Abstract
Hypertension is a typical example of long-term disease posing formidable challenges to health care. One goal of antihypertensive therapy is to achieve optimal blood pressure (BP) control and reduce co-occurring chronic conditions (multimorbidity). This study aimed to assess the influence of multimorbidity on medication adherence, and to explore the association between poor BP control and multimorbidity, with implications for hypertension management.
A cross-sectional design with multistage sampling was adopted to recruit Chinese hypertensive patients attending general out-patient clinics from 3 geographic regions in Hong Kong. A modified systemic sampling methodology with 1 patient as a sampling unit was used to recruit consecutive samples in each general out-patient clinic. Data were collected by face-to-face interviews using a standardized protocol. Poor BP control was defined as having systolic BP/diastolic BP ≥130/80 mm Hg for those with diabetes or chronic kidney disease; and ≥140/90 mm Hg for others. Medication adherence was assessed by a validated Chinese version of the Morisky Medication Adherence Scale. A simple unweighted enumeration was adopted to measure the combinations of coexisting long-term conditions. Binary logistic regression analysis was conducted with medication adherence and multimorbidity as outcome variables, respectively, after controlling for effects of patient-level covariates.
The prevalence of multimorbidity was 47.4% (95% confidence interval [CI] 45.4%–49.4%) among a total of 2445 hypertensive patients. The proportion of subjects having 0, 1, and ≥2 additional long-term conditions was 52.6%, 29.1%, and 18.3%, respectively. The overall rate of poor adherence to medication was 46.6%, whereas the rate of suboptimal BP control was 48.7%. Albeit the influence of multimorbidity on medication adherence was not found to be statistically significant, patients with poorly controlled BP were more likely to have multimorbidity (adjusted odds ratio 2.07, 95% CI 1.70–2.53, P < 0.001). Diabetes was the most prevalent concomitant long-term condition among hypertensive patients with poor BP control (38.6%, 95% CI 35.8–41.4 vs 19.7%, 95% CI 17.5–21.9 for patients with good BP control, P < 0.001).
Multimorbidity was common among hypertensive patients, and was associated with poor BP control. Subjects with coexisting diabetes, heart disease, or chronic kidney disorder should receive more clinical attention to achieve better clinical outcomes.
INTRODUCTION
Hypertension is one of the most prevalent long-term diseases seen in primary care settings in many countries. High blood pressure (BP) is often asymptomatic; yet it accounts for approximately half of the incidence of stroke and ischemic heart diseases worldwide, posing a formidable challenge to health care.1,2 There is a tendency for risk factor clustering among hypertensive patients.3,4 More importantly, the number needed to treat to prevent a cardiovascular event or a death from all causes is significantly lower among hypertensive patients with added cardiovascular diseases or other complications, when compared with hypertension alone.5 Multimorbidity, often defined as the coexistence of more than 1 long-term condition within 1 subject,6 represents a critical healthcare issue internationally.6–9 A study with a large, nationally representative sample in Scotland, UK, showed that there were more people living with multimorbidity than a single disease alone.10 The co-existing long-term conditions have many challenges,11 including higher treatment burden7and more complex healthcare need.10,12
Similar to the that in the United Kingdom, the public healthcare sector in Hong Kong provides primary care services that are heavily subsidised by the government. The majority of chronic disease care is delivered by primary care physicians working at the general out-patient clinics (GOPCs).13 The load of Chinese adult patients with hypertension is increasing.14 A Hong Kong Reference Framework for Hypertension Care for Adults in Primary Care Settings was firstly released in 2010 to enhance the disease management of hypertension in primary care.15 It consisted of a series of different modules addressing various components of disease management including prevention, early identification, clinical care, and patient empowerment. The ultimate goal of hypertension management is to obtain maximal reduction in cardiovascular morbidity and mortality through BP-lowering strategy. Antihypertensive medication therapy plays an important role to achieve optimal BP control and reduce co-occurring chronic conditions. The benefits from patients’ adherence to antihypertensive therapies could be reflected by substantial reductions in the incidence of stroke (by 35%–40%), myocardial infarction (by 20%–25%), and heart failure (by >50%).16
However, the rates of BP control remain unsatisfactory across the globe.17,18 Only 1 or 2 out of 10 patients with hypertension achieved optimal BP control worldwide.19 Of patients receiving anti-hypertensive drug therapies, many remain above recommended BP targets.20 Global statics showed that developed countries had slightly higher BP control rate in all hypertensive patients (10.8% vs 9.8% for males; and 17.3% vs 16.2% for females) when compared with developing countries; yet there were no significant differences.19 Insufficient optimal BP control remains a major challenge in the community in both developed and developing countries, particularly for healthcare settings heavily burdened with chronic disease care. Nevertheless, there is a paucity of data investigating the adherence in medicine taking in the presence of accompanying chronic conditions, and few studies have examined how BP control is linked with additional disorders among hypertensive individuals. The main objectives of our study were therefore to assess the influence of multimorbidity on medication adherence, and to explore the association between suboptimal BP control and multimorbidity among hypertensive patients seen in primary care settings.
METHODS
Settings and Sampling Method
The GOPCs in Hong Kong are the primary care provider for all citizens in the public healthcare sector, operated under the Hospital Authority in Hong Kong. GOPCs are organized into 7 hospital clusters based on 3 geographic locations—the Hong Kong Island, Kowloon, and the New Territories. The healthcare services provided in GOPCs include management of both chronic conditions and episodic illnesses, covering the entire Hong Kong population. Hypertension is one of the most long-term conditions seen in the GOPCs.13 A multistage sampling design was adopted in this study. In the first stage, 1 cluster was randomly selected in each of the 3 geographic regions (Hong Kong West cluster which operates 7 GOPCs in Hong Kong Island; Kowloon Central Cluster which operates 6 GOPCs in Kowloon; and New Territories East Cluster which operates 7 GOPCs in the New Territories). In the second stage, 1 GOPC was randomly selected in each cluster, respectively. Each GOPC clinic is managed by approximately 10 to 15 family physicians with qualified clinical training. There are around 300 to 500 patient visits daily in each clinic, excluding evening clinic sessions. In the third stage, a modified systemic random sampling methodology with 1 patient as a sampling unit was used to recruit consecutive samples in each GOPC. We divided the estimated number of hypertensive patients visiting the practice on the day of recruitment (Ntotal) by the number of hypertensive patients planned to recruit on that day (Nproposed), which gave a number X. An integer was then randomly selected from 1 to X, say 3, and the 1st, 4th, 7th, 10th, …, consecutive patients were invited to participate in the study. The total number of patients recruited in each clinic was determined by the population proportion in the respective region.
Outcome Variables and Covariates
Optimal BP control was defined as having a clinical measurement of systolic BP (SBP) <140 mm Hg and diastolic BP (DBP) <90 mm Hg, whereas for patients with diabetes mellitus or chronic kidney diseases, the corresponding threshold was SBP <130 mm Hg and DBP <80 mm Hg.15,21–24 Medication adherence was assessed by the 8-item Morisky Medication Adherence Scale (MMAS-8), which is a commonly used, validated, and self-reported adherence measure of cardiovascular mediations.25 The MMAS-8 total score was calculated by summing the values from all 8 items, with reverse coding when necessary. A cut-off score of 6 (out of a full range of 8) was used to identify optimal medication adherence (MMAS-8 score >6).26–28
A simple unweighted enumeration of the number of chronic diseases29,30 was adopted to measure the combinations of coexisting long-term conditions. International references were made to a UK definition10 and our previous study conducted in China.8 To take into account the local healthcare context, long-term conditions that were mostly self-reported by patients in a recent territory-wide survey in Hong Kong31 were also included after a panel review among a family physician, 2 public health professionals, and an epidemiologist. All conditions were physician-diagnosed, and were either prevalent among the general patients (eg, inflammatory connective tissue disorders), or concomitant comorbidities related to hypertension (eg, diabetes, lipid disorders, heart disease, cerebrovascular disease, nephritis, and chronic kidney disorder). Multimorbidity was defined as the presence of 1 or more long-term condition in addition to hypertension.32
Sample Size Estimation
The Kish L formula33: N = ([Zα/2]2 × P × [1 − P] × [1 + m])/(d2), with Zα/2 = 1.96, α = 0.05, was used to explore the prevalence of coexisting long-term conditions (multimorbidity) among hypertensive patients. We estimated the prevalence of additional chronic conditions among hypertensive patients attending primary care settings as P = 50%. The allowable error was set at 0.03 and the allowable missing data were set at 0.1. The above formula gave a minimum sample size of 1986 in total, which was also deemed adequate for logistic regression analysis based on the rule of thumb, suggesting a minimum of 10 events per predictor variable for logistic models.34
Subject and Interviewer Recruitment
When attending GOPCs, all patients need to register at the reception. After registration, patients usually queue up at the BP-measuring station in a separate area inside the waiting hall, before consulting the physician. All patients attending on the day of study recruitment were instructed to have their BP measured. We followed the inclusion criteria to invite eligible patients to participate in the study: Chinese patients aged 18 years or above; with physician-diagnosed hypertension including both essential and secondary hypertension; already on antihypertensive medication regime for at least 4 weeks before the study; mentally capable to communicate in Chinese; and willing to give written informed consent to participate in the study. Patients with newly diagnosed hypertension on the day of the recruitment were excluded as their medication adherence afterwards was unable to measure in this cross-sectional study. Eligible subjects were then interviewed by trained interviewers in a private consultation session during their clinic visits. We recruited interviewers from university medical students and conducted 4 training sessions (delivered by KQLL and HHXW) to standardize interview processes and minimize inter-interviewer variances.
A total of 2700 consecutive adult patients taking antihypertensive medication were approached and 2445 patients completed the study (488/554 in Hong Kong Island; 738/834 in Kowloon; 1219/1312 in New Territories). The overall response rate was 90.6%, with no significant differences among study sites (chi-square test P = 0.221). The sex distribution in nonrespondents (female, 58.8%) was similar compared with that in participants (female, 54.2%). The major reason for nonparticipation was that people were too busy to complete the onsite survey in the clinic.
Data Collection
A valid questionnaire was used for data collection, with its face validity assessed by the same research panel. A pilot study was conducted in 1 GOPC in October 2012 to test the reliability of the questionnaire. The field work started from October 2012 until March 2013. The questionnaire documented patients’ information on demographics, socioeconomic characteristics, and clinical details including long-term conditions and BPs. A validated Chinese version of the MMAS-8 previously developed by our research team26–28 was incorporated into the questionnaire. We followed a standard procedure of collecting BP readings in this cross-sectional survey and BP readings on the day of patient recruitment onsite at the clinic for all study participants were used. All BP were measured at least 1 hour after the subject's last meal and at least 30 minutes after smoking or consumption of alcohol or caffeinated beverages. Before BP measurement, participants were instructed to rest in a sitting position for at least 10 minutes. BP was measured by frontline nurses using a regularly calibrated random-zero sphygmomanometer in the right arm, with an appropriately sized cuff in a clinically standardized manner. The first and fifth Korotkoff sounds were recorded as SBP and DBP, respectively. For all study participants, BP measurements were conducted 3 times in a sitting posture, and the mean of 3 BP readings was calculated to determine whether BP targets were achieved. The anthropometric measurements and categorization of body mass index (BMI) levels followed a standard protocol used in our previous studies.35,36 Body weight was measured by a regularly calibrated weight scale while on light clothing, and the height was measured by a standiometer without wearing shoes.
A research nurse further referred to the electronic health record for study subjects who self-reported the presence of comorbid conditions in addition to hypertension to improve the validity of patients’ reported additional conditions through cross-check. Any discrepancies were addressed by the on-site attending physician. Each interview lasted for approximately 15 to 20 minutes.
Statistical Analysis
The characteristics of all patients were compared among those having 0, 1, and ≥2 additional long-term conditions by 2-tailed chi-square test (for categorical variables) and independent Student t test or analysis of variance (for continuous variables when appropriate). Binary logistic regression equations with backward stepwise algorithm were modeled with medication adherence and the presence of multimorbidity (having 1 or more long-term conditions in addition to hypertension) as outcome variables, respectively. Medication adherence and BP control were also tested in 2 separate logistic regression models for their association with multimorbidity. We examined the absence of multicollinearity to ensure the robustness of all regression models. Any P values ≤0.05 were considered statistically significant. All statistical analyses were performed using IBM SPSS Statistics 20.0 (SPSS, Chicago, IL).
Ethics Review
The study was conducted with the understanding and the written consent of each participant. The ethical approval of the study was obtained from the Cluster Research Ethics Committee of the Hospital Authority, Hong Kong (CREC-2012.346; KC/KE-12–0185/ER-1; UW13–016) and the Survey and Behavioural Research Ethics Committee of The Chinese University of Hong Kong. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki.
RESULTS
A total of 2445 subjects participated in the study, with an average age of 65.3 years (SD 11.0). The crude prevalence of multimorbidity was 47.4% (1159/2445), with 95% confidence interval (CI) of 45.4% to 49.4% among all study subjects. The proportion of hypertensive patients having 0, 1, and ≥2 additional long-term conditions was 52.6%, 29.1%, and 18.3%, respectively. Slightly more than half (53.4%) of patients had satisfactory medication adherence and 51.3% had optimal control of both SBP and DBP simultaneously. Higher crude proportion of multimorbidity was observed among study participants who were older (aged 70 years and above); female sex; having lower education level; retired or part-time employed; having lower monthly household income; single living without companion; longer duration and greater categories of antihypertensive drug use (Table 1).
TABLE 1.
Characteristics of Hypertensive Patients by the Number of Coexisting Long-term Conditions
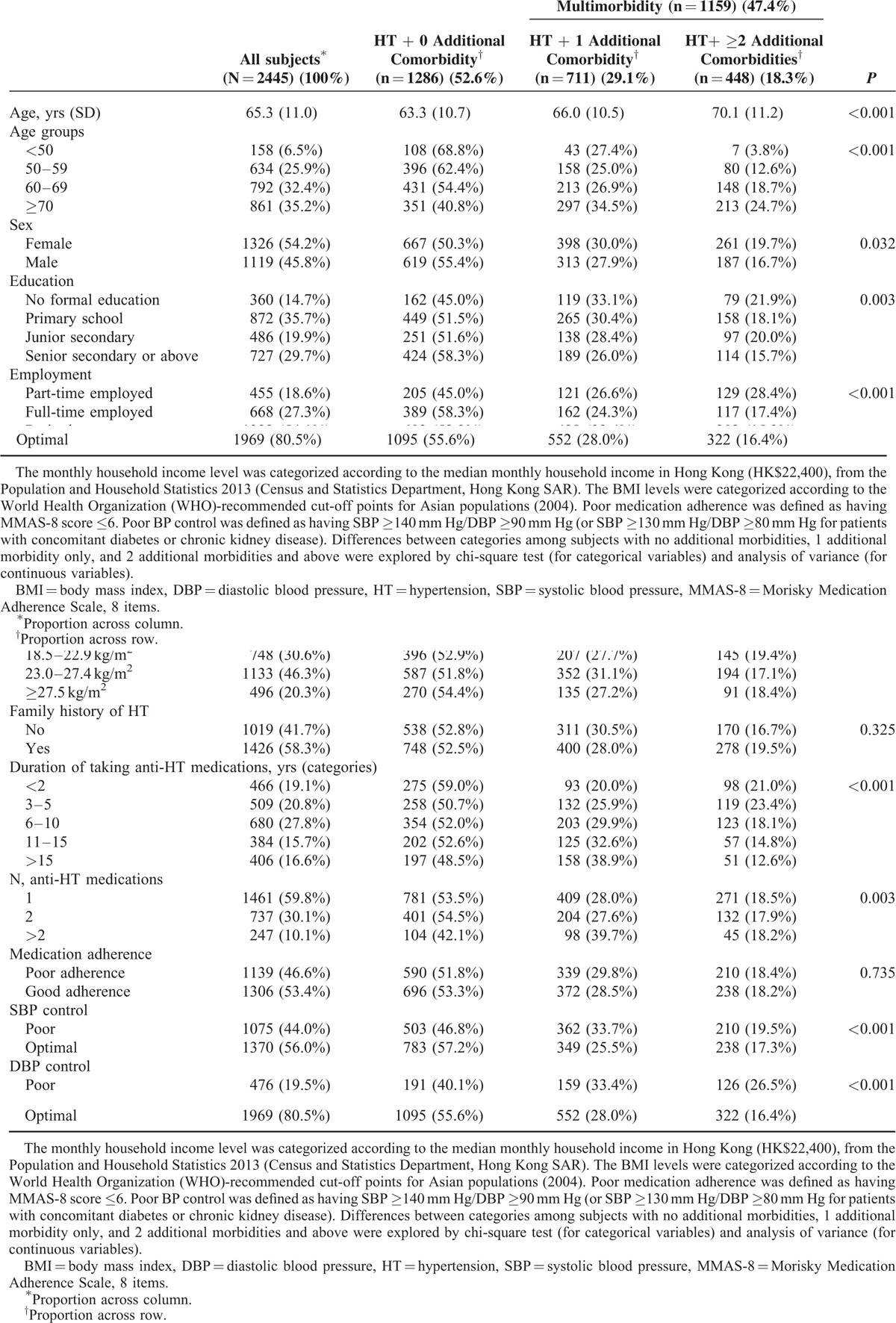
The crude percentage of subjects having multimorbidity was not significantly different between hypertensive patients with poor versus good medication adherence (48.2% [549/1139] vs 46.7% [610/1306]; P = 0.735), but was significantly higher among those who had poor SBP control (53.2% [572/1075] vs 42.8% [587/1370]; P < 0.001) and poor DBP control (59.9% [285/476] vs 44.4% [874/1969]; P < 0.001) (Table 1). When compared with hypertensive patients having poor BP control, those with satisfactory BP control had significantly lower percentage of having coexisting long-term conditions (22.6%, 95% CI 20.3–24.9 for patients with poor medication adherence; and 19.8%, 95% CI 17.5–22.2 for patients with good medication adherence) (Figure 1).
FIGURE 1.
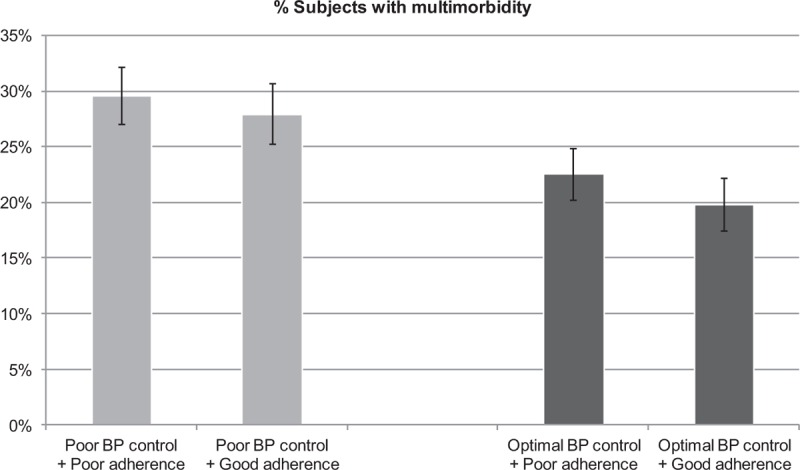
Proportion of subjects having multimorbidity by medical adherence and blood pressure (BP) control.
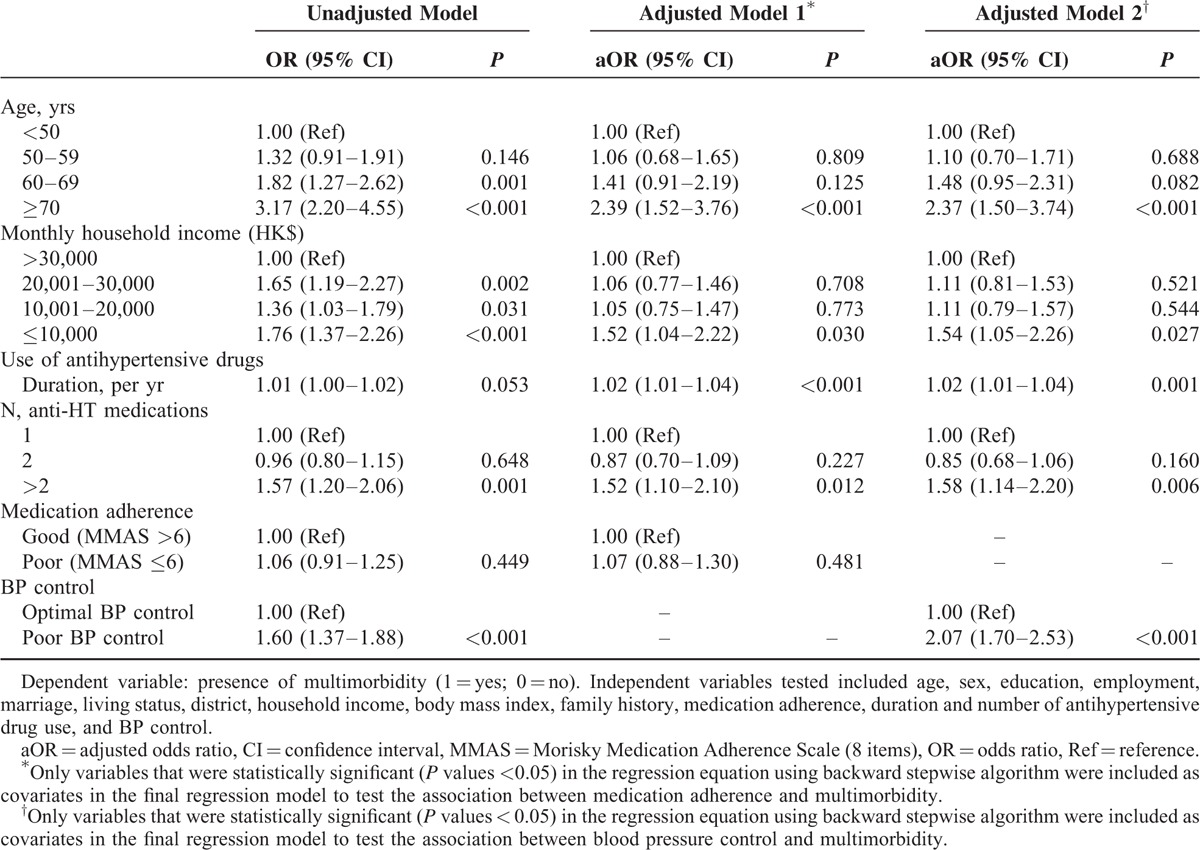
From binary logistic regression analysis, it was found that having multimorbidity seemed to be unlikely to achieve good adherence in antihypertensive medicine taking, although such influence was not found to be statistically significant (adjusted odds ratio [aOR] 0.97, 95% CI 0.80–1.19, P = 0.802) (Table 2). On the other hand, we found that the presence of accompanying long-term conditions was significantly associated with poor BP control (aOR 2.07, 95% CI 1.70–2.53, P < 0.001), whereas no significant association was detected between poor medication adherence level and multimorbidity (aOR 1.07, 95% CI 0.88–1.30, P = 0.481). Older age (≥70 years), lower monthly household income level, longer duration of antihypertensive drug use, and higher number of drug use were common contributing factors that were significantly associated with the presence of multimorbidity in both models, with medication adherence and BP control as covariates, respectively (Table 3).
TABLE 2.
Influence of Multimorbidity on Medication Adherence by Logistic Regression Analysis
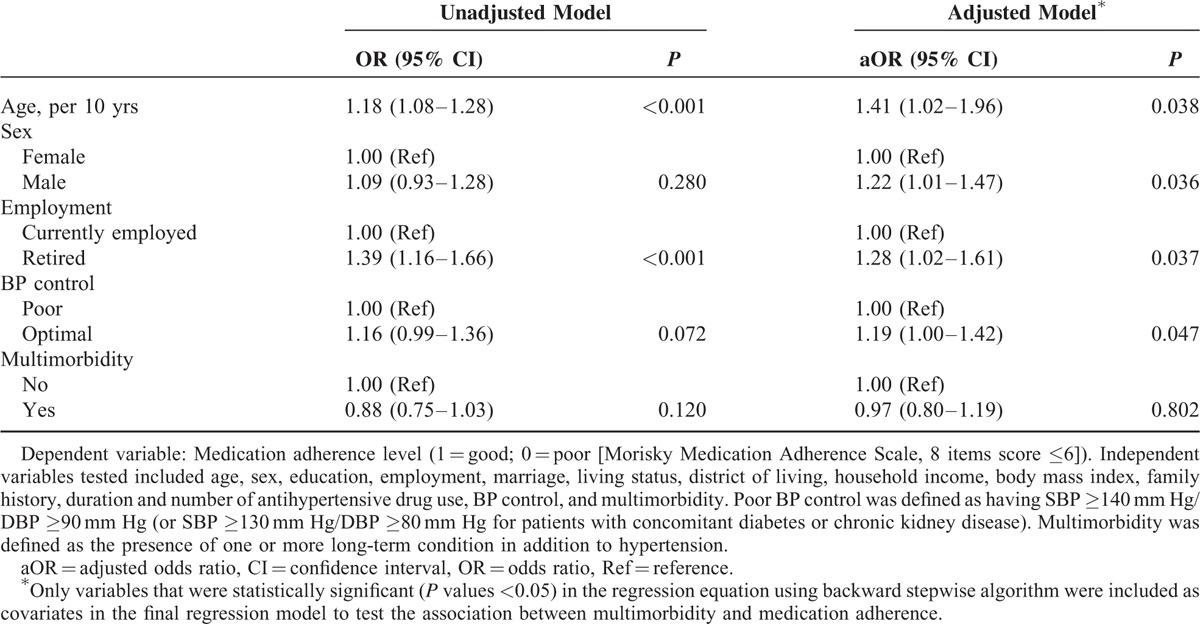
TABLE 3.
Factors Association With the Presence of Multimorbidity Among Hypertensive patients
Hypertensive subjects with poor BP control had higher prevalence of additional long-term conditions, particularly with regard to diabetes mellitus (38.6%, 95% CI 35.8–41.4 vs 19.7%, 95% CI 17.5–21.9), heart disease (19.2%, 95% CI 17.0–21.4 vs 11.9%, 95% CI 10.0–13.7), and nephritis and chronic kidney disorder (14.5%, 95% CI 12.5–16.5 vs 9.1%, 95% CI 7.5–10.7) when compared with patients whose BP levels were below the levels considered optimal. Diabetes mellitus was the most prevalent concomitant long-term condition among hypertensive patients with poor BP control (Figure 2).
FIGURE 2.
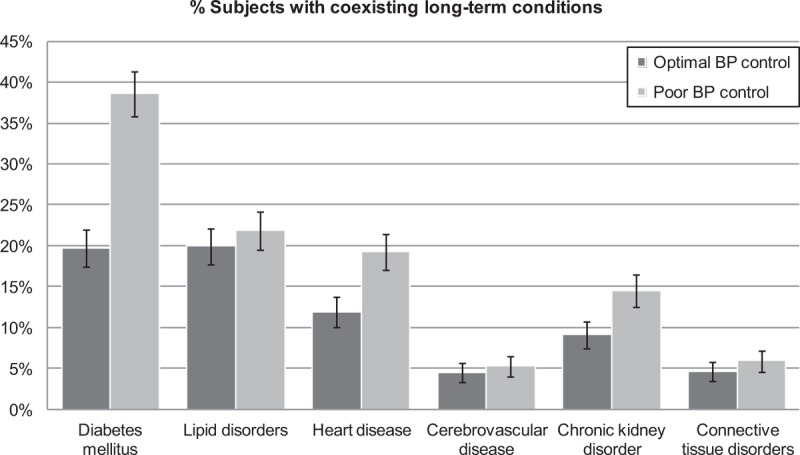
Prevalence of major coexisting long-term conditions among participants by blood pressure (BP) control.
DISCUSSION
Statement of Principal Findings
From this cross-sectional study of more than 2440 Chinese hypertensive patients, it was found that nearly half of the adult hypertensive subjects had coexisting long-term conditions. The presence of multimorbidity was independently associated with advanced age, lower household income, longer duration of antihypertensive medication use, higher number of drugs taken, and poor BP control. We did not observe significant influence of multimorbidity on patients’ adherence to antihypertensive medications; whereas individuals with BP above the levels considered optimal were significantly more likely to suffer from coexisting long-term conditions such as diabetes, heart disease, or chronic kidney disorder.
Relationship With Literature and Explanation of Findings
Patients with multiple long-term conditions are very frequently encountered in routine clinical practice particularly among those with hypertension. Previous investigations on the determinants of medication adherence and BP control in the same Hong Kong primary care population suggested the necessity for further research from a multimorbidity perspective.37 National data collected in Scotland, UK, showed that 78% of hypertensive patients seen in general practice had at least 1 other long-term conditions from a list of 40 chronic conditions.10 There have also been heterogeneous methods used across observational studies to define multimorbidity among different study populations. An earlier systematic review38 showed that the proportion of multimorbidity increased as age advanced, and its prevalence in older persons ranged from 55% to 98%, suggesting considerable disease complexity and enormous burden on health care. In our study, the crude proportion of multimorbidity was lower than that reported in the United Kingdom, which may be due (at least in part) to the differences in the number of chronic diseases considered and the data collection approach used. We found that the household income level was an independent factor associated with multimorbidity, meaning that hypertensive subjects living in deprived household were more likely to confront multiple comorbid conditions. The findings are compatible with previous studies in the western countries, reporting that with higher degrees of deprivation, the mix of multiple medical problems become greater,9,10 or what has been recognized as the “inverse care law.”39
There is a large volume of epidemiological evidence that consistent BP control is linked with improved cardiovascular outcome.40 The Danish General Practice Database study previously evaluated the association between multimorbidity and rate of BP control in a large cohort of hypertensive patients which showed that the BP control rates differed substantially between patients with comorbidities.32 In particular, only 16.5% of hypertensive patients with diabetes in Danish general practice had BP below 130/80 mm Hg, which was a recommended therapeutic target for individuals with diabetes mellitus.15,21–24 In our study where the same BP cut-off value was used, the findings that the prevalence of diabetes was the highest among individuals with poor BP control were complementary to earlier observations in Denmark. Another study conducted by the British Hypertension Society pointed out that the BP of <130/80 mm Hg as a rigorous target in patients with diabetes may be more difficult to reach than BP targets of <140/90 mm Hg.41 Further research might need to identify the ideal BP level at which maximum protection against diabetic complications is conferred, and below which the reduction no longer delivers a benefit that exceeds risk42 for the diabetes population of different age groups, particularly for the Asian population. Another explanation could be that some physicians may consider 140/90 mm Hg as “close enough to target,” and with clinical inertia, physicians prefer to only deal with the most pressing or symptomatic problem alone while observing if the BP level is not very high. It is also possible that the perceptions of physicians towards optimal BP control may be different between patients with or without multimorbidities.43 In contrast to the methodology used in a more recent UK study in which multiple SBP measures collected from the Lambeth DataNet were analyzed as continuous variables,44 it is worth noting that our study sought to identify success or failure in achieving the BP target. The perspective on BP control provides real-world clinical insights as lowering BP to particular target values often represents a more difficult issue. Although there is a need to exercise some caution in the interpretation as we were unable to comprehensively retrieve from the entire subjects a whole spectrum covering all previous BP measurements in past visits, the evidence from our findings suggests that the focus on achieving good BP control in the Chinese population should not be neglected.
Previous literature has suggested that patient nonadherence to prescribed antihypertensive therapy could serve as a major obstacle to achieving good clinical outcomes.45 In our study, however, we did not detect a significant association between medication adherence and the presence of multimorbidity. It might be that having accompanying chronic conditions requires higher intensity and complexity of treatment regime such that polypharmacy and multiple daily dosing may reduce the drug adherence.45,46 One may argue otherwise that the presence of multimorbidity may be linked with increased adherence to the medication because of the perceived seriousness of multiple conditions47; despite that, we did not collect such information. Nevertheless, it seems likely that hypertensive subjects were prone to have poor adherence to medications in the presence of concomitant long-term conditions based on our study findings, albeit such association was not statistically significant. We therefore speculated that the association might be mediated by factors such as prescription pattern, treatment intensification, or health behaviors,48 which needs further in-depth causal investigation. The US National Health and Nutrition Examination Study depicted a picture of unsatisfactory BP control, despite the awareness of hypertension among people who were more likely to be taking antihypertensive medications.49 Our results that coexisting diabetes, heart disease, or chronic kidney disorder was more prevalent in people with poor BP control also echoed earlier US studies in which adults with diabetes had the greatest population burden of uncontrolled BP, followed by adults with chronic kidney disease and cardiovascular disease.49 A study in Australia showed that multimorbidity could lead to difficulties in pharmaceutical care management in primary care.50 Given that most medication treatments are delivered according to single-disease-oriented guidelines,51 the exploration of appropriateness of medication prescriptions among multimorbid hypertensive patients is warranted.
Strengths and Limitations of the Study
This study adopted a multistage sampling design to recruit hypertensive patients in the public primary care setting of Hong Kong. Multimorbidity was assessed using a well-recognised methodology supplemented by physician documentations. Medication adherence was evaluated by a validated tool, and BP was examined in a standardized approach. However, a number of limitations should be addressed. Firstly, it should be noted that we only included 1 GOPC in each geographic region, which could limit the generalizability of our findings to the entire population of Hong Kong. Secondly, the cross-sectional design could only evaluate association, instead of cause-and-effect relationships. Thirdly, a patient self-report survey restricted the inclusion of questions on physician-prescribing patterns that might differ among physicians and regions, and the discrimination between essential and secondary hypertension was not accounted for in this study. In addition, recall bias might exist in using MMAS-8 as a self-report measure, and the Hawthorne effect may also bias patients’ answers in reporting their adherence to antihypertensive medications. Last but not the least, subjects’ ambulatory or home BP readings in out-of-clinic settings52 were not monitored in our study, and thus the determination of optimal BP control was based on clinic-based measurement alone instead of an average over a period of time. One may argue that people with ’masked hypertension’ would be misclassified, albeit this phenomenon was seen much more frequently in younger patients. Given that those under 50 years of age only accounted for a very small proportion (6.5%), the effects of possible misclassification of ’masked hypertension’ on the study results were therefore considered minimum.
Conclusions and Future Prospects
This study indicated that hypertensive patients presented with poor BP control should be evaluated in a more meticulous manner for the possible presence of other coexisting medical conditions, in particular, diabetes. On the other hand, hypertensive patients with multimorbidity should have their BP monitored more closely as they tended to have poorer BP control. This has important implications for both policy makers and physicians, because the high prevalence of multimorbidity points towards the need to prioritize more healthcare resources to address the multiple medical conditions among hypertensive patients. It was well-recognised that earlier detection of shared risk factors could lead to better clinical outcomes by reducing long-term complications.53 From a healthcare system's point of view, health services delivery should be reviewed and oriented to address the rising challenges of multimorbidity.54,55 These include combined efforts to enhance continuity of care, coordination among different healthcare professionals, and the promulgation of adopting holistic care models. The findings also call for more prospective studies to evaluate the effect of multidrug prescribing patterns on multimorbidity, and the best primary care-based interventional strategies to handle the complexity of hypertension management which demands urgent attention.
Acknowledgments
We thank healthcare staff from Central Kowloon Health Centre (Kowloon), Wong Siu Ching Family Medicine Centre (New Territories), and Tsan Yuk Hospital-General Outpatient Clinics (Hong Kong Island), whose support ensured high-quality data collection.
Footnotes
Abbreviations: BP = blood pressure, MMAS = Morisky Medication Adherence Scale.
The result of this study was presented at the American Heart Association High Blood Pressure Research 2014 Scientific Sessions, September 9–12, 2014, San Francisco, USA: 14-HBPR-A-179-AHA-ABSTRACT410.
HHXW conceived the study. Data collection was mainly done by KQLL, HHXW, and GKYL. YTL cleaned and analysed the data. HHXW wrote the first draft of the report. YTL and HHXW revised subsequent draft. All authors contributed to and approved the final report.
This work was supported by the Direct Grant, Faculty of Medicine, The Chinese University of Hong Kong. HHXW was supported by New Faculty Start-Up Research Fund, Sun Yat-Sen University (51000-18821202). The funding body has no role in the design of the study, collection and analysis of data, and decision to publish.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Bromfield S, Muntner P. High blood pressure: the leading global burden of disease risk factor and the need for worldwide prevention programs. Curr Hypertens Rep 2013; 15:134–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lawes CMM, Vander Hoorn S, Rodgers A, et al. Global burden of blood-pressure-related disease, 2001. Lancet 2008; 371:1513–1518. [DOI] [PubMed] [Google Scholar]
- 3.Ohta Y, Tsuchihashi T, Onaka U, et al. Clustering of cardiovascular risk factors and blood pressure control status in hypertensive patients. Intern Med 2010; 49:1483–1487. [DOI] [PubMed] [Google Scholar]
- 4.Wong MCS, Wang HHX, Cheung CSK, et al. Factors associated with multimorbidity and its link with poor blood pressure control among 223,286 hypertensive patients. Int J Cardiol 2014; 177:202–208. [DOI] [PubMed] [Google Scholar]
- 5.Ogden LG, He JA, Lydick E, et al. Long-term absolute benefit of lowering blood pressure in hypertensive patients according to the JNC VI risk stratification. Hypertension 2000; 35:539–543. [DOI] [PubMed] [Google Scholar]
- 6.Fortin M, Bravo G, Hudon C, et al. Prevalence of multimorbidity among adults seen in family practice. Ann Fam Med 2005; 3:223–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gallacher KI, Batty G, McLean G, et al. Stroke, multimorbidity and polypharmacy in a nationally representative sample of 1,424,378 patients in Scotland: implications for treatment burden. BMC Med 2014; 12:151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang HHX, Wang JJ, Wong SYS, et al. Epidemiology of multimorbidity in China and implications for the healthcare system: cross-sectional survey among 162,464 community household residents in southern China. BMC Med 2014; 12:188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang HHX, Wang JJ, Lawson KD, et al. Relationships of multimorbidity and income with hospital admissions in 3 health care systems. Ann Fam Med 2015; 13:164–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012; 380:37–43. [DOI] [PubMed] [Google Scholar]
- 11.Stange KC. In this issue: challenges of managing multimorbidity. Ann Fam Med 2012; 10:2–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bayliss EA, Ellis JL, Steiner JF. Barriers to self-management and quality-of-life outcomes in seniors with multimorbidities. Ann Fam Med 2007; 5:395–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lo YY, Lam CL, Mercer SW, et al. Patient morbidity and management patterns of community-based primary health care services in Hong Kong. Hong Kong Med J 2011; 17:33–37. [PubMed] [Google Scholar]
- 14.Wong MCS, Wang HHX, Leung MCM, et al. The rising prevalence of self-reported hypertension among Chinese subjects: a population-based study from 121,895 household interviews. QJM-An Int J Med 2015; 108:9–17. [DOI] [PubMed] [Google Scholar]
- 15.Hong Kong Reference Framework for Hypertension Care for Adults in Primary Care Settings. Task Force on Conceptual Model and Preventive Protocols of the Working Group on Primary Care. The Government of Hong Kong Special Administrative Region. 2010. [Google Scholar]
- 16.Neal B, MacMahon S, Chapman N, et al. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Lancet 2000; 356:1955–1964. [DOI] [PubMed] [Google Scholar]
- 17.Whelton PK. The elusiveness of population-wide high blood pressure control. Annu Rev Public Health 2015; 36:109–130. [DOI] [PubMed] [Google Scholar]
- 18.Wolf-Maier K, Cooper RS, Banegas JR, et al. Hypertension, prevalence and blood pressure levels in 6 European countries, Canada, and the United States. JAMA 2003; 289:2363–2369. [DOI] [PubMed] [Google Scholar]
- 19.Pereira M, Lunet N, Azevedo A, et al. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens 2009; 27:963–975. [DOI] [PubMed] [Google Scholar]
- 20.Guo F, He D, Zhang W, et al. Trends in prevalence, awareness, management, and control of hypertension among United States adults, 1999 to 2010. J Am Coll Cardiol 2012; 60:599–606. [DOI] [PubMed] [Google Scholar]
- 21.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013; 34:2159–2219. [DOI] [PubMed] [Google Scholar]
- 22.Shimamoto K, Ando K, Fujita T, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res 2014; 37:253–387. [DOI] [PubMed] [Google Scholar]
- 23.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. JAMA 2003; 289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 24.Wang JG. Chinese hypertension guidelines. Pulse (Basel) 2015; 3:14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morisky DE, Ang A, Krousel-Wood M, et al. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens 2008; 10:348–354. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 26.Lee GKY, Wang HHX, Liu KQL, et al. Determinants of medication adherence to antihypertensive medications among a Chinese population using Morisky Medication Adherence Scale. Plos One 2013; 8:e62775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wong MCS, Liu KQL, Wang HHX, et al. Effectiveness of a pharmacist-led drug counseling on enhancing antihypertensive adherence and blood pressure control: a randomized controlled trial. J Clin Pharmacol 2013; 53:753–761. [DOI] [PubMed] [Google Scholar]
- 28.Wong MCS, Wu CHM, Wang HHX, et al. Association between the 8-item Morisky Medication Adherence Scale (MMAS-8) score and glycaemic control among Chinese diabetes patients. J Clin Pharmacol 2015; 55:279–287. [DOI] [PubMed] [Google Scholar]
- 29.Huntley AL, Johnson R, Purdy S, et al. Measures of multimorbidity and morbidity burden for use in primary care and community settings: a systematic review and guide. Ann Fam Med 2012; 10:134–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fortin M, Stewart M, Poitras ME, et al. A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med 2012; 10:142–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thematic Household Survey (2011), Census and Statistics Department, The Government of Hong Kong Special Administrative Region. 2011. [Google Scholar]
- 32.Paulsen MS, Andersen M, Thomsen JL, et al. Multimorbidity and blood pressure control in 37,651 hypertensive patients from Danish general practice. J Am Heart Assoc 2013; 2:e004531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kish L. Survey Sampling. 1965; New York: Chichester: Wiley, (1995 [printing]). [Google Scholar]
- 34.Peduzzi P, Concato J, Kemper E, et al. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 1996; 49:1373–1379. [DOI] [PubMed] [Google Scholar]
- 35.Wang HHX, Wong MCS, Mok RY, et al. Factors associated with grade 1 hypertension: implications for hypertension care based on the Dietary Approaches to Stop Hypertension (DASH) in primary care settings. BMC Fam Pract 2015; 16:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wong MCS, Wang HHX, Kwan MWM, et al. Dietary counselling has no effect on cardiovascular risk factors among Chinese Grade 1 hypertensive patients: a randomized controlled trial. Eur Heart J 2015; 36:2598–2607. [DOI] [PubMed] [Google Scholar]
- 37.Kang CD, Tsang PP, Li WT, et al. Determinants of medication adherence and blood pressure control among hypertensive patients in Hong Kong: a cross-sectional study. Int J Cardiol 2015; 182:250–257. [DOI] [PubMed] [Google Scholar]
- 38.Marengoni A, Angleman S, Melis R, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev 2011; 10:430–439. [DOI] [PubMed] [Google Scholar]
- 39.Mercer SW, Watt GC. The inverse care law: clinical primary care encounters in deprived and affluent areas of Scotland. Ann Fam Med 2007; 5:503–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meredith PA, Lloyd SM, Ford I, et al. Importance of sustained and “tight” blood pressure control in patients with high cardiovascular risk. Blood Press 2016; 25:74–82. [DOI] [PubMed] [Google Scholar]
- 41.Williams B, Poulter NR, Brown MJ, et al. Guidelines for management of hypertension: report of the fourth working party of the British Hypertension Society, 2004-BHS IV. J Hum Hypertens 2004; 18:139–185. [DOI] [PubMed] [Google Scholar]
- 42.Lipman ML, Schiffrin EL. What is the ideal blood pressure goal for patients with diabetes mellitus and nephropathy? Curr Cardiol Rep 2012; 14:651–659. [DOI] [PubMed] [Google Scholar]
- 43.Ogedegbe G. Barriers to optimal hypertension control. J Clin Hypertens (Greenwich) 2008; 10:644–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sarkar C, Dodhia H, Crompton J, et al. Hypertension: a cross-sectional study of the role of multimorbidity in blood pressure control. BMC Fam Pract 2015; 16:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Krousel-Wood M, Thomas S, Muntner P, et al. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol 2004; 19:357–362. [DOI] [PubMed] [Google Scholar]
- 46.Daugherty SL, Powers JD, Magid DJ, et al. The association between medication adherence and treatment intensification with blood pressure control in resistant hypertension. Hypertension 2012; 60:303–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.DiMatteo MR, Haskard KB, Williams SL. Health beliefs, disease severity, and patient adherence: a meta-analysis. Med Care 2007; 45:521–528. [DOI] [PubMed] [Google Scholar]
- 48.Margolis KL, Asche SE, Bergdall AR, et al. A successful multifaceted trial to improve hypertension control in primary care: Why did it work? J Gen Intern Med 2015; 30:1665–1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bertoia ML, Waring ME, Gupta PS, et al. Implications of new hypertension guidelines in the United States. Hypertension 2011; 58:361–366. [DOI] [PubMed] [Google Scholar]
- 50.Roughead EE, Barratt JD, Gilbert AL. Medication-related problems commonly occurring in an Australian community setting. Pharmacoepidemiol Drug Saf 2004; 13:83–87. [DOI] [PubMed] [Google Scholar]
- 51.Tinetti ME, Bogardus ST, Jr, Agostini JV. Potential pitfalls of disease-specific guidelines for patients with multiple conditions. N Engl J Med 2004; 351:2870–2874. [DOI] [PubMed] [Google Scholar]
- 52.Sharman JE, Blizzard L, Kosmala W, et al. Pragmatic method using blood pressure diaries to assess blood pressure control. Ann Fam Med 2016; 14:63–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wallace E, Salisbury C, Guthrie B, et al. Managing patients with multimorbidity in primary care. BMJ 2015; 350:h176. [DOI] [PubMed] [Google Scholar]
- 54.Mercer SW, Gunn J, Bower P, et al. Managing patients with mental and physical multimorbidity. BMJ 2012; 345:e5559. [DOI] [PubMed] [Google Scholar]
- 55.Moffat K, Mercer SW. Challenges of managing people with multimorbidity in today's healthcare systems. BMC Fam Pract 2015; 16:129. [DOI] [PMC free article] [PubMed] [Google Scholar]


