Abstract
To investigate the outcomes and reliability of hybrid surgery (HS) versus anterior cervical discectomy and fusion (ACDF) for the treatment of multilevel cervical spondylosis and disc diseases.
Hybrid surgery, combining cervical disc arthroplasty (CDA) with fusion, is a novel treatment to multilevel cervical degenerated disc disease in recent years. However, the effect and reliability of HS are still unclear compared with ACDF.
To investigate the studies of HS versus ACDF in patients with multilevel cervical disease, electronic databases (Medline, Embase, Pubmed, Cochrane library, and Cochrane Central Register of Controlled Trials) were searched. Studies were included when they compared HS with ACDF and reported at least one of the following outcomes: functionality, neck pain, arm pain, cervical range of motion (ROM), quality of life, and incidence of complications. No language restrictions were used. Two authors independently assessed the methodological quality of included studies and extracted the relevant data.
Seven clinical controlled trials were included in this study. Two trials were prospective and the other 5 were retrospective. The results of the meta-analysis indicated that HS achieved better recovery of NDI score (P = 0.038) and similar recovery of VAS score (P = 0.058) compared with ACDF at 2 years follow-up. Moreover, the total cervical ROM (C2–C7) after HS was preserved significantly more than the cervical ROM after ACDF (P = 0.000) at 2 years follow-up. Notably, the compensatory increase of the ROM of superior and inferior adjacent segments was significant in ACDF groups at 2-year follow-up (P < 0.01), compared with HS.
The results demonstrate that HS provides equivalent outcomes and functional recovery for cervical disc diseases, and significantly better preservation of cervical ROM compared with ACDF in 2-year follow-up. This suggests the HS is an effective alternative invention for the treatment of multilevel cervical spondylosis to preserve cervical ROM and reduce the risk of adjacent disc degeneration. Nonetheless, more well-designed studies with large groups of patients are required to provide further evidence for the benefit and reliability of HS for the treatment of cervical disk diseases.
INTRODUCTION
Anteriorcervical discectomy and fusion (ACDF) has been the standard surgical treatment for cervical spondylosis and disc diseases for decades. It is proved to achieve neural decompression, segmental stabilization, and excellent clinical outcomes.1–3 However, ACDF results in a loss of mobility at the treated segment and increases the stress on adjacent segments, which may cause more rapid disc degeneration and lead to adjacent segment diseases (ASD).4–6 In recent years, cervical disc arthroplasty (CDA) was developed as an alternative procedure to preserve segmental motion and theoretically prevent adjacent segment degeneration.7,8An accumulation of short- and intermediate-term follow-up studies9 and a few long-term studies10,11 demonstrate the legitimacy of CDA. The theoretical advantages of CDA include: preservation of the motion patterns and the range of motion (ROM), reconstitution of disc height and spinal alignment, and earlier recovery of cervical function. However, in cases of multilevel cervical spondylosis and disc diseases, the affected discs may show different types and degrees of degeneration at each level. Consequently, CDA may not be suitable for all the affected levels, for instance, the levels with no motion, a collapsed intervertebral space, facet degeneration, or bony spurs.12 Meanwhile, there is no need to fuse all the affected levels if an alternative, safe, and effective surgery can be performed, because longer fusion may cause larger loss of ROM and greater stress at adjacent levels.
The hybrid surgery (HS), combining CDA with fusion, is a novel treatment for patients with multilevel cervical degenerated disc disease in recent years. The rationale of HS comes from the notion that the most suitable treatment should be utilized at each cervical disc, respectively, based on the deferent status of cervical levels.12 Previous meta-analysis reviews focus on the comparison between single-level CDA and ACDF; however, the clinical and radiologic outcomes of HS compared with ACDF in patients with multilevel degenerated disc disease are less clear. The purpose of this meta-analysis is to compare outcomes of HS with ACDF in multilevel cervical disc diseases to evaluate the safety, efficiency, and reliability of HS.
Box 1.
no caption available
MATERIALS AND METHODS
Search Strategy
To search all of the relevant literature, we conducted a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)-compliant search of Medline, Embase, Pubmed, Cochrane library, and Cochrane Central Register of Controlled Trials (CENTRAL) by using combinations of the following keywords “hybrid surgery,” “cervical discarthroplasty,” “cervical artificial disc replacement,” “cervicalprosthesis,” “anteriorcervical discectomy and fusion,” “cervical discarthroplasty combined with fusion,” “artificial disc replacement combined with fusion,” and “total disc replacement combined with ACDF.” We searched for randomized controlled trails (RCTs), prospective and retrospective clinical controlled trials published between January, 1990 and December, 2015 that compared HS with ACDF. We placed no restrictions on the language of the publication. References cited in the relevant articles were also reviewed. All researches were carefully estimated to identify repeated data. Criteria used to define duplicate data included study centers, treatment information, and any additional inclusion criteria.
Inclusion and Exclusion Criteria
Clinical trials that conformed to the following criteria were eligible for inclusion in this study: original clinical trials; studies that include HS compared with ACDF; and studies with follow-up more than 1 year. We excluded in vitro human cadaveric biomechanical studies, articles that were duplicate reports of an earlier trial, reviews, and case-reports.
Data Extraction
Two of the authors extracted the data from eligible studies independently, discussed discrepancies, and reached conformity for all items. The indispensable information extracted from all primary researches included the titles, author names, year of publication, original country, study design, sample size, type of arthroplasty prosthesis, duration of follow-up, and outcome parameters. The corresponding author of each study was contacted to obtain any missing information if it was required. This study included 7 clinical controlled trials from different countries, in each trial the comparison of these 2 different surgical methods was studied in the same center. The extracted data were rechecked for accuracy or against the inclusion criteria by the corresponding author.
Outcomes
The following outcomes were extracted from the included publications.
Disability was assessed postoperatively using the neck disability index (NDI).
Pain was assessed using the arm and neck visual analog scale (VAS).
Total cervical ROM (C2–C7) was assessed by dynamic flexion and extension lateral cervical radiographs.
ROM of superior and inferior adjacent levels was also obtained.
Complications: heterotopic ossification (HO), adjacent disc degeneration, implant subsidence, dysphagia, dysphonia, limb symptoms, dura/spinal cord injury, and infections.
Quality of life: health score, SF-36 score, and EQ-5D.
Quality Assessment
The quality of each study was independently assessed by the authors according to the Newcastle–Ottawa Scale (NOS). The manual was downloaded from Ottawa Hospital Research Institute online. The NOS uses a pentagram symbol “fx1” rating system (a pentagram symbol stands for 1 score) to judge quality of cohorts based on 3 aspects of the cohort studies: selection, comparability, and outcomes. Scores were ranged from 0 to 9. Studies with a score ≥ 7 were regarded to be of high quality.
Statistical Analysis
We performed all meta-analyses with the STATA 12.0 (StataCorp LP, College Station, TX). For continuous outcomes, means and standard deviations were pooled to generate a mean difference, and 95% confidence intervals (CIs) were generated. For dichotomous outcomes, the risk ratio or the odds ratio and 95% CI were assessed. A probability of P < 0.05 was considered to be statistically significant. Assessment for statistical heterogeneity was calculated using the I2 tests, which described the proportion of the total variation in meta-analysis assessments from 0% to 100%.13 The random effects model was used for the analysis when an obvious heterogeneity was observed among the included studies (I2 >50%). The fixed-effects model was used when there was no significant heterogeneity between the included studies (I2 ≤50%).14 The possibility of publishing bias was not evaluated because there were less than 10 studies assessed.
We performed this article based on the methods recommended by Cochrane collaboration and reported the summarized results according to PRISMA statement. As our study was performed based on previous studies, so the ethical approval and informed consent were not required.
RESULTS
Study Characteristics
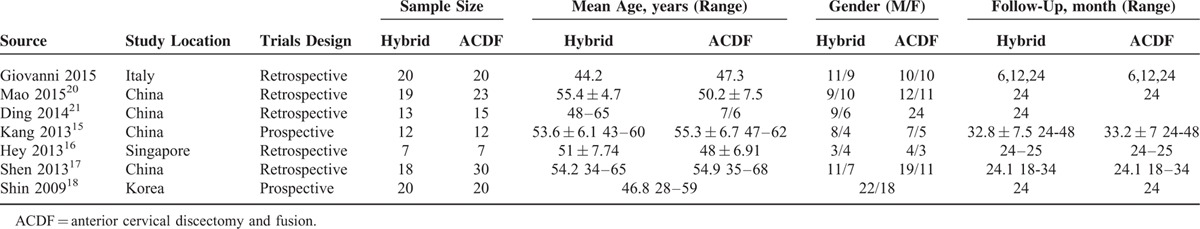
By searching in PubMed, Embase, Medline, Cochrane library, and CENTRAL, 87 studies were initially identified. A total of 74 studies were excluded because they did not meet the inclusion criteria. A flow diagram of the selection process for relative articles is shown in Figure 1. Finally, 7 studies were included into our meta-analysis and the characteristics are presented in Table 1. Out of the 7 studies, 2 are designed as prospective trials and the other 5 are retrospective. Totally, 109 patients were undergone HS and 127 patients were undergone ACDF for multilevel cervical disc diseases.
FIGURE 1.
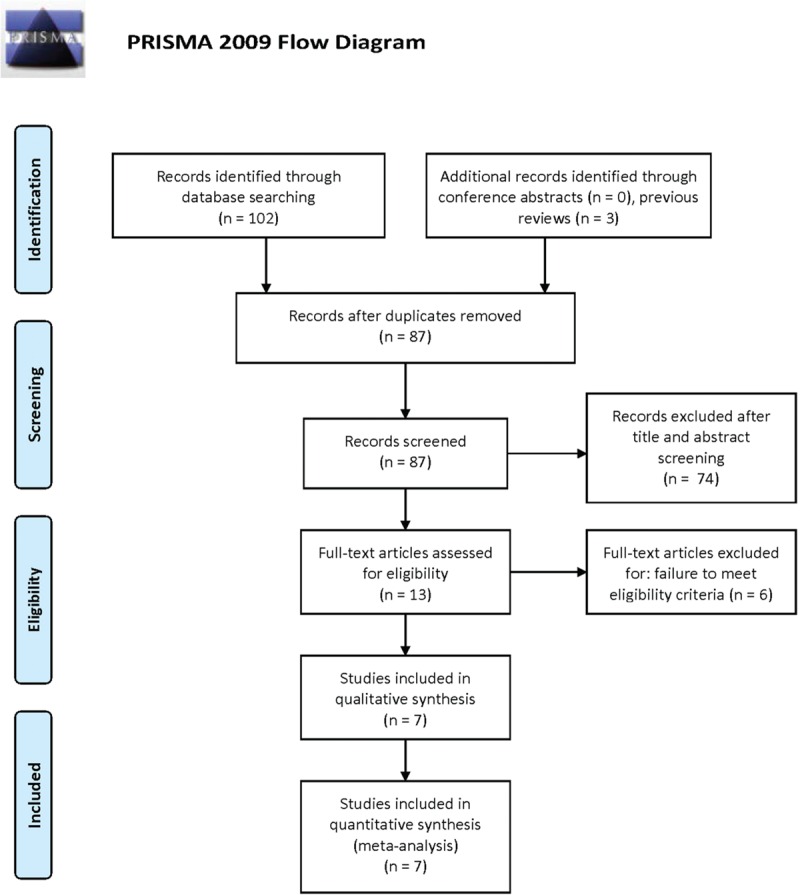
The flow diagram of the selection process for relative studies. A PRISMA-compliant search of Medline, Embase, Pubmed, Cochrane library, and CENTRAL was performed. CENTRAL = Cochrane Central Register of Controlled Trials, PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
TABLE 1.
Patient and Study Characteristics of the 4 Included Studies in the Meta-Analysis
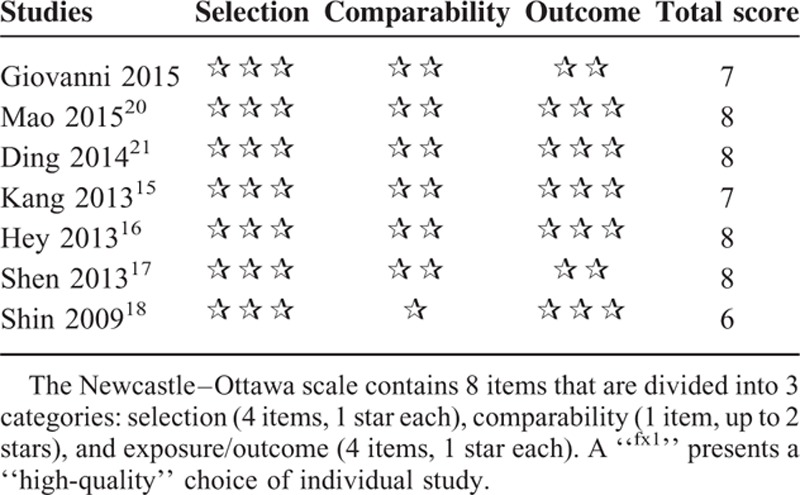
Quality Assessment
Assessment of the study specific quality scores from NOS system is shown in Table 2. The median score of included studies was 7.43, with a range from 6 to 8, and 6 of the 7 studies were identified as relatively high-quality.
TABLE 2.
Methodological Quality of Studies Included in the Meta-Analysis Assessed by the Newcastle–Ottawa Scale
Outcomes Analysis
Comparison between the HS and ACDF was based on usual clinical outcomes and functional recovery, including NDI, VAS, total cervical ROM, superior segmental ROM, inferior segmental ROM, reoperation rate, HO, and quality of life satisfaction (EQ-5D, SF-36 score, and health score). The age, gender, affected levels, NDI, and VAS score were comparable preoperatively between the 2 groups (P > 0.05) in these studies.15–21
NDI
Seven studies reported a postoperative NDI score of HS and ACDF. All of the 7 trails completed 2-year follow-up. The meta-analysis showed that the between-study heterogeneity was high (I2 = 72.8%), in this case a random effects model was used to calculate the summary risk ratio with corresponding 95% CI. The standardized mean difference (SMD) was −0.552 for the NDI (95% CI = −1.074 to −0.030; z = 2.07, P = 0.038), indicating that HS showed lower NDI than ACDF at 2-year follow-up (the diamond located on the left of the null line) (Figure 2). Through analyzing the data, we found out the high heterogeneity comes from the study of Shin et al.18 After exclusion of this study, the heterogeneity was apparently reduced (I2 = 0.0%). A fixed effects model was used to show that the SMD was −0.245 for the NDI (95% CI = −0.530 to 0.041; z = 1.68, P = 0.093), indicating there was no significant difference in NDI between the 2 groups at 2-year follow-up (Figure 3). In the forest plots, the overall effect estimate was showed by the diamond of total or subtotal 95% CIs, when overlapped the vertical line of no effect (P ≥ 0.05), indicating there was no statistically significant difference in NDI score between the 2 treatment groups.
FIGURE 2.
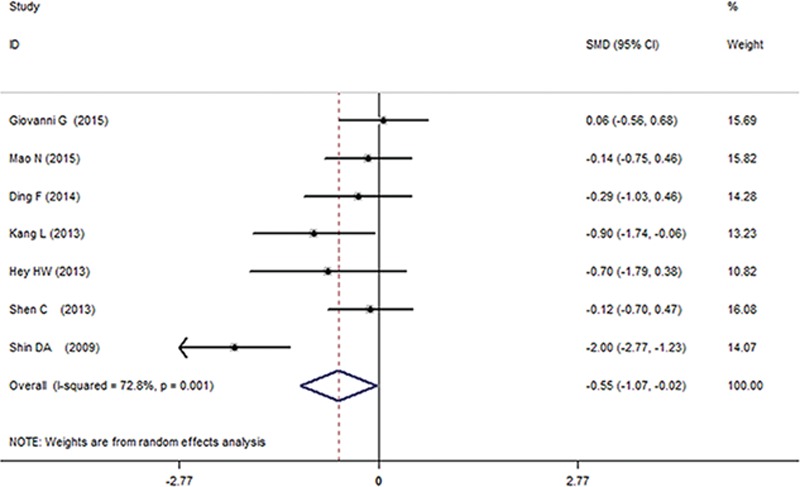
Forest plot of the meta-analysis of the NDI score comparing hybrid surgery with ACDF by a random effects model. Seven studies with high heterogeneity (I2 = 72.8%) were analyzed to calculate the summary risk ratio with corresponding 95% CI. The SMD was −0.552 for the NDI (P = 0.038, the diamond locates on the left of the null line), indicating that hybrid surgery showed lower NDI than ACDF at 2-year follow-up. ACDF = anterior cervical discectomy and fusion, CI = confidence interval, NDI = neck disability index, SMD = standardized mean difference.
FIGURE 3.
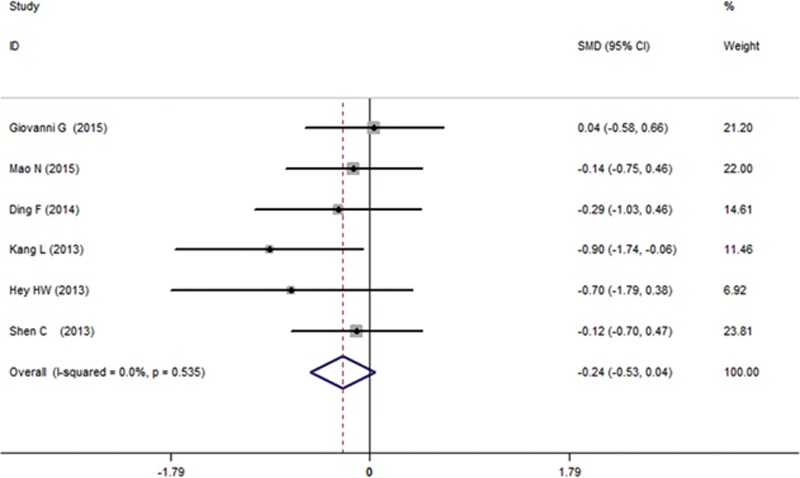
Meta-analysis of the NDI score comparing hybrid surgery with ACDF by a fixed effects model. After exclusion of high heterogeneity (I2 decreased to 0.0%), 6 studies were analyzed by a fixed effects model, indicating there was no significant difference in NDI between the hybrid surgery and ACDF at 2-year follow-up (P = 0.093, the diamond overlaps the null line). ACDF = anterior cervical discectomy and fusion, NDI = neck disability index.
VAS
Seven studies reported neck VAS score postoperatively at 2-year follow-up and the data were pooled to be analyzed. The fixed effects model was used because the heterogeneity was not significant (I2 = 5.3% in 2-year follow-up). The data at 2-year follow-up showed no significant difference in VAS score between HS and ACDF (SMD = −0.254, 95% CI = −0.517 to 0.006; z = 1.89, P = 0.058) (Figure 4).
FIGURE 4.
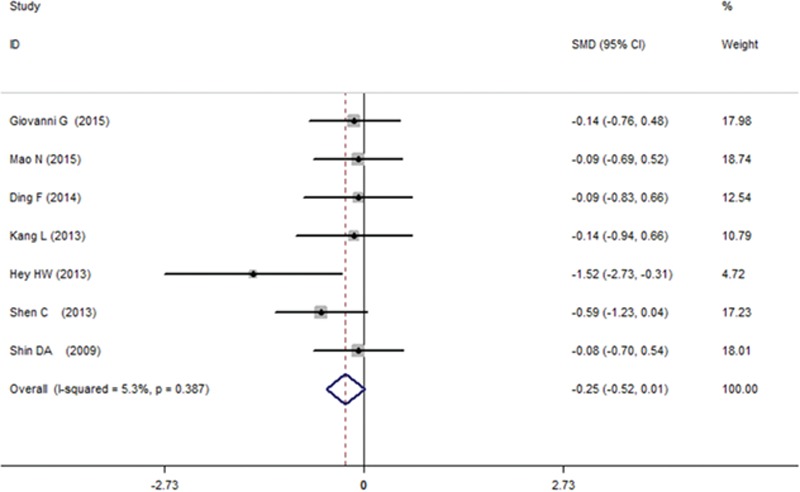
Forest plot of the meta-analysis of the VAS score comparing hybrid surgery with ACDF. The data at 2-year follow-up showed no significant difference in VAS score between hybrid surgery and ACDF (P = 0.058, the diamond overlaps the null line). ACDF = anterior cervical discectomy and fusion, VAS = visual analogue scale.
ROM of C2–C7
The total cervical ROM (C2–C7) was reported postoperatively in the 7 included studies at 2-year follow-up. Three studies15,17,18 stated there was no significant difference of cervical ROM in hybrid groups at 2-year postoperatively compared with preoperative ROM (P > 0.05), indicating HS could preserve cervical ROM effectively. On the contrary, the ROM was significantly lost postoperatively in ACDF groups at 2-year follow-up (P < 0.05). Only 1 study16 reported no significant difference of the total ROM 2 years postoperatively between HS and ACDF (P > 0.05). Our meta-analysis of the pooled data showed that HS significantly preserved more ROM of C2–C7 than ACDF at 2-year follow-up (SMD = 0.700, 95% CI = 0.332–1.068; z = 3.73, P = 0.000) (Figure 5).
FIGURE 5.
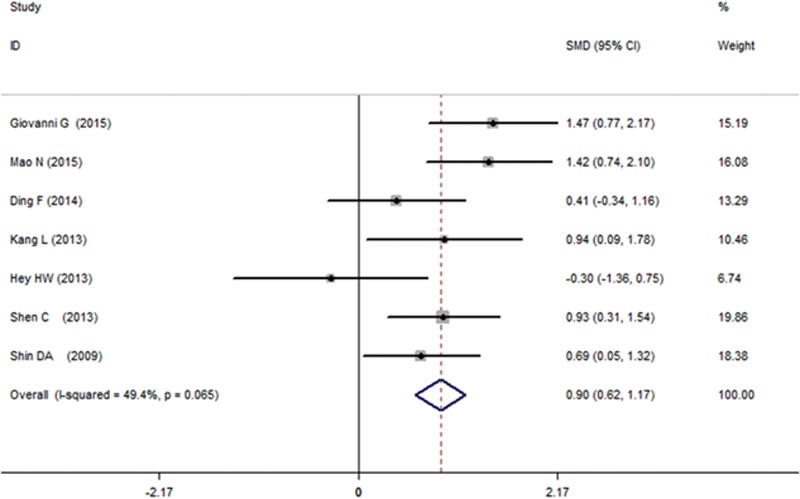
Forest plot of the meta-analysis of total cervical ROM comparing hybrid surgery with ACDF. The meta-analysis of the pooled data showed that hybrid surgery significantly preserved more ROM of C2–C7 than ACDF (2-year follow-up: P = 0.000; the diamond located on the right of the null line). ACDF = anterior cervical discectomy and fusion, ROM = range of motion.
ROM of Adjacent Segments
Four studies reported ROM of the superior and inferior adjacent segments at 2-year follow-up and 2 studies reported 1-year follow-up. They reported that the ROM of adjacent segments at 1 or 2 years after HS did not differ significantly from that preoperatively (P > 0.05). However, the superior and inferior adjacent segments in ACDF group displayed a significantly increased ROM at 2 years postoperatively when compared with preoperative ROM (P < 0.05), which was considered as a cause to the long-term cervical disc degeneration at the adjacent levels. Also the difference between the 2 groups was significant at 2-year follow-up.15,17,18 The meta-analysis showed that ACDF significantly increased ROM of the superior and inferior adjacent segments at 2 years postoperatively compared with HS. ROM of the superior segment: (2-year follow-up: SMD = −0.875, 95% CI = −1.228 to −0.521; z = 4.85, P = 0.000; the diamond located on the left of the null line) (Figure 6). ROM of the inferior segment: (2-year follow-up: SMD = −0.720, 95% CI = −1.067 to −0.373; z = 4.07, P = 0.000; the diamond located on the left of the null line) (Figure 7).
FIGURE 6.
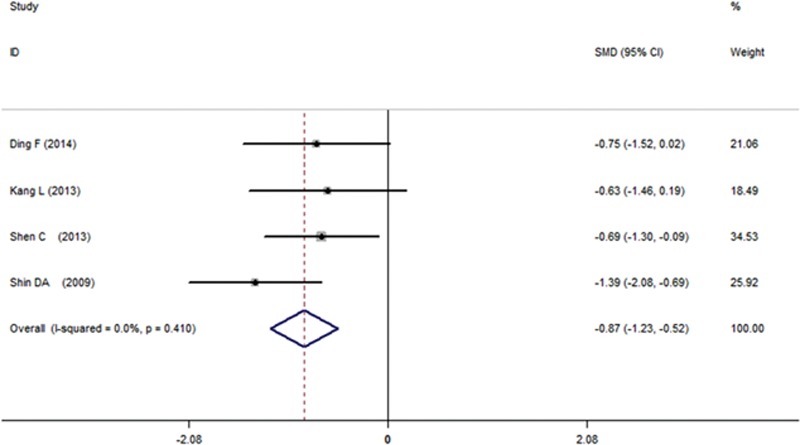
Forest plot of the meta-analysis of the ROM of superior adjacent segments in hybrid surgery group comparing with ACDF. The meta-analysis showed that ACDF significantly increased the compensatory ROM of superior adjacent segments at 2 years postoperatively, compared with hybrid surgery (P = 0.000; the diamond located on the left of the null line). ACDF = anterior cervical discectomy and fusion, ROM = range of motion.
FIGURE 7.
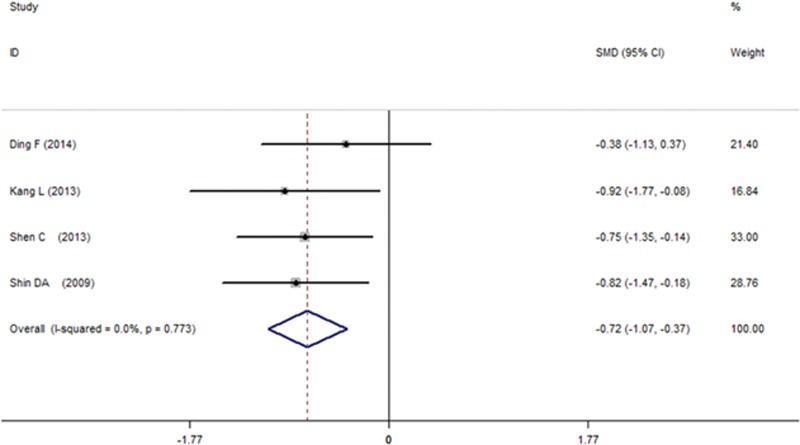
Forest plot of the meta-analysis of the inferior segmental ROM postoperatively comparing hybrid surgery with ACDF. The meta-analysis showed that ACDF also significantly increased the inferior segmental ROM at 2 years postoperatively, compared with hybrid surgery (P = 0.000; the diamond located on the left of the null line). ACDF = anterior cervical discectomy and fusion, ROM = range of motion.
Adverse Events
The included studies did not report significant difference of the complications between the HS and ACDF. Kang et al15 reported that 1 patient developed HO without the need of further intervention in HS. In ACDF group, 1 patient developed ASD with another surgical intervention after 27 months, and 1 patient with asymptomatic implant subsidence was reported. Hey et al16 reported 3 patients had residual limb symptoms that improved 6 weeks postoperatively, and 1 patient had dysphagia which resolved at 2 weeks after surgery. No significant complication was reported in the other 2 studies. Longer-term follow-up and more data were required to analyze the incidence of adverse events after HS and ACDF.
Quality of Life
Hey et al16 reported no significant difference in the quality of life between the patients with HS and ACDF. The value of EQ-5D was 0.264 ± 0.175 in HS group versus 0.689 ± 0.327 in ACDF group (P = 0.275). The health score was 80 ± 49.33 in HS group versus 70 ± 15.28 in ACDF group (P = 0.658).
DISCUSSION
ACDF has been widely accepted as a standard surgery for multilevel cervical disc diseases. However, the multilevel ACDF may cause the loss of cervical ROM and increase the stress of adjacent cervical levels, which may accelerate the degeneration of the adjacent discs. Biomechanical studies have reported that the fusion of cervical segments increased both stress and motion at adjacent levels.22–25 Moreover, clinical studies also reported that symptomatic disc degeneration at the adjacent levels were due to ACDF.26,27 Theoretically, intact segments will compensate for the motion loss of the fused levels to attempt to maintain the total ROM after ACDF.23 Therefore, multilevel fusion will cause a compensatory increase of the motion at the adjacent levels, which will lead to ASD consequently in long-term follow-up.26,28
CDA is believed to preserve the segmental motion and prevent adjacent disc degeneration compared with ACDF.29–31 Previous meta-analysis reports that the clinical outcomes of cervical arthroplasty are equivalent or superior to the outcomes of ACDF for the treatment of single-level cervical diseases.32,33 However, in most cases of multilevel cervical disc diseases, it may not be suitable for CDA at each affected disc. On the one hand, it is unnecessary to perform CDA at levels with no motion, collapsed intervertebral space, severe facet degeneration, and bony spurs. On the other hand, along-level fusion of all the affected segments are not the best choice either, because of the loss of all segmental motions and the higher risk of ASD. The design of HS is to combine CDA with fusion to treat multilevel degenerative disc disease, aiming to treat each cervical level with the most suitable choice, preserve more a better alternative treatment for multilevel cervical disc segmental ROM, and prevent long-term adjacent disc degeneration.12 However, as a relatively novel treatment, the outcomes and reliability of HS remain debated.
To investigate whether the outcomes and reliability of HS is superior to ACDF, we focused on the studies comparing the 2 methods of surgery when we searched the literature. Only 7 clinical trials met the including criteria of our meta-analysis. No RCT comparing HS with ACDF was obtained. The methodological quality assessment from NOS system showed that 6 studies were identified as relatively high-quality and one was moderate. Clinical heterogeneity was induced by different patient population, different intention of surgery, different cervical implants, and the biophysical environment in the included studies. As a result, these methodological quality deficits should be considered when interpreting the findings of this meta-analysis. The possibility of publication bias was assessed because of the small number of included studies.
In our meta-analysis, the HS showed more beneficial to the NDI compared with ACDF group. The heterogeneity was generated from the study of Shin et al,18 who showed the overall mean improvement in the NDI in hybrid group was even better versus the ACDF group with statistically significant difference (P < 0.05) at 2 years after surgery. Without this study, the heterogeneity was reduced (I2 = 0.0%). The pooled data showed there was no significant difference in NDI between hybrid and ACDF group in 2 years follow-up. Seven included studies reported neck VAS score postoperatively at 2-year follow-up. The meta-analysis showed no significant difference in VAS score between HS and ACDF at 2-year follow-up, indicating the spinal root impingement was efficiently removed after surgery. Furthermore, no significant difference in the quality of life or incidence of complications was reported between the patients with HS and ACDF in the included studies. Totally, the data of NDI, VAS, and quality of life were analyzed and our results showed that HS was as effective as ACDF to improve the outcomes and functional recovery of patients with multilevel cervical disc diseases, even better in the recovery of NDI score when using a random effects model in the meta-analysis. This demonstrates the clinical effect of cervical cord decompression of HS and ACDF are similar. However, the accident-related disc degeneration combined with instability of cervical spine may not be appropriate to perform HS because the cervical stability should be reconstructed by ACDF.
The meta-analysis demonstrated that HS preserved similar cervical ROM 2 years postoperatively, compared with preoperative ROM, whereas, the total cervical ROM was significantly decreased postoperatively at 2 years after ACDF. Furthermore, the compensatory increased ROM of the superior and inferior adjacent segments was significant at 2 years after ACDF compared with HS. Therefore, the HS, combining artificial disc replacement and fusion, largely maintains total cervical ROM and the physiological status of adjacent levels. Based on the above data, HS may provide a better alternative treatment for multilevel cervical disc diseases, decreasing the stress on adjacent segments, reducing the risk of adjacent disc degeneration, and averting the drawbacks of multilevel ACDF.
The present study is the first meta-analysis on this topic to investigate the outcomes and efficiency of HS versus ACDF for multilevel cervical disc diseases. There are several strengths and limitations of this study. The strengths include arigorous search strategy, no language limitations, article screening and methodological assessments performed in duplicate, abstracted data verified by a 2nd reviewer, and utilization of the NOS system to judge the quality of the evidence. However, several limitations of this study should be acknowledged. First, there was no RCT comparing the outcomes between HS and ACDF. The studies included were composed of 7 clinical controlled trials, the statistic quality of which was inferior to RCTs. Second, the statistical power could be improved in the future by including more studies. Owing to the small number of included studies, some parameters could not be analyzed by subgroups to avoid a high heterogeneity which may exert instability on the consistency of the outcomes. Third, the follow-up was up to 2 years, which was not enough to observe the long-term recovery and complications. In addition, the clinical heterogeneity might be caused by the different indications for surgery, various implants, and surgical technologies used at different treatment centers.
In summary, this meta-analysis indicates that the novel HS, combining CDA and fusion, provides equivalent outcomes and functional recovery for cervical disc diseases, even better recovery of NDI and preservation of cervical ROM, reducing the risk of adjacent disc degeneration. However, more well-designed studies with large groups of patients and long-term follow-up are required to provide further evidence for the benefit and reliability of HS in the treatment of multilevel cervical disc diseases.
Footnotes
Abbreviations: ACDF = anterior cervical discectomy and fusion, ASD = adjacent segment diseases, CDA = cervical disc arthroplasty, CI = confidence interval, HO = heterotopic ossification, HS = hybrid surgery, NDI = neck disability index, NOS = Newcastle–Ottawa Scale, RCT = randomized controlled trail, ROM = range of motion, RR = risk ratio, VAS = visual analog scale.
Jianfeng Zhang and Fanxin Meng contributed equally to this work and all the authors are with Master Degree.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Bohlman HH, Emery SE, Goodfellow DB, et al. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am 1993; 75:1298–1307. [DOI] [PubMed] [Google Scholar]
- 2.Bose B. Anterior cervical fusion using Caspar plating: analysis of results and review of the literature. Surg Neurol 1998; 49:25–31. [DOI] [PubMed] [Google Scholar]
- 3.Kaiser MG, Subach BR, et al. Jr HR. Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery 2002; 50:229–236.discussion 236-8. [DOI] [PubMed] [Google Scholar]
- 4.Eck JC, Humphreys SC, Lim TH, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976) 2002; 27:2431–2434. [DOI] [PubMed] [Google Scholar]
- 5.Hilibrand AS, Carlson GD, Palumbo MA, et al. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 1999; 81:519–528. [DOI] [PubMed] [Google Scholar]
- 6.Matsunaga S, Kabayama S, Yamamoto T, et al. Strain on intervertebral discs after anterior cervical decompression and fusion. Spine (Phila Pa 1976) 1999; 24:670–675. [DOI] [PubMed] [Google Scholar]
- 7.Pickett GE, Rouleau JP, Duggal N. Kinematic analysis of the cervical spine following implantation of an artificial cervical disc. Spine (Phila Pa 1976) 2005; 30:1949–1954. [DOI] [PubMed] [Google Scholar]
- 8.Sasso RC, Best NM. Cervical kinematics after fusion and Bryan disc arthroplasty. J Spinal Disord Tech 2008; 21:19–22. [DOI] [PubMed] [Google Scholar]
- 9.Clements DH, O’Leary PF. Anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 1990; 15:1023–1025. [DOI] [PubMed] [Google Scholar]
- 10.Goffin J, Van LJ, Van CF, et al. A clinical analysis of 4- and 6-year follow-up results after cervical disc replacement surgery using the Bryan Cervical Disc Prosthesis. J Neurosurg Spine 2010; 12:261–269. [DOI] [PubMed] [Google Scholar]
- 11.Robertson JT, Metcalf NH. Long-term outcome after implantation of the Prestige I disc in an end-stage indication: 4-year results from a pilot study. Neurosurg Focus 2004; 17:E10. [DOI] [PubMed] [Google Scholar]
- 12.Lee SB, Cho KS, Kim JY, et al. Hybrid surgery of multilevel cervical degenerative disc disease: review of literature and clinical results. J Korean Neurosurg Soc 2012; 52:452–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003; 327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 1959; 22:719–748. [PubMed] [Google Scholar]
- 15.Kang L, Lin D, Ding Z, et al. Artificial disk replacement combined with midlevel ACDF versus multilevel fusion for cervical disk disease involving 3 levels. Orthopedics 2013; 36:88–94. [DOI] [PubMed] [Google Scholar]
- 16.Hey HWD, Hong CC, Long AS, et al. Is hybrid surgery of the cervical spine a good balance between fusion and arthroplasty? Pilot results from a single surgeon series. Eur Spine J 2013; 22:116–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shen C, Shen Y, Ding W, et al. [Contrastive analysis of neck axial symptoms after hybrid surgery or traditional anterior cervical discectomy and fusion for treatment of two-level cervical disease]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2013; 27:58–61. [PubMed] [Google Scholar]
- 18.Shin DA, Yi S, Yoon DH, et al. Artificial disc replacement combined with fusion versus two-level fusion in cervical two-level disc disease. Spine (Phila Pa 1976) 2009; 34:1153–1159.discussion 1160-1. [DOI] [PubMed] [Google Scholar]
- 19.Grasso G. Clinical and radiological features of hybrid surgery in multilevel cervical degenerative disc disease. Eur Spine J 2015. [DOI] [PubMed] [Google Scholar]
- 20.Mao N, Wu J, Zhang Y, et al. A comparison of anterior cervical corpectomy and fusion combined with artificial disc replacement and cage fusion in patients with multilevel cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2015; 40:1277–1283. [DOI] [PubMed] [Google Scholar]
- 21.Ding F, Jia Z, Wu Y, et al. Fusion-nonfusion hybrid construct versus anterior cervical hybrid decompression and fusion: a comparative study for 3-level cervical degenerative disc diseases. Spine (Phila Pa 1976) 2014; 39:1934–1942. [DOI] [PubMed] [Google Scholar]
- 22.Cho BY, Lim J, Sim HB, et al. Biomechanical analysis of the range of motion after placement of a two-level cervical ProDisc-C versus hybrid construct. Spine (Phila Pa 1976) 2010; 35:1769–1776. [DOI] [PubMed] [Google Scholar]
- 23.Lee MJ, Dumonski M, Phillips FM, et al. Disc replacement adjacent to cervical fusion: a biomechanical comparison of hybrid construct versus two-level fusion. Spine (Phila Pa 1976) 2011; 36:1932–1939. [DOI] [PubMed] [Google Scholar]
- 24.Barrey C, Campana S, Persohn S, et al. Cervical disc prosthesis versus arthrodesis using one-level, hybrid and two-level constructs: an in vitro investigation. Eur Spine J 2012; 21:432–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Park J, Shin JJ, Lim J. Biomechanical analysis of disc pressure and facet contact force following simulated two-level cervical surgeries (fusion and arthroplasty) and hybrid surgery. World Neurosurg 2014. [DOI] [PubMed] [Google Scholar]
- 26.Jacobs W, Anderson PG, Limbeek JV, et al. Single or double-level anterior interbody fusion techniques for cervical degenerative disc disease. Cochrane Database Syst Rev 2011; CD004958. [DOI] [PubMed] [Google Scholar]
- 27.Vicario C, Lopez-Oliva F, Sánchez-Lorente T, et al. [Anterior cervical fusion with tantalum interbody implants. Clinical and radiological results in a prospective study]. Neurocirugia (Astur) 2006; 17:132–139.discussion 139. [PubMed] [Google Scholar]
- 28.Park DH, Ramakrishnan P, Cho TH, et al. Effect of lower two-level anterior cervical fusion on the superior adjacent level. J Neurosurg Spine 2007; 7:336–340. [DOI] [PubMed] [Google Scholar]
- 29.Cardoso MJ, Rosner MK. Multilevel cervical arthroplasty with artificial disc replacement. Neurosurg Focus 2010; 28:E19. [DOI] [PubMed] [Google Scholar]
- 30.Pimenta L, Mcafee PC, Cappuccino A, et al. Superiority of multilevel cervical arthroplasty outcomes versus single-level outcomes: 229 consecutive PCM prostheses. Spine (Phila Pa 1976) 2007; 32:1337–1344. [DOI] [PubMed] [Google Scholar]
- 31.Burkus JK, Traynelis VC, Haid RW, et al. Clinical and radiographic analysis of an artificial cervical disc: 7-year follow-up from the Prestige prospective randomized controlled clinical trial. J Neurosurg Spine 2014; 1–13. [DOI] [PubMed] [Google Scholar]
- 32.Dan X, Ma XL, Ma JX, et al. A meta-analysis of cervical arthroplasty compared to anterior cervical discectomy and fusion for single-level cervical disc disease. J Clin Neurosci 2013; 20:970–978. [DOI] [PubMed] [Google Scholar]
- 33.Fallah A, Akl EA, Ebrahim S, et al. Anterior cervical discectomy with arthroplasty versus arthrodesis for single-level cervical spondylosis: a systematic review and meta-analysis. PLoS One 2012; 7:e43407. [DOI] [PMC free article] [PubMed] [Google Scholar]


