Abstract
Test-specific reminder letters can improve cancer screening adherence. Little is known about the effectiveness of a reminder system that targets the whole person by including multiple screening recommendations per letter. We compared the effectiveness of a Pap-specific reminder letter sent 27 months after a woman’s last Pap, to a reminder letter that included up to seven preventive service recommendations sent before a woman’s birthday (“birthday letter”) on Pap smear adherence from a natural experiment occurring in routine clinical care. Participants included 82,016 women from Washington state who received 72,615 Pap-specific letters between 2003–2007 and 100,218 birthday letters between 2009–2012. We defined adherence as having a Pap test within a six month window around the Pap test due date. Using logistic regression, we calculated adjusted odds ratios (OR) for adherence with 95% confidence intervals (CI) following the birthday letter with 1–2 recommendations, 3–5 recommendations, and 6–7 recommendations compared to the Pap-specific letter. All analyses were stratified by whether a woman was up-to-date or overdue for screening at the time she received a letter. Adjusted ORs showed reduced adherence following the birthday letter compared with the Pap-specific letter for up-to-date women whether the letter had 1–2 recommendations (OR=0.37, 95%CI=0.36–0.39), 3–5 recommendations (OR=0.44, 95%CI=0.42–0.45), or 6–7 recommendations (OR=0.36, 95%CI=0.32–0.40). We noted no difference in Pap-test adherence between letter types for overdue women. In conclusion, for women regularly adherent to screening, an annual birthday letter containing reminders for multiple preventive services was less effective at promoting cervical cancer screening compared with a Pap-specific letter.
Keywords: cervical cancer, reminder letters, adherence, preventive care, outreach, screening programs
Background
Cervical cancer is highly preventable through regular and appropriate screening. In 2012, National Healthcare Effectiveness Data and Information Set (HEDIS) data demonstrated that between 65–75% of women ages 21–64 received a Pap exam in the past three years.(1) Cervical cancer screening is both underused and overused (50% of eligible women are screened more frequently than recommended).(2–4) One explanation for under- and overuse of Pap testing may be the rapid evolution of cervical cancer screening guidelines over the past decade. These changes include narrower screening ages (starting at an older age and ending at a younger age) and wider screening intervals (from annual to every 3–5 years),(5, 6) and may lead to confusion among women and providers about screening frequency.
Reminders are one of the most effective interventions for increasing and maintaining Pap test adherence.(7) Studies have shown reminder letters increase adherence to screening for breast,(8–11) colon,(12, 13) and cervical cancers.(14–16) Most previous studies of reminders have evaluated the effectiveness of a letter or phone call that targets a single preventive service. For example, a 55-year old woman might receive three separate reminder letters for breast, colon, and cervical cancer screenings with three different due dates. Reminders for these screenings may co-occur with other recommended prevention activities such as cholesterol screening or getting a flu shot, making it highly complex and costly for a provider or healthcare system to send individual reminders for each.
A consolidated reminder letter sent once per year that targets the whole person by including multiple preventive service recommendations might be more efficient and coordinated than sending multiple test-specific reminders. However, sending a single reminder letter annually would not be timed with due dates for preventive services. The potential benefits and drawbacks of this type of reminder system are not well understood. We previously conducted an analysis comparing the effectiveness of a single reminder letter for multiple preventive services sent around the time of a person’s birthday, to a reminder letter for mammography only sent right before a woman was due.(10) We found that the birthday letter resulted in poorer adherence to breast cancer screening compared with the mammogram-specific letter. We conducted an analysis to compare the effectiveness of the birthday reminder letter to a cervical cancer screening-specific reminder letter on Pap test adherence.
Materials and Methods
This study took place at Group Health (GH), a mixed-model health care delivery system in Washington State that provides health care and/or health insurance to its 600,000 members. We evaluated a natural experiment that occurred in routine clinical practice using different prevention reminder letters. From 2003 through 2007, GH sent letters to women ages 20–65 years reminding them that they were due for a Pap test. Starting in 2007, GH phased out the Pap-specific reminder letters and phased in a new letter sent before a woman’s birthday that reminded her of all preventive services she was due for in the future (the next 12 months and beyond for services with longer screening intervals) based on gender, age, and risk factors. The birthday letters completely replaced the Pap-specific letters by December 2008. Additional details about each letter type are described below. The GH Human Subjects Review Committee approved all study procedures.
Study population
We included women who were between the ages of 21–64 years and who received a reminder letter (either Pap-specific or birthday letter) for cervical cancer screening at GH between 2003–2012. To be eligible for our study, women had to be continuously enrolled in GH for 3 years before the reminder letter was sent in order to determine whether they were up-to-date or overdue for cervical cancer screening at the time they received either reminder letter (N=88,421 women sent Pap letters and 112,722 women sent birthday letters, Figure 1). Women were excluded from our analysis if they had a hysterectomy; received multiple letters within 6 months of each other with similar due dates because we could not attribute cervical cancer screening adherence to one letter over another; received letters between April 2007 and December 2008 during the overlapping transition period between the two reminder strategies, because we could not attribute cervical cancer screening to one letter over another; did not have enough follow-up time after receiving their letter (because they disenrolled or died) to get a Pap test; or received birthday letters with a previous Pap date that was inconsistent with data sources and could not be verified. Our final sample sizes were 53,571 women (60.6% of original sample) receiving 72,615 Pap letters and 65,926 women (58.5% of original sample) receiving 100,218 birthday letters.
Figure 1. CONSORT diagram of women (and letters) included in the study after each exclusion criterion was applied.
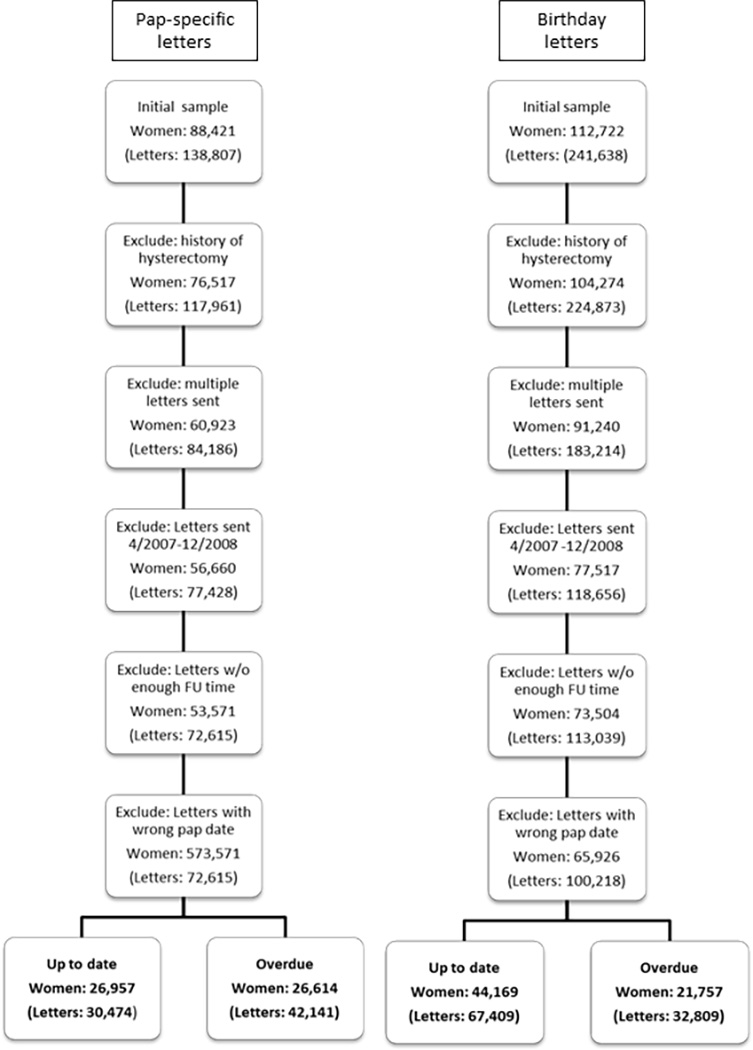
Figure 1 is a CONSORT-like diagram showing the number of women (and letters in parenthesis) in the initial sample and remaining after each exclusion criterion was applied. At the bottom of the figure are the final sample sizes of women (and letters) included by letter type and whether women were up-to-date or overdue for screening.
Reminder letters
Pap-specific letters were sent 27 months after a woman’s last Pap test if she was up-to- date with screening, regardless of the last test results. Pap-specific letters were sent yearly thereafter if a woman was overdue. The letter did not include the date of her last test or due date for her next test but said “it is time to schedule your routine Pap test”. The letter only reminded women about cervical cancer screening.
Birthday letters were sent annually, approximately two weeks before a woman’s birthday. If she was up-to-date with cervical cancer screening, the birthday letter included a reminder for cervical cancer screening with a future due date. Since due dates could be up to three years in the future, we only included letters that had a due date within the upcoming 12 months. If a woman was overdue for cervical cancer screening, the due date was replaced with the statement “due now”. The birthday letters could include anywhere from 1–7 recommendations for preventive services (services in addition to cervical cancer screening could include breast cancer screening, colorectal cancer screening, cholesterol maintenance tests [only among people with diabetes or cardiovascular disease], and 3 diabetes maintenance tests [HbA1c, microalbuminuria, and diabetic retinal exam]), all with different due dates.
Cervical cancer screening adherence
We hypothesized that current screening adherence would depend on past adherence.(17, 18) Therefore, we determined whether each woman was up-to-date or overdue for screening at the time each letter was sent using HEDIS definitions, accounting for changes in the definitions each year.(19) HEDIS is a tool used by U.S. health plans to measure performance on various aspects of healthcare and service. HEDIS definitions are maintained by the National Committee for Quality Assurance to ensure they are relevant and use current diagnostic and procedure codes. Based on HEDIS definitions, women were considered up-to-date if they had a Pap test in the previous 3 years; otherwise they were considered overdue.
We examined cervical cancer screening adherence using CPT, HCPCS, and ICD-9 Procedure codes from HEDIS(19) within a 6 month window around the due date in the letter as shown in Figure 2:
Women up-to-date with screening who received a letter with a due date >3 months in the future had to have a Pap test within the 3 months before or after her due date to be adherent (example (a))
Women up-to-date with screening who received a letter with a due date <3 months in the future had to have a Pap test within 6 months after receiving the letter to be adherent (example (b)).
Women who were overdue for a Pap test had to have a Pap test within 6 months of receiving the letter to be adherent (example (c)).
In this manner, all women had an equal window of time (6 months) to obtain cervical cancer screening.
Figure 2. Adherence definitions for screening based on timing of reminder letter and whether women were overdue for a Pap test.
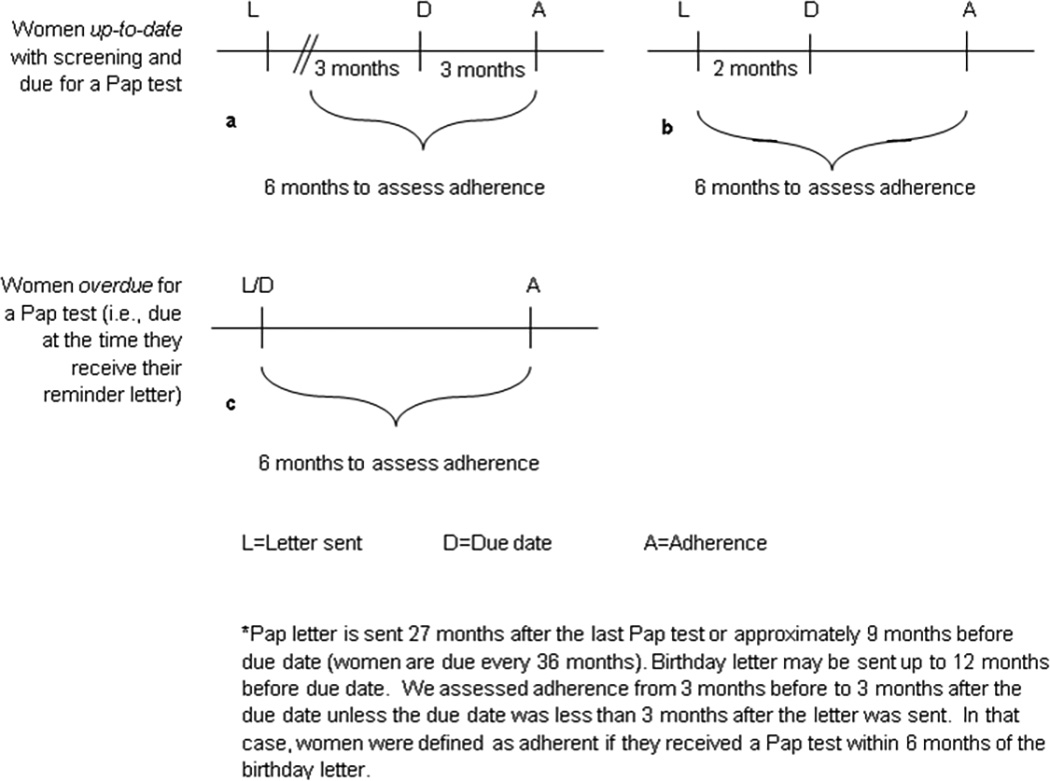
Figure 2 depicts the definitions we used for cervical cancer screening adherence by the timing of the reminder letter and by whether women were up-to-date with screening or overdue for a Pap test from 2003–2012 in Washington State. Each inset figure (a-c) shows that each group had a 6-month window around the test due date to be adherent.
Covariates
We used Group Health’s Virtual Data Warehouse,(20) which contains administrative, diagnostic, and procedure data for all Group Health enrollees, to obtain covariate data at the time each letter was sent.(21) Administrative and demographic covariates included age at letter receipt, race, education level, and body mass index (BMI in kg/m2). We calculated the Charlson comorbidity score using ICD-9 diagnosis codes from the 12 months before the letter was sent.(22) We used procedure data to count the number of primary care, preventive care, and OB/GYN visits in the 12 months prior to letter receipt. From the birthday letter only, we collected information on the number of recommendations included in the letter. We also examined elements of their insurance benefit including whether they had a preventive care waiver covering all preventive services in full, including Pap tests, and whether the person was enrolled in a plan with an annual deductible ≥$500.
Statistical analysis
All analyses were stratified by whether women were up-to-date or overdue for screening at the time they received each letter. We calculated unadjusted adherence rates with 95% confidence intervals (CIs) for each letter type overall, and each letter type stratified by covariates to determine whether any substantially modified adherence. Women could receive more than one letter over time (i.e. a Pap letter each time they were due or a birthday letter at each birthday); we used letters as the level of analysis. Therefore, we used logistic regression to account for repeated measures per woman to estimate adjusted odds ratios (with 95% CIs) for cervical cancer screening adherence following the birthday letter compared with the Pap letter. To understand whether the number of recommendations in the birthday letter impacted adherence, we categorized birthday letters into 3 groups in adjusted analyses: letters with 1–2 recommendations, letters with 3–5 recommendations, and letters with 6–7 recommendations. Each of these groups was compared to the Pap letter reference group. We adjusted models for age (continuous), ≥$500 deductible plan, preventive care waiver, Charlson score (0/1+), and number of healthcare visits in the 12 months prior to receiving the letter (0/1+, primary care, preventive care, and OBGYN visits were combined due to small numbers). Variables with substantial amounts of missing data (BMI, education, and race) were not included in the adjusted models; no other covariates included in the models had missing data. We ran models stratified by each covariate to evaluate whether any substantially modified the association between reminder letter type and adherence; in these models, we included all adjustment variables except the one used for stratification (for example, models stratified by high deductible plan were not adjusted for high deductible plan). Age was the exception – models stratified by age group were adjusted for age as a continuous variable. Last, we examined whether the due date on the birthday letter influenced adherence by plotting adherence rates by the number of months between the date the letter was mailed and the due date. For this analysis, we examined adherence for three years after receipt of the birthday letter, even though women would have received an additional birthday letter each year with a closer due date. All analyses were conducted using SAS (Cary, NC).
Results
Approximately 57% of letters were sent to women who were up-to-date with screening, and 43% were sent to women who were overdue (Table 1). The mean ages were 46.5 years for women up-to-date with screening and 45.7 years for women overdue for screening. The majority of our population was white with at least some college education. Women who were up-to-date tended to have lower BMIs, more preventive care visits, and more OB/GYN visits suggesting a slightly healthier population compared to overdue women. Women who received birthday letters were slightly more likely to have health plans with a deductible ≥$500 than women who received Pap letters, reflecting changes in health insurance options over time.
Table 1.
Characteristics of women eligible for cervical cancer screening by reminder letter type from 2003–2012 in Washington state*
| Up-to-date with screening N (Col %) |
Overdue for screening N (Col %) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Pap letter | Birthday letter | Pap letter | Birthday letter | |||||
| N=30,474 | N=67,409 | N=42,141 | N=32,809 | |||||
| Age | ||||||||
| 21–30 | 2445 | (8.0) | 7557 | (11.2) | 6208 | (14.7) | 5059 | (15.4) |
| 31–40 | 5606 | (18.4) | 13688 | (20.3) | 6656 | (15.8) | 4818 | (14.7) |
| 41–50 | 9570 | (31.4) | 17471 | (25.9) | 12755 | (30.3) | 7908 | (24.1) |
| 51–64 | 12853 | (42.2) | 28693 | (42.6) | 16522 | (39.2) | 15024 | (45.8) |
| Preventive care waiver | ||||||||
| Yes | 22348 | (73.3) | 52387 | (77.7) | 30327 | (72) | 28000 | (85.3) |
| No | 8126 | (26.7) | 15022 | (22.3) | 11814 | (28) | 4809 | (14.7) |
| Deductible ≥$500 annually | ||||||||
| Yes | 3210 | (10.5) | 10914 | (16.2) | 4576 | (10.9) | 7220 | (22) |
| No | 27264 | (89.5) | 56495 | (83.8) | 37565 | (89.1) | 25589 | (78) |
| Race | ||||||||
| Non-white | 4785 | (15.7) | 13242 | (19.6) | 6013 | (14.3) | 6015 | (18.3) |
| White | 22078 | (72.4) | 49257 | (73.1) | 25334 | (60.1) | 21481 | (65.5) |
| Unknown | 3611 | (11.8) | 4910 | (7.3) | 10794 | (25.6) | 5313 | (16.2) |
| Education | ||||||||
| <=High School | 2536 | (8.3) | 5374 | (8) | 2610 | (6.2) | 1703 | (5.2) |
| Some College | 6345 | (20.8) | 12912 | (19.2) | 5665 | (13.4) | 3911 | (11.9) |
| College Graduate | 4885 | (16) | 11452 | (17) | 3590 | (8.5) | 3053 | (9.3) |
| Post-College | 5466 | (17.9) | 11728 | (17.4) | 3520 | (8.4) | 2607 | (7.9) |
| Unknown | 11242 | (36.9) | 25943 | (38.5) | 26756 | (63.5) | 21535 | (65.6) |
| BMI in kg/m2 | ||||||||
| <25 | 9481 | (31.1) | 25807 | (38.3) | 7845 | (18.6) | 8937 | (27.2) |
| 25–29.9 | 6933 | (22.8) | 18896 | (28) | 6463 | (15.3) | 7078 | (21.6) |
| 30–34.9 | 3982 | (13.1) | 10967 | (16.3) | 4412 | (10.5) | 5049 | (15.4) |
| 35+ | 3978 | (13.1) | 10974 | (16.3) | 5329 | (12.6) | 6763 | (20.6) |
| Unknown | 6100 | (20.0) | 765 | (1.1) | 18092 | (42.9) | 4982 | (15.2) |
| Charlson score | ||||||||
| 0 | 26295 | (86.3) | 57293 | (85) | 36868 | (87.5) | 27950 | (85.2) |
| 1 | 2953 | (9.7) | 6824 | (10.1) | 3570 | (8.5) | 2996 | (9.1) |
| 2 | 868 | (2.8) | 2227 | (3.3) | 1176 | (2.8) | 1161 | (3.5) |
| 3+ | 358 | (1.2) | 1065 | (1.6) | 527 | (1.3) | 702 | (2.1) |
| # of primary care visits in past 12 months | ||||||||
| 0 | 9246 | (30.3) | 18275 | (27.1) | 19703 | (46.8) | 17286 | (52.7) |
| 1 | 7868 | (25.8) | 19320 | (28.7) | 9173 | (21.8) | 7562 | (23.0) |
| 2+ | 13360 | (43.8) | 29814 | (44.2) | 13265 | (31.5) | 7961 | (24.3) |
| # of preventive care visits in past 12 months | ||||||||
| 0 | 27665 | (90.8) | 52205 | (77.4) | 40979 | (97.2) | 31658 | (96.5) |
| 1+ | 2809 | (9.2) | 15204 | (22.6) | 1162 | (3.1) | 1151 | (3.5) |
| # of OBGYN visits in past 12 months | ||||||||
| 0 | 29604 | (97.1) | 60429 | (89.6) | 42057 | (99.8) | 32645 | (99.5) |
| 1+ | 870 | (2.8) | 6980 | (10.4) | 84 | (0.2) | 164 | (0.5) |
| Year letter received | ||||||||
| 2003 | 7118 | (23.4) | 6628 | (15.7) | ||||
| 2004 | 6049 | (19.8) | 13563 | (32.2) | ||||
| 2005 | 7012 | (23) | 11712 | (27.8) | ||||
| 2006 | 8772 | (28.8) | 9002 | (21.4) | ||||
| 2007 | 1523 | (5.0) | 1236 | (2.9) | ||||
| 2009 | 36724 | (54.5) | 6217 | (18.9) | ||||
| 2010 | 15731 | (23.3) | 6746 | (20.6) | ||||
| 2011 | 12981 | (19.3) | 13297 | (40.5) | ||||
| 2012 | 1973 | (2.9) | 6549 | (20.0) | ||||
| Number of services recommended in birthday letter | ||||||||
| 1–2 | 33984 | (50.4) | 15422 | (47.0) | ||||
| 3–5 | 30050 | (44.6) | 15212 | (46.4) | ||||
| 6–7 | 3375 | (5.0) | 2175 | (6.6) | ||||
p-values from Chi-square tests comparing characteristics between Pap letters and birthday letters were <0.0001 for every characteristic within both the up-to-date and overdue columns.
Among women who were up-to-date, unadjusted cervical cancer screening adherence was significantly higher following the Pap-specific compared with the birthday letter (Table 2, 46.8% vs 26.0%, respectively, p<0.001). Adherence following the birthday letter increased over time from 22.9% in 2009 to 44.6% in 2012, which was similar to adherence in the last year of the Pap-specific letter (47.2% in 2007). Among overdue women, adherence did not differ by type of letter (21.1% for Pap-specific reminder vs 21.6% for birthday reminder). Adherence following the birthday letter also increased overtime from 16.7% in 2009 to 24.4% in 2012.
Table 2.
Unadjusted adherence* to cervical cancer screening within 6 months of letter receipt by reminder letter type and patient characteristics from 2003–2012 in Washington state
| Up-to-date with screening | Overdue for screening | |||
|---|---|---|---|---|
| Pap letter | Birthday letter | Pap letter | Birthday letter | |
| Unadjusted adherence (95% CI) |
Unadjusted adherence (95% CI) |
Unadjusted adherence (95% CI) |
Unadjusted adherence (95% CI) |
|
| N=30,474 | N=67,409 | N=42,141 | N=32,809 | |
| Overall | 46.8 (46.3, 47.4) | 26.0 (25.7, 26.3) | 22.1 (21.7, 22.5) | 21.6 (21.2, 22.1) |
| Age | ||||
| 21–30 | 37.3 (35.4, 39.2) | 22.7 (21.8, 23.7) | 18.2 (17.3, 19.2) | 17.5 (16.5, 18.6) |
| 31–40 | 44.3 (43.0, 45.6) | 24.7 (24.0, 25.5) | 24.1 (23.0, 25.1) | 24.8 (23.6, 26.1) |
| 41–50 | 46.6 (45.6, 47.6) | 25.5 (24.8, 26.1) | 22.5 (21.8, 23.2) | 23.0 (22.0, 23.9) |
| 51–64 | 49.9 (49.1, 50.8) | 27.8 (27.3, 28.3) | 22.5 (21.8, 23.1) | 21.3 (20.6, 21.9) |
| Preventive care waiver | ||||
| Yes | 46.8 (46.1, 47.4) | 26.5 (26.1, 26.8) | 22.2 (21.7, 22.7) | 21.9 (21.4, 22.4) |
| No | 46.9 (45.8, 48.0) | 24.4 (23.7, 25.1) | 21.9 (21.1, 22.6) | 20.2 (19.1, 21.3) |
| Deductible ≥$500 annually | ||||
| Yes | 45.3 (43.6, 47.0) | 25.2 (24.4, 26.0) | 20.4 (19.2, 21.6) | 18.5 (17.6, 19.4) |
| No | 47.0 (46.4, 47.6) | 26.1 (25.8, 26.5) | 22.3 (21.9, 22.7) | 22.5 (22.0, 23.0) |
| Race | ||||
| Non-white | 47.3 (45.9, 48.7) | 26.5 (25.8, 27.3) | 25.5 (24.4, 26.6) | 23.9 (22.8, 25.0) |
| White | 49.0 (48.4, 49.7) | 27.2 (26.8, 27.6) | 25.5 (25.0, 26.1) | 24.5 (23.9, 25.0) |
| Unknown | 32.6 (31.1, 34.2) | 12.6 (11.7, 13.6) | 12.2 (11.6, 12.9) | 7.6 (6.9, 8.3) |
| Education | ||||
| <=High School | 46.1 (44.2, 48.1) | 25.9 (24.8, 27.1) | 28.5 (26.8, 30.2) | 26.2 (24.2, 28.3) |
| Some College | 47.9 (46.7, 49.1) | 26.4 (25.6, 27.2) | 30.3 (29.1, 31.5) | 31.1 (29.6, 32.5) |
| College Graduate | 54.4 (53.0, 55.8) | 28.5 (27.7, 29.3) | 36.7 (35.2, 38.3) | 35.1 (33.4, 36.8) |
| Post-College | 58.3 (57.0, 59.6) | 30.4 (29.6, 31.2) | 38.0 (36.4, 39.6) | 37.6 (35.7, 39.5) |
| Unknown | 37.5 (36.6, 38.4) | 22.7 (22.2, 23.2) | 15.7 (15.3, 16.1) | 15.7 (15.2, 16.2) |
| BMI (kg/m2) | ||||
| <25 | 54.5 (53.5, 55.5) | 27.1 (26.5, 27.6) | 32.9 (31.9, 34.0) | 26.5 (25.6, 27.4) |
| 25–29.9 | 50.2 (49.1, 51.4) | 27.0 (26.4, 27.6) | 31.0 (29.9, 32.1) | 27.3 (26.2, 28.3) |
| 30–34.9 | 46.8 (45.2, 48.3) | 25.2 (24.4, 26.0) | 26.2 (24.9, 27.5) | 23.0 (21.8, 24.2) |
| 35+ | 41.6 (40.1, 43.1) | 23.1 (22.4, 23.9) | 22.8 (21.7, 23.9) | 20.6 (19.7, 21.6) |
| Unknown | 34.3 (33.2, 35.5) | 17.6 (14.9, 20.4) | 13.0 (12.5, 13.5) | 4.9 (4.3, 5.5) |
| Charlson score | ||||
| 0 | 47.2 (46.6, 47.8) | 25.9 (25.6, 26.3) | 22.2 (21.8, 22.6) | 21.4 (20.9, 21.9) |
| 1+ | 44.6 (43.0, 46.1) | 26.4 (25.5, 27.3) | 21.3 (20.2, 22.4) | 23.1 (21.9, 24.3) |
| # healthcare visits in past 12 months | ||||
| 0 | 46.4 (45.3, 47.4) | 25.7 (25.1, 26.4) | 17.6 (17.1, 18.2) | 18.3 (17.7, 18.8) |
| 1 | 47.0 (46.3, 47.7) | 26.1 (25.7, 26.5) | 26.0 (25.4, 26.6) | 25.4 (24.7, 26.0) |
| Year letter received | ||||
| 2003 | 43.9 (42.7, 45.1) | 16.4 (15.5, 17.3) | ||
| 2004 | 46.5 (45.2, 47.7) | 25.3 (24.6, 26.1) | ||
| 2005 | 46.7 (45.5, 47.9) | 21.2 (20.5, 22.0) | ||
| 2006 | 49.4 (48.4, 50.5) | 21.3 (20.4, 22.1) | ||
| 2007 | 47.2 (44.7, 49.7) | 32.0 (29.4, 34.6) | ||
| 2009 | 22.9 (22.5, 23.4) | 16.7 (15.8, 17.6) | ||
| 2010 | 25.9 (25.2, 26.6) | 19.6 (18.6, 20.5) | ||
| 2011 | 32.0 (31.2, 32.8) | 23.6 (22.9, 24.3) | ||
| 2012 | 44.6 (42.4, 46.8) | 24.4 (23.4, 25.5) | ||
| Number of services recommended in birthday letter | ||||
| 1–2 | 24.6 (24.2, 25.1) | 21.9 (21.3, 22.6) | ||
| 3–5 | 27.8 (27.3, 28.3) | 21.4 (20.7, 22.0) | ||
| 6–7 | 23.9 (22.5, 25.4) | 21.2 (19.5, 22.9) | ||
Adherence defined using CPT codes, HCPCS, and ICD-9 codes found within the 6 month window around the due date in the reminder letter.
After adjustment, adherence was still significantly worse among up-to-date women following the birthday letter compared with the Pap letter whether the birthday letter had 1–2 recommendations (OR=0.37, 95%CI=0.36–0.39), 3–5 recommendations (OR=0.44, 95%CI=0.42–0.45), or 6–7 recommendations (OR=0.36, 95%CI=0.32–0.40) (Table 3). Adherence for up-to-date women varied slightly when stratified by patient characteristics. Among overdue women, adjusted adherence did not differ by letter type whether the birthday letter had 1–2 recommendations (OR=0.99, 95%CI=0.95–1.04), 3–5 recommendations (OR=0.96, 95%CI=0.91–1.00), or 6–7 recommendations (OR=0.95, 95%CI=0.85–1.06). However, adherence was slightly worse for the birthday letters with 1–2 recommendations compared to the Pap letter when limiting to women with a high-deductible health plan (OR=0.88, 95%CI=0.79–0.99), and slightly better among women with a Charlson score of 1 or higher (OR=1.17, 95%CI=0.99–1.38 for letters with 1–2 recommendations and OR=1.20, 95%CI=1.06–1.35 for 3–5 recommendations).
Table 3.
Adjusted* odds of cervical cancer screening adherence after receiving a birthday letter compared to a Pap-specific letter, stratified by up-to-date and overdue status, and by risk factors from 2003–2012 in Washington state.
| Number of prevention recommendations in the birthday letter | ||||||
|---|---|---|---|---|---|---|
| 1–2 recommendations | 3–5 recommendations | 6–7 recommendations | ||||
| OR* | 95% CI | OR* | 95% CI | OR* | 95% CI | |
| Up-to-date women: Overall results | ||||||
| N=33,984 | N=30,050 | N=3,375 | ||||
| Pap-specific letter N=30,474 (reference) |
1.00 | 1.00 | 1.00 | |||
| Birthday letter | 0.37 | (0.36, 0.39) | 0.44 | (0.42, 0.45) | 0.36 | (0.32, 0.40) |
| Stratified by group (reference=Pap-specific letter for each model)** | ||||||
| Age: 21–30 | 0.49 | (0.44, 0.55) | 0.69 | (0.37, 1.27) | 1.68 | (0.11, 26.91) |
| Age: 31–40 | 0.42 | (0.39, 0.45) | 0.33 | (0.23, 0.48) | 0.31 | (0.19, 0.52) |
| Age: 41–50 | 0.39 | (0.37, 0.42) | 0.41 | (0.38, 0.45) | 0.33 | (0.27, 0.42) |
| Age: 51–64 | 0.52 | (0.38, 0.70) | 0.39 | (0.37, 0.41) | 0.33 | (0.29, 0.37) |
| Preventive care waiver: Yes | 0.38 | (0.36, 0.40) | 0.45 | (0.43, 0.47) | 0.37 | (0.33, 0.41) |
| Preventive care waiver: No | 0.35 | (0.32, 0.37) | 0.40 | (0.37, 0.43) | 0.33 | (0.26, 0.41) |
| Deductible ≥$500: Yes | 0.36 | (0.32, 0.40) | 0.47 | (0.42, 0.52) | 0.40 | (0.30, 0.54) |
| Deductible ≥$500: No | 0.38 | (0.36, 0.39) | 0.43 | (0.42, 0.45) | 0.35 | (0.32, 0.40) |
| Charlson score: 1+ | 0.42 | (0.38, 0.47) | 0.51 | (0.46, 0.56) | 0.39 | (0.35, 0.44) |
| Charlson score: 0 | 0.37 | (0.35, 0.38) | 0.43 | (0.41, 0.45) | 0.34 | (0.24, 0.46) |
| 1+ healthcare visit: Yes | 0.37 | (0.35, 0.38) | 0.44 | (0.42, 0.46) | 0.36 | (0.32, 0.40) |
| 1+ healthcare visit: No | 0.38 | (0.36, 0.41) | 0.44 | (0.41, 0.47) | 0.31 | (0.23, 0.42) |
| Overdue women: Overall results | ||||||
| N=15,422 | N=15,212 | N=2,175 | ||||
| Pap-specific letter N=42,141 (reference) |
1.00 | 1.00 | 1.00 | |||
| Birthday letter | 0.99 | (0.95, 1.04) | 0.96 | (0.91, 1.00) | 0.95 | (0.85, 1.06) |
| Stratified by group (reference=Pap-specific letter for each model)** | ||||||
| Age: 21–30 | 0.95 | (0.86, 1.05) | 0.75 | (0.33, 1.72) | 0.75 | (0.33, 1.72) |
| Age: 31–40 | 1.06 | (0.97, 1.15) | 0.66 | (0.40, 1.07) | 1.02 | (0.51, 2.05) |
| Age: 41–50 | 1.04 | (0.96, 1.13) | 1.00 | (0.89, 1.13) | 0.99 | (0.78, 1.25) |
| Age: 51–64 | 1.24 | (0.82, 1.87) | 0.93 | (0.88, 0.99) | 0.91 | (0.80, 1.03) |
| Preventive care waiver: Yes | 1.00 | (0.95, 1.05) | 0.97 | (0.92, 1.02) | 0.97 | (0.86, 1.09) |
| Preventive care waiver: No | 0.94 | (0.85, 1.05) | 0.87 | (0.77, 0.99) | 0.83 | (0.61, 1.12) |
| Deductible ≥$500: Yes | 0.88 | (0.79, 0.99) | 0.91 | (0.81, 1.02) | 0.80 | (0.59, 1.08) |
| Deductible ≥$500: No | 1.04 | (0.99, 1.10) | 0.99 | (0.94, 1.04) | 0.98 | (0.87, 1.10) |
| Charlson score: 1+ | 1.17 | (0.99, 1.38) | 1.20 | (1.06, 1.35) | 0.99 | (0.87, 1.13) |
| Charlson score: 0 | 0.98 | (0.93, 1.02) | 0.93 | (0.88, 0.97) | 0.97 | (0.72, 1.31) |
| 1+ healthcare visit: Yes | 0.98 | (0.92, 1.04) | 1.00 | (0.94, 1.07) | 0.80 | (0.70, 0.90) |
| 1+ healthcare visit: No | 1.10 | (1.03, 1.17) | 0.99 | (0.92, 1.06) | 1.08 | (0.85, 1.38) |
Adjusted for age, ≥$500 deductible plan, preventive care waiver, Charlson score, and number of healthcare visits in the 12 months prior to receiving the letter.
The reference for each stratified model is the Pap-specific letter for the same group. For example, the row “Age: 21–30” compares the birthday letter to the Pap-specific letter among women aged 21–30 only. The row “Age: 31–40” compares the birthday letter to the Pap-specific letter among women aged 31–40 only.
Adherence to screening following the birthday letter was related to the amount of time between when the birthday letter was sent and a woman’s due date (Figure 3). For example, 8.3% of women due at the time they received their letter had a Pap test right away; an additional 12.2% had a Pap test within 1 month of receiving the letter. Among women due within 1–6 months of receiving their letter, 7.3% had a Pap test within 1 month, 8.1% within 1–2 months, 6.8% within 2–3 months, 7.0% within 3–4, months, 5.8% within 4–5 months, and 5.1% within 5–6 months for a total of 40% . Many women received screening outside of their due date window. Approximately 24% percent of women due within 7–12 months of receiving their birthday letter came in before 7 months, whereas 26% came in within 7–12 months. Women who were overdue were less likely to come in for a Pap test at any point in time after receiving the birthday letter.
Figure 3. Percent of women who received a Pap test within 36 months after receiving their birthday letter, according to their due dates.
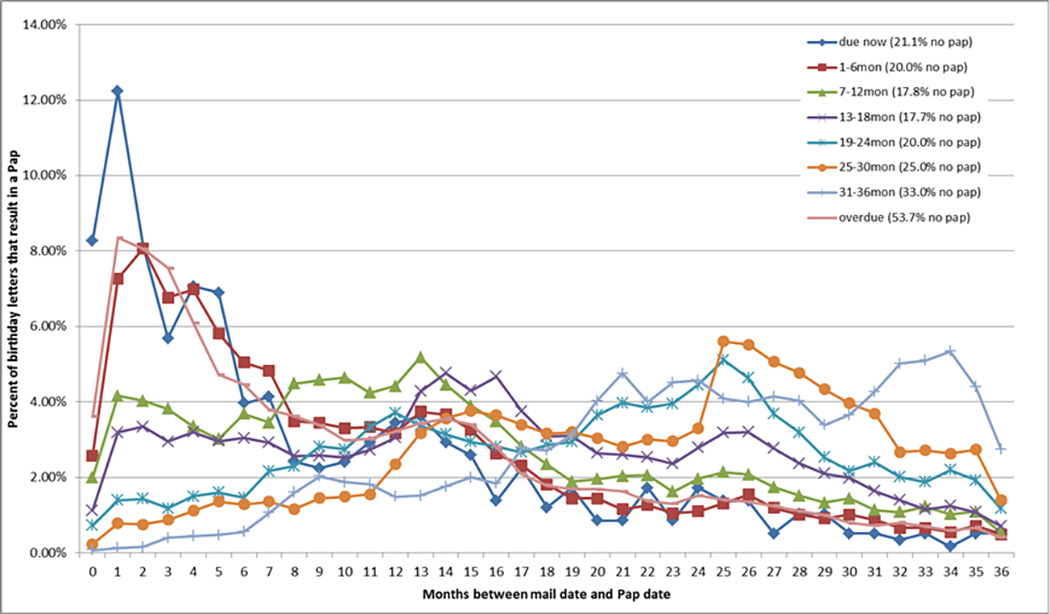
Figure 3 applies to birthday letters only. It depicts the percent of women who received a Pap test within 3 years after receiving their birthday letter over time from 2009–2012 in Washington State. Each line represents a different group depending on when women were due. The first blue line represents women who were due now (within 1 month of receiving the letter) and shows the percent of women who received a subsequent Pap test peaked a 1 month and trailed off thereafter. The numbers in parentheses in the legend show that 21.1% of women who were “due now” did not have a Pap test within 36 months of receiving their letter. The red line represents women who were due between 1–6 months after receiving their letter, and the percent of women who came in after receiving their letter peaked at 2 months. Percents declined thereafter but women due 1–6 months after receiving their letter had Pap tests throughout the 36 months depicted in the figure. The green line shows that women due within 7–12 months after receiving their letter peaked at 13 months – but many came in for a Pap test before and after that time. The pink line represents the percent of women overdue for a Pap test at the time they received their letter. The percent of overdue women who received a Pap test peaked at 1 month following the letter and sharply declined thereafter with 53.7% of these women not receiving a Pap test within 36 months.
Conclusions
Group Health’s birthday letter was implemented to facilitate a whole-person, patient-centered approach to prevention by including multiple reminders in a single letter; but it was not as clinically effective as a targeted, single-service reminder in promoting Pap test adherence. In evaluating adherence following each letter, it is important to note the differences between the letters in terms of purpose, timing, and recommendations. The Pap-specific letter only included a reminder for a Pap test due in the near future; whereas, the birthday letter contained multiple preventive reminders, including a Pap test reminder, which may not have been due for up to 12 months in the future. Importantly, the number of recommendations in the birthday letter did not adversely impact Pap screening rates. It is possible that adherence to other preventive services increased following the birthday letter, but we could not evaluate this in our study. Increased adherence to other services could improve overall prevention increasing the value of the birthday letter, even if cervical cancer adherence decreased, because it fits with the whole-person approach to prevention and eliminates the need for a separate reminder letter for each test.
We cannot definitively conclude why the birthday letters resulted in lower adherence compared to the Pap letters among up-to-date women, because the letters were mailed as a natural experiment without a true control group comparison. However, we can hypothesize potential reasons for the differences in adherence rates. The timing of these letters is one possible explanation – the Pap-specific letters were sent just before a woman was due whereas the birthday letters were sent up to a year before a woman was due. This explanation is consistent with our observation that women came in early for their Pap test when they received their birthday letter. Consistent with prior literature, women who regularly come in for screening may also be in the habit of doing so, and would come in whether they received a reminder letter or not.(23–26) Additionally, we may have observed a learning effect in our population for the birthday letter. Screening adherence following the birthday letter was 22.9% in 2009, but increased to 44.6% in 2012. As with most changes in clinical practice, it takes time for both patients and providers to get used to new ideas and methods.(27–31)
Neither letter was very effective among women overdue for cervical cancer screening. This highlights an important public health issue of effectively encouraging overdue women to come in for cervical cancer screening. The lack of effectiveness of reminders on women overdue for cervical cancer screening has been demonstrated in previous studies.(15) Women who are overdue for screening are more likely to have cancer detected at a later stage because they do not seek care until they are symptomatic.(32–34) Adherence in overdue women in our study was slightly higher among women with a Charlson score of 1 or more following the birthday letter compared to the Pap-specific letter. It is possible that these women had comorbidities that required them to seek healthcare more often, and additional healthcare visits provided convenient opportunities for a Pap test. Overdue women with an annual deductible ≥$500 or no preventive care waiver were less likely to be adherent following the birthday letter compared to the Pap-specific letter; these results suggest cost of care could have been a barrier to screening, consistent with other screening studies.(35, 36)
Our results also demonstrate that even with preventive care coverage, innovative methods are needed to encourage women who are overdue for cervical cancer testing to obtain screening in a timely manner. Studies have explored text messages, electronic medical record prompts, and web-based campaigns (e.g. social media) to promote cancer screening;(37, 38) although the practicality of these methods are limited by Health Insurance Portability and Accountability Act restrictions to prevent unintentional disclosures of identifiable health information.(39–42) Approaches beyond reminders and education, such as navigators and other strategies to increase convenience of testing may be necessary to increase screening participation in overdue women.(43–45)
Overall, our Pap test adherence results were lower than in other studies because we calculated adherence differently than other commonly used methods such as HEDIS.(19) Our approach resulted in lower screening adherence rates than other studies because our window for adherence was only six months; whereas HEDIS calculates adherence over three years. Therefore, adherence rates in our analysis should not be directly compared to HEDIS or other studies that evaluated adherence over longer time periods.
Our study has several additional limitations. First, we did not have a true control group. We conducted this evaluation using data from a natural experiment. Second, we could not evaluate overuse of cervical cancer screening. Overuse is an important issue in cervical cancer screening because women tend to be screened more often than current guidelines recommend.(46, 47) We did not have enough follow-up time to study overuse given the years of our data (2003–2012). Third, one reminder letter was phased in as the other was phased out; therefore, we could not compare the two letters during the same time period. Instead, we took advantage of a natural experiment when a health plan changed reminder systems. If adherence changed over time in our population regardless of the letter, our results may have been affected. However, Pap test adherence rates at GH during the later years of our study were fairly constant and similar to adherence rates in the surrounding community,(48) suggesting changes over time had little impact on our results. Fourth, we could not account for other interventions at GH that may have contributed to the increase in Pap test adherence following the birthday letter. For example, clinics implemented electronic medical record reports to highlight women overdue for screening tests and contact them directly. These types of interventions occur regularly at GH and other organizations to increase and maintain cancer-screening adherence. These were not recorded systematically and we have no way of knowing which patients received additional interventions. Nonetheless, this natural experiment could also increase the generalizability and applicability of our results to other community practices because the letters were sent as part of clinical care, not as part of a controlled trial. Finally, our use of deductibles and preventive care waivers as measures of out-of-pocket costs and access to care may be considered crude assessments of these potential barriers to screening. Obtaining information on the cost of care at any given point in time for an individual is nearly impossible given one has to take into account what a person has already paid in terms of premiums, co-pays, co-insurance, and deductibles. However, we were able to eliminate a complete lack of health insurance as a barrier to screening in our population, because all of our study participants had some level of healthcare.
In conclusion, a single reminder letter with multiple preventive services sent around the time of a person’s birthday and not timed to due dates was not as effective for cervical cancer screening as a reminder letter tied to one specific screening service sent just before a woman is due. While it had a patient-centered focus by using a whole-person approach to prevention, it did not initially result in similar adherence to Pap testing compared with the Pap-specific reminder letter. This study should have relevance for other health plans and organizations looking to adopt new or modify current preventive reminder systems - it appears an appropriately timed, test-specific letter is more effective in promoting appropriate screening adherence compared to an annual, multi-service reminder letter.
Acknowledgments
We acknowledge the assistance of Arika Wieneke in reviewing the literature on this topic. This study was funded by the American Cancer Society RSGI-11-100-01-CPHPS (PI D. Buist), and the National Cancer Institute U01CA63731 (PI D. Buist). The funding sources had no involvement in the study design; collection, analysis, and interpretation of data; writing of the report; or the decision to submit the article for publication.
Footnotes
Conflict of interest statement
The authors declare that there are no conflicts of interest
References
- 1.Improving Quality and Patient Experience: The State of Health Care Quality 2013. National Committee for Quality Assurance. 2013
- 2.Coronado G, Petrik A, Spofford M, et al. Perceptions of Under and Overutilization of Cervical Cancer Screening Services at Latino-Serving Community Health Centers. J Commun Health. 2013;38(5):915–918. doi: 10.1007/s10900-013-9701-1. [DOI] [PubMed] [Google Scholar]
- 3.Korenstein D, Falk R, Howell EA, et al. Overuse of health care services in the United States: an understudied problem. Arch Intern Med. 2012;172(2):171–178. doi: 10.1001/archinternmed.2011.772. Epub 2012/01/25. [DOI] [PubMed] [Google Scholar]
- 4.Almeida CM, Rodriguez MA, Skootsky S, et al. Cervical Cancer Screening Overuse and Underuse: Patient and Physician Factors. Am J Manag Care. 2013;19(6):482–489. Epub 2013/07/13. [PubMed] [Google Scholar]
- 5.Moyer VA. Screening for Cervical Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2012;156(12):880–891. doi: 10.7326/0003-4819-156-12-201206190-00424. Epub 15 March 2012. [DOI] [PubMed] [Google Scholar]
- 6.ACOG Practice Bulletin no. 109: Cervical cytology screening. Obstet Gynecol. 2009;114(6):1409–1420. doi: 10.1097/AOG.0b013e3181c6f8a4. [DOI] [PubMed] [Google Scholar]
- 7.Everett T, Bryant A, Griffin MF, et al. Interventions targeted at women to encourage the uptake of cervical screening. The Cochrane database of systematic reviews. 2011;(5):CD002834. doi: 10.1002/14651858.CD002834.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jean S, Major D, Rochette L, et al. Screening mammography participation and invitational strategy: the Quebec Breast Cancer Screening Program, 1998–2000. Chronic Dis Can. 2005;26(2–3):52–58. Epub 2005/10/28. [PubMed] [Google Scholar]
- 9.Saywell RM, Jr, Champion VL, Skinner CS, et al. A cost-effectiveness comparison of three tailored interventions to increase mammography screening. J Womens Health (Larchmt) 2004;13(8):909–918. doi: 10.1089/jwh.2004.13.909. Epub 2005/01/27. [DOI] [PubMed] [Google Scholar]
- 10.Romaire MA, Bowles EJ, Anderson ML, et al. Comparative effectiveness of mailed reminder letters on mammography screening compliance. Prev Med. 2012 doi: 10.1016/j.ypmed.2012.05.009. Epub 2012/05/26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaczorowski J, Karwalajtys T, Lohfeld L, et al. Women's views on reminder letters for screening mammography: Mixed methods study of women from 23 family health networks. Canadian family physician Medecin de famille canadien. 2009;55(6):622–623. e1-4. [PMC free article] [PubMed] [Google Scholar]
- 12.Cronin P, Goodall S, Lockett T, et al. Cost-effectiveness of an advance notification letter to increase colorectal cancer screening. Int J Technol Assess. 2013;29(3):261–268. doi: 10.1017/S0266462313000226. [DOI] [PubMed] [Google Scholar]
- 13.van Roon AH, Hol L, Wilschut JA, et al. Advance notification letters increase adherence in colorectal cancer screening: a population-based randomized trial. Prev Med. 2011;52(6):448–451. doi: 10.1016/j.ypmed.2011.01.032. [DOI] [PubMed] [Google Scholar]
- 14.Virtanen A, Anttila A, Luostarinen T, et al. Improving cervical cancer screening attendance in Finland. Int J Cancer. 2014 doi: 10.1002/ijc.29176. [DOI] [PubMed] [Google Scholar]
- 15.MacLaughlin KL, Swanson KM, Naessens JM, et al. Cervical cancer screening: a prospective cohort study of the effects of historical patient compliance and a population-based informatics prompted reminder on screening rates. J Eval Clin Pract. 2014;20(2):136–143. doi: 10.1111/jep.12098. [DOI] [PubMed] [Google Scholar]
- 16.Forbes C, Jepson R, Martin-Hirsch P. Interventions targeted at women to encourage the uptake of cervical screening. Cochrane Database Syst Rev. 2002;(3):CD002834. doi: 10.1002/14651858.CD002834. Epub 2002/07/26. [DOI] [PubMed] [Google Scholar]
- 17.Wirth MD, Brandt HM, Dolinger H, et al. Examining connections between screening for breast, cervical and prostate cancer and colorectal cancer screening. Colorectal Cancer. 2014;3(3):253–263. doi: 10.2217/crc.14.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murphy CC, Vernon SW, Haddock NM, et al. Longitudinal predictors of colorectal cancer screening among participants in a randomized controlled trial. Prev Med. 2014;66:123–130. doi: 10.1016/j.ypmed.2014.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. [cited 2014 November 7];Healthcare Effectiveness Data and Information Set (HEDIS) Available at: http://www.ncqa.org/HEDISQualityMeasurement.aspx.
- 20.Ross TR, Ng D, Brown JS, et al. The HMO Research Network Virtual Data Warehouse: A Public Model to Support Collboration. eGEMs. 2014;2(1) doi: 10.13063/2327-9214.1049. Article 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hornbrook MC, Hart G, Ellis JL, et al. Building a virtual cancer research organization. J Natl Cancer Inst Monogr. 2005;(35):12–25. doi: 10.1093/jncimonographs/lgi033. [DOI] [PubMed] [Google Scholar]
- 22.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. Epub 1987/01/01. [DOI] [PubMed] [Google Scholar]
- 23.Seeff LC, Nadel MR, Klabunde CN, et al. Patterns and predictors of colorectal cancer test use in the adult U.S. population. Cancer. 2004;100(10):2093–2103. doi: 10.1002/cncr.20276. [DOI] [PubMed] [Google Scholar]
- 24.Shapiro JA, Seeff LC, Nadel MR. Colorectal cancer-screening tests and associated health behaviors. Am J Prev Med. 2001;21(2):132–137. doi: 10.1016/s0749-3797(01)00329-4. [DOI] [PubMed] [Google Scholar]
- 25.Meissner HI, Yabroff KR, Dodd KW, et al. Are patterns of health behavior associated with cancer screening? Am J Health Promot. 2009;23(3):168–175. doi: 10.4278/ajhp.07082085. [DOI] [PubMed] [Google Scholar]
- 26.Blackwell DL, Martinez ME, Gentleman JF. Women's compliance with public health guidelines for mammograms and pap tests in Canada and the United States: an analysis of data from the Joint Canada/United States Survey Of Health. Women Health Iss. 2008;18(2):85–99. doi: 10.1016/j.whi.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 27.Pace LE, He Y, Keating NL. Trends in mammography screening rates after publication of the 2009 US Preventive Services Task Force recommendations. Cancer. 2013;119(14):2518–2523. doi: 10.1002/cncr.28105. [DOI] [PubMed] [Google Scholar]
- 28.Corbelli J, Borrero S, Bonnema R, et al. Differences among primary care physicians' adherence to 2009 ACOG guidelines for cervical cancer screening. J Womens Health. 2014;23(5):397–403. doi: 10.1089/jwh.2013.4475. Epub 2014/01/02. [DOI] [PubMed] [Google Scholar]
- 29.Corbelli J, Borrero S, Bonnema R, et al. Physician adherence to U.S. Preventive Services Task Force mammography guidelines. Women Health Iss. 2014;24(3):e313–e319. doi: 10.1016/j.whi.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 30.Saraiya M, Berkowitz Z, Yabroff KR, et al. Cervical cancer screening with both human papillomavirus and Papanicolaou testing vs Papanicolaou testing alone: what screening intervals are physicians recommending? Arch Int Med. 2010;170(11):977–985. doi: 10.1001/archinternmed.2010.134. [DOI] [PubMed] [Google Scholar]
- 31.Cuzick J, Myers O, Hunt WC, et al. A population-based evaluation of cervical screening in the United States: 2008–2011. Cancer Epidem Biomar. 2014;23(5):765–773. doi: 10.1158/1055-9965.EPI-13-0973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aarts MJ, Voogd AC, Duijm LE, et al. Socioeconomic inequalities in attending the mass screening for breast cancer in the south of the Netherlands--associations with stage at diagnosis and survival. Breast Cancer Res. 2011;128(2):517–525. doi: 10.1007/s10549-011-1363-z. [DOI] [PubMed] [Google Scholar]
- 33.Kamineni A, Weinmann S, Shy KK, et al. Efficacy of screening in preventing cervical cancer among older women. Cancer Cause Control. 2013;24(9):1653–1660. doi: 10.1007/s10552-013-0239-4. [DOI] [PubMed] [Google Scholar]
- 34.Leyden WA, Manos MM, Geiger AM, et al. Cervical cancer in women with comprehensive health care access: attributable factors in the screening process. J Natl Cancer Inst. 2005;97(9):675–683. doi: 10.1093/jnci/dji115. [DOI] [PubMed] [Google Scholar]
- 35.Stanley SL, Thomas CC, King JB, et al. Predictors of never being screened for cervical cancer by metropolitan area. J Comm Health. 2014;39(2):400–408. doi: 10.1007/s10900-013-9778-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen HY, Kessler CL, Mori N, et al. Cervical cancer screening in the United States, 1993–2010: characteristics of women who are never screened. J Womens Health (2002) 2012;21(11):1132–1138. doi: 10.1089/jwh.2011.3418. [DOI] [PubMed] [Google Scholar]
- 37.Lee HY, Koopmeiners JS, Rhee TG, et al. Mobile phone text messaging intervention for cervical cancer screening: changes in knowledge and behavior pre-post intervention. J Med Internet Res. 2014;16(8):e196. doi: 10.2196/jmir.3576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.White P, Kenton K. Use of electronic medical record-based tools to improve compliance with cervical cancer screening guidelines: effect of an educational intervention on physicians' practice patterns. J Low Genit Tract Dis. 2013;17(2):175–181. doi: 10.1097/LGT.0b013e3182607137. [DOI] [PubMed] [Google Scholar]
- 39.Weinberg DS, Keenan E, Ruth K, et al. A randomized comparison of print and web communication on colorectal cancer screening. JAMA Intern Med. 2013;173(2):122–129. doi: 10.1001/2013.jamainternmed.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vernon SW, Bartholomew LK, McQueen A, et al. A randomized controlled trial of a tailored interactive computer-delivered intervention to promote colorectal cancer screening: sometimes more is just the same. Ann Behav Med. 2011;41(3):284–299. doi: 10.1007/s12160-010-9258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yabroff KR, Zapka J, Klabunde CN, et al. Systems strategies to support cancer screening in U.S. primary care practice. Cancer Epidem Biomar. 2011;20(12):2471–2479. doi: 10.1158/1055-9965.EPI-11-0783. Epub 2011/10/07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cutrona SL, Roblin DW, Wagner JL, et al. Adult Willingness to Use Email and Social Media for Peer-to-Peer Cancer Screening Communication: Quantitative Interview Study. JMIR Res Protoc. 2013;2(2):e52. doi: 10.2196/resprot.2886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Drake BF, Tannan S, Anwuri VV, et al. A Community-Based Partnership to Successfully Implement and Maintain a Breast Health Navigation Program. J Comm Health. 2015 doi: 10.1007/s10900-015-0051-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sultana F, Mullins R, Murphy M, et al. Women's views on human papillomavirus self-sampling: focus groups to assess acceptability, invitation letters and a test kit in the Australian setting. Sex Health. 2015;12(4):279–286. doi: 10.1071/SH14236. [DOI] [PubMed] [Google Scholar]
- 45.Khaliq W, Howell EE, Wright SM. What do hospitalists think about inpatient mammography for hospitalized women who are overdue for their breast cancer screening? J Hosp Med. 2015;10(4):242–245. doi: 10.1002/jhm.2322. [DOI] [PubMed] [Google Scholar]
- 46.Kepka D, Breen N, King JB, et al. Demographic factors associated with overuse of pap testing. Am J Prev Med. 2014;47(5):629–633. doi: 10.1016/j.amepre.2014.07.034. [DOI] [PubMed] [Google Scholar]
- 47.Roland KB, Benard VB, Soman A, et al. Cervical cancer screening among young adult women in the United States. Cancer Epidel Biomar. 2013;22(4):580–588. doi: 10.1158/1055-9965.EPI-12-1266. Epub 2013/01/29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. [January 21, 2015];Washington Health Alliance. Available at: http://wahealthalliance.org/


