Abstract
Cataract surgery in eyes with microcornea is associated with frequent complications such as corneal edema, posterior capsular rent, and risk of unplanned aphakia. We describe an improved surgical technique for the creation of surgical incisions during phacoemulsification in eyes with cataract associated with microcornea. A retrospective analysis of eight patients (8 eyes) operated at our center was undertaken. The mean age of the patients was 29.5 ± 10.9 years. All eyes were operated using the scleral pocket incision for phacoemulsification. This scleral pocket incision was tangential to the limbus and created approximately 2.5 mm behind limbus through which phacoemulsification probe was inserted. Because of the posterior placement of incision, the anterior chamber crowding was minimized. There was no incidence of port-site peripheral corneal edema. Fifty percent eyes developed transient central corneal edema, the intraocular lens in bag was implanted in 5/8 eyes, and none developed Descemet's membrane detachment. Mean best-corrected visual acuity improved from 1.85 ± 0.38 logarithm of minimum angle of resolution (LogMAR) to 1.26 ± 0.70 LogMAR postoperatively (P = 0.01; paired t-test). Posterior incision placement during phacoemulsification in microcornea helps achieve favorable postoperative outcomes in contrast to outcomes using clear corneal approach described in literature.
Keywords: Cataract, microcornea, phacoemulsification, scleral pocket incision
Cataract surgery in eyes with microcornea is challenging for the operating surgeon because of issues related to the choice of anesthesia, surgical technique, decision to implant intraocular lens (IOL), and final postoperative rehabilitation. Due to anatomical peculiarities, these eyes have a greater incidence of intraoperative complications and limited postoperative outcome; and hence require a meticulous preoperative management plan. We describe our outcomes of phacoemulsification using scleral pocket incision in such eyes.
In this retrospective study, surgical records of patients which presented with microcornea and a complicated cataract at the “Lens services” of a tertiary care center during January 2013 to December 2013 were obtained. Written informed consent was taken from the patients before surgery. The study adhered to the principles of the Declaration of Helsinki. Details regarding age, gender, presenting visual acuity, intra-operative measurement of horizontal and vertical corneal diameter, associated ocular anomalies, grade of nuclear sclerosis (NS), anterior vitrectomy (if performed,) and IOL status were recorded. Best-corrected visual acuity (Snellen's equivalent) recorded at 1-month postoperatively along with salient postoperative outcomes were obtained.
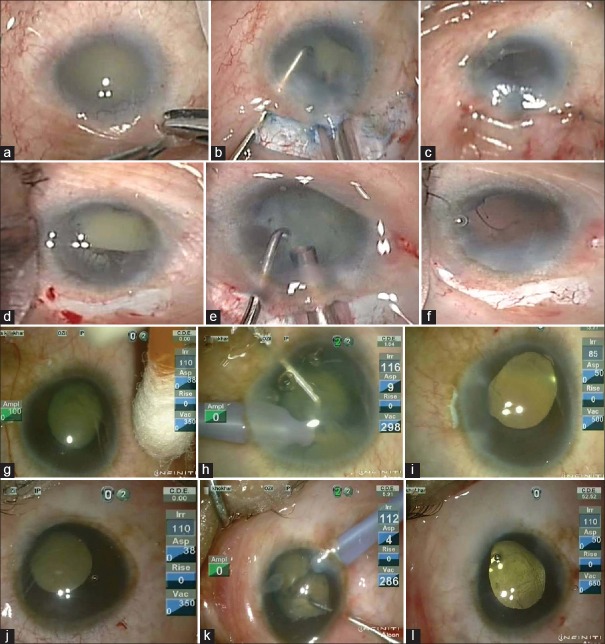
Under appropriate anesthesia, a partial thickness lamellar scleral incision was created 2.5 mm behind the limbus either transconjunctivally or through localized peritomy [Fig. 1]. A 2.8 mm triplanar scleral incision was created in Cases 1 and 2 [Table 1], and a 2.2 mm main port was made 2.5 mm behind the sclera temporally in Cases 3-8. One side port was made at 6 o'clock position. “Arshinoff soft shell” technique was used for corneal endothelial protection during phacoemulsification. Nuclear fragmentation was achieved using primary chopping. Microincision phacoemulsification using OZil torsional (Infiniti Vision System, Alcon Inc., Fort Worth, Texas, USA) coupled with OZil IP system (Intelligent phacoemulsification) was used. High efficiency 45° angled Kelman phaco tip with 1.1 mm miniflare design was used to increase surface area for efficient phacoemulsification. Parameters were set as bottle height of 110 cm, 100% continuous torsional energy, vacuum of 350 mmHg, and aspiration flow rate at 35 cc/min (Video). Modified Sanders-Retzlaff-Kraff II was used for IOL power calculation.
Figure 1.
Intraoperative photographs showing microophthalmos with partial aniridia with complicated brunescent cataract (a-c: Case #3) (d-f: Case #4) (g-i: Case #1) (j-l: Case #2). The corneal diameter can be estimated from the size of phaco probe (2.2 mm in a-f; 2.8 mm in g-l). The scleral tunnel has been made after localized peritomy in a-f. Because of inability to implant any implant intraocular lens in such microphthalmic eyes in Cases 3 and 4, patients were left aphakic after doing limited anterior vitrectomy to decrease the risk of visual axis obscuration from posterior capsular opacification. On the contrary, implant intraocular lens has been implanted in Cases 1 and 2
Table 1.
The clinical details of patients who were operated with scleral tunnel phacoemulsification
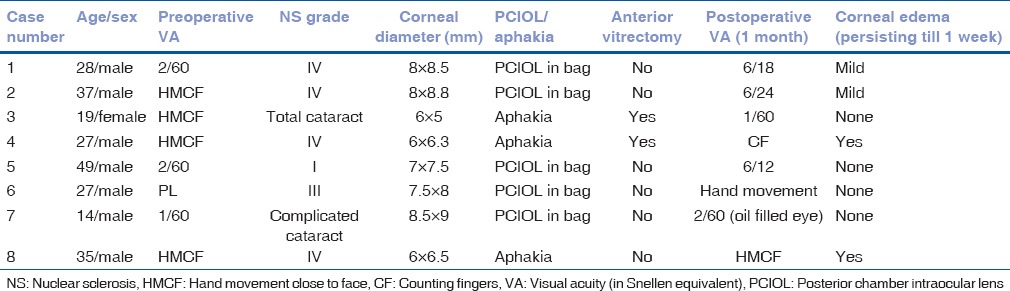
Eight eyes (eight patients) with overall corneal diameter <11 mm (range 5-9 mm) were operated. The mean age of the operated patients was 29.5 ± 10.9 years. All eyes had severe microcornea <9 mm in our series and 3/8 eyes had very severe microcornea <7 mm. Seven patients had associated iridofundal coloboma, whereas one (patient #3) had microcornea, microphthalmos, and an ill-formed iris with total cataract [Table 1]. Mean best-corrected visual acuity improved from 1.85 ± 0.38 logarithm of minimum angle of resolution (LogMAR) to 1.26 ± 0.70 LogMAR postoperatively (P = 0.01; paired t-test).
All patients were operated under peribulbar anesthesia except one (patient #7) for whom general anesthesia was administered. Removal of the posterior capsule and anterior vitrectomy were performed in three eyes which were left aphakic as the corneal diameter in each of these was < 6.5 mm. An inadvertent posterior capsular rent had occurred in Case #4 during phacoemulsification. In others, anterior vitrectomy and complete removal of the posterior capsule were performed to prevent visual axis opacification which is difficult to treat by neodymium-doped:yttrium aluminum garnet laser capsulotomy postoperatively due to associated nystagmus.
Posterior chamber IOL (aspheric AcrySof IQ IOL, Alcon, Fort Worth, Texas, USA) was implanted in the bag in 5/8 of eyes; the minimum corneal diameter to receive an implant was 7 mm × 7.5 mm in patient #5 [Table 1 and Fig. 1]. The mean cumulative dissipated energy (CDE) was 32.44 CDE units (range: 13.27-52.43 CDE units). Port site Descemet's detachment was not seen in any of these eyes. The central corneal edema was observed in 4/8 eyes postoperatively [Table 1] of which two had transient central edema; none developed port-site peripheral corneal edema. Two eyes had edema which persisted for >1 week postoperatively; they had NS Grade IV and severe microcornea and had undergone anterior vitrectomy.
Microcornea is defined as corneal diameter <2 standard deviation below normal population range or <11 mm horizontally.[1] Cataract surgery in eyes with microcornea is challenging. Nystagmus makes preoperative assessment difficult. Crowded anterior chamber makes intraoperative maneuvers difficult. If associated with coloboma, nuclei are bulkier, harder, and tackier to chop than what they appear to be preoperatively.[2] In addition, these eyes may be associated with poor corneal surface/sclerocornea, nondilating pupils/iris coloboma, zonular laxity, and increased risk of zonular dialysis, posterior capsular tear, vitreous prolapse, and poor visual gain due to foveal hypoplasia/macular coloboma or amblyopia.[1,2,3,4,5,6]
We could place a 6 mm optic in 5/8 eyes suggesting that the foldable acrylic lenses can be implanted safely in eyes with small corneal diameter. Determining actual sulcus diameter biomicroscopically could provide more accurate information about bag and IOL sizing.
Posterior incision placement provided an enlarged anterior chamber while minimizing the risk of port-site Descemet's detachment, postoperative peripheral corneal edema, and formation of the clear corneal scar, commonly seen with clear corneal incisions. In addition, scleral incisions impart greater wound strength and induce lesser astigmatism when compared with corneal incisions.[7]
Following lens aspiration in twenty pediatric microphthalmic eyes, corneal incision was associated with severe corneal edema and corneal opacity in 3/10 eyes.[3] Nishina et al. described lensectomy with anterior vitrectomy for pediatric cataracts in severe microcornea.[4] Chaurasia et al. described phacoemulsification in 3 eyes with microcornea with choroidal coloboma which was uncomplicated in 3 eyes and small incision cataract surgery in 3 eyes, of which 2 eyes required anterior vitrectomy.[5] Larger incisions for cataract extraction in these eyes may be associated with an increased incidence of vitreous prolapse due to greater anterior chamber collapse.[8]
Nordlund et al. in their series of choroidal coloboma with cataract, 2 of the eyes with microphthalmos were operated using superior scleral incision and aphakia and clear corneal temporal incision in the second. Temporal scleral approach seems to be better as forehead restricts the movement of phaco handpiece in the superior approach. Hence, varied approaches with regards to incision location, length, and placement as well as the technique of cataract extraction have been performed in eyes with microcornea, with not so appropriate outcomes. We recommend performing scleral tunnel temporal incisions in eyes with microcornea. Limitations include lack of a control group and outcomes in a small series with relatively short follow-up period. Nevertheless, the described technique allows easy intraoperative maneuverability along with providing favorable short-term postoperative outcomes.
Video Available on: www.ijo.in
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Batra DV, Paul SD. Microcornea with myopia. Br J Ophthalmol. 1967;51:57–60. doi: 10.1136/bjo.51.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khokhar S, Gupta S, Kusumesh R, Kumar G. Outcomes of phacoemulsification in eyes with congenital choroidal coloboma. Graefes Arch Clin Exp Ophthalmol. 2013;251:2489–90. doi: 10.1007/s00417-013-2397-1. [DOI] [PubMed] [Google Scholar]
- 3.Yu YS, Kim SJ, Choung HK. Posterior chamber intraocular lens implantation in pediatric cataract with microcornea and/or microphthalmos. Korean J Ophthalmol. 2006;20:151–5. doi: 10.3341/kjo.2006.20.3.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nishina S, Noda E, Azuma N. Outcome of early surgery for bilateral congenital cataracts in eyes with microcornea. Am J Ophthalmol. 2007;144:276–280. doi: 10.1016/j.ajo.2007.04.019. [DOI] [PubMed] [Google Scholar]
- 5.Chaurasia S, Ramappa M, Sangwan VS. Cataract surgery in eyes with congenital iridolenticular choroidal coloboma. Br J Ophthalmol. 2012;96:138–40. doi: 10.1136/bjophthalmol-2011-300233. [DOI] [PubMed] [Google Scholar]
- 6.Nordlund ML, Sugar A, Moroi SE. Phacoemulsification and intraocular lens placement in eyes with cataract and congenital coloboma: Visual acuity and complications. J Cataract Refract Surg. 2000;26:1035–40. doi: 10.1016/s0886-3350(00)00433-8. [DOI] [PubMed] [Google Scholar]
- 7.Freeman JM. Scleral stretch incision for cataract surgery. A technique for no-suture closure and control of astigmatism. J Cataract Refract Surg. 1991;17(Suppl):696–701. [PubMed] [Google Scholar]
- 8.Nixeaman DH. Cataract extraction in a case of congenital coloboma of the iris. Br J Ophthalmol. 1968;52:625–7. doi: 10.1136/bjo.52.8.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.