnicity-stratified analyses of obesity prevalence with both genders combined, state-specific obesity prevalences were spatially clustered for all groups except among the non-Hispanic, Multi-Racial group (data not shown). Column one of Figure 1 shows state-specific obesity prevalence and results from LMI analyses of cluster locations: states with high obesity prevalence cluster in the South and Midwest.
Table 1.
Prevalence of US adult obesity by selected demographic characteristics, 2013
Data source: 2013 Behavioral Risk Factor Surveillance System. Statistical weights and age-standardized (to US 2000 projected population) were applied for prevalence calculations. Other races include: Asian, Native American, Alaskan Native and Pacific Islander.
| n | (%) | Obesity Prevalence (%) | (95% CI) | |
|---|---|---|---|---|
|
|
||||
| N | 478,934 | (100) | 28.3 | (28.0, 28.6) |
| Missing Outcome | 26,152 | |||
| Sex | ||||
| Female | 282,598 | (59.0) | 28.2 | (27.9, 28.7) |
| Male | 196,336 | (41.0) | 28.3 | (27.9, 28.7) |
| Race/Ethnicity | ||||
| White, Non-Hispanic | 374,018 | (78.1) | 27.1 | (26.8, 27.3) |
| Black, Non-Hispanic | 36,951 | (7.7) | 37.8 | (36.8, 38.7) |
| Hispanic | 30,808 | (6.4) | 31.2 | (30.3, 32.1) |
| Other, Non-Hispanic | 20,004 | (4.2) | 15.5 | (14.5, 16.6) |
| Multi-racial, Non-Hispanic | 8,781 | (1.8) | 31.7 | (29.2, 34.1) |
| Census Region | ||||
| Midwest | 132,002 | (27.6) | 30.0 | (29.5, 30.5) |
| Northeast | 84,058 | (17.6) | 26.3 | (25.7, 26.9) |
| South | 154,945 | (32.4) | 30.3 | (29.8, 30.8) |
| West | 197,929 | (22.5) | 24.9 | (24.2, 25.6) |
|
|
||||
Gender Inequality - Geographic Variation
State-specific prevalence ratios (Figure 1, column 3) hover closely around the null value of one, whereas prevalence differences (Figure 1, column 2) vacillate up to 7 percentage points in either direction of the null (i.e. −7 to +7). Gender prevalence differences were spatially autocorrelated (z-score=4.89, p-value <0.001) but did not show the same clustering patterns as overall obesity prevalence. LMI statistics indicated a cluster of states (Mississippi, Tennessee, North Carolina) in the Southeastern US which have higher obesity prevalence among females (Figure 1, column 2, row 2: ‘high-high’ indicates high difference values among states with similarly high difference values); and a cluster (Montana, North Dakota, South Dakota, Minnesota) where males have higher prevalence in the North Central (Figure 1, column 2, row 2: ‘low-low’ indicates low difference values among states with similarly low difference values). Additionally, when states are ordered from lowest to highest obesity prevalence, the obesity gender difference does not similarly increase, nor does it decrease, but rather shows a seemingly random pattern (data not shown).
Gender Inequality - Racial-Ethnic Variation
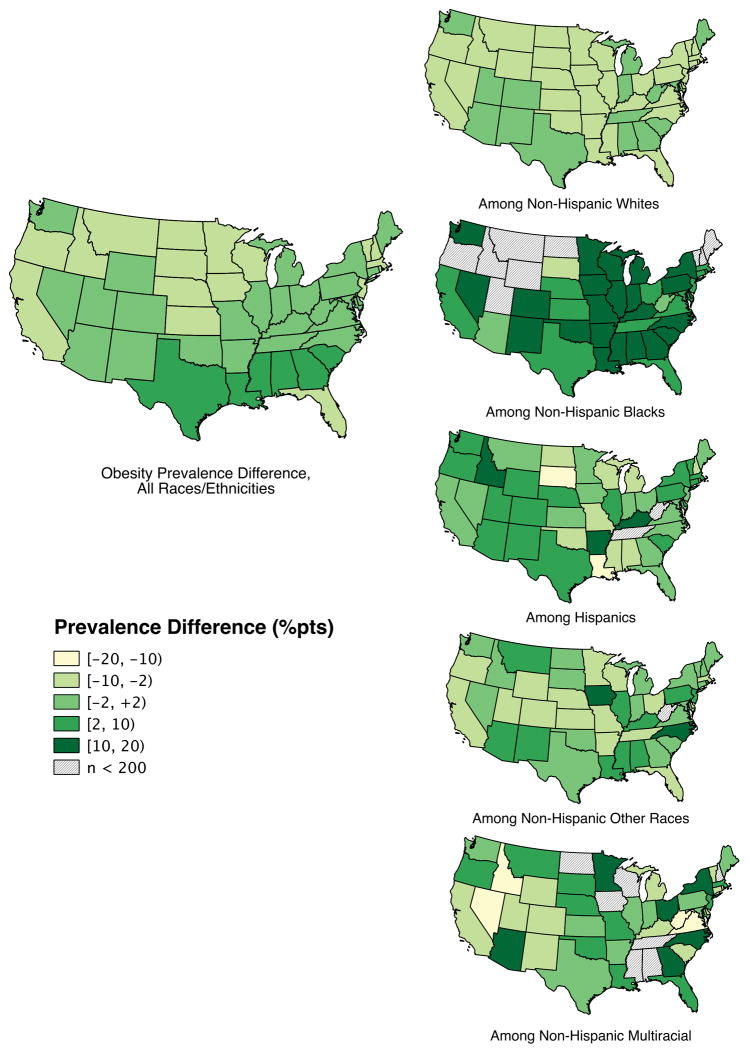
When stratified by race-ethnicity, the gender prevalence difference was positively spatially autocorrelated among non-Hispanic Whites only (z-score=3.25, p-value <0.001) (Figure 2). Additionally, state-specific prevalence difference values tend to group around the null for all race/ethnicities except among the Non-Hispanic Black group, which has a median prevalence difference above 10 percentage points.
Figure 2. Age-adjusted obesity gender difference, by race/ethnicity.
Data source: 2013 Behavioral Risk Factor Surveillance System, data pooled across 2011–13 for the four non-White racial/ethnic groups. Data were age-standardized to US 2000 projected population. The darkest color represents states with higher female prevalence and the lightest represents states with higher male prevalence. States patterned with diagonal lines were excluded from spatial analysis due to small sample sizes (n <200). Gender difference among all race/ethnicities combined (z-score = 4.89, p-value < 0.001) and among non-Hispanic Whites (z-score = 3.25, p-value < 0.001) show positive global spatial autocorrelation; GMI of prevalence differences among non-NH White races/ethnicities are not significant at the 0.05 level.. Other races include: Asian, Native American, Alaskan Native and Pacific Islander.
DISCUSSION
This study used a national- and state-level representative dataset and applied exploratory spatial techniques, Global and Local Moran’s Indices, to 1) characterize the distribution of obesity gender inequalities among US states, 2) determine whether the geographic distribution of obesity gender inequality is spatially clustered throughout the contiguous US, and 3) contrast spatial clustering of gender obesity inequality versus spatial clustering of overall obesity prevalence. Our results demonstrated the novel findings that gender obesity inequalities are spatially clustered and that the clustering pattern differs from that of overall obesity prevalence.
Gender Inequality Measures
When characterizing obesity gender inequality, we found different patterns than overall obesity prevalence. As in previous work, we found that high overall obesity prevalence clusters in the South and Midwest, whereas the Southwest and Northeast include locations with relatively low obesity prevalence. The patterns for gender inequality were different: LMI statistics indicated that the Southeast is marked by a cluster of states with higher female obesity prevalence, while the North Central is marked by a cluster of states where males have relatively higher obesity prevalence. This evidence indicates that, at the state level, spatial drivers of overall obesity prevalence and gender obesity inequality likely differ.
Spatial Clustering
The geographic distribution of gender obesity inequality is spatially clustered throughout the contiguous US indicating that it may be driven by state or regional level policies or social norms. Clustering patterns seen in this study may be driven by occupational, physical activity, transportation, or nutrition policies with differential impacts among genders. Unfortunately, the determinants of obesity in rural areas - those states showing clustering in this study - are poorly understood (19). Potential determinants include gendered household or work roles, food and beverage taxes, SNAP/WIC options, menu labeling efforts, access to recreational or health-focused amenities, and transportation and commuting patterns. The clustering may also be a reflection of historical patterns of residential segregation by race/ethnicity as the cluster of states with higher female obesity prevalence overlaps with an area of the US that has a high proportion of non-Hispanic Black residents. Therefore, the high prevalence of obesity among non-Hispanic Black women in this area may be the driving force behind this clustering pattern.
Once stratified by race/ethnicity, spatial clustering of the prevalence difference is only present among non-Hispanic Whites (Figure 2: a cluster of states in the Southeast and a cluster of states in the Southwest is driving the autocorrelation). The lack of clustering among non-Whites could result from several factors: limited statistical power, absence of spatial correlates that relate to the inequality among non-Whites, or that spatial drivers may differ by race/ethnicity or operate at other spatial levels (e.g. county or neighborhood). Additional research is needed to clarify spatial patterns of gender inequalities among non-Whites.
Limitations
Our study used self-reported BRFSS data which have been shown to underestimate objectively measured obesity prevalence by up to 9.5 percentage points (20). Further, self-reported weights and heights show differential reporting by gender, race/ethnicity (21), and US region (22). Even after pooling, small sample sizes among non-White race/ethnic groups make it difficult to adequately characterize spatial clusters or outliers. Finally, as with other geographic research, it is unclear what geographic level of analysis is most appropriate for the study of obesity or gender obesity inequality (23).
CONCLUSION
This study used exploratory spatial analyses to determine that the spatial distribution of gender obesity inequalities differ from that of overall obesity prevalence. The presence of spatial clustering of gender obesity inequalities suggests there is spatial structure to this phenomenon. Further investigation of policies implemented at the state level may provide insight into the etiology of this inequality. Understanding and reducing obesity gender inequalities will require explicit research exploring the intersectionality of geography and gender.
Supplementary Material
Data source: 2013 Behavioral Risk Factor Surveillance System, data pooled across 2011–13 for the four non-White racial/ethnic groups. States with (nmen + nwomen)< 200 after pooling were excluded. Data were age-standardized to US 2000 projected population. Spatial weights matrices were row standardized and based on a first-order, queen contiguity definition of neighbors. GMI were standardized to z-scores with p-values ≤ 0.05, indicating statistical significance. A positive z-score (p-value ≤ 0.05) suggests presence of positive global spatial autocorrelation (i.e. clustering). Other races include: Asian, Native American, Alaskan Native and Pacific Islander.
Acknowledgments
Funding: This research received support from the Population Research Training grant (T32 HD007168) and the Population Research Infrastructure Program (R24 HD050924) awarded to the Carolina Population Center at The University of North Carolina at Chapel Hill by the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
LIST OF ABBREVIATIONS & ACRONYMS
- BMI
Body mass index
- BRFSS
Behavioral Risk Factor Surveillance System
- CDC
Centers for Disease Control and Prevention
- GMI
Global Moran’s Index
- LMI
Local Moran’s Index
- US
United States
Footnotes
Disclosure: The authors have no conflicts of interest to disclose.
Author Contributions: DG and WR conceived of the project; DG carried out the analysis and generated the figures. All authors were involved in interpreting the results, writing the paper and had final approval of the submitted version.
References
- 1.Borrell LN, Samuel L. Body mass index categories and mortality risk in US adults: the effect of overweight and obesity on advancing death. American journal of public health. 2014;104(3):512–9. doi: 10.2105/AJPH.2013.301597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA : the journal of the American Medical Association. 2012;307(5):491–7. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 3.Harper S, Lynch J. Measuring Health Inequalities. In: Oakes JMK, Jay S, editors. Methods in Social Epidemiology. San Francisco, CA: John Wiley & Sons, Inc; 2006. pp. 134–68. [Google Scholar]
- 4.Slack T, Myers CA, Martin CK, Heymsfield SB. The geographic concentration of US adult obesity prevalence and associated social, economic, and environmental factors. Obesity (Silver Spring, Md) 2014;22(3):868–74. doi: 10.1002/oby.20502. [DOI] [PubMed] [Google Scholar]
- 5.Boardman JD, Saint Onge JM, Rogers RG, Denney JT. Race differentials in obesity: the impact of place. Journal of health and social behavior. 2005;46(3):229–43. doi: 10.1177/002214650504600302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Michimi A, Wimberly MC. Spatial patterns of obesity and associated risk factors in the conterminous U.S. American journal of preventive medicine. 2010;39(2):e1–e12. doi: 10.1016/j.amepre.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 7.Wells JC, Marphatia AA, Cole TJ, McCoy D. Associations of economic and gender inequality with global obesity prevalence: understanding the female excess. Social science & medicine (1982) 2012;75(3):482–90. doi: 10.1016/j.socscimed.2012.03.029. [DOI] [PubMed] [Google Scholar]
- 8.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of Obesity Among Adults: United States, 2011–2012. NCHS Data Brief; Hyattsville, MD: 2013. [PubMed] [Google Scholar]
- 9.Borders TF, Rohrer JE, Cardarelli KM. Gender-specific disparities in obesity. Journal of community health. 2006;31(1):57–68. doi: 10.1007/s10900-005-8189-8. [DOI] [PubMed] [Google Scholar]
- 10.Read JG, Gorman BK. Gender inequalities in US adult health: the interplay of race and ethnicity. Social science & medicine (1982) 2006;62(5):1045–65. doi: 10.1016/j.socscimed.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 11.Beydoun MA, Wang Y. Gender-ethnic disparity in BMI and waist circumference distribution shifts in US adults. Obesity (Silver Spring, Md) 2009;17(1):169–76. doi: 10.1038/oby.2008.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robinson WR, Gordon-Larsen P, Kaufman JS, Suchindran CM, Stevens J. The female-male disparity in obesity prevalence among black American young adults: contributions of sociodemographic characteristics of the childhood family. The American journal of clinical nutrition. 2009;89(4):1204–12. doi: 10.3945/ajcn.2007.25751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kanter R, Caballero B. Global gender disparities in obesity: a review. Advances in nutrition (Bethesda, Md) 2012;3(4):491–8. doi: 10.3945/an.112.002063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seamans MJ, Robinson WR, Thorpe RJ, Jr, Cole SR, LaVeist TA. Exploring racial differences in the obesity gender gap. Annals of epidemiology. 2015;25(6):420–5. doi: 10.1016/j.annepidem.2015.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Myers CA, Slack T, Martin CK, Broyles ST, Heymsfield SB. Regional disparities in obesity prevalence in the United States: A spatial regime analysis. Obesity (Silver Spring, Md) 2015;23(2):481–7. doi: 10.1002/oby.20963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pierannunzi C, Town M, Garvin M, Shaw FD, Balluz L. Methodologic changes in the Behavioral Risk Factor Surveillance System in 2011 and potential effects on prevalence estimates. MMWR Morbidity and mortality weekly report. 2012;61(22):410–3. [PubMed] [Google Scholar]
- 17.Anselin L. European Science F. The moran scatterplot as an ESDA tool to assess local instability in spatial association. In: Fischer MM, Scholten HJ, Unwin D, editors. Spatial analytical perspectives on GIS. GISDATA London: Bristol, PA: Taylor & Francis; 1996. pp. 111–25. [Google Scholar]
- 18.Anselin L. Local Indicators of Spatial Association—LISA. Geographical Analysis. 1995;27(2):93–115. [Google Scholar]
- 19.Johnson DB, Quinn E, Sitaker M, Ammerman A, Byker C, Dean W, et al. Developing an agenda for research about policies to improve access to healthy foods in rural communities: a concept mapping study. BMC public health. 2014;14:592. doi: 10.1186/1471-2458-14-592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yun S, Zhu BP, Black W, Brownson RC. A comparison of national estimates of obesity prevalence from the behavioral risk factor surveillance system and the national health and nutrition examination survey. Int J Obes Relat Metab Disord. 2005;30(1):164–70. doi: 10.1038/sj.ijo.0803125. [DOI] [PubMed] [Google Scholar]
- 21.Richmond TK, Thurston I, Sonneville K, Milliren CE, Walls CE, Austin SB. Racial/ethnic differences in accuracy of body mass index reporting in a diverse cohort of young adults. International journal of obesity (2005) 2015;39(3):546–8. doi: 10.1038/ijo.2014.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Le A, Judd SE, Allison DB, Oza-Frank R, Affuso O, Safford MM, et al. The geographic distribution of obesity in the US and the potential regional differences in misreporting of obesity. Obesity (Silver Spring, Md) 2014;22(1):300–6. doi: 10.1002/oby.20451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kwan M-P. The uncertain geographic context problem. Annals of the Association of American Geographers. 2012;102(5):958–68. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data source: 2013 Behavioral Risk Factor Surveillance System, data pooled across 2011–13 for the four non-White racial/ethnic groups. States with (nmen + nwomen)< 200 after pooling were excluded. Data were age-standardized to US 2000 projected population. Spatial weights matrices were row standardized and based on a first-order, queen contiguity definition of neighbors. GMI were standardized to z-scores with p-values ≤ 0.05, indicating statistical significance. A positive z-score (p-value ≤ 0.05) suggests presence of positive global spatial autocorrelation (i.e. clustering). Other races include: Asian, Native American, Alaskan Native and Pacific Islander.