Abstract
Background
There is excellent evidence that surgical safety checklists contribute to decreased morbidity and mortality.
Objective
To develop a surgical checklist comprising the key phases of care for rectal cancer patients.
Design
Consensus-oriented decision-making model involving iterative input from subject matter experts under the auspices of the American Society of Colon and Rectal Surgeons.
Results
The process generated a 25-item checklist covering the spectrum of care for rectal cancer patients undergoing surgery.
Limitations
Lack of prospective validation.
Conclusions
The American Society of Colon and Rectal Surgeons Rectal Cancer Surgery checklist comprises the essential elements of pre-, intra- and postoperative care that must be addressed during the surgical treatment of patients with rectal cancer.
Keywords: Checklist, Rectal neoplasms, Safety, Consensus, Medical errors, Surgeons
Introduction
The utilization of checklists for complex processes is widely advocated in diverse fields such as aviation, manufacturing and industrial safety sciences. As in aviation, errors in medicine may arise from procedural violations, poor communication, lack of proficiency, and/or conscious violation of recommendations.1 To avoid these errors, some clinicians have promoted checklist development within clinical healthcare, with particular attention paid towards procedural-based specialties such as surgery. The World Health Organization Surgical Safety Checklist (WHO SSC) is the most widely-distributed instrument aimed at reducing surgical error. Focusing on actions exclusively within the operating room itself, WHO SSC implementation is credited with significant reductions in rates of inpatient complications and perioperative mortality in both developing and mature healthcare systems.2, 3
Checklists help to eliminate omission of crucial steps, particularly during uncommon procedures or at times when information complexity may reduce situational awareness.4 The management of rectal cancer fulfills these criteria. The majority of rectal cancer patients in North America are treated by surgeons who perform 10 or fewer cases annually.5 Moreover, the disease routinely requires coordination between surgeons, radiation and medical oncologists, and other clinical personnel such as radiologists, pathologists and wound-ostomy nurses. Decision-making is highly patient-centric and management often individualized, based on both tumor and patient characteristics. The operative technique of total mesorectal excision is technically demanding, and is rarely objectively assessed and recorded by pathologists. Importantly, a clear correlation exists between surgeons’ experience and knowledge, and patient outcomes, which may partially explain observed discrepancies between high- and low-volume surgeons.6 Thus, the care of rectal cancer patients provides a surfeit of opportunities for both justified and arbitrary variation in care.
Recognizing the potential value of checklists in improving patient safety and outcomes, the Quality and Safety Assessment Committee of the American Society of Colon and Rectal Surgeons (ASCRS) developed a comprehensive rectal cancer surgery checklist. The purposes of the initiative were multiple: 1) to provide a guide to enhance safety and quality of care for rectal cancer patients undergoing surgery, 2) to incorporate best practices in treating these patients, 3) to raise general awareness of the importance of each individual checklist item, and 4) to serve as a potential foundation for building centers of excellence in rectal cancer treatment.
Organizational barriers to effective communication and perceived lack of ownership over the safety initiative (so-called physician buy-in) are major obstacles to successful checklist deployment.7, 8 To counter these effects and to ensure validity of checklist items, ASCRS leadership sought the iterative inclusion of many subject-matter experts and members during checklist development. Through the use of an iterative model based upon sequential meetings and discussion to consensus, the ASCRS produced a checklist that spans the preoperative, intraoperative and postoperative course of the typical patient with rectal cancer. This report describes the development process and resulting ASCRS Rectal Cancer Surgery checklist.
Methods
There are several different formal processes for developing action lists. The modified Delphi approach determines final conclusions based on expert consensus using an iterative approach. The classic methodology relies on literature review, multiple anonymous voting rounds, and a final in-person discussion and ranking. While the anonymity reduces bias caused by prominent contributors, the lack of open discussion can stifle ideas.9 For the ASCRS Rectal Cancer Surgery checklist, the process was modified to create the checklist items through an initial literature review, followed by the combination of contributions and critiques with serial meetings of subject matter experts, culminating in anonymous input from members at the ASCRS 2011 Annual Meeting. The final product was the result of multiple iterative revisions and discussion to consensus without formal voting. The project was managed by one of the authors (A.M.M.) under the auspices of the ASCRS Quality Assessment and Safety committee. Institutional Review Board approval was not required.
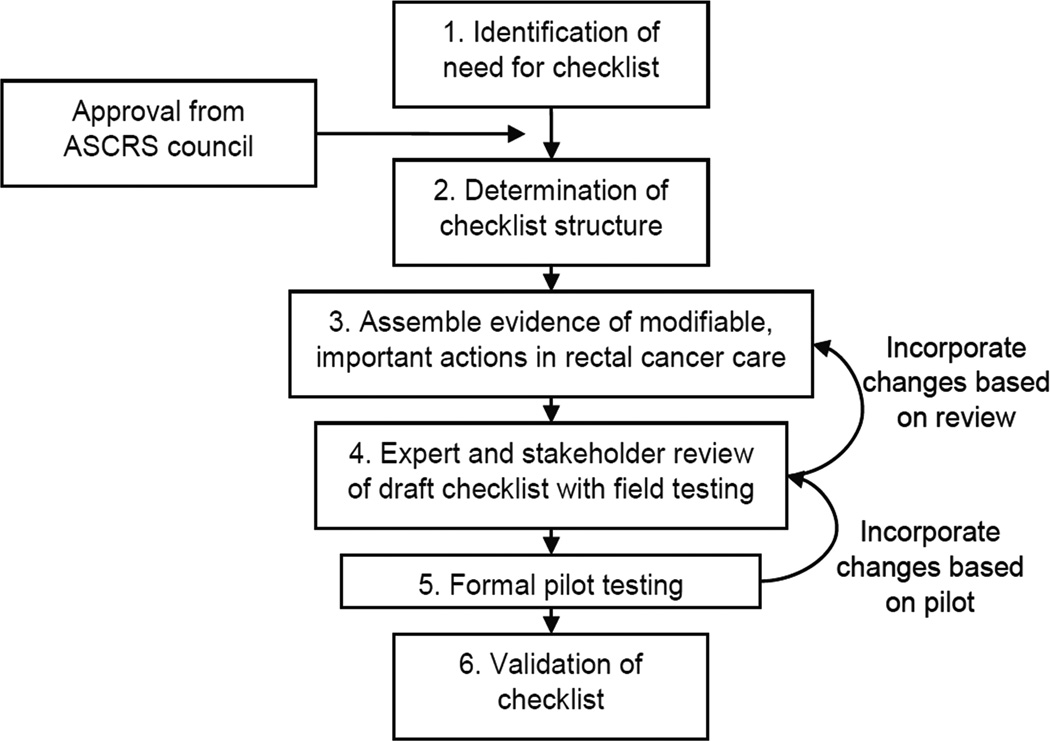
The creators of the WHO SSC delineated six distinct steps in checklist development,2, 10 which were followed in the early stages of developing the ASCRS Rectal Cancer Surgery checklist: 1) identification of the need for a checklist, 2) determination of the checklist structure, 3) assembling evidence of modifiable and important actions in rectal cancer care, 4) expert and stakeholder review of draft, along with limited field testing, 5) formal pilot testing, and 6) validation of the checklist (Figure 1). Since much of rectal cancer therapy relies on decision-making outside of the operating room, the checklist was designed to encompass three phases of patient care. Checklist items for pre-, intra- and postoperative phases of care were collected based on review of the existing peer-reviewed literature. Other primary source documents included the Surgical Care and Outcomes Assessment Program (SCOAP) Rectal and Diverticulitis Surgery Dictation Guide.11 All sources were reviewed by members of the Quality Assessment and Safety and the Standards committees, and information condensed based on quality of available evidence and cumulative professional experience.
Figure 1.
Checklist development process
After discrete item formulation, the checklist underwent critical review by all members of the ASCRS Quality Assessment and Safety committee. Critiques were collected and then re-distributed to members for a second review, with changes incorporated based on majority consensus. The initial Rectal Cancer Surgery checklist was then made available to the general membership for review during the ASCRS Annual Convention in Vancouver, BC, in 2010. Member comments and recommendations were reviewed, discussed in committee, and selectively incorporated into revision. At this time a near final draft of rectal cancer practice guidelines became available and the checklist was therefore vetted by the Guidelines Committee chair. In a final step, the draft checklist went to the ASCRS Executive Council and Standards Committee to ensure consistent messaging.
Results
Using a consensus-based decision-making model for creation of the ASCRS Rectal Cancer Surgery checklist, a total of five initial committee meetings yielded the rough draft that was then reviewed by the membership as a whole. A total of 49 individual comments were collected from members, all of whom are also subject matter experts as practicing colorectal surgeons; sample comments are shown in Table 1. In turn, the comments were re-incorporated into the checklist. Items suggested by ASCRS members, and incorporated in the final checklist, included documenting family history, determining the relationship of the tumor to the levator musculature, consideration of diverting loop ileostomy and/or postoperative medical oncology consultation in appropriate patients, and ensuring documentation of radial and distal margins on final pathology. The final ASCRS Best Practices Checklist for Rectal Cancer Surgery was approved by the Executive Committee in 2012 and published electronically to the Society webpage (Figure 2).12
Table 1.
Representative comments from ASCRS membership
| Supportive | |
| “Agree with reassessment of tumor response immediately preop…” | |
| “Great job.” | |
| “Ideally should be best practice, but might not be achievable. May be more useful as minimum acceptable.” | |
| “To maintain or ensure standards, probably needs some sort of reporting to be sure it gets done.” | |
| Too Restrictive | |
| “I don’t think we need to advocate for repeating any radiographic imaging after neoadjuvant treatment, do we?” | |
| “Referral to medical oncologist [for specific stages]?” | |
| “Don’t need postop checklist.” | |
| “Pouch vs. no pouch sounds mandatory.” | |
| “Would seem colorectal specialists don’t need a checklist.” | |
| “Tumor board not always applicable – hurts high-volume practice.” | |
| Too Vague | |
| “”Need relation of tumor to [rectal] valves and anterior/posterior.” | |
| “Consider assessment of post-op sexual function, quality of life, bowel function, & stoma management.” | |
| “Request standardization of pathology reporting” | |
| “Need pathologist’s synoptic report.” | |
| “Add [intraoperative assessment] for ureter.” | |
| “Add family history to pre-op evaluation.” |
Figure 2.
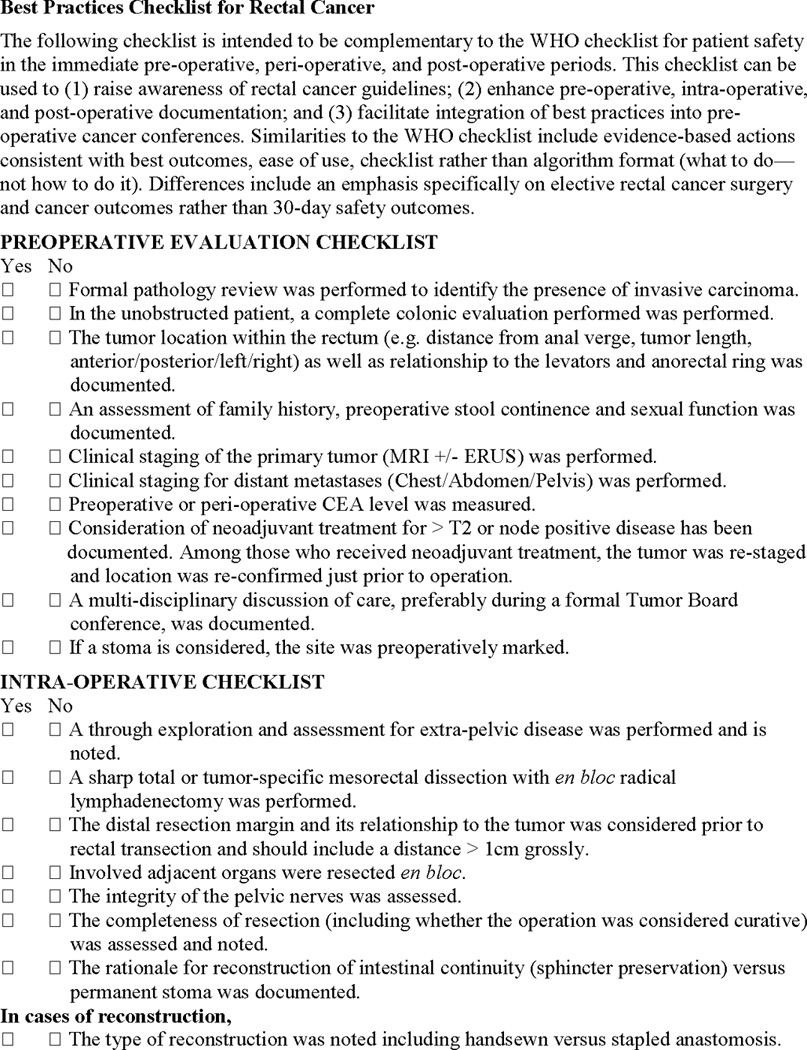
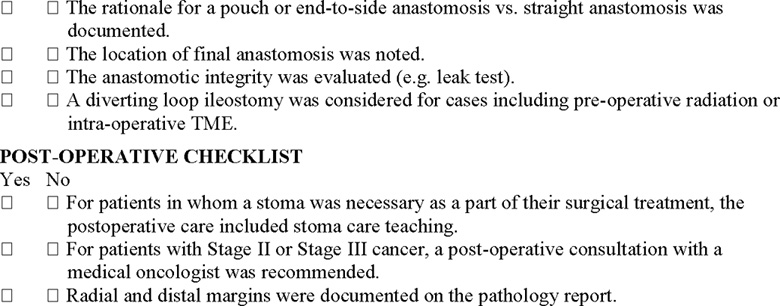
Final version of the American Society of Colon and Rectal Surgeons (ASCRS) Rectal Cancer Surgery Checklist
Discussion
The ASCRS Rectal Cancer Surgery checklist represents an initial effort to establish a comprehensive pathway in the multidisciplinary treatment of a complex disease process. The checklist spans the continuum of patient treatment and provides “critical steps” for each phase, with the goal of improving and standardizing clinical care. In drafting the checklist, committee members aligned checklist items with ASCRS Clinical Practice Guidelines that were under development, to ensure a consistent message from the organization.13 Furthermore, society members were given ample opportunity to recommend, review and revise the checklist items through an iterative process.
Checklists must be carefully designed to ensure that they support rather than interfere with patient care. The goal is to create a tool that supports clinical practice without attempting to substitute a rigid algorithm for professional judgment. It should not supplant decision-making but rather remind clinicians of tasks that, if forgotten, may lead to serious consequences.10 In crafting the Rectal Cancer Surgery checklist, the committee felt it was important to avoid being proscriptive with checklist items; for example, mandating that all rectal cancers within 4 cm of the anal verge require abdominoperineal resection. Additionally, the checklist is meant to allow surgeons to focus on complex issues while ensuring that simple tasks are addressed for every patient, every time.10 To this end, several of the intraoperative items serve as simple reminders to document technical steps that colorectal fellowship-trained surgeons routinely employ, such as sharp mesorectal excision. Lastly, compliance with the checklist should help surgeons avoid potentially catastrophic errors of omission, e.g. failure to screen the entire colon for synchronous neoplasms prior to definitive rectal surgery in non-obstructed patients. Such error-trapping techniques have long been employed in the aviation community to mitigate the impact of human error.14
Several comments from ASCRS members questioned whether the checklist should comprise ideal parameters (e.g. best practices) in contrast to the minimum acceptable steps in treating rectal cancer patients. Other commenters stated that the term “checklist” itself confers a negative connotation. According to Gawande, the true utility of checklists is to remind operators of the minimum necessary steps in a process; checklists not only offer the possibility of verification, but instill discipline and higher performance.4 As such, the ASCRS Rectal Cancer Surgery checklist should not be viewed as a practice guideline or least threshold, but a living document intended as a tool for ASCRS members that may be used to individualize specific patient scenarios, with ongoing opportunities to comment through the ASCRS website. Suggested issues for review include necessity for rigid proctoscopy and assessment of anal sphincter tone, timing of CEA testing, identification of structures such as the ureters, and absolute minimums for both radial and axial margins of resection. The ongoing review of the checklist has been operationalized to ensure that it remains aligned with current literature and other ASCRS efforts.
Regardless of a surgeon’s individual view of safety checklists, there is clear evidence that successful checklist implementation relies on strong physician leadership.8 Implementation requires an understanding as to why a checklist is needed, along with significant buy-in from potential checklist users. Common obstacles to utilization include perceived design issues with the checklist itself, and resistance from senior clinicians.7 Some of this reluctance may be mitigated when using this checklist, which has been created and endorsed by senior leaders within the ASCRS. In fact, the ASCRS Executive Council has reviewed and endorsed the checklist on 2 occasions (2012 and 2015), along with on-going review by members of the ASCRS Quality Assessment and Safety committee. Ultimately, each individual colorectal surgeon must recognize that surgical safety checklists are one of the strongest evidence-based interventions available for reducing patient harm, and should consciously choose to implement this checklist.15
The ASCRS Rectal Cancer Surgery checklist is novel in that it spans patient care in both location and time through the division of treatment into three distinct phases. Preoperative items include measuring the serum CEA, ensuring that staging was performed for both regional and distant metastatic disease, and marking for an abdominal stoma if indicated. The intraoperative checklist deals predominantly with the documentation of surgery-specific items such as sharp mesorectal excision with radical lymphadenectomy, but it also provides reminders of clinical tasks that may not be routinely performed by all surgeons (e.g. assessing integrity of pelvic nerves). The postoperative tasks include structured ostomy teaching and referral to medical oncology, depending on final pathologic stage. While all 25 of these items seem obvious in isolation, it is doubtful that all patients in every clinical setting meet each and every one of these criteria. Use of the ASCRS Rectal Cancer Surgery checklist has the potential to improve care of these complex cases by reducing the possibility of omission.
Several limitations with respect to the checklist development process should be acknowledged. First, as with any widely-distributed document built by consensus, it is difficult to know the extent of its circulation among ASCRS members. Checklist utilization may be limited by the feeling, among some members, that they are not represented in the process. Ideally, this limitation will be overcome through broader use of the ASCRS website and acceptance of the checklist by surgeons as a useful tool. Secondly, the checklist may not be applicable to every clinical presentation; for example, many checklist items do not pertain to a patient presenting with acute obstruction. Lastly, it should be emphasized that the ASCRS Rectal Cancer Surgery Checklist is a living document, amenable to change as new evidence or clinical practices develop. As such, the checklist may not be a complete synopsis of other, equally useful, published material.
The ASCRS Rectal Cancer Surgery checklist may be most beneficial in low-volume practices in which a regional referral is not feasible or desired. Going forward, prospective checklist validation using a mix of practice types and case volumes is important. Future directions for the checklist include development of a mobile application to facilitate use and potential incorporation into mature electronic medical record systems. Opportunity exists for collaboration with other professional surgical organizations to facilitate widespread adoption of this best-practice. Aspects such as consistent grading of TME quality or ensuring completion of adjuvant chemotherapy lend themselves to partnership with non-surgical specialists. Importantly, the ASCRS Rectal Cancer Surgery checklist is a living document available to colorectal surgeons on the ASCRS website. Surgeons have the opportunity to make comments about the checklist, which are reviewed semi-annually by the Quality and Safety Assessment Committee, and changes may be made to the document as new evidence arises. It provides a compelling opportunity to improve patient outcomes through the consistent and systematic application of established practices in rectal cancer treatment.
Acknowledgments
The authors thank the 2011–2012 members of the Quality and Safety Assessment Committee for discussion and insights.
Source of Funding: This study was funded in part by the Memorial Sloan Kettering cancer center core grant P30 CA008748. (Dr. Larissa Temple)
Footnotes
Disclaimers: The views expressed in this article are those of the authors and do not reflect the official policy of the United States Air Force, Department of Defense, or the U.S. Government.
Conflicts of Interest: The authors declare no conflicts of interest.
Presented in part as a poster at the American Society of Colon and Rectal Surgeons 2011 Annual Meeting, Vancouver, BC, Canada, May 14th – 18th, 2011
Author Contributions:
Concept & design: Glasgow, Morris, Baxter, Fleshman, Alavi, Luchtefeld, Monson, Chang, Temple
Acquisition of data: Morris, Baxter, Temple
Analysis & interpretation: Glasgow, Morris, Baxter, Fleshman, Alavi, Luchtefeld, Monson, Chang, Temple
Drafting of manuscript: Glasgow, Morris, Temple
Critical revision: Baxter, Fleshman, Alavi, Luchtefeld, Monson, Chang
References
- 1.Helmreich RL. On error management: lessons from aviation. BMJ. 2000;320:781–785. doi: 10.1136/bmj.320.7237.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360:491–499. doi: 10.1056/NEJMsa0810119. [DOI] [PubMed] [Google Scholar]
- 3.de Vries EN, Prins HA, Crolla RM, et al. Effect of a comprehensive surgical safety system on patient outcomes. N Engl J Med. 2010;363:1928–1237. doi: 10.1056/NEJMsa0911535. [DOI] [PubMed] [Google Scholar]
- 4.Gawande A. The Checklist Manifesto: How to Get Things Right. New York: Metropolitan Books; 2009. [Google Scholar]
- 5.Richardson DP, Porter GA, Johnson PM. Self-reported practice patterns and knowledge of rectal cancer care among Canadian general surgeons. Can J Surg. 2014;57:385–390. doi: 10.1503/cjs.001814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Richardson DP, Porter GA, Johnson PM. Surgeon knowledge contributes to the relationship between surgeon volume and patient outcomes in rectal cancer. Ann Surg. 2013;257:295–301. doi: 10.1097/SLA.0b013e31825ffdca. [DOI] [PubMed] [Google Scholar]
- 7.Russ SJ, Sevdalis N, Moorthy K, et al. A qualitative evaluation of the barriers and facilitators toward implementation of the WHO surgical safety checklist across hospitals in England: lessons from the "Surgical Checklist Implementation Project". Ann Surg. 2015;261:81–91. doi: 10.1097/SLA.0000000000000793. [DOI] [PubMed] [Google Scholar]
- 8.Conley DM, Singer SJ, Edmondson L, Berry WR, Gawande AA. Effective surgical safety checklist implementation. J Am Coll Surg. 2011;212:873–879. doi: 10.1016/j.jamcollsurg.2011.01.052. [DOI] [PubMed] [Google Scholar]
- 9.Graham B, Regehr G, Wright JG. Delphi as a method to establish consensus for diagnostic criteria. J Clin Epidemiol. 2003;56:1150–1156. doi: 10.1016/s0895-4356(03)00211-7. [DOI] [PubMed] [Google Scholar]
- 10.Weiser TG, Haynes AB, Lashoher A, et al. Perspectives in quality: designing the WHO Surgical Safety Checklist. Int J Qual Health Care. 2010;22:365–370. doi: 10.1093/intqhc/mzq039. [DOI] [PubMed] [Google Scholar]
- 11. [Accessed January 31, 2015];SCOAP Rectal Cancer and Diverticulitis Surgery Dictation Guide. at http://www.scoap.org/downloads/SCOAP-Rectal-Cancer-and-Diverticulitis-Sugery-Dictation-Guide.pdf.
- 12.ASCRS Rectal Cancer Surgery checklist. [Accessed January 31, 2015]. at http://www.fascrs.org/gedownload!/Best%20Practices%20Checklist%20for%20Rectal%20Cancer%20final.pdf?item_id=17004774&version_id=17004775. [Google Scholar]
- 13.Monson JR, Weiser MR, Buie WD, et al. Practice parameters for the management of rectal cancer (revised) Dis Colon Rectum. 2013;56:535–550. doi: 10.1097/DCR.0b013e31828cb66c. [DOI] [PubMed] [Google Scholar]
- 14.Turner T. Controlling Pilot Error: Checklists & Compliance. New York: McGraw-Hill Professional; 2001. [Google Scholar]
- 15.Howell AM, Panesar SS, Burns EM, Donaldson LJ, Darzi A. Reducing the burden of surgical harm: a systematic review of the interventions used to reduce adverse events in surgery. Ann Surg. 2014;259:630–641. doi: 10.1097/SLA.0000000000000371. [DOI] [PubMed] [Google Scholar]