Abstract
Background
Patients’ positive illness perceptions (IPs) significantly contribute to treatment success. The Brief Illness Perception Questionnaire (Brief IPQ) is widely used in various diseases for assessing IPs. It was developed in English-speaking countries and studies on it in Arab countries are scarce.
Objectives, Setting and design
This observational cross-sectional study aimed to cross-culturally adapt the Brief IPQ English version into a modern Arabic language version and determine its psychometric properties in a sample of Lebanese cardiac disease patients. This study was approved by the Institutional Review Board of Saint Joseph University of Beirut, Lebanon.
Participants
A convenience sample of 30 patients with cardiac disease were recruited during routine visits to cardiologists’ offices in Beirut, Lebanon. Inclusion criteria were at least one cardiac disease for at least 6 months with no acute episode or exacerbation of the disease during the 6 preceding months, age≥18 years, and the ability to read and comprehend Arabic. The pre-final version of the Brief IPQ Arabic version was tested for face and content validity. The meaning, comprehensibility, and acceptability were studied by individual interviews. For discriminant validity and internal consistency of the Brief IPQ Arabic version (Brief IPQ-Ar), 100 patients were recruited in a similar manner using the same inclusion criteria. To assess reproducibility, 30 patients, selected randomly from the 100 patients, filled the questionnaire a second time, 3–4 weeks after its first administration and under the same conditions.
Main outcome measures
Psychometric properties of the Brief IPQ-Ar among Lebanese patients suffering from cardiac diseases.
Results
Semantic equivalence between the Brief IPQ-Ar questions and patients’ descriptions was 100%. Cronbach's alpha was 0.717, which shows good internal consistency. Reproducibility was satisfactory (ICC values>0.776). Moreover, the Brief IPQ-Ar discriminated participants according to the type of cardiac disease and treatment-related characteristics.
Conclusions
We confirm that the Brief IPQ-Ar is appropriate for exploring IPs in cardiac disease patients whose first language is Arabic. Further research should be conducted to test this Arabic version in other types of diseases.
Keywords: adaptation, Arabic, Brief IPQ, cardiology, cross-cultural, psychometric
Heart diseases are a leading cause of mortality worldwide and a frequent cause of hospital admissions, including in Lebanon (1, 2). The prevalence of coronary artery disease was estimated at 20% in Lebanon (3). Patients’ beliefs about their diseases are one of the factors predicting the decision to seek care (4). Illness perceptions (IPs) are the patients’ thoughts about the symptoms they experience, and are among the psychosocial factors that could explain the variance in physical functioning among patients (5).
IP belongs to the core concepts in the Commonsense Model of Self-Regulation (CSM) developed by Leventhal et al. (6). It addresses how individuals respond emotionally and cognitively (illness representations) to a specific internal or external stimulus, such as a symptom or sign of illness, and how these cognitions and emotions guide coping responses (7). According to the CSM, there are five dimensions of cognitive representations of illness: identity (individual's label for the symptom), consequences (individual's beliefs about the consequences of illness), timeline (individual's beliefs about the duration of illness), control (individual's beliefs about whether the illness can be treated or kept under personal control), and cause (individual's beliefs about the cause of the illness) (6). CSM also postulates that these cognitions have a causal effect on individuals’ coping efforts in the face of a health threat, such as a chronic condition (8). Coping behavior is defined as efforts to manage a stressful situation by changing cognitions or behavior (9). Coping styles used by patients could include problem-focused coping, emotion-focused coping, avoidant coping, and socially supported coping (10). Avoidant coping has been strongly associated with adverse emotional outcomes, such as anxiety, depression, and negative affectivity (11–13). Coping and IPs are associated: negative IPs are linked to increased psychological distress and maladaptive coping (14). Interventions to align CSM with medical knowledge and to provide patients with the adaptive understanding required to manage their own health are increasingly prevalent (15).
Cardiovascular diseases (CVD) are the main cause of death and activity limitations worldwide, and several studies have shown that the manifestation and clinical evolution of CVD are related to psychosocial factors such as anger, hostility, perceived stress, anxiety, and depression (16). The American guidelines for cardiac rehabilitation (17) as well as European (18) and Australian guidelines (19) suggest that rehabilitation programs should therefore be focused on psychosocial issues to improve patients’ well-being and achieve a better quality of life. For patients with congestive heart failure, affect is considered an essential aspect of emotional well-being (20).
An important factor in the adjustment to chronic conditions is the patient's illness perception (21). Negative IPs are reportedly associated with more complications after CVD (22), and various studies have indicated that perceptions of less negative illness consequences are associated with better clinical outcomes (23). Negative IPs in post-myocardial infarction are associated with fatigue; fatigued patients tend to expect longer illness duration, have more negative emotional beliefs, and perceive more serious consequences (7). Illness perception is also an important aspect in the management of hypertension besides pharmacological interventions (24).
In patients with congestive heart failure, changing patients’ IPs has been shown to improve (1) recovery following myocardial infarction (25), (2) hypertension management (24), and (3) emotional distress (anxiety and depression) (26). Given all the reasons above, examining patients’ IPs in chronic diseases and specifically in cardiac diseases is of paramount importance.
The assessment of IPs has evolved from interviews to validated questionnaires (27). One of the questionnaires, developed in 1996, is the Illness Perception Questionnaire (IPQ), which has over 80 items (28). The Brief IPQ, developed and validated in 2006 (29), has been widely used for assessing IPs in various diseases (30, 31) and among adults and adolescents (32). It has the advantages of being brief and easy to understand.
The IPQ and the Brief IPQ were developed in English-speaking countries and have been translated and validated in different cultures. To assess IPs across cultures, it is generally recommended to adapt questionnaires to the target language and culture (29, 33, 34). To the best of our knowledge, no validation of the Brief IPQ has been done in Arab countries so far, where the cultural context is different. One study published an adapted Arabic version of the full-length IPQ, but it concluded that the factor structure did not concur with prior findings on the IPQ (35). Another translated the Brief-IPQ to Arabic and used it, but the authors did not validate their version (36).
The aim of this study was to cross-culturally adapt the nine-item Brief IPQ English version into the Brief IPQ Arabic version (Brief IPQ-Ar) (Modern Standard Arabic) and determine its face validity, content validity, reproducibility, and concurrent validity in a sample of Lebanese patients suffering from cardiac diseases.
Methods
Ethical considerations
The study was approved by the Institutional Review Board of Saint Joseph University of Beirut, Lebanon (ref. Usj-2014-1). All participants provided their written informed consent to participate in this study.
Perception of illness measure: the Brief IPQ
The Brief IPQ is a nine-item questionnaire designed to assess each dimension of illness perception. Five items assess cognitive illness representations: consequences(item 1), timeline (item 2), personal control (item 3), treatment control (item 4), and identity (item 5). Two items assess emotional representations: concern (item 6) and emotions (item 8). Finally, one item assesses illness comprehensibility (item 7). Responses are scored on a scale ranging from 0 to 10. For items 1, 2, 5, 6, and 8, a 0 score indicates a good disease perception, and a score of 10 indicates a bad disease perception. For items 3, 4, and 7, a score of 0 indicates a bad disease perception, and 10 indicates a good disease perception. Assessment of the causal representation is by an open-ended response item, which asks patients to list the three most important causal factors in their illness (item 9) (29).
Transcultural adaptation
The Brief IPQ (29) was cross-culturally adapted using the guidelines of Beaton et al. (33). First, two bilingual translators whose mother tongue is Arabic produced two independent translations from English to Arabic. The two translators and the research leader synthesized the results of the two translations and reached a consensus on a common translation. Then, two translators whose mother tongue is English and blinded to the original English version translated the Arabic version back into English. The first author of the Brief IPQ (29) was contacted for approval of the backward translation. A committee consisting of experts in questionnaire validation, an Arabic linguist, and all the translators reached a consensus on semantic equivalence. This equivalence means that the word of the target language has the same meaning as the corresponding word of the source language and also reflects the same nuance. This means that the corresponding words in the original English version and the Arabic version have the same meaning. This committee contacted the first author of the Brief IPQ (29) for approval of the backward translation.
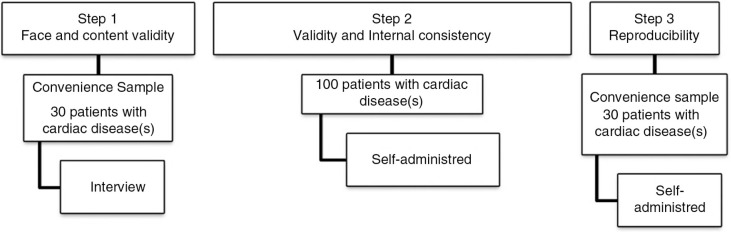
Step 1: face and content validity
Face and content validity of the pre-final version of the Brief IPQ-Ar A were tested on a convenience sample of 30 Lebanese patients (Fig. 1). Patients had at least one cardiac disease for at least 6 months but no acute episode or exacerbation of the disease during the 6 preceding months, were aged ≥ 18 years, and could read and comprehend Arabic. The meaning, comprehensibility, and acceptability were studied in individual interviews with the participants about what they thought was meant by each question.
Fig. 1.
Procedure and stages of the assessment of the validity and reproducibility of the Arabic version of the Brief Illness Perception Questionnaire.
Step 2: discriminant validity and internal consistency
One hundred Lebanese patients were recruited using the same inclusion criteria as in step 1. Discriminant validity and internal consistency of the Brief IPQ-Ar were assessed.
Step 3: reproducibility
To assess reproducibility, 30 patients selected randomly from the 100 participants in step 2 filled the questionnaire a second time in the same conditions 2 weeks after the first administration.
Study population
In this observational cross-sectional study, patients were recruited during their routine visits to cardiologists between 15 January and 15 March 2015 (convenience sampling). Criteria for inclusion were: Lebanese patients diagnosed with at least one cardiac disease for at least 6 months with no acute episode or exacerbation of the disease during the 6 preceding months, aged 18 years or older. Participants had to be able to read and comprehend Arabic language.
All eligible patients were recruited in person and invited to enroll after providing their written consent. Step 1 interviews were conducted by a trained research assistant. For steps 2 and 3, participants completed a self-administered questionnaire consisting of basic socio-demographic profile, clinical information, and the Brief IPQ-Ar (Fig. 1). Questionnaires were completed in the cardiology clinic. The socio-demographic characteristics of the participants included their age, gender, marital status, and level of education.
Clinical information about the participants included the type of cardiac disease according to the WHO classification (37) and treatment-related characteristics, such as the number of drugs taken by the patient, the number of drug intakes per day, the number of drug pills per day, and treatment duration. The presence or absence of concomitant non-cardiac disease(s) was also recorded.
Statistical analysis
Statistical analysis was performed using SPSS for windows version 17.0 (USA). The alpha error was set at 0.05. For a cross-cultural adaptation of the original Brief IPQ into Brief IPQ-Ar, the percentage of agreement on semantic equivalence in patients for face and content validity was calculated. Internal consistency, reproducibility, and discriminant properties were evaluated.
As the scores of the Brief IPQ-Ar and continuous variables (numbers of pills/day, and treatment duration) were not normally distributed (Kolmogorof Smirnov test). The Kruskal-Wallis test, Mann Whitney test, and Spearman correlation coefficient were used.
To assess the degree of internal consistency, scores of items 3, 4, and 7 were reversed and Cronbach's alpha coefficients were calculated; Spearman correlation coefficients were used to measure the item-score correlations. The acceptable level for the overall scale was set at 0.80 for Cronbach's alpha.
Reproducibility is a component of precision in a measurement system. It is the ability of a questionnaire to consistently reproduce the same measurement under the same conditions. It was assessed by repeating the administration of the Brief IPQ-Ar to 30 subjects among the 100 who filled the questionnaire the first time, 2 weeks after the first administration. Intra-class correlation coefficients (ICC) with 95% confidence interval were calculated. ICC values ≥ 0.7 were considered acceptable.
Discriminant validity was evaluated by measuring the degree to which the scores of the different items of the Brief IPQ-Ar and clinical data were related. It was supposed that the Brief IPQ-Ar can discriminate between participants according to their clinical data as represented by the type of cardiac disease, treatment duration, number of pills per day, concomitant diseases, number of drugs taken, number of drug intakes, and number of pills per day. The Kruskal-Wallis test, Mann Whitney test, and Spearman correlation coefficient were used for this purpose.
Considering that it is widely recognized that chronicity and the difficulty of living with severe chronic conditions tax the individual's psychological and emotional resources (11), it was hypothesized that patients having factors adding to their disease management burden would have poorer IPs for some dimensions, such as treatment or timeline dimensions. Contributing factors include concomitant disease(s), a large number of drugs and pills taken daily, a large number of drug intakes per day, and long treatment duration.
The relationships between sociodemographic variables and the different items of the Brief IPQ-Ar were also studied by the Kruskal-Wallis test, Mann Whitney test, and Spearman correlation coefficient.
Results
Step 1: face and content validity (n=30)
Thirty patients (51% male) participated; 64% were <65 years old, 65% were married, and 79% had a secondary or better level of schooling.
Testing of the pre-final version of the Brief IPQ-Ar showed a 100% semantic equivalence between the Brief IPQ-Ar questions and patients’ descriptions. All the patients stated that they understood the questions and gave semantic equivalences.
Step 2: assessment of internal consistency (n=100)
A total of 100 patients (53% male) were included in the study; 62% were <65 years old, 69% were married, and 81% had a secondary or better level of schooling. The major socio-demographic and disease/drug related characteristics of the participants are presented in Table 1.
Table 1.
Socio-demographic and disease/drug related characteristics of the participants (n=100)
| Characteristics | Number (%) |
|---|---|
| Gender | |
| Male | 53 (53.0) |
| Female | 47 (47.0) |
| Age (years) | |
| <55 | 22 (22.0) |
| 55−65 | 30 (30.0) |
| >65 | 47 (47.0) |
| Marital status | |
| Single | 20 (20.0) |
| Married | 69 (69.0) |
| Divorced | 4 (4.0) |
| Widowed | 6 (6.0) |
| Missing data | 1 (1.0) |
| Level of education | |
| Primary | 17 (17.0) |
| Secondary | 45 (45.0) |
| University degree | 36 (36.0) |
| Missing data | 2 (2.0) |
| Type of cardiac disease | |
| Hypertension | 25 (25.0) |
| Heart failure | 10 (10.0) |
| Cardiac arrhythmias | 8 (8.0) |
| Cardiomyopathies | 4 (4.0) |
| Ischemic heart disease or coronary artery disease | 21 (21.0) |
| More than one disease | 32 (32.0) |
| Presence of concomitant non-cardiac diseases | |
| No | 22 (22.0) |
| Yes | 78 (78.0) |
| Number of drugs taken by the patienta | |
| 1 | 50 (50.0) |
| 2 | 38 (38.0) |
| ≥ 3 | 12 (12.0) |
| Number of drug intakes per daya | |
| 1 | 36 (36.0) |
| 2 | 51 (51.0) |
| ≥ 3 | 13 (13.0) |
| Number of drug pills per daya | |
| 1 | 34 (34.0) |
| 2 | 43 (43.0) |
| 3 | 12 (12.0) |
| ≥ 4 | 11 (11.0) |
| Duration of treatment (months)a | 8.5±5.4 |
Only drugs used to treat cardiac diseases are considered in this table.
Twenty-five percent of the participants had hypertension, 10% heart failure, 8% cardiac arrhythmias, 4% cardiomyopathies, and 32% presented more than one cardiac disease at the time of questionnaire completion. The average treatment duration of cardiac disease(s) was 8.5±5.4 years.
Table 2 summarizes the answers of participants to the questions of the Brief IPQ-Ar. Cronbach's alpha was 0.717 and varied from 0.649 to 0.743 when item 1 or 3 was deleted, respectively. Item scale correlations varied from 0.373 (item 3) to 0.727 (item 8) (Table 3). The score of each Brief IPQ-Ar item was significantly correlated with the total Brief IPQ-Ar score (p<0.05) (Table 4).
Table 2.
Percent distribution of the participants’ answers to each item of the Arabic version of the Brief Illness Perception Questionnaire
| Consequences (How much does your illness affect your life?) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No affect at all | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 Severely affects |
| 25% | 10% | 10% | 10% | 4% | 10% | 5% | 15% | 7% | 1% | 3% | |
|
| |||||||||||
| Timeline (How long do you think your illness will continue?) | |||||||||||
|
| |||||||||||
| A very short time | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 Forever |
| 25% | 0% | 1% | 3% | 3% | 6% | 6% | 5% | 8% | 9% | 58% | |
|
| |||||||||||
| Personal control (How much control do you feel you have over your illness?) | |||||||||||
|
| |||||||||||
| Absolutely no control | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 Extreme control |
| 14% | 2% | 7% | 13% | 2% | 20% | 6% | 16% | 11% | 4% | 5% | |
|
| |||||||||||
| Treatment control (How much do you think your treatment can help your illness?) | |||||||||||
|
| |||||||||||
| Not at all | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 Extremely helpful |
| 0% | 0% | 3% | 2% | 4% | 14% | 8% | 21% | 22% | 10% | 16% | |
|
| |||||||||||
| Identity (How much do you experience symptoms from your illness?) | |||||||||||
|
| |||||||||||
| No symptoms at all | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 Many severe |
| 17% | 5% | 16% | 17% | 9% | 13% | 6% | 9% | 7% | 1% | 0% | |
|
| |||||||||||
| Concern (How concerned are you about your illness?) | |||||||||||
|
| |||||||||||
| Not at all concerned | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 Extremely concerned |
| 20% | 6% | 12% | 8% | 8% | 17% | 5% | 12% | 6% | 3% | 3% | |
|
| |||||||||||
| Understanding (How well do you feel you understand your illness?) | |||||||||||
|
| |||||||||||
| Don't understand | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 Very clearly |
| 3% | 2% | 6% | 2% | 3% | 16% | 4% | 20% | 19% | 4% | 21% | |
|
| |||||||||||
| Emotional response (How much does your illness affect you emotionally: Makes you angry, scared, upset or depressed?) | |||||||||||
|
| |||||||||||
| Not affected | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 Extremely affected |
| 23% | 5% | 9% | 10% | 9% | 12% | 8% | 15% | 6% | 0% | 3% | |
Table 3.
Internal consistency and reproducibility of the Arabic version of the Brief Illness Perception Questionnaire
| Internal consistency | ||||
|---|---|---|---|---|
|
| ||||
| Cronbach's Alpha | No. of items | |||
|
|
|
|||
| 0.717 | 8 | |||
|
|
|
|||
| Item-total statistics | Scale mean if item deleted | Scale variance if item deleted | Corrected item-total correlation | Cronbach's alpha if item deleted |
| Consequence | 25.64 | 116.576 | 0.574 | 0.649 |
| Timeline | 27.69 | 138.681 | 0.370 | 0.697 |
| Personal control | 24.05 | 144.573 | 0.153 | 0.743 |
| Treatment control | 26.39 | 141.614 | 0.377 | 0.697 |
| Identity | 25.67 | 128.728 | 0.504 | 0.670 |
| Concern | 25.30 | 119.444 | 0.560 | 0.653 |
| Understanding | 24.26 | 137.225 | 0.220 | 0.734 |
| Emotional response | 25.40 | 118.323 | 0.588 | 0.647 |
|
| ||||
| Reproducibility | ||||
|
| ||||
| 95% confidence interval | ||||
|
|
||||
| Intra-class correlation | Lower bound | Upper bound | p | |
|
| ||||
| Consequence | 0.981 | 0.960 | 0.991 | <0.0001 |
| Timeline | 0.952 | 0.902 | 0.977 | <0.0001 |
| Personal control | 0.955 | 0.907 | 0.979 | <0.0001 |
| Treatment control | 0.776 | 0.580 | 0.887 | <0.0001 |
| Identity | 0.938 | 0.874 | 0.970 | <0.0001 |
| Concern | 0.964 | 0.926 | 0.983 | <0.0001 |
| Understanding | 0.939 | 0.875 | 0.970 | <0.0001 |
| Emotional response | 0.966 | 0.930 | 0.984 | <0.0001 |
Table 4.
Spearman's correlations between the Arabic version of the Brief Illness Perception Questionnaire (Brief IPQ-Ar) dimension scores and the global Brief IPQ-Ar score (n=100)
| Dimension | p |
|---|---|
| Consequence | 0.724** |
| Timeline | 0.520** |
| Personal control | 0.373** |
| Treatment control | 0.509** |
| Identity | 0.644** |
| Concern | 0.707** |
| Understanding | 0.451** |
| Emotional response | 0.727** |
p-value (2-tailed) <0.001.
Assessment of discriminant validity (n=100)
Participants suffering from concomitant non-cardiac diseases scored significantly higher in the following dimensions: timeline, personal control, and coherence. They thought that their illness would continue for a longer period of time: average scores were 6.73±3.12 when no non-cardiac disease was associated, and 8.99±1.73 when non-cardiac diseases were associated (p<0.0001). They also felt that they understood their illness (average scores were 5.77±2.96 versus 7.01±5.56; p=0.003) and have control over it (average scores were 3.23±2.96 versus 5.31±2.78; p=0.005), when compared to participants with no concomitant non-cardiac diseases.
Moreover, for the timeline dimension, significant differences were also observed: those who felt that their illness would last longer had more than one cardiac disease (average score 9.06±1.70), while participants with cardiac arrhythmias felt that their illness would be shorter (average score 7.00±2.33; p=0.05). Furthermore, concern and emotional response were significantly higher among participants suffering from cardiomyopathies (average scores 6.50±3.11 and 7.00±2.94; p=0.05 and 0.03, respectively) (Table 5).
Table 5.
Comparison of average scores among participants with different cardiac diseases for the eight dimensions of the Brief-IPQ
| Consequence | Timeline* | Personal control | Treatment control | Identity | Concern* | Understanding | Emotional response* | |
|---|---|---|---|---|---|---|---|---|
| Hypertension (n=25) | 3.08±3.265 | 7.68±3.185 | 4.24±3.257 | 7.28±2.031 | 2.88±2.315 | 2.84±2.853 | 6.00±2.930 | 3.12±2.934 |
| Heart failure (n=10) | 5.20±2.700 | 9.40±1.350 | 4.40±2.757 | 7.10±1.663 | 4.30±2.541 | 4.90±1.912 | 6.50±1.958 | 5.80±1.932 |
| Cardiac arrhythmias (n=8) | 3.38±2.387 | 7.00±2.330 | 4.12±2.642 | 7.50±2.390 | 3.75±2.866 | 5.50±1.927 | 6.62±3.021 | 4.12±2.748 |
| Cardiomyopathies (n=4) | 4.50±3.697 | 9.25±1.500 | 4.75±1.708 | 6.75±1.500 | 3.75±3.500 | 6.50±3.109 | 4.00±2.944 | 7.00±2.944 |
| More than one disease (n=32) | 3.12±3.056 | 9.06±1.703 | 5.25±2.828 | 6.66±2.336 | 3.94±2.675 | 3.69±3.146 | 7.50±2.110 | 3.47±3.037 |
| Ischemic heart disease/coronary artery disease (n=21) | 3.90±3.113 | 8.57±1.912 | 5.48±3.140 | 7.90±1.546 | 3.19±2.272 | 3.90±2.965 | 7.14±2.988 | 3.43±2.580 |
Kruskal-Wallis test;
p≤0.05.
The number of drug intakes per day was significantly associated with the identity dimension: participants with three or more drug intakes per day reported more symptoms of their illness than those with fewer daily drug intakes: average scores 2.72±2.54 with one drug intake/day, 3.78±2.39 with two, and 4.77±2.45 with three or more (p=0.02). However, the number of drugs taken by the patients was not significantly associated with any dimension of the Brief IPQ-Ar (p>0.05).
Participants with longer treatment duration were less concerned about their cardiac disease (p<0.0001, r=−0.35) and thought their cardiac disease would continue for a longer time (p=0.002, r=0.31), (Table 6).
Table 6.
Spearman correlations between the Brief IPQ-Ar dimensions and level of education, treatment duration, and the number of pills ingested daily by the participants
| Level of education† (n=98) | Treatment duration (n=100) | Number of pills/day (n=100) | |
|---|---|---|---|
| Consequence | 0.040 | −0.063 | 0.200* |
| Timeline | −0.058 | 0.307** | 0.048 |
| Personal control | −0.005 | −0.068 | 0.032 |
| Treatment control | 0.034 | −0.106 | −0.007 |
| Identity | 0.085 | −0.053 | 0.262** |
| Concern | 0.209* | −0.347** | 0.074 |
| Understanding | 0.053 | −0.060 | −0.084 |
| Emotional response | 0.112 | −0.246* | 0.098 |
Spearman correlation;
p<0.05;
p<0.01;
missing values.
Participants taking more drug pills per day felt that their illness affected their lives more (p=0.03, r=0.21) and that they experienced more symptoms compared to those who took fewer pills (p=0.009, r=0.277) (Table 6).
Relationship between Brief IPQ-Ar version scores and sociodemographic variables (n=100)
When comparing item scores between males and females, the identity dimension showed a significant difference between sexes (p=0.049), with higher scores among males (4.0±2.5) than among females (3.0±2.5). Men experienced more symptoms from their cardiac disease compared to women.
The timeline and coherence dimensions were significantly related to marital status (p=0.006 and 0.02, respectively). Single participants thought that their illness would continue for a shorter time (average score: 6.90±2.90) than other participants, and divorced participants felt they understood their illness to be worse than that of other participants (average score 2.75±4.85).
The age of the participants was significantly related to the timeline, concern, and emotional response. Elderly participants (>65 years) thought that their illness would continue longer than younger participants (average score: 9.23±1.83; p<0.0001). However, they were less concerned about their illness (average score: 3.06±2.94; p=0.02) and less affected emotionally than younger participants (average score: 3.04±2.87), (p=0.03).
Participants with higher levels of education were more concerned about their illness than participants with lower levels of education (p=0.04, r=0.21) (Table 6).
Step 3: assessment of reproducibility
Thirty subjects (52% male) participated; 61% were <65 years old, 68% were married, and 77% had a secondary or better level of schooling. Reproducibility was satisfactory, with ICC values >0.776 (Table 3).
Discussion
Patients’ evaluations of their health care are now an established component of quality assessment (38). In chronic diseases, the current literature points to the value of assessing illness representations in understanding and predicting mental and physical outcomes (39). Therefore, a reliable and simple tool to evaluate IPs in various diseases is needed in Arab countries, and specifically in cardiac diseases because cardiometabolic diseases are the leading cause of mortality in the Middle East and North Africa, accounting for nearly one million deaths annually (40, 41).
The adaptation of a questionnaire for use in another country and another language is time consuming and costly. However, to date, it is the best way to get an equivalent metric for any self-attribute being considered (33). The cross-cultural adaptation of a health-status self-administered questionnaire for use in a new country, culture, and/or language necessitates the use of a unique method to reach equivalence between the original source and target versions of the questionnaires (33).
This study was the first to translate to Arabic and validate a widely used tool, the Brief IPQ, and perform a cross-cultural adaptation on a group of Lebanese patients. The study was conducted according to the methodology adopted by the International Society of Quality of Life Assessment (IQOLA) (42, 43). The process described in this paper was a process of translating to Arabic and adapting the Brief IPQ to make it relevant and valid in a new culture. Translation does not automatically provide a valid measure of another culture's health, and this was carefully verified throughout the process and the testing described in this paper.
The Brief IPQ-Ar showed good psychometric properties among Lebanese patients suffering from cardiac diseases. There was a 100% semantic equivalence between the Brief IPQ-Ar questions and patients’ descriptions. Cronbach's alpha was 0.717, which indicates good internal consistency, and it was 0.649 and 0.743 when, respectively, item 1 or 3 was deleted. Reproducibility was satisfactory, with ICC values above 0.776. Moreover, different items of the Brief IPQ-Ar were able to discriminate between patients according to the type of cardiac disease, concomitant non-cardiac diseases, and treatment-related characteristics.
The timeline dimension scores were worse among patients above 65 years, patients with concomitant non-cardiac diseases, widowed patients, and those with a longer duration of treatment. This means that these patients feel that their illness would be present for a very long time. For the personal control dimension, the scores were better among patients suffering from concomitant non-cardiac diseases compared to those who had no non-cardiac diseases. For the coherence dimension, scores were worse in patients with concomitant non-cardiac diseases and better among single patients. For the identity dimension, males scored higher than females, and patients with a greater number of daily drug intakes showed higher scores. Mohammed et al. (36), using the Brief-IPQ in patients suffering from tuberculosis (TB) in Sudan, previously showed that patients who experienced more symptoms (identity) expected severe consequences and had poor personal control over their illness, but that study did not examine differences between males and females nor did it explore drug intakes among patients. For the concern dimension, bad scores were found among patients above 65 years and patients suffering from ischemic heart disease or coronary artery disease. However, concern was better among participants with higher levels of education and those taking a high number of drug pills per day, which could mean that they perceived their illness as less threatening. We could not find published studies to help explain all our results because no previous studies assessed all the factors examined in our present work. We think that our observations justify future investigations with larger sample size and different clinical conditions; examining patients’ satisfaction with treatment together with illness perception could also help understand what was observed in our study regarding the relation between some dimensions of the Brief IPQ-Ar and patients’ treatment characteristics.
Finally, for the emotional response dimension, lower scores were observed among patients above 65 years; these patients, with poor emotional representations, would be expected to have a poor quality of life, as reported in a previous study done in Sudan using the Brief-IPQ (36).
Three dimensions of the Brief-IPQ (identity, emotional impact, and concern) have been associated with anxiety or depression in previous studies (44), whose authors proposed that IPs may be a useful basis for determining the need for psychological interventions in some patients. Our results encourage such interventions in patients with cardiac diseases, based on their Brief-IPQ domain scores.
Study limitations
This study was conducted on a convenience sample, which means that the representativeness of the sample could be an issue. Moreover, the study relied on a self-reported questionnaire and thus there is a risk of reporting and social desirability bias. The respondents may have forgotten pertinent details or over- or underestimated them to avoid revealing private information. The participants were assured that the results were confidential, so external pressures were unlikely to have significantly affected the responses. Finally, associations between IPs and coping behavior may be bi-directional, but the cross-sectional nature of this study did not allow us to assess directionality.
Conclusions
The results indicate that the Brief IPQ-Ar version is an appropriate instrument to explore illness perception in native Arabic-speaking patients suffering from cardiac diseases. Further research should be conducted to test this Arabic version in other types of diseases. The results also shed light on factors, not examined before, that could affect illness perception items in such patients, in particular, the number of drug pills taken daily by the patient and the number of drug intakes.
Authors' contributions
All authors have contributed to the design of the study or collection of data or writing the manuscript. All authors have read and approved the current manuscript.
Conflict of interest and funding
The authors declare that they have no conflict of interest.
References
- 1.Ministry of Health. Statistical bulletin-2006. Beirut, Lebanon: Ministry of Health; 2007. [Google Scholar]
- 2.Nawfal H. Resident issues in Lebanon ten years after the World Conference on Residents and Development: the national Report 2004. Beirut: Dar El Koutoub; 2004. [Google Scholar]
- 3.Sibai A, Hwalla N. WHO STEPS chronic disease factor surveillance: data book for Lebanon. Beirut, Lebanon: American University of Beirut; 2010. [Google Scholar]
- 4.Noureddine S, Froelicher ES, Sibai AM, Dakik H. Response to a cardiac event in relation to cardiac knowledge and risk perception in a Lebanese sample: a cross sectional survey. Int J Nurs Stud. 2010;47:332–41. doi: 10.1016/j.ijnurstu.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 5.Riley GA, Fisher G, Hagger BF, Elliott A, Le Serve H, Oyebode JR. The Birmingham Relationship Continuity Measure: the development and evaluation of a measure of the perceived continuity of spousal relationships in dementia. Int Psychogeriatr. 2013;25:263–74. doi: 10.1017/S1041610212001743. [DOI] [PubMed] [Google Scholar]
- 6.Leventhal H, Benyamini Y, Brownlee S, Diefenbach M, Leventhal E, Patrick-Muller L, et al. Perceptions of health & illness. Illness representations: theoretical foundations. United Kingdom: Harwood Academic; 1997. pp. 19–45. [Google Scholar]
- 7.Alsen P, Eriksson M. Illness perceptions of fatigue and the association with sense of coherence and stress in patients one year after myocardial infarction. J Clin Nurs. 2016;25:526–33. doi: 10.1111/jocn.13088. [DOI] [PubMed] [Google Scholar]
- 8.Leventhal H, Safer MA, Panagis DM. The impact of communications on the self-regulation of health beliefs, decisions, and behavior. Health Educ Q. 1983;10:3–29. doi: 10.1177/109019818301000101. [DOI] [PubMed] [Google Scholar]
- 9.DeLongis A, Folkman S, Lazarus RS. The impact of daily stress on health and mood: psychological and social resources as mediators. J Pers Soc Psychol. 1988;54:486–95. doi: 10.1037//0022-3514.54.3.486. [DOI] [PubMed] [Google Scholar]
- 10.Nahlen Bose C, Elfstrom ML, Bjorling G, Persson H, Saboonchi F. Patterns and the mediating role of avoidant coping style and illness perception on anxiety and depression in patients with chronic heart failure. Scand J Caring Sci. 2016 doi: 10.1111/scs.12297. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 11.Nahlen C, Saboonchi F. Coping, sense of coherence and the dimensions of affect in patients with chronic heart failure. Eur J Cardiovasc Nurs. 2010;9:118–25. doi: 10.1016/j.ejcnurse.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 12.Trivedi RB, Blumenthal JA, O'Connor C, Adams K, Hinderliter A, Dupree C, et al. Coping styles in heart failure patients with depressive symptoms. J Psychosom Res. 2009;67:339–46. doi: 10.1016/j.jpsychores.2009.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eisenberg SA, Shen BJ, Schwarz ER, Mallon S. Avoidant coping moderates the association between anxiety and patient-rated physical functioning in heart failure patients. J Behav Med. 2012;35:253–61. doi: 10.1007/s10865-011-9358-0. [DOI] [PubMed] [Google Scholar]
- 14.Knowles SR, Cook SI, Tribbick D. Relationship between health status, illness perceptions, coping strategies and psychological morbidity: a preliminary study with IBD stoma patients. J Crohns Colitis. 2013;7:e471–8. doi: 10.1016/j.crohns.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 15.Phillips LA, Leventhal H, Leventhal EA. Physicians’ communication of the common-sense self-regulation model results in greater reported adherence than physicians’ use of interpersonal skills. Br J Health Psychol. 2012;17:244–57. doi: 10.1111/j.2044-8287.2011.02035.x. [DOI] [PubMed] [Google Scholar]
- 16.Ladwig KH, Lederbogen F, Albus C, Angermann C, Borggrefe M, Fischer D, et al. Position paper on the importance of psychosocial factors in cardiology: update 2013. Ger Med Sci. 2014;12 doi: 10.3205/000194. Doc09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Balady GJ, Williams MA, Ades PA, Bittner V, Comoss P, Foody JM, et al. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: a scientific statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity, and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2007;115:2675–82. doi: 10.1161/CIRCULATIONAHA.106.180945. [DOI] [PubMed] [Google Scholar]
- 18.Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R, et al. European guidelines on cardiovascular disease prevention in clinical practice: executive summary. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts) Eur Heart J. 2007;28:2375–414. doi: 10.1093/eurheartj/ehm316. [DOI] [PubMed] [Google Scholar]
- 19.Goble AJ, Worcester MU, The Heart Research Center Best practice guidelines for cardiac rehabilitation and secondary prevention: a synopsis. 1999. Available from: http://www.rehabilitacioncardiaca.org/files/Guidelines_Rehabilitation_Australia_0.pdf [cited 16 May 2016]
- 20.Carels RA. The association between disease severity, functional status, depression and daily quality of life in congestive heart failure patients. Qual Life Res. 2004;13:63–72. doi: 10.1023/B:QURE.0000015301.58054.51. [DOI] [PubMed] [Google Scholar]
- 21.Petrie KJ, Jago LA, Devcich DA. The role of illness perceptions in patients with medical conditions. Curr Opin Psychiatry. 2007;20:163–7. doi: 10.1097/YCO.0b013e328014a871. [DOI] [PubMed] [Google Scholar]
- 22.Le Grande MR, Elliott PC, Worcester MU, Murphy BM, Goble AJ, Kugathasan V, et al. Identifying illness perception schemata and their association with depression and quality of life in cardiac patients. Psychol Health Med. 2012;17:709–22. doi: 10.1080/13548506.2012.661865. [DOI] [PubMed] [Google Scholar]
- 23.Goodman H, Firouzi A, Banya W, Lau-Walker M, Cowie MR. Illness perception, self-care behaviour and quality of life of heart failure patients: a longitudinal questionnaire survey. Int J Nurs Stud. 2013;50:945–53. doi: 10.1016/j.ijnurstu.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 24.Ross S, Walker A, MacLeod MJ. Patient compliance in hypertension: role of illness perceptions and treatment beliefs. J Hum Hypertens. 2004;18:607–13. doi: 10.1038/sj.jhh.1001721. [DOI] [PubMed] [Google Scholar]
- 25.Petrie KJ, Cameron LD, Ellis CJ, Buick D, Weinman J. Changing illness perceptions after myocardial infarction: an early intervention randomized controlled trial. Psychosom Med. 2002;64:580–6. doi: 10.1097/00006842-200207000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Nahlen Bose C, Persson H, Bjorling G, Ljunggren G, Elfstrom ML, Saboonchi F. Evaluation of a coping effectiveness training intervention in patients with chronic heart failure – a randomized controlled trial. Eur J Cardiovasc Nurs. 2016 doi: 10.1177/1474515115625033. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 27.Kaptein AA, Broadbent E. Illness cognition assessment. In: Ayers S, Baum A, McManus C, Newman S, Wallston K, Weinman J, et al., editors. Handbook of psychology, health and medicine. Cambridge: Cambridge University Press; 2007. pp. 268–73. [Google Scholar]
- 28.Weinman J, Petrie K, Moss-Morris R, Horne R. The illness perception questionnaire: a new method for assessing the cognitive representation of illness. Psychol Health. 1996;11:431–46. [Google Scholar]
- 29.Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60:631–7. doi: 10.1016/j.jpsychores.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 30.Kale MS, Federman AD, Krauskopf K, Wolf M, O'Conor R, Martynenko M, et al. The association of health literacy with illness and medication beliefs among patients with chronic obstructive pulmonary disease. PLoS One. 2015;10:e0123937. doi: 10.1371/journal.pone.0123937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kaptein AA, Yamaoka K, Snoei L, Kobayashi K, Uchida Y, van der Kloot WA, et al. Illness perceptions and quality of life in Japanese and Dutch patients with non-small-cell lung cancer. Lung Cancer. 2011;72:384–90. doi: 10.1016/j.lungcan.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 32.van der Velde JL, Flokstra-de Blok BM, Hamp A, Knibb RC, Duiverman EJ, Dubois AE. Adolescent-parent disagreement on health-related quality of life of food-allergic adolescents: who makes the difference? Allergy. 2011;66:1580–9. doi: 10.1111/j.1398-9995.2011.02726.x. [DOI] [PubMed] [Google Scholar]
- 33.Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976) 2000;25:3186–91. doi: 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]
- 34.Broadbent E, Kaptein AA, Petrie KJ. Double Dutch: the ‘think-aloud’ Brief IPQ study uses a Dutch translation with confusing wording and the wrong instructions. Br J Health Psychol. 2011;16:246–9. doi: 10.1111/j.2044-8287.2011.02021.x. [DOI] [PubMed] [Google Scholar]
- 35.Noureddine S, Froelicher ES. Psychometric testing of an Arabic version of the illness perception questionnaire for heart disease. Heart Lung. 2013;42:51–8. doi: 10.1016/j.hrtlng.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 36.Mohammed S, Nagla S, Morten S, Asma E, Arja A. Illness perceptions and quality of life among tuberculosis patients in Gezira, Sudan. Afr Health Sci. 2015;15:385–93. doi: 10.4314/ahs.v15i2.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.WHO. Global atlas on cardiovascular disease prevention and control. Available from: http://www.who.int/cardiovascular_diseases/publications/atlas_cvd/en/ [cited 8 June 2015]
- 38.Saarti S, Hajj A, Karam L, Jabbour H, Sarkis A, Osta N, et al. Association between adherence, treatment satisfaction and illness perception in hypertensive patients. J Hum Hypertens. 2015;30:341–5. doi: 10.1038/jhh.2015.86. [DOI] [PubMed] [Google Scholar]
- 39.Stanton AL, Revenson TA, Tennen H. Health psychology: psychological adjustment to chronic disease. Annu Rev Psychol. 2007;58:565–92. doi: 10.1146/annurev.psych.58.110405.085615. [DOI] [PubMed] [Google Scholar]
- 40.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380:2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ware JE, Jr., Gandek B. Methods for testing data quality, scaling assumptions, and reliability: the IQOLA Project approach. International Quality of Life Assessment. J Clin Epidemiol. 1998;51:945–52. doi: 10.1016/s0895-4356(98)00085-7. [DOI] [PubMed] [Google Scholar]
- 43.Ware JE, Jr., Keller SD, Gandek B, Brazier JE, Sullivan M. Evaluating translations of health status questionnaires. Methods from the IQOLA project. International Quality of Life Assessment. Int J Technol Assess Health Care. 1995;11:525–51. doi: 10.1017/s0266462300008710. [DOI] [PubMed] [Google Scholar]
- 44.Costa EC, Vale S, Sobral M, Graca Pereira M. Illness perceptions are the main predictors of depression and anxiety symptoms in patients with chronic pain. Psychol Health Med. 2015:1–13. doi: 10.1080/13548506.2015.1109673. [DOI] [PubMed] [Google Scholar]