Abstract
Background:
Calvarial hemangiomas are one of the rarest neoplasms affecting the skull, predominantly occurring in parietal and frontal bones.
Case Description:
We report a parietal hemangioma in a middle-aged female which presented as a painless swelling that was progressively increasing in size and was treated surgically.
Conclusion:
Although rare, calvarial hemangioma should be a part of the differential diagnosis of calvarial swellings.
Keywords: Calvarial, hemangioma, skull
INTRODUCTION
Primary intraosseous hemangiomas are benign slow-growing neoplasms. More than 50% of incidences occur in the vertebrae and skull.[20] They are rare tumors in the calvarium and represent 2% of osseous calvarial lesions and 0.2% of all bone neoplasms.[13] The parietal and frontal bones are the most common locations, but may occur in any skull bone. In very rare instances, multifocal hemangiomas may occur. They are found more frequently in females.[13,20]
CASE REPORT
A 40-year-old female with no history of head trauma presented with painless swelling in the parietal area, progressively increasing in size, since last 2 years. The patient complained of local tenderness. Anteroposterior and lateral views of plain X-ray skull revealed classical honeycomb appearance lesion [Figures 1 and 2]. The diploe was enlarged and both tables of the skull were bulging, outer more than the inner. There was no intracranial extension. A computed tomography (CT) scan of head with bone window images showed the hypodense lesions with sharp, thickened, sclerotic margins [Figures 3 and 4]. Trabeculae which were vertically oriented were widely separated. Evaluation for primary malignancy elsewhere proved to be negative including ultrasonography (USG) neck for thyroid and cervical lymph nodes. 99mTechnitium (Tc) labeled bone scan showed no abnormal uptake elsewhere excepting mild increase at the calvarial site. En bloc excision of the tumor-bearing bone and wide curettage was done till healthy margins of the bone were seen all around. Underneath, dura mater was not involved and was healthy. Curetted vascular tumor was routinely sent for frozen/crush smear examination, which was reported as hemangioma and rest of the material along with the bone pieces was sent for histopathological examination, which was also subsequently reported as hemangioma. The patient was left with an oblong craniectomy defect, measuring 8 cm × 10 cm. Cranioplasty was done in the same sitting using polymethyl methacrylate [Figure 5]. Postoperatively, the patient had mild wound infection, which was treated effectively by systemic antibiotics.
Figure 1.

Lateral views of plain X-ray skull that revealed classical honeycomb appearance lesion
Figure 2.
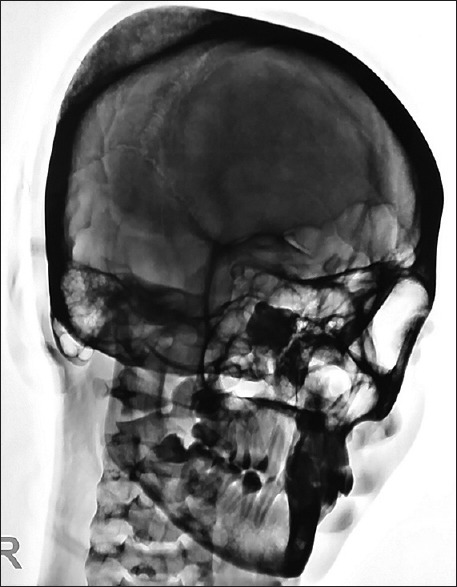
Lateral views of plain X-ray (negative image) skull that revealed classical honeycomb appearance lesion
Figure 3.
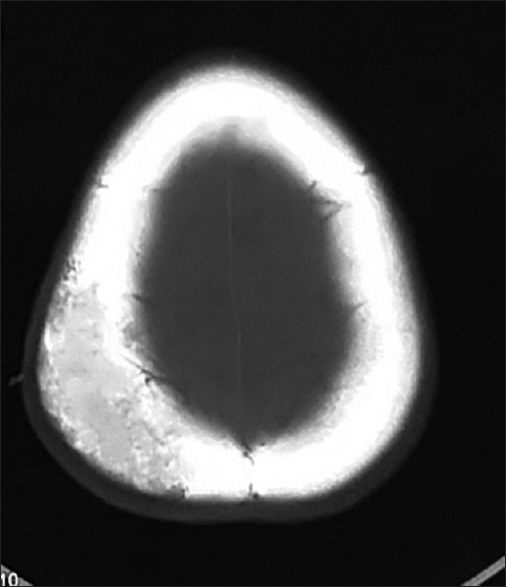
Noncontrast computed tomography head (axial view and bone window) image showing the hypodense lesions with sharp, thickened, sclerotic margins
Figure 4.
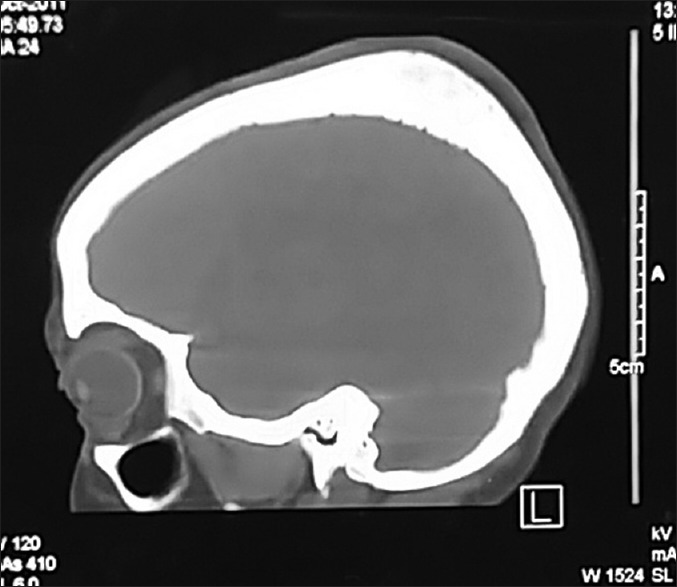
Noncontrast computed tomography head (sagittal and bone window) image showing the hypodense lesions in parietal region
Figure 5.

Postoperative X-ray skull anteroposterior and lateral view showing postoperative defect
DISCUSSION
Presentation
Calvarial hemangiomas are benign, malformed vascular lesions, are usually asymptomatic, and are usually discovered incidentally on imaging or postmortem examination. They are mostly encountered in the middle-aged persons, generally occurs more commonly in females than males with a ratio of 3:2. There is no documental racial variation in the frequency of hemangiomas of skull, worldwide. Though cranial hemangiomas are second only to vertebral hemangiomas in frequency, such lesions are rarely congenital and multiple. It is probable that the true incidence of congenital calvarial hemangiomas is higher than that reported in the literature, as they are unlikely to undergo imaging, most being asymptomatic and without a significant soft tissue component.[9,13,20]
Symptomatic patients present with headaches, often with focal scalp pain or swelling. A palpable bony sessile mass may or may not be present.[13] Palpability is due to a lump produced by an expansion of the outer table of the bone involved.[14] A bruit is uncommon. Trauma may be an antecedent factor, although this is not elicited in the patients’ history.[3]
Cases have been reported from the roof of the orbit when they present with proptosis, blindness, or extraocular palsies.[1] Hemangiomas of the petrous bone may present with deafness and cranial nerve palsies. Rarely, intracranial extension of the tumor is seen.[15] Hemangioma of the calvaria had hemorrhaged and eroded through the inner table of the skull and dura mater and presented as subdural hematoma.[5] Few cases of patients presenting with intradiploic or epidural hemorrhage have been reported in the literature.[7] Congenital hemangioma of the temporal bone has been reported, which was detected by USG and magnetic resonance imaging (MRI) of the fetus in the 32nd week of gestation as a large extra-axial tumor with intra- and extra-cranial extension. After birth, the mass was totally removed on the 4th day of life and was found at surgery to originate from the skull. Histopathological diagnosis was a calvarial hemangioma. Multiple focal hemangiomas were reported in association with a nasal osteoma.[11] Multiple calvarial hemangiomas of the inner table extension were observed in middle-aged women.[10]
Differential diagnosis
The differential diagnosis of a solitary circumscribed expansile intradiploic cranial lesion includes an osteoma, aneurysmal bone cyst, giant cell tumor, fibrous dysplasia, Langerhans’ cell histiocytosis, sarcoma, meningioma, metastatic disease, Paget's disease, lymphoma, and dermoid tumor.[11,20]
Pathology
According to the predominant type of vascular channel, four histological variants of hemangiomas are known; cavernous, capillary, arteriovenous, and venous. Bone hemangiomas are predominantly of the cavernous and capillary varieties. Cavernous hemangiomas most frequently occur in the skull whereas capillary hemangiomas predominate in the vertebral column; overall cavernous ones are commonly seen. Malignant degeneration is virtually unknown. Rarely, locally aggressive growth patterns are recognized, mimicking malignant lesions. Gross pathology reveals well-demarcated, unencapsulated lesions with cystic red cavities. Microscopic examination shows hamartomatous proliferations of vascular tissue within endothelial-lined spaces, but may also contain fat, smooth muscle, fibrous tissue, and thrombus.[6,14,17] An abnormal capillary bed is consequent to faulty differentiation of primordial vessels. Variable-sized sinusoidal channels are interposed between an artery and a vein. In the cavernous type, enlargement occurs as these blood-filled sinusoidal channels erode through or remodel contiguous tissues. Necrotic changes are present when larger tumors outgrow their blood supply.[13] Growth occurs by expansion of the outer table and rarely there is intracranial penetration.[20]
Radiographic features
Plain film
Evaluation of cranial vault hemangioma starts with a plain radiograph, which usually shows lytic lesion with a sclerotic rim (usually with a honeycomb or sunburst-like appearance). Outer table is usually involved with the preservation of the inner table. Prominent vascular grooves are usually present.
Computed tomography
CT scan is required for further characterization of these lesions as it is useful for assessing the changes in bone trabeculae and supports the plain radiographic findings, in a greater detail. Usually, it presents as an expansive bone lesion with thin borders and characteristic sunburst pattern of trabecular thickening radiating from a common center. Erosions of both internal and external plates can occur and may be associated with internal or external tumor expansion. On contrast administration, homogenous enhancement is seen.[6,14,17]
Magnetic resonance imaging
MRI features largely depend on the proportion of fat and vascularity of the lesions. Scattered foci of hyper- and hypo-intense T1 signal with predominant intermediate T1 signal are seen on MRI imaging. Low signal intensity on T1-weighted images indicates decreased marrow fat or greater vascular component, may be correlated with more aggressive behavior. Thickened trabeculae demonstrate low signal intensity on MRIs obtained in all sequences.[20]
On T2-weighted images, hemangiomas generally appear as multiple high-signal intensity lobules that resemble a bunch of grapes. This appearance is due to cavernous or cystic vascular spaces containing stagnant blood. Fluid-fluid levels can also be noted within these spaces.[16] Punctate or reticular low-signal intensity areas may be present, representing fibrous tissue, fast flow within vessels, or foci of calcification. Areas of thrombosis appear as circular low-signal intensity areas at MRI similar to phleboliths. Hyperintense signal on T2-weighted images correlates with intralesional fat content. Hemangiomas demonstrate avid enhancement after gadolinium administration.[20] Small capillary hemangiomas can demonstrate homogeneous signal intensity and high perfusion whereas cavernous hemangiomas demonstrate low perfusion.[21]
Digital subtraction angiography
Angiography confirms the hypervascularity of the lesions showing enlargement of the external carotid artery branches.[15] Rarely, there may be an internal carotid supply.[12] Angiography is usually performed in conjunction with embolization of systematic hemangiomas prior to surgery. As majority of the lesions are seen in parietal and frontal bones, middle meningeal and superficial temporal arteries tend to be the most common arterial feeders. The feeding vessels often have a coarse appearance. No direct arterial or venous communication exists, so no draining vein is identified in early arterial phase. However, due to increased flow, dilated and tortuous veins may be seen.[2,18]
Skeletal scintigraphy
On 99mTc methylene diphosphonate scintigrams, calvarial hemangiomas may show a level of radionucleotide uptake that is lower than, equal to, or slightly higher than that in surrounding bone. Hence, in addition, use of adjunctive99m Tc-labeled red blood cell (RBC) scans is made. Likewise the dynamic scintigraphic imaging in the diagnosis of hepatic hemangiomas which is characterized by increased accumulation of a RBC tracer on delayed blood pool images, similar criterion has been used in the diagnosis of calvarial hemangiomas; however, detection is limited in lesions <10 mm.[8,19] Scans show increased activity on blood flow studies and continued accumulation on delayed static images.[4]
Treatment and prognosis
Treatment is not always necessary and indications include mass effects, hemorrhage control, and esthetic improvement. Whenever indicated, total surgical removal is the recommended treatment and is determinant of a definitive diagnosis. Radiotherapy is advisable in situations where excision is not feasible. Doses up to 30 Gy (3000 rads), in 3 weeks, may be required. In addition to these, embolization to reduce the intraoperative blood loss and intralesional steroid injection have also been tried.[12,17]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Contributor Information
Altaf Rehman Kirmani, Email: altafkirmani@yahoo.com.
Arif Hussain Sarmast, Email: arifhsarmast@gmail.com.
Abdul Rashid Bhat, Email: abdulrashid@yahoo.com.
REFERENCES
- 1.Banerji D, Inao S, Sugita K, Kaur A, Chhabra DK. Primary intraosseous orbital hemangioma: A case report and review of the literature. Neurosurgery. 1994;35:1131–4. doi: 10.1227/00006123-199412000-00017. [DOI] [PubMed] [Google Scholar]
- 2.Davis DO, Rumbaugh CL, Petty J. Calvarial hemangioma: Tumor stain and meningeal artery blood supply. Case report. J Neurosurg. 1966;25:561–3. doi: 10.3171/jns.1966.25.5.0561. [DOI] [PubMed] [Google Scholar]
- 3.Dorfman HD, Steiner GC, Jaffe HL. Vascular tumors of bone. Hum Pathol. 1971;2:349–76. doi: 10.1016/s0046-8177(71)80004-7. [DOI] [PubMed] [Google Scholar]
- 4.Gavant ML, Massie JD, Gerald B. Radionuclide blood pool imaging of calvarial hemangioma. Clin Nucl Med. 1983;8:495–6. doi: 10.1097/00003072-198310000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Gottfried ON, Gluf WM, Schmidt MH. Cavernous hemangioma of the skull presenting with subdural hematoma. Case report. Neurosurg Focus. 2004;17:ECP1. doi: 10.3171/foc.2004.17.4.7. [DOI] [PubMed] [Google Scholar]
- 6.Gourin CG, Millay DJ. Pathology forum: Quiz case 3. Diagnosis: Cavernous hemangioma of the nasal bones. Arch Otolaryngol Head Neck Surg. 2000;126(902):906–7. [PubMed] [Google Scholar]
- 7.Honda M, Toda K, Baba H, Yonekura M. Congenital cavernous angioma of the temporal bone: Case report. Surg Neurol. 2003;59:120–3. doi: 10.1016/s0090-3019(02)00985-0. [DOI] [PubMed] [Google Scholar]
- 8.Ki WW, Shin JW, Won KS, Ryu JS, Yang SO, Lee HK, et al. Diagnosis of orbital cavernous hemangioma with Tc-99m RBC SPECT. Clin Nucl Med. 1997;22:546–9. doi: 10.1097/00003072-199708000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Koulouris G, Rao P. Multiple congenital cranial hemangiomas. Skeletal Radiol. 2005;34:485–9. doi: 10.1007/s00256-004-0891-6. [DOI] [PubMed] [Google Scholar]
- 10.Kumar NA, Ranganadham P, Bhaskar G, Chowdhury AR. Multiple calvarial cavernous haemangiomas: Case report and review of the literature. Neuroradiology. 1996;38(Suppl 1):S83–5. doi: 10.1007/BF02278128. [DOI] [PubMed] [Google Scholar]
- 11.Kuzeyli K, Usul H, Cakir E, Caylan R, Rei A, Baykal S, et al. Multifocal intradiploic cavernous hemangioma of the skull associated with nasal osteoma. Acta Neurochir (Wien) 2003;145:323–6. doi: 10.1007/s00701-003-0005-6. [DOI] [PubMed] [Google Scholar]
- 12.Moss WT. The heart and blood vessels. In: Brand WN, Battifora H, editors. Radiation Oncology, Rationale, Technique, Results. St. Louis: CV Mosby Co; 1973. pp. 248–56. [Google Scholar]
- 13.Peterson DL, Murk SE, Story JL. Multifocal cavernous hemangioma of the skull: Report of a case and review of the literature. Neurosurgery. 1992;30:778–81. [PubMed] [Google Scholar]
- 14.Politi M, Romeike BF, Papanagiotou P, Nabhan A, Struffert T, Feiden W, et al. Intraosseous hemangioma of the skull with dural tail sign: Radiologic features with pathologic correlation. AJNR Am J Neuroradiol. 2005;26:2049–52. [PMC free article] [PubMed] [Google Scholar]
- 15.Ramamurthi B, Narasimhan ST, Pillai KM. Haemangioma of the skull. J Indian Med Assoc. 1959;32:201–3. [PubMed] [Google Scholar]
- 16.Ramon F. Tumors and tumor-like lesions of blood vessels. In: De Schepper AM, editor. Imaging of Soft Tissue Tumors. 2nd ed. Berlin, Germany: Springer-Verlag; 2001. pp. 225–44. [Google Scholar]
- 17.Reis BL, Carvalho GT, Sousa AA, Freitas WB, Brandão RA. Primary hemangioma of the skull. Arq Neuropsiquiatr. 2008;66:569–71. doi: 10.1590/s0004-282x2008000400029. [DOI] [PubMed] [Google Scholar]
- 18.Rosenbaum AE, Rossi P, Schechter MM, Sheehan JP. Angiography of haemangiomata of the calvarium. Br J Radiol. 1969;42:682–7. doi: 10.1259/0007-1285-42-501-682. [DOI] [PubMed] [Google Scholar]
- 19.Sayit E, Durak I, Capakaya G, Yilmaz M, Durak H. The role of Tc-99m RBC scintigraphy in the differential diagnosis of orbital cavernous hemangioma. Ann Nucl Med. 2001;15:149–51. doi: 10.1007/BF02988606. [DOI] [PubMed] [Google Scholar]
- 20.Suzuki Y, Ikeda H, Matsumoto K. Neuroradiological features of intraosseous cavernous hemangioma – case report. Neurol Med Chir (Tokyo) 2001;41:279–82. doi: 10.2176/nmc.41.279. [DOI] [PubMed] [Google Scholar]
- 21.van Rijswijk CS, van der Linden E, van der Woude HJ, van Baalen JM, Bloem JL. Value of dynamic contrast-enhanced MR imaging in diagnosing and classifying peripheral vascular malformations. AJR Am J Roentgenol. 2002;178:1181–7. doi: 10.2214/ajr.178.5.1781181. [DOI] [PubMed] [Google Scholar]


