Abstract
Even after successful weight restoration, many patients with anorexia nervosa (AN) continue to exhibit maladaptive eating including repetitive behaviors (i.e., food rituals) used to decrease anxiety about food, and to describe fears related to food content its effect on shape and weight. While there are important differences between eating disorders and anxiety disorders, the shared clinical phenomena suggest potentially useful overlap in treatment strategies. This case study will describe treatment of a woman with AN using Exposure and Response Prevention for Anorexia Nervosa (AN-EXRP) as an adjunct to concurrent inpatient treatment. This is a novel use of a treatment approach with established efficacy in the treatment of anxiety disorders. AN-EXRP specifically targets eating-related anxiety with the intent to improve the restrictive eating patterns that persist after acute weight restoration. The case study described includes descriptions of (1) the treatment rationale and its phases of implementation, (2) illustrative sample dialogue between the patient and therapist, (3) pre- and post-treatment data on outcome measures of interest (e.g., food intake at a laboratory meal, self-report anxiety ratings, self-report eating-related rituals and preoccupations), and (4) therapist considerations (e.g., maintaining alliance, adhering to treatment frame).
Several lines of evidence support links between anorexia nervosa (AN) and anxiety. Anxiety disorders commonly precede the onset of AN (Bulik, Sullivan, Fear, & Joyce, 1997), and individuals with AN manifest high levels of anxiety, even following weight restoration (e.g., Pollice, Kaye, Greeno, & Weltzin, 1997). More specifically, individuals with AN describe fears related to food (e.g., Sunday, Halmi, & Einhorn, 1995), including anxiety in anticipation of eating, concern about food contents, and fear of food’s effect on shape and weight. They manifest repetitive behaviors (i.e., food rituals) used to decrease anxiety about food, which bear strong similarities to obsessive compulsive disorder (e.g., Hsu, Kaye, & Weltzin, 1993). While there are important differences between eating disorders (EDs) and anxiety disorders, the shared clinical phenomena suggest potentially useful overlap in treatment strategies (Steinglass et al., 2011).
The existing data indicate that even after successful weight restoration, many patients with AN continue to exhibit maladaptive eating. For example, they continue to eat significantly fewer calories and less fat than healthy peers even after a return to healthy weight (Mayer, Schebendach, Bodell, Shingleton, & Walsh, 2012; Sysko, Walsh, Schebendach, & Wilson, 2005). Weight-restored individuals with AN who eat a diet low in variety and low in energy density are significantly more likely to have a poor long-term course post-hospitalization (e.g., Schebendach et al., 2012).
Exposure and Response Prevention for Anorexia Nervosa (AN-EXRP) is a novel treatment approach that specifically targets eating-related anxiety with the intent to improve the restrictive eating patterns that persist after acute weight restoration. This case study will describe treatment of a woman with AN using AN-EXRP as an adjunct to concurrent inpatient treatment. AN-EXRP was developed using techniques with established efficacy in the treatment of anxiety disorders (e.g., Goldfarb, Fuhr, Tsujimoto, & Fischman, 1987; Kozak & Foa, 1997). The case1 was selected from a randomized controlled trial of AN-EXRP (see Steinglass et al., 2014). Prior to the start of therapy, the patient provided written informed consent to participate in the study, including consent for video recording of therapy sessions. Prior to the publication of this case, she signed a separate informed consent for her data and session content to be published individually. Her name and identifying information have been changed to protect her confidentiality.
The goal of AN-EXRP is to activate eating-related fears through exposure in the absence of anxiety-reducing rituals. Unlike standard CBT for EDs, AN-EXRP relies primarily on the behavioral techniques of exposure and response prevention to address anxiety about eating. Exposure sessions push beyond the practice of “normal” or “regular” eating and, at times, introduce elements of uncertainty (as uncertainty is typically feared), to induce high levels of anxiety around feared situations. Exposures are initiated gradually to establish alliance, build self-efficacy, and foster confidence in the treatment approach.
Emily
Emily was a 21 year old nursing student who lived with her parents at the time of her hospitalization. Per her recollection, her history of AN dated from age 15, when she began dieting and exercising regularly to deal with “stress” and develop an “identity” within her family. This routine became rigid and excessive, and her weight decreased. She began binge eating and vomiting at age 16 and her first hospital admission was that year. Emily was hospitalized several times in high school and early adulthood, repeatedly gaining weight in the structured setting and relapsing following discharge. Prior to the current episode, she had a year of relative recovery, with Body Mass Index (BMI) =19.1 kg/m2, regular menses, and restrictive intake without compensatory behaviors. BMI provides a measure of weight standardized for height. According to Centers for Disease Control (CDC) standards, a BMI between 18.5 kg/m2 and 24 kg/m2 is in the normal range. The CDC defines underweight as a BMI 18.5 kg/m2. Emily reported she became “more stressed” in nursing school and stopped eating lunch because she “needed to study.” Over time she became more restrictive, increased her exercise, and resumed binge eating and purging. Her weight plummeted, though she felt “huge” (especially after meals), and she intensely feared becoming fat. Emily endorsed severe restriction at the time of her current hospitalization, stating at times she lived on “coffee and hard candies,” and described a daily intake of 200–300 kilocalories (kcal). Her BMI at intake was 16.5 kg/m2.
Inpatient Treatment Course
Emily’s inpatient treatment consisted of a structured behavioral treatment program aimed at normalizing eating behavior and weight (see Attia & Walsh, 2009). Emily’s caloric prescription was initiated at 1800 kcal and raised at regular intervals; she was expected to gain 3–5 lbs per week. Treatment included family, individual, and group therapy. Emily began AN-EXRP approximately 6 weeks after admission, when she had restored weight to 104 lbs (BMI = 19.33 kg/m2) and was sufficiently nourished to participate. Emily’s course of AN-EXRP began prior to and ended during the weight maintenance phase of treatment. During this residential-like phase of treatment, autonomy increases and more time is spent off the unit before discharge. 2
Assessment
Food Intake
The Laboratory Meal (Steinglass et al., 2012) is modeled after Behavior Avoidance Tasks for anxiety (e.g., Beidel, Turner, Jacob, & Cooley, 1989). Participants consume a standard breakfast, and then have no food or drink until the laboratory meal at noon. The meal is presented as a turkey submarine sandwich (600 kcal), a bowl of potato chips (455 kcal), a jar of mayonnaise, and an 8 oz. bottle of water on a tray. Participants are instructed to eat as much or as little as they would like for lunch, and to indicate when they are done. Each food item was weighed before and after the meal and total caloric intake was calculated.
Anxiety
The Spielberger Anxiety Inventory, State version (STAI-S; Spielberger, Gorsuch, & Lushene, 1970), a commonly used measure of anxiety, was administered prior to the test meal. The State anxiety scale measures current anxiety. Items are scored on a 4-point Likert scale, from 1= “not at all” to 4= “very much so,” in response to prompts such as “I am tense” or “I am calm” (reverse-scored). The score total can range from 20 to 80 (higher scores indicating more anxiety), with a score of 45 considered the clinical cut-off. Pre-meal anxiety has been associated with caloric intake (Steinglass et al., 2010).
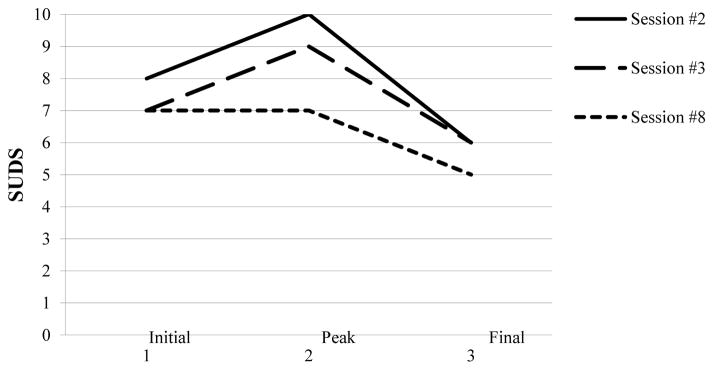
Subjective Units of Distress (SUDS; Wolpe & Lazarus, 1966), rated from 0–10 (≥7 = severe anxiety; 4–6 = moderate anxiety), were reported prior to and every three minutes during the laboratory meal. SUDS ratings were also used during exposure sessions. SUDs units are self-reported by the patient as a clinical tool in exposure therapy, to rate anticipatory anxiety associated with particular exposure exercises, and then to report actual (subjective) anxiety as it typically increases and then diminishes over the course of an exposure exercise and over the course of repeated exercises (see Figure 1). It is meant as a clinical tool to demonstrate within-session and between-session habituation to anxiety-provoking situations, and patients are expected to both tolerate higher self-reported levels of distress and to report lower levels of distress in the process of an effective course of therapy.
Figure 1. Example of Habituation Across Sessions.
In each of these sessions, Emily was exposed to coffee with milk and sugar. Each line depicts the increase in anxiety rating (SUDS) during that session followed by within-session habituation. Between-session habituation is depicted by SUDS ratings decreases with repeated exposure.
Reprinted from Glasofer et al., 2015.
The Yale-Brown-Cornell Eating Disorder Scale (YBC-EDS; Mazure, Halmi, Sunday, Romano, & Einhorn, 1994) is a semi-structured interview yielding two subscales reflecting the severity of current eating disorder “Rituals” (e.g., “needs to manipulate or stir food”) and “Preoccupations” (e.g. “thinks excessively about the fat content of food”). The YBC-EDS has 19 questions; separate scores are generated for severity of Preoccupations and severity of Rituals, and can be summed for a total score. In previous research, reported mean total YBC-EDS scores for individuals currently hospitalized for anorexia nervosa range from 7 to 18 (Sunday, Halmi, & Einhorn, 1994; Jordan, Joyce, Carter, McIntosh, Luty, McKenzie, Frampton, & Bulik, 2009). These totals are higher than those of individuals in recovery from an eating disorder (mean = 3), dieters (mean = 3), and non-dieters (mean = 0) (Sunday & Halmi, 2000).
Baseline Results
Emily was essentially unable to eat at the baseline meal (total intake = 18 kcal), taking only small bites of the lettuce and tomato that were provided as part of the sandwich. She recorded her thoughts following the meal, as “I really don’t want to eat this” and “Put your fork down now. If you continue eating, you’ll regret it later.” Her pre-meal STAI-S was 54, which is severe; for comparison, healthy individuals prior to a test meal report M = 25.0 ± 4.6 (Steinglass et al., 2010). Her pre-meal SUDS rating was also in the severe range, reported as 8 on a scale of 0–10. Emily’s baseline YBC-EDS score was 25 (Rituals = 12; Preoccupations = 13), reflecting “extreme distress” related to preoccupations, and “yielding to all” rituals.
Treatment
AN-EXRP begins with an assessment and extended treatment planning session. The goal is to identify details of the beliefs the patient has about eating, the stimuli that generate the most anxiety and avoidance, the feared consequences of eating, and rituals and avoidance behaviors intended to reduce anxiety. The therapist provides psychoeducation about the characteristics of anxiety, including the natural time course, and the role of irrational beliefs in AN. The rationale for exposure therapy and response prevention is provided explicitly:
THERAPIST: The goal of this treatment is to reduce the power that eating-related anxiety [or distress] has over your behavior. Unless you confront the feelings/situations you may continue to believe that the situation is dangerous, and continue to feel anxiety [or distress]. If you confront the feelings in the situation, you will find out that it is not as scary as you believed, that what you fear is not really happening, and that your anxiety will diminish with repeated confrontations.
Together, the patient and therapist arrange situations and behaviors associated with fear in a hierarchy, rating the severity of each fear using the SUDS (see Table 1). The first exposure is planned for the next session, using an item low on the hierarchy to build trust in the therapist and treatment through a successful exposure experience, illustrated below. Self-monitoring homework is assigned, focused on increasing awareness of anxiety and the use of avoidance and rituals (see Table 2 for rituals that are common among individuals with anorexia nervosa).
Table 1.
Selections from Emily’s Exposure Hierarchy.
| SUDS | Eating-related situations and foods |
|---|---|
| 10 | French fries; pasta with olive oil; pizza |
| 9 | Finishing whole plate of food; portioning at a buffet; butter on toast/muffin; eating a meal at an “off” time |
| 8 | Iced latte; bagel and cream cheese (portioning from container); eating whole sandwich without picking apart; picking a snack quickly; not changing order at restaurant |
| 7 | Hot latte; smoothie from street cart (unknown calories); bagel and single-serve cream cheese; finishing a yogurt, small bag of chips; not walking after a meal |
| 6 | Eating ½ sandwich without picking it apart; not fidgeting/body-checking at a meal; hard- boiled egg; eating a snack at an “off” time |
| 5 | Bites of sandwich without picking it apart; instant oatmeal with fruit mixed in; drinking sips of juice at an “off” time; not fidgeting after a meal |
| 4 | Coffee with milk and sugar; fruit juice; finishing a portion of fruit salad; instant oatmeal; drinking sips of water at an “off” time |
| 3 | Fat free popcorn; cucumbers; lettuce |
| 2 | Egg whites |
| 1 | Plain coffee, water |
| Reprinted from Glasofer et al., 2015 | |
Note: The full hierarchy used in treatment was much longer and spread across multiple pages.
Table 2.
Common Food Rituals in Eating Disorders
| Common Food Rituals |
|---|
| Eating slowly or quickly |
| Cutting food into small pieces |
| Preventing foods from touching each other or mixing |
| Using specific cutlery or china |
| Being informed about the calorie content and ingredients |
| Leaving a portion unfinished |
| Avoiding foods with particular ingredients or from particular “categories” |
| Chewing food a particular number of times |
| Eating foods in a particular order |
| Adding or eliminating condiments |
| Eating only foods of a certain temperature |
| Eating pre-portioned food from certain containers |
| Drinking or not drinking while eating |
| Taking large/small bites or sips |
| Eating only with particular people, or alone |
In Emily’s first session, she described her many eating symptoms and fears. It became clear, that her primary fear related to unending weight gain: “I will get fat…so fat that I will be physically unable to move.” With probing, Emily also articulated a “fear of fear itself:” “I don’t know what might happen. I’d just get really, really anxious.” She identified situations related to these feared consequences, in which she believed she would become so anxious that she “could not manage.” Feared foods and situations were arranged in Emily’s hierarchy (Table 1).
Emily identified behaviors that she relied upon to reduce anxiety: estimating caloric content of each food she ate and tallying up the day’s total repeatedly; picking apart, separating or manipulating foods; drinking fluids slowly; and fidgeting or pacing frequently to burn calories. It was agreed that these behaviors could be named “rituals.” Emily also described recurrent behaviors to avoid anxiety-provoking intake: not finishing her plate of food, under-portioning, avoiding calorically dense foods, and enforcing strict rules regarding timing of meals and snacks. These were named as “avoidant behaviors.” The self-monitoring forms that she subsequently completed indicated she felt high anxiety most of the time, in most food-related situations. She reported: “[The homework] makes me much more aware of it, as I am doing it, and I think of ways to combat the rituals.”
Emily and her therapist planned to use coffee with milk and sugar as the first exposure. This was selected from the bottom third of her hierarchy, rated at a SUDS of 3 or 4, reflecting an exposure associated with low-to-moderate anxiety, chosen to facilitate successful introduction to the skills of exposure. The therapist introduced the structure for the planned exposure, and the therapist’s role as a “coach” aiming to help her stick with a situation that may feel “difficult and demanding,” and to work on things that were “challenging but not totally overwhelming.” After collaborating on a session goal, the exposure began.
In early treatment (Sessions 2 and 3), the emphasis of AN-EXRP is to have exposure-based sessions that successfully demonstrate the individual’s capacity to engage with, learn about, and begin to tolerate anxiety. SUDS ratings are acquired every 5–10 minutes throughout the session, and the session continues until the anxiety decreases by at least 25% from its peak. Before the eating exposure begins, the patient articulates her goal for the session; goals are consistent with the treatment rationale (e.g., “to stay aware of my anxiety and not distract myself.”). The food is placed on the table and the patient is encouraged to approach and begin. The therapist helps prevent avoidant behaviors and promote awareness by coaching her to look at the food, bring the food close, experience the texture and flavor, and to talk about how the food tastes. At the end of the session, the patient identifies something she learned from the exposure (i.e., a “take-home message”). Specific practice assignments are created at the end of each session to be conducted repeatedly between sessions, and the content of the next session is identified.
In Emily’s second session, review of her self-monitoring forms indicated she experienced high anxiety most of the time in food-related situations, though it showed modest fluctuations. Emily had identified anxiety-provoking situations and the responses of fidgeting or pacing to reduce distress. Emily reported the homework helped her to be aware of automatic behaviors and develop ways to “combat” these rituals.
In accordance with the plan developed in the first session, the therapist laid out the table with cups of coffee varying in size, milk poured out into separate cups, and sugar. The fat content of the milk was not identified. The element of uncertainty was selected to invite anxiety. Emily appeared flushed and described feeling warm, noticing tightness in her chest and throat as well as racing thoughts. She leaned away from the coffee and directed her gaze away from the drink. The therapist reiterated the rationale for exposure therapy and reminded Emily of experiences she had of overcoming fear in the past. The therapist coached her first to face, then lean towards, then hold the drink in her hands while expressing her fears aloud and describing all physical sensations of anxiety as they occurred.
THERAPIST: Where should we start?
EMILY: I really don’t want to drink this.
THERAPIST: I know. Remember, in these sessions we go after the situations where there is going to be a lot of resistance. Kind of like how at first when you did your clinical rotation, you did not want to approach the patient and then with practice it got easier. What we work on here is noticing this fear and going for it.
Emily added milk and sugar to her coffee and began to drink it. After a sip, she put the lid back on, put the cup on the table and leaned back in chair.
EMILY: Can we wait a little? If we wait a little, I’ll be less full then.
THERAPIST: Part of what we’re working on here is this fear that fullness is actually dangerous.
Emily picked up cup, uncovered it, and continued to drink.
EMILY: I’m just so heavy.
THERAPIST: Where is the heaviness in your body?
EMILY: My abdomen.
THERAPIST: And what are you feeling there right now?
Emily pinched her stomach.
EMILY: Oh now, see, I went right to body checking.
THERAPIST: Okay, let’s keep your hand on the coffee cup.
EMILY: At least I noticed it, I see the connection.
THERAPIST: Yeah, that’s good. The body checking, the ritual, is definitely connected to the anxiety. Stay with it [the anxiety].
Emily continued to hold the cup and drink the coffee.
EMILY: I think I’ll take a bigger sip and see what happens.
THERAPIST: That’s a good idea. Let’s give it a shot and see what happens.
Emily took a large mouthful of her drink, and then started to put the cup down.
THERAPIST: Keep hold of the cup. Stay with it and tell me what you are feeling.
EMILY: It was too big. Now I’ve put too much in my body …I am just so afraid of being so full…I won’t be able to move…
THERAPIST: Let’s try again to lean into the anxiety…and see what happens. You can try taking another big sip, you can add more milk or sugar to what you already have, or you can take one of the cups…that I mixed ahead of time.
EMILY: I really, really don’t want to do this, but I’m going to do this because this is the thing I really don’t want to do and I think it will make me so, so anxious.
She reached for the pre-mixed drink and took a sip.
EMILY: I feel the same.
THERAPIST: Good, that was not what you expected.
The therapist emphasized the “disconfirming of the feared consequence” that is the goal of every exposure session. The therapist continued to urge Emily to take steps that would increase, rather than decrease, her anxiety. Later in the exposure, Emily anticipated that she would become so anxious and fat that she would be “unable to move.” After taking the step she feared, she was in fact more full, but she was not unable to move.
Following the exposure, the therapist explained that anxiety has a natural time course and will dissipate on its own without rituals or avoidance. As part of this discussion, the therapist drew a curve depicting a steep increase, a plateau, and a slow downward decline. This curve represents the natural experience of anxiety over time, and shows that if left alone, anxiety will ultimately decline. There are two important components to the psychoeducation around anxiety: 1) depicting that the patient generally fears that the anxiety will increase forever; 2) by using a ritual or avoidance technique, the patient has taken an “escape hatch” which successfully drops anxiety more quickly in the moment, but does not allow the person to experience the natural decrement in anxiety that happens with time. Observing the in-session SUDs ratings, the therapist described how the patient was “riding the wave of anxiety down from its peak” without using rituals and avoidance. Looking at a plot of her SUDS ratings from the session, Emily noted, “That looks good. I allowed myself to be challenged and my anxiety still went down.” The therapist introduced the goal of between-session habituation (e.g., “feeling less anxious with repeated practice”) across future sessions.
In Session 3, Emily repeated the coffee exposure with lower anxiety levels (see Figure 1). She moved faster to begin preparing, holding, and drinking the coffee, milk and sugar, and agreed to close her eyes while the therapist mixed in milk and sugar, to increase her anxiety about uncertain calories. When she expressed discomfort with the uncertainty of the caloric content, the therapist encouraged her to use this uncertainty to invite anxiety, saying “Yes, between all the milk and the sugar in there, it might just be considered a high-calorie drink.” She again verbalized her discomfort with her fullness, stating it was “like a 10 pound weight sitting on [my] stomach.” However, Emily herself recognized the exaggeration in her belief. Emily identified several take-home messages, such as: “The longer I delay, the more the anxiety builds up;” “I drank ‘the unknown’ and my anxiety did not spike;” and “I can push through and do uncomfortable things.” Homework successfully completed between these sessions included taking sips of liquids throughout the day and drinking all beverages slowly at meals and snack-time. Additional assignments required Emily to stay still in anxiety-provoking situations, rather than fidgeting to avoid anxiety or walking to burn calories.
In the middle portion of AN-EXRP, exposure content moves up the individual’s hierarchy as rapidly as possible. Therapist interventions during the exposure are similar to those utilized in earlier sessions, including encouragement to verbalize somatic, emotional, and cognitive experience and helping to interrupt avoidant and ritualistic behaviors. For example, she was able to identify that “Not being able to eat in a certain order makes me so uncomfortable. I eat vegetables and fruit first. I can’t eat my main meal before my vegetables. And if I don’t have my coffee first then I can’t start eating at all.” Working backward from the experience of a ritual, Emily identified that it made her feel “uncomfortable” (somatic, emotional), and ultimately that she believed eating the vegetables first prevented “bad” food could get into her system and that drinking coffee first spurred her metabolism to burn the subsequent calories more efficiently (anxious cognitions, not based in fact, promoting the ritualistic behavior).
In Sessions 4 through 6, Emily gradually worked her way up to in-session exposure to foods and situations that were higher on her hierarchy, such as bagels and cream cheese (SUDS rating = 8), and portioning food for herself from a large container (SUDS rating = 9). Environmental exposures were conducted in the hospital courtyard and a local restaurant. Emily began to independently verbalize her anxiety state or feared consequence, after which she was able to immediately eat without prompting. Her focus shifted from specific fears about eating (e.g., “Eating the bagel together with the cream cheese will immediately make me fat, worse than the two parts separately”) to more generalized meta-beliefs regarding anxiety and avoidance (e.g., “I know the anxiety goes higher the longer that I procrastinate, and it will go down the moment I start eating”). This shift from the identification of specific fears to new learning about how to successfully approach fears in general is intentional in EXRP. Emily described having the knowledge that her anxiety would always decrease over time, and that this was “relieving” and “empowering.”
Emily was encouraged to eliminate her rituals and avoidance between sessions, and reported being able to do so when her anxiety was moderate; when she was unable to resist a ritual, she was encouraged to “undo” the ritual or avoidance by deliberately choosing and engaging in a thought or behavior that provoked anxiety. For example, when her anxiety was only moderate, she was able to sit still despite the urge to walk (a ritual she engaged in to reduce the anxiety associated with consuming calories). However, at other times when her anxiety was higher she could not resist beginning to walk: in these cases, after noticing her immediate drop in anxiety, to “undo” the ritual, she made herself pause, choose a shorter walking route, and finally make herself sit still for several minutes. The therapist might explain the rationale for “undoing” in terms such as the following:
Sometimes you might find yourself starting a ritual before you have a chance to resist it. When you perform the ritual it actually gathers more power--it reduces your anxiety in the short-term, which makes it more likely to repeat again in the future. That is reinforcement. So when this happens, as soon as possible, you want to teach yourself the opposite lesson. You want to make yourself do the very thing that causes anxiety, and then not do the ritual, to “undo” the power that the ritual won back.
Emily commonly avoided her anxiety by “checking out,” either becoming distracted internally, or changing the topic of conversation. In one case, during an exposure, she began talking about a conversation she had on the unit that was only tangentially related. The following interaction between the therapist and the patient illustrates how this was addressed as Emily became aware of her own avoidance: THERAPISTt: Let’s keep it [our focus] here.
EMILY: I don’t want to keep it here.
THERAPIST: I know. Why is that?
EMILY: It would be so much easier if I could talk about anything else…then I wouldn’t have to concentrate on this.
THERAPIST: What’s the benefit of checking back in?
EMILY: Being able to deal with the anxiety.
In another case, when Emily became aware that she had “checked out” during a meal, she “un-did” the avoidance by making herself stare intently at each item on the tray to reconnect with awareness of eating food.
As treatment progressed, Emily grew increasingly aware of avoidant behaviors and took responsibility for reducing them. Ultimately, treatment progressed with Emily engaging in exposures higher up on the hierarchy to challenge her rituals during and between her exposure sessions. She practiced eating big bites, eating without manipulating foods (e.g., not separating a sandwich), eating “out of order,” finishing items completely, and taking a bite she considered “extra” to challenge fears of fullness and weight gain.
In Emily’s final AN-EXRP session (Session 12), she prepared and finished eating a peanut butter and jelly sandwich, portioned chips from a large bag, and drank a caloric beverage (juice). This content was a repetition from a prior session, to facilitate her sense of accomplishment at the completion of therapy. With minimal guidance from the therapist, she approached and then tolerated anxiety using a variety of behavioral strategies: she portioned more peanut butter than she felt was “safe,” she kept the sandwich together, she took bites from the middle of the sandwich while actively focusing on the “filling” of peanut butter and jelly, and she resisted the urge to fidget. Emily finished each item in its entirety. She described an overall decrease in anxiety (SUDS level started at 7.5, peaked at 7.5, and lowered to 3.5) compared with earlier sessions. During the debriefing after the exposure, Emily articulated a good understanding of why it would be critical for her to continue to challenge rituals and avoidant behaviors.
EMILY: This is good. This is hard but it’s good. This is what I’m going to need to know how to do. When I go out to eat, I can’t possibly know what’s in the food or how much I need.
THERAPIST: That’s right and here you really went against that.
EMILY: I know. Like I even took more chips than I wanted because I knew I had not taken enough.
Post-Treatment Assessment
Emily’s caloric intake in the test meal improved substantially, from 18 kcal to 209 kcal. Her pre-meal anxiety decreased, though she was symptomatic: her pre-meal SUDS rating decreased from 8 to 6.5 (from severe to moderate-to-severe), and her pre-meal STAI-S score decreased slightly from 54 to 51 (clinically significant cutoff = 45). Consistent with the goal of AN-EXRP, she demonstrated an ability to eat at the test meal in the presence of substantial anxiety. Her Thought Record (post-meal reporting of thoughts she had during the meal) showed important qualitative changes: post-treatment, she reported the thoughts “I think I can challenge myself to the chips,” “I want to rip this sandwich apart, but I won’t,” and “Just a few more bites,” in contrast to her pre-treatment self-talk which had been entirely centered on inhibiting eating. More broadly, her overall obsessive and compulsive ED symptoms improved, with a YBC-EDS total score of 20 (Preoccupations = 9, Rituals = 11), reflecting change from “extreme” to “moderate” for preoccupations, and a new ability to “make some effort to resist” rituals.
CONCLUSION
As an inpatient, Emily used the behaviorally oriented, structured program to successfully achieve weight restoration. Through the addition of AN-EXRP, a novel adjunctive treatment for AN, Emily focused on residual symptoms of anxiety about eating. Treatment revealed how her eating behavior was organized around catastrophic fears regarding the effect of food on weight and “fear of fear.” By confronting her fears through exposure and response prevention, she learned experientially that her fears were excessive, that anxiety is not constant, and that she could, in fact, feel more in control around eating by decreasing avoidant and ritualistic behaviors. Emily’s experience illustrates the results from a larger randomized, controlled trial (Steinglass et al., 2014): behavioral change occurred, though this was concurrent with inpatient treatment, and the improvement described with this brief intervention was not sufficient to constitute recovery. AN-EXRP creates a new lens through which patients and therapists can view eating-related emotions and behaviors, and offers new techniques to increase healthy eating behavior among individuals with AN.
Therapist Comments3
Being an EXRP therapist involves development of certain skills that can feel like training for an athletic event. The task requires that the therapist resist common instincts for reassurance, and direct the patient toward the feelings and situations that they most intensely fear and avoid, and to do so without the customary protections upon which they depend. Though other forms of therapy — arguably all forms of effective therapy — require the experience of unpleasant or avoided affect to some degree, EXRP is a highly directive approach, specifically designed to stimulate anxiety and coach an individual through it.
As we trained in EXRP under the supervision of our colleagues with expertise in anxiety disorders and OCD, we were warned that EXRP is not for every clinician. The treatment asks the therapist to contain/hold high levels of anxiety with the patient, and to remain relaxed and unfazed in the presence of anxiety. Because the therapeutic identity is often linked to providing reassurance, this stance can be uncomfortable. Recent research in the dissemination of exposure therapy suggests that therapists who have higher personal tolerance of anxiety and are less drawn to the reassuring and reflecting functions of therapy are more likely to utilize exposure, such as EXRP, effectively (Harned et al., 2013, 2014). Once at ease with the techniques of exposure therapy, one can feel well prepared to help the patient face and overcome her fears, and therapist empathy and support can be mobilized to produce positive behavioral outcomes.
EXRP demands that the therapist engage in a variety of delicate balancing acts—having a therapeutic stance that shifts between tough and compassionate (always allied against the eating disorder), as well as calibrating structure and creativity. Similar to conducting a standard CBT session, a plan for each session is created collaboratively with the patient. The therapist coaches towards completion of an exposure in the presence of high levels of anxiety – a rigid pose, in some ways; comfort with this develops over time. However, the therapist must also be able to shift stance when required in the moment (i.e., when anxiety is inappropriately high) and devise creative intermediate steps to ensure a successful exposure. Creativity, experience, and agility will help an EXRP therapist achieve the necessary balance between structure and innovation.
Challenging aspects of EXRP
One challenge for the EXRP therapist is to ensure that the relationship feels collaborative. The therapist nudges the patient forward, yet always with permission from the patient. The therapy proceeds successfully when the patient has fully embraced the rationale of tolerating difficult experiences in service of overcoming symptoms, and the therapist may return to the rationale frequently, prior to suggesting a step forward. The relationship can feel very intimate, as the therapist is bearing witness to the patient’s most intense fears–the large and irrational fears that emerge mostly when confronted with food.
Adding to the intimacy, EXRP at times puts the therapist in a position of personal disclosure. Unlike in other common forms of individual therapy, the EXRP therapist may choose to eat during sessions. Sometimes the therapist is modeling normal behavior (e.g., beginning to eat without a delay); sometimes the therapist is modeling how an exposure uses exaggerations of behavior to elicit particular fears (e.g., putting hands in a bowl of soup to experience that making a mess with food is not dangerous). Additionally, for some patients, social eating is the fear. For a successful exposure to these types of fears, the patient must speak frankly about what she imagines the therapist (or anyone else in the dining environment) is thinking: for example, that the therapist is judging her for having so much food on her plate, or that the waiter is critical of her for ordering a particular item off the menu. The therapist, in turn, must resist the impulse to reassure the patient in any way and instead may ask questions to expose the patient to more uncertainty (and thus, more anxiety; e.g., “Well, maybe that is a lot of food.” or, “Possibly the waiter did think that was a bad choice”). Depending on the specific context and the particular patient, these aspects of the treatment can be experienced as helpful coaching.
Satisfying aspects of EXRP
The most satisfying aspect of treatment is the feeling that you are really in there, wrestling with the very essence of the illness. Patients are quick to agree that this is the kind of treatment they need– something to grapple directly with the fear that engulfs them around eating. It is also a creative treatment. Every patient’s fears are different, and it requires imagination to best elicit and draw out these fears so that they can be reworked. When the patient develops mastery over the fears, they can often become playful – a very rewarding moment.
For example, an outpatient working on relapse prevention came in for dessert sessions. In the early sessions, the therapist placed a large wrapped brownie in front of her and she voiced her fears out loud.
PATIENT: (poking at the brownie, not picking it up) “I can bake brownies. I can sell brownies. But I can’t even touch this.” As she drew it towards her and tried to break off a bite, she fell into tears, so frustrated to find that the illness had this hold on her. That session was spent sitting in a lot of silence, with the therapist recurrently asking, “What would it be like to hold it?” or, “What if you took one bite?” This content was repeated for 3 sessions. In the 4th session, the therapist placed a different, unknown brand of brownie on the table. The patient reached for it, without hesitation, and took a bite. The brownies were exceptionally rich and sweet. Moments after her bite, the patient said, “Well, at least we know what’s in these!”
Her newfound ease in this situation allowed both therapist and patient to laugh, and created a moment of therapeutic connection.
Promoting the Alliance in EXRP
In the initial session, the therapist requests an example from the patient of her experience–unrelated to illness – of overcoming a fear. This personalized example emphasizes the individual’s strengths and creates a useful touchstone to which the patient and therapist can return throughout treatment, especially in difficult moments.
THERAPIST: Can you think of an example from your life, nothing to do with the illness, where you were afraid of something, but you stuck with it?
EMILY: When I first started clinical rotations at the hospital, I was really anxious but the more I went the more accustomed I became to it…at first, I’d be terrified to even approach a patient, but eventually it became just like I was changing a dressing and it would be totally okay.
THERAPIST: That’s a great example. At first you were afraid of making a mistake. How did you get past that?
EMILY: well, after I did it a few times, I noticed that I was doing okay. Also, I realized that my supervisors were helping me out when I made a mistake – they weren’t getting mad.
This story, which embodies the spirit of exposure, was returned to throughout Emily’s AN-EXRP sessions to reiterate the rationale for treatment and maintain her motivation.
Creating and reworking the treatment hierarchy also enhances the therapeutic alliance. This component of treatment planning demonstrates to the patient that the therapist is 1) aware, unfazed, and sensitive to the depth and breadth of problematic behaviors; 2) interested in individualizing the therapy; and 3) flexible in re-evaluating the rank order of feared situations as needed. For example, referring to Emily’s hierarchy (partially reproduced in Table 1), the patient might suggest a behavioral item such as eating a “bagel and cream cheese,” and the therapist might add “portioning it from a container?” indicating her understanding that pre-measured cream cheese packages are less anxiety provoking than self-portioned. This suggestion serves multiple purposes: it nudges the patient forward, indicates matter-of-fact knowledge and acceptance about the disorder in general, and personalizes the hierarchy to closely focus on the often invisible ways that the anxiety is maintained by rituals and avoidance, even in the context of “eating.” The patient ideally has the experience of being clearly seen and described, as well as supported to add all the pieces to the plan that is necessary to succeed.
The alliance is strengthened during EXRP moments of “survival.” When a patient has tolerated a high level of anxiety to complete an exposure task and comes out the other side of that experience, the therapist and patient together relish that success. In Emily’s case, at the end she chose to eat extra chips and the patient and therapist were able to acknowledge that triumph. This promotes a sense of team-ness, reinforcing that therapist and patient are in it together as they take on anxiety-provoking challenges.
Enduring a patient’s anxieties for 90 minutes can be draining for the therapist, especially because patients with anorexia nervosa, by virtue of their very diagnosis, waver in their investment in overcoming rituals and changing eating behavior. For example, one inpatient was grappling with a particularly high degree of ambivalence about recovery. She doubted whether or not it was possible for her and had a lot of fear about giving up the rituals upon which she had relied for so long. During most EXRP sessions, her anxiety manifested as endless, sometimes uncontrollable sobbing and shaking. As the patient worked to challenge behaviors, such as eating a sandwich without picking it apart, the fears she acknowledged were often presented in language riddled with self-loathing. The intense affect in the room and the patient’s extreme language were difficult for the therapist to sit with over an extended timeframe —she was clearly in such a state of anguish. It was challenging to keep to ensure that the patient was exposed to her anxiety, rather than her self-hatred. The treatment alliance, and the treatment itself, were helped by ongoing frank discussions about the patient’s ambivalence. For example, the therapist offered, “I understand that you don’t always feel like openly inviting your anxiety – I wouldn’t expect you to want to do something that is obviously so uncomfortable. But I wonder, do you think it might help you to do this, even though a part of you doesn’t want to?” Self-hatred was labeled as such, and the therapist invited the patient to, “See if you can leave some of the anger that you have at yourself outside of this room. I’d rather you be angry at the illness than yourself, and that we focus in here, right now, on what you’re feeling scared of instead. Would that be okay with you? How could I help you to do that?” Seeking permission from the patient helped her move forward with behavioral challenges.
The alliance between therapist and patient has rarely been strained (in the opinion of the clinical trial therapists), and if so, it was our observation that this occurred with patients who did not find the premise of the treatment relevant to them. EXRP is a high-intensity approach; it demands a lot of patients both during and between sessions. Therefore, it is essential for patients to “buy in” to the treatment rationale. This is addressed in the treatment planning session and again as part of the debriefing after the first active exposure, when the therapist asks the patient how she thought it went, how different it was from what she expected, and if she could have imagined that changes in anxiety would be noticeable by “sticking with the feeling, rather than avoiding it.” While some ambivalence is of course expected, there is cause for concern if the patient is consistently disinterested in the treatment or uncertain about its relevance for his/her symptoms. In these cases, rather than further strain the therapist-patient alliance, alternate treatment approaches (including motivational work to move towards readiness for EXRP) should be considered.
Footnotes
For a more detailed presentation of the case, see the Casebook of Evidence-Based Therapy for Eating Disorders, Thompson-Brenner (Ed.), 2015. The relevant chapter is presented more briefly in this special section, with additional material concerning the therapist experience.
In this case study it is not possible to separate the effects of EXRP from those of ongoing inpatient treatment. For AN-EXRP randomized controlled trial results see Steinglass et al., 2014.
As part of the special section on approaches to improving the treatment of AN, the authors were requested to write a section reflecting on the experience of treating patients with AN using the innovative adjunctive approach, including the quality of the relationship, challenges and satisfactions relative to customary treatment approaches.
References
- Attia E, Walsh BT. Behavioral management for anorexia nervosa. New England Journal of Medicine. 2009;360:500–6. doi: 10.1056/NEJMct0805569. [DOI] [PubMed] [Google Scholar]
- Beidel DC, Turner SM, Jacob RG, Cooley MR. Assessment of social phobia: Reliability of an impromptu speech task. Journal of Anxiety Disorders. 1989;3:149–158. [Google Scholar]
- Bulik CM, Sullivan PF, Fear JL, Joyce PR. Eating disorders and antecedent anxiety disorders: a controlled study. Acta Psychiatr Scand. 1997;96(2):101–107. doi: 10.1111/j.1600-0447.1997.tb09913.x. [DOI] [PubMed] [Google Scholar]
- Fairburn CG. Cognitive Behavior Therapy and Eating Disorders. New York: Guilford Press; 2008. [Google Scholar]
- Goldfarb LA, Fuhr R, Tsujimoto RN, Fischman SE. Systematic desensitization and relaxation as adjuncts in the treatment of anorexia nervosa: a preliminary study. Psychol Rep. 1987;60(2):511–518. doi: 10.2466/pr0.1987.60.2.511. [DOI] [PubMed] [Google Scholar]
- Harned MS, Dimeff LA, Woodcock EA, Contreras I. Predicting adoption of exposure therapy in a randomized controlled dissemination trial. Journal of Anxiety Disorders. 2013;27:754–762. doi: 10.1016/j.janxdis.2013.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harned MS, Dimeff LA, Woodcock EA, Kelly T, Zavertnik J, Contreras I, Danner SM. clinicians to exposure: A randomized controlled dissemination trial of exposure therapy for anxiety disorders. Behavior Therapy. 2014;45:731–744. doi: 10.1016/j.beth.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu GLK, Kaye W, Weltzin T. Are the eating disorders related to Obsessive Compulsive Disorder? International Journal of Eating Disorders. 1993;14:305–318. doi: 10.1002/1098-108x(199311)14:3<305::aid-eat2260140309>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Jordan J, Joyce PR, Carter FA, McIntosh VV, Luty SE, McKenzie JM, Frampton CM, Bulik CM. The Yale-Brown-Cornell eating disorder scale in women with anorexia nervosa: what is it measuring? Internation Journal of Eating Disorders. 2003;42(3):267–274. doi: 10.1002/eat.20605. [DOI] [PubMed] [Google Scholar]
- Kozak MJ, Foa EB. Mastery of Obsessive-Compulsive Disorder. New York: Oxford University Press; 1997. [Google Scholar]
- Mayer LE, Schebendach J, Bodell LP, Shingleton RM, Walsh BT. Eating behavior in anorexia nervosa. International Journal of Eating Disorders. 2012;45:290–293. doi: 10.1002/eat.20924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazure CM, Halmi KA, Sunday SR, Romano SJ, Einhorn AM. The Yale-Brown-Cornell eating disorder scale: development, use, reliability and validity. Journal of Psychiatric Research. 1994;28:425–445. doi: 10.1016/0022-3956(94)90002-7. [DOI] [PubMed] [Google Scholar]
- Pollice C, Kaye WH, Greeno CG, Weltzin TE. Relationship of depression, anxiety, and obsessionality to state of illness in anorexia nervosa. International Journal of Eating Disorders. 1997;21:367–376. doi: 10.1002/(sici)1098-108x(1997)21:4<367::aid-eat10>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- Schebendach J, Mayer LE, Devlin MJ, Attia E, Walsh BT. Dietary energy density and diet variety as risk factors for relapse in anorexia nervosa: a replication. International Journal of Eating Disorders. 2012;45:79–84. doi: 10.1002/eat.20922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene RE. Manual for the state-trait inventory. Palo Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- Steinglass J, Albano AM, Simpson HB, Carpenter K, Schebendach J, Attia E. Fear of food as a treatment target: exposure and response prevention for anorexia nervosa in an open series. International Journal of Eating Disorders. 2012;45:615–621. doi: 10.1002/eat.20936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinglass JE, Albano A, Simpson HB, Wang Y, Zou J, Attia E, Walsh BT. Confronting Fear Using Exposure and Response Prevention for Anorexia Nervosa. International Journal of Eating Disorders. 2014;47:174–80. doi: 10.1002/eat.22214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinglass JE, Sysko R, Glasofer D, Albano AM, Simpson HB, Walsh BT. Rationale for the application of exposure and response prevention to the treatment of anorexia nervosa. International Journal of Eating Disorders. 2011;44:134–141. doi: 10.1002/eat.20784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinglass JE, Sysko R, Mayer L, Berner LA, Schebendach J, Wang Y, … Walsh BT. Pre-meal anxiety and food intake in anorexia nervosa. Appetite. 2010;55:214–218. doi: 10.1016/j.appet.2010.05.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sunday SR, Halmi KA. Comparison of the Yale-Brown-Cornell Eating Disorders Scale in recovered eating disorder patients, restrained dieters, and nondieting controls. Int J Eat Disord. 2000;28(4):455–459. doi: 10.1002/1098-108x(200012)28:4<455::aid-eat15>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Sunday SR, Halmi KA, Einhorn A. The Yale-Brown-Cornell Eating Disorder Scale: a new scale to assess eating disorder symptomatology. Int J Eat Disord. 1995;18(3):237–245. doi: 10.1002/1098-108x(199511)18:3<237::aid-eat2260180305>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Thompson-Brenner H, editor. Casebook of Evidence-Based Therapy for Eating Disorders. New York, NY: Guilford Press; 2015. [Google Scholar]
- Walsh BT, Kaplan AS, Attia E, Olmsted M, Parides M, Carter JC, … Rockert W. Fluoxetine after weight restoration in anorexia nervosa: a randomized controlled trial. JAMA. 2006;295(22):2605–2612. doi: 10.1001/jama.295.22.2605. [DOI] [PubMed] [Google Scholar]
- Wolpe J, Lazarus AA. Behavior therapy techniques. New York: Pergamon; 1966. [Google Scholar]