Supplemental Digital Content is available in the text
Abstract
Presently, there is no recommendation on how to assess functional status of chronic obstructive pulmonary disease (COPD) patients. This study aimed to summarize and systematically evaluate these measures.
Studies on measures of COPD patients’ functional status published before the end of January 2015 were included using a search filters in PubMed and Web of Science, screening reference lists of all included studies, and cross-checking against some relevant reviews. After title, abstract, and main text screening, the remaining was appraised using the Consensus-based Standards for the Selection of Health Measurement Instruments (COSMIN) 4-point checklist. All measures from these studies were rated according to best-evidence synthesis and the best-rated measures were selected.
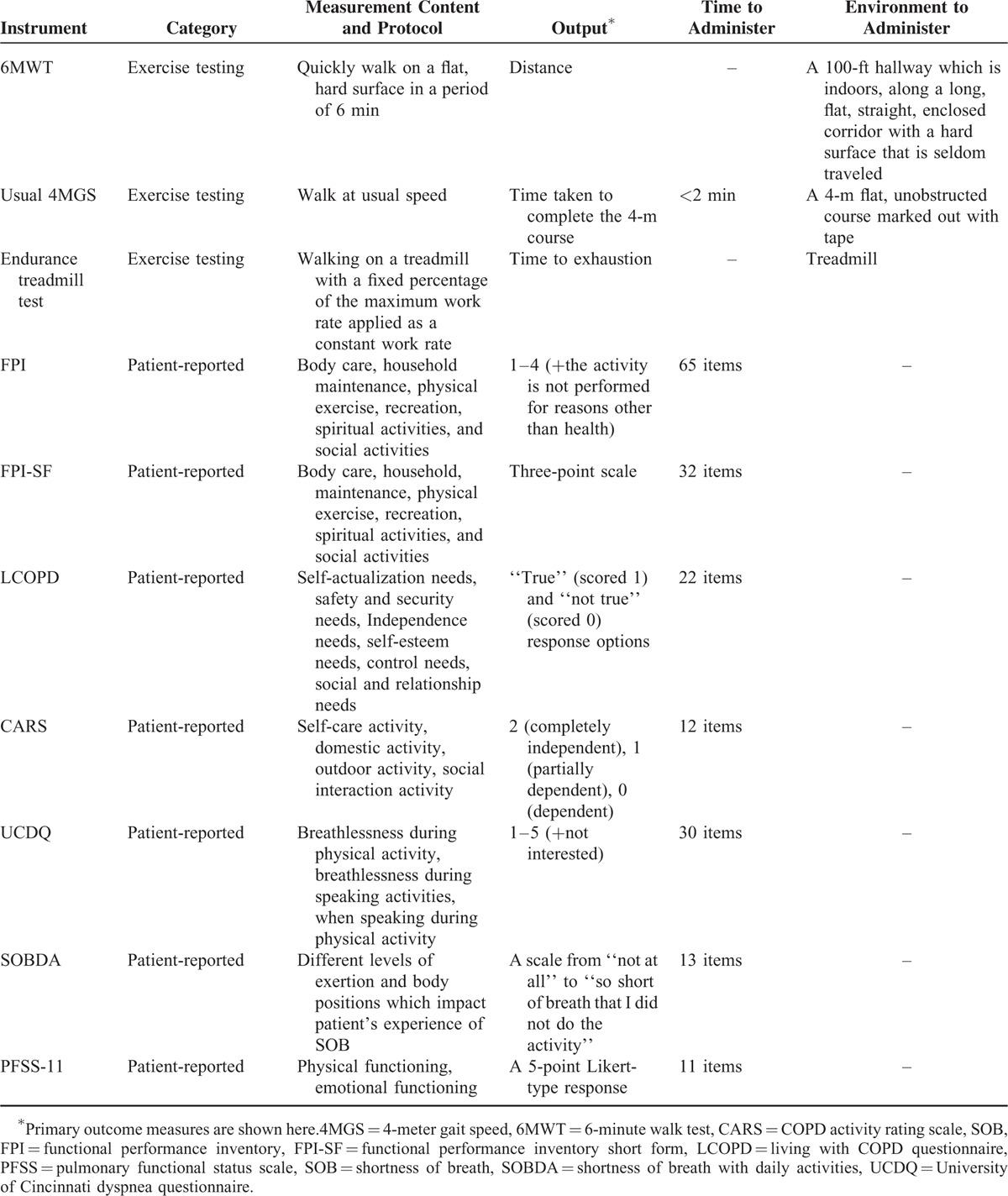
A total of 6447 records were found and 102 studies were reviewed, suggesting 44 performance-based measures and 14 patient-reported measures. The majority of the studies focused on internal consistency, reliability, and hypothesis testing, but only 21% of them employed good or excellent methodology. Their common weaknesses include lack of checks for unidimensionality, inadequate sample sizes, no prior hypotheses, and improper methods. On average, patient-reported measures perform better than performance-based measures. The best-rated patient-reported measures are functional performance inventory (FPI), functional performance inventory short form (FPI-SF), living with COPD questionnaire (LCOPD), COPD activity rating scale (CARS), University of Cincinnati dyspnea questionnaire (UCDQ), shortness of breath with daily activities (SOBDA), and short-form pulmonary functional status scale (PFSS-11), and the best-rated performance-based measures are exercise testing: 6-minute walk test (6MWT), endurance treadmill test, and usual 4-meter gait speed (usual 4MGS).
Further research is needed to evaluate the reliability and validity of performance-based measures since present studies failed to provide convincing evidence. FPI, FPI-SF, LCOPD, CARS, UCDQ, SOBDA, PFSS-11, 6MWT, endurance treadmill test, and usual 4MGS performed well and are preferable to assess functional status of COPD patients.
INTRODUCTION
Chronic obstructive pulmonary disease (COPD), characterized by persistent airflow limitation, is usually progressive and associated with an enhanced chronic inflammatory response in the airways and the lung to noxious particles or gases.1 When the disease becomes aggravated, patients suffer from deteriorated functional status and limitations to daily life. The impaired functional status is proven to be predictors of exacerbations, hospital admissions, and mortality.2,3 The worsening functional status presents a tough challenge for patients and their families and causes an increasing burden for the society.4 Therefore, assessing functional status accurately and systemically is one of demanding require of COPD treatments, as indicated in COPD guidelines.1,5,6
Measuring the type and magnitude of functional damage and evaluating treatment effect on functional improvement is a challenging work in clinical practice. Even in some large pulmonary rehabilitation programs, variables like activities of daily living (ADLs) and exercise tolerance were not adequately assessed.7,8 Functional status contains multidimensional constructs and is often confused with other relevant constructs.9–13 According to the Wilson-Cleary framework, functional status was broadly defined as the ability to perform particular defined tasks in multiple domains, including physical function, social function, role function, and psychological function.14,15 Similarly, there are also many aspects of functional status in terms of intension, including functional capacity, functional performance, functional reserve, and functional capacity utilization. Correspondingly, many functional status instruments were proposed for different purposes, including performance-based measures and patient-reported measures.12,16–19 Two limitations in present studies, undermining the development and validation of these instruments, are (1) lack of an assessment of the quality of methodology used, resulting in unconvincing conclusions of measures’ development and/or validation; (2) lack of a clear-defined, systematical, and quantifiable assessment standard, resulting in partial and ambiguous judgments on measures performance.20–22
Consensus-based standards for the selection of health measurement instruments (COSMIN) was proposed in 2006.20–23 Besides evaluating the quality of studies on measurement property critically, COSMIN also includes the measurement properties systematically. It has been used in many systematic reviews to evaluate studies and instruments of various diseases, such as hip and knee osteoarthritis, geriatrics, non-small cell lung carcinoma, and neuro-rehabilitation patients.24–27 In terms of COPD, COSMIN has been used to assess COPD assessment test (CAT) questionnaire, health-related quality of life (HRQOL) questionnaires, and arm exercise capacity.28–30 In this article, we employed COSMIN to review both patient-reported measures and performance-based measures of COPD patients’ functional status.
The objectives of this review is threefold: (1) to appraise the quality of methodology in the studies on the measures of COPD patients’ functional status and to provide insights for future researches, (2) to summarize all candidate instruments and to make recommendations for instrument selection, and (3) to compare performance-based measures and patients-reported measures.
METHOD
Search Strategy
We searched PubMed, Web of Science using a search filter developed by Terwee to identify studies describing development or evaluation of measurement properties of instruments measuring functional status of COPD patients up to the end of January 2015. (See text, Supplemental Digital Content 1, which describes the detailed search strategy.)31
1# Construct search
2# Population search
3# Instrument search
4# #1 AND #2 AND #3 AND filter for measurement properties
5# #4 NOT exclusion filter
For supplement, we searched each instrument in the entire database and looked up the references of each included article. Finally, our review was cross-checked against some relevant reviews.16,17,19,24
Eligibility Criteria and Study Selection
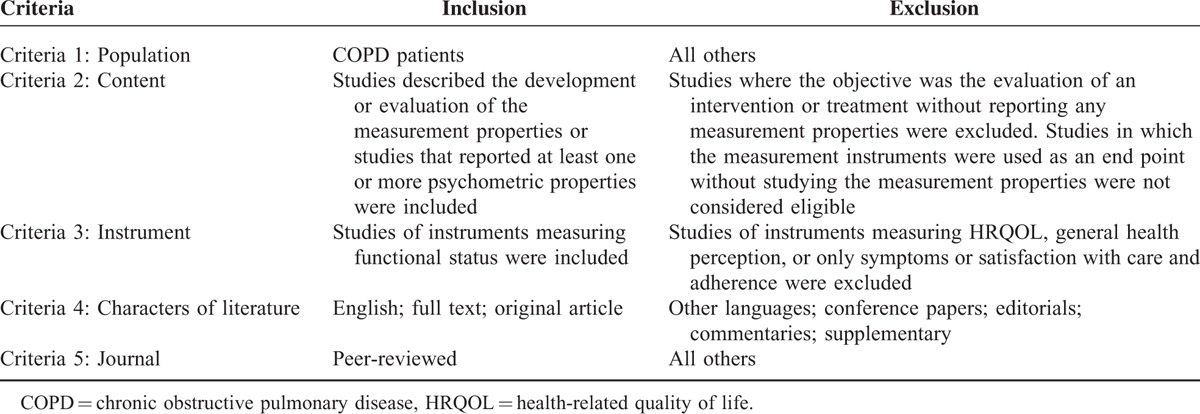
By applying the inclusion and exclusion criteria (Table 1), 3 reviewers (YL, HL, and ND) independently screened titles and abstracts of the identified records and independently assessed full texts for eligibility. Discussion was conducted when there were differences concerning exclusion criteria. If consensus could not be reached, the final decision was made by the forth reviewer (NW).
TABLE 1.
Inclusion Criteria and Exclusion Criteria for Eligible Studies
Evaluation of Methodological Quality of the Included Studies
Before the evaluation of methodological quality of the included studies, descriptive variables of these studies including authors/year, country, study sample, study design, sex (female, %), mean age years ± SD (range), mean percentage of the forced vital capacity (FEV1%) predicted ± SD, and patients status were collected. Then the methodological quality of included studies was evaluated according to the COSMIN 4-point checklist.32 The COSMIN checklist consists of 9 boxes concerning methodological standards on how each measurement property should be assessed, including 5 to 18 items in each box. The overall score (i.e., poor, fair, good, or excellent) for each item was obtained by taking the lowest score for any question within the item.
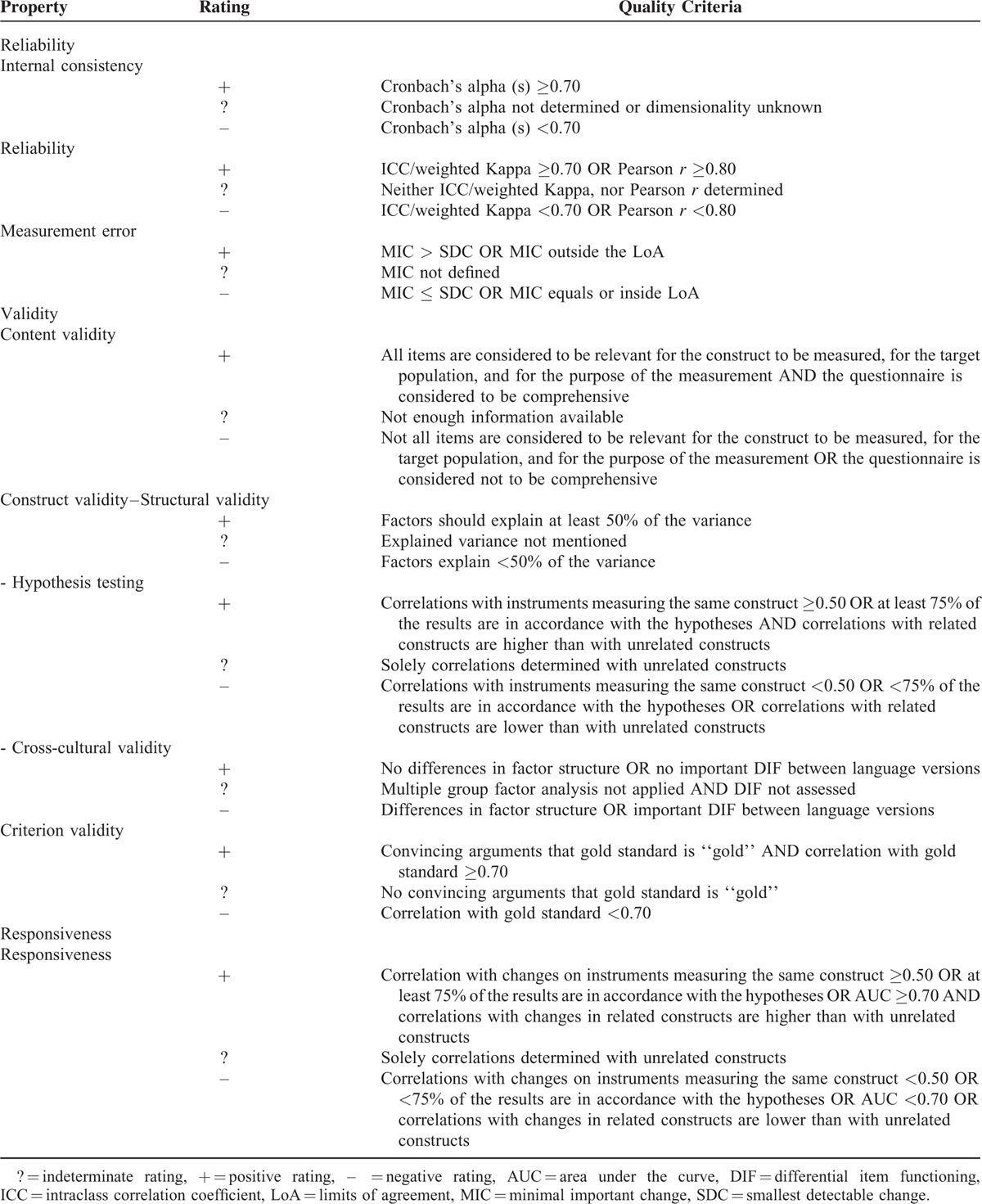
Quality Assessment of Instruments
The quality of the instruments was determined according to the rating system provided by Terwee (Table 2). It contains criteria for content validity, internal consistency, criterion validity, construct validity, reproducibility (agreement and reliability), responsiveness, floor and ceiling effects, and interpretability. Each measurement property was reported by positive (+), intermediate (?), negative (–), or no information available (0). The version provided by Terwee was used in this review.
TABLE 2.
Quality Criteria for Measurement Properties7
Data Synthesis and Quality Assessment
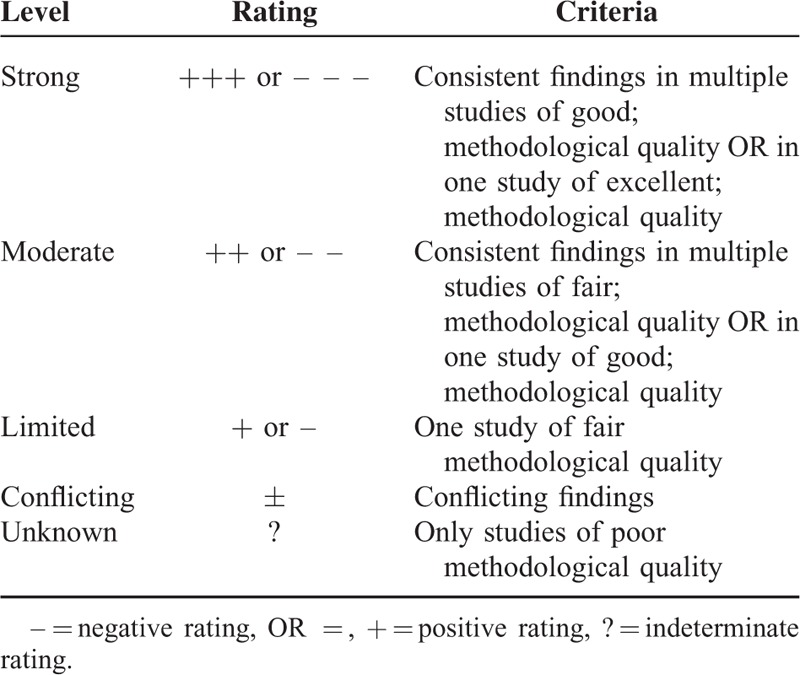
To synthesize the evidence, “best-evidence synthesis” was performed. As proposed by the Cochrane Back Review Group, the levels of evidence were “strong,” ““moderate,” “limited,” “conflicting,” or “unknown” (Table 3).33,34 Methodological quality of the studies (COSMIN score), rating of quality assessment of instruments, consistency between different studies, and the number of studies were taken into consideration using the synthesis. We defined best rated instruments as those which had a “+++” (strong positive) in at least one measurement property or a “+” or “++” in at least three measurement properties according to the results of data synthesis.
TABLE 3.
Levels of Evidence for the Quality of the Measurement Property34
Since this study merely reviewed the articles already published without involving any human participants directly, ethical approval is not necessary.
RESULTS
Electronic Literature Search Results
The selection process for all studies is shown in Figure 1. With the search filter, 6447 records were identified. After screening the title and abstract, 6225 records were excluded. The remaining 222 records were screened for full text, among which 145 records were excluded for various reasons shown in Figure 1. Twenty-five additional records were identified through screening of references lists and review articles and searching for each particular instrument in PubMed. A total of 102 articles were analyzed in the review.
FIGURE 1.
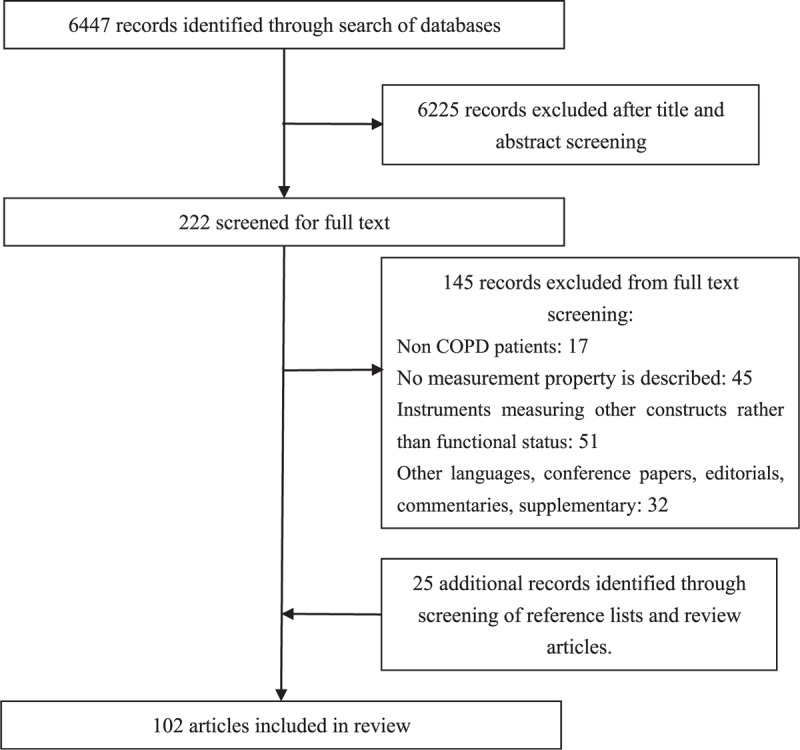
Flow diagram of search results.
Description of the Included Studies and Included Instruments
A total of 95 of the 102 studies were published after 2000. These included cross-sectional studies, longitudinal studies, and randomized double-blind studies. Mean age of subjects include in these studies ranged from 51.0 to 74.7 years. Fifty of the 102 studies declared that subjects include in their studies were stable patients. In total, 58 instruments were identified, including 44 performance-based measures and 14 patient-reported measures. The 44 performance-based measures could be divided into 28 exercise tests and 16 activity monitors. (See table, Supplemental Digital Content 2, which describes the included studies.)
Quality of the Included Studies
The quality of included studies can be found in Tables 4 and 5 . The methodological quality of the existing studies ranged from poor to excellent, with good and excellent collectively taking 21%.
TABLE 4.
Results of Quality of Design, Methods, and Reporting for Included Studies on Performance-Based Measures
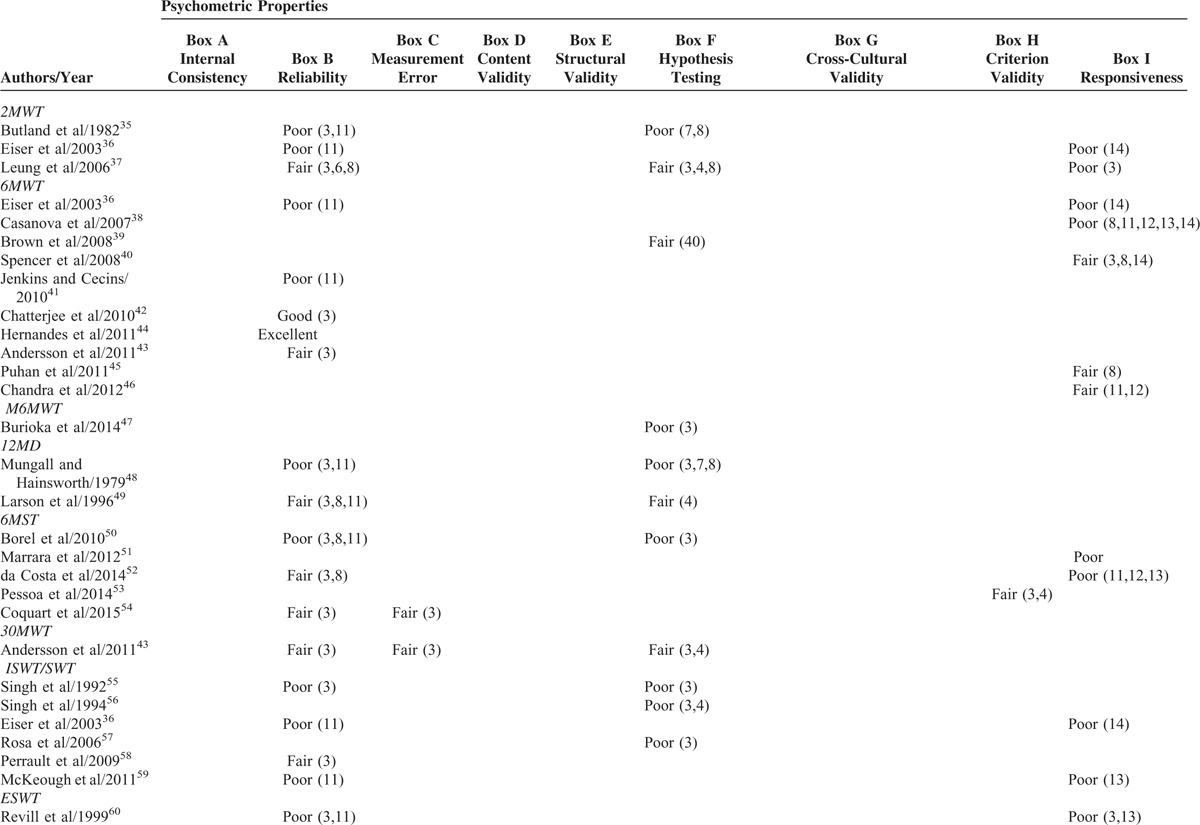
TABLE 4 (Continued).
Results of Quality of Design, Methods, and Reporting for Included Studies on Performance-Based Measures
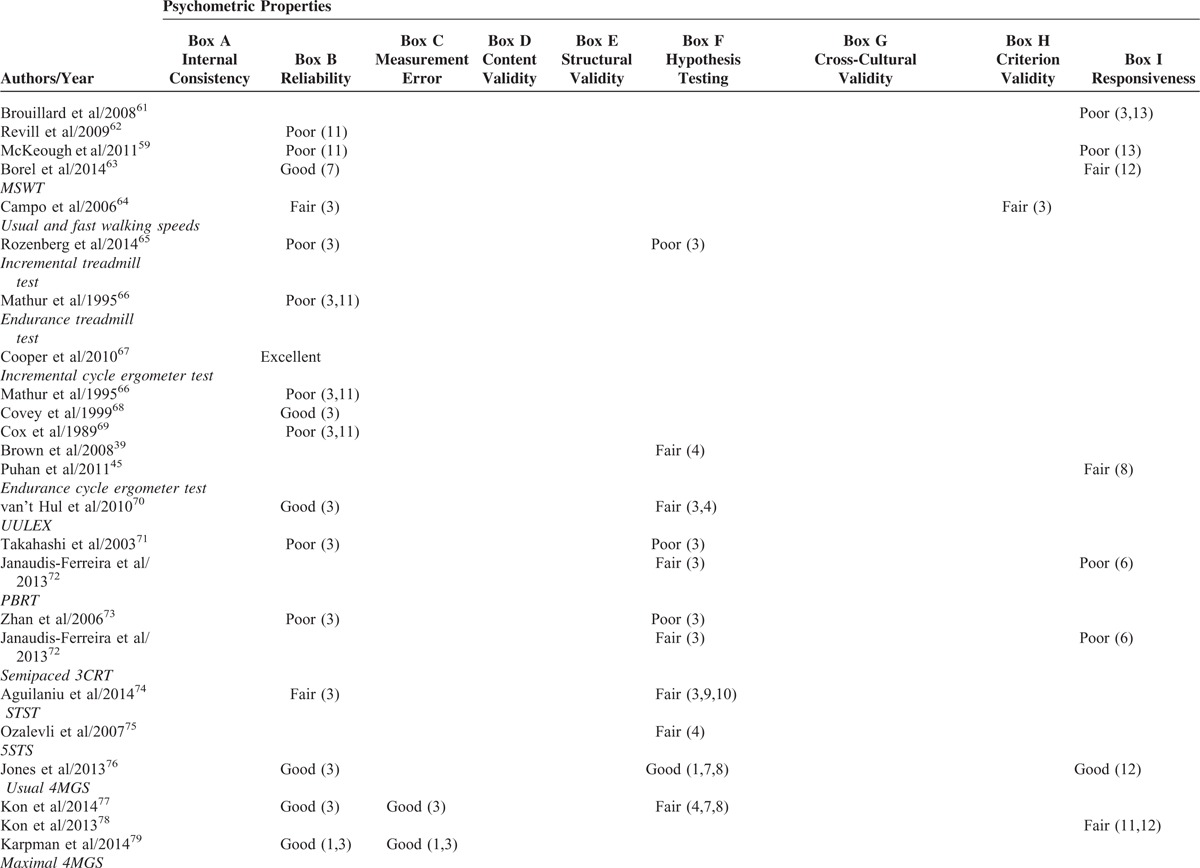
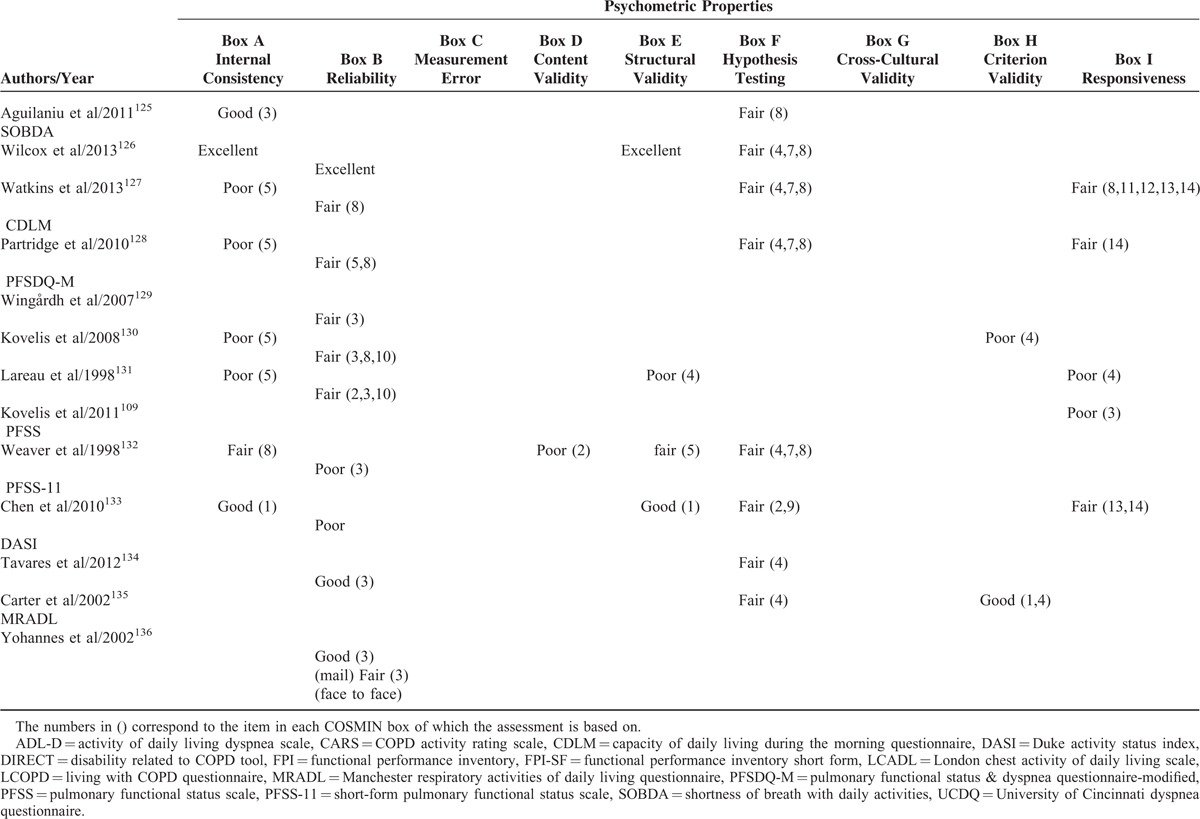
TABLE 5.
Results of Quality of Design, Methods, and Reporting for Included Studies on Patient-Reported Measures
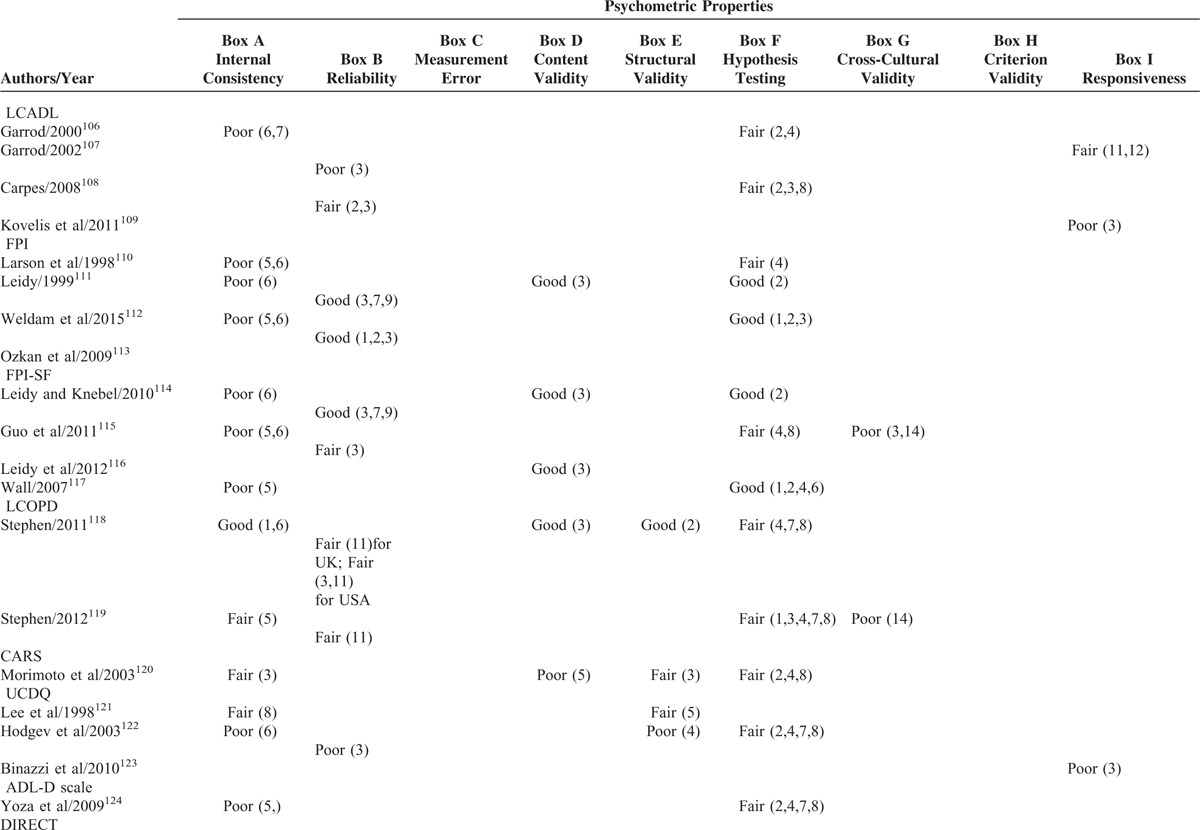
TABLE 5 (Continued).
Results of Quality of Design, Methods, and Reporting for Included Studies on Patient-Reported Measures
Studies on performance-based measures
There were 89 studies that analyzed the measurement properties of performance-based measures. Reliability and hypothesis testing were the most reported measurement properties of this type of instrument (reported in 52 studies and 35 studies, respectively). Criterion validity and responsiveness were reported in 20 studies and 24 studies, respectively. Unlike the patient-reported measures, performance-based measures had some evidence of measurement error from 7 studies.
Of the studies reporting on reliability, 2 were excellent, 12 were good, 12 were fair, and 26 were poor. Inadequate sample size and no intraclass correlation coefficient (ICC) or Pearson or Spearman correlations calculated were the main reasons contributing to poor quality of the study. For hypothesis testing, 2 studies were good, 16 fair, and 17 poor. The main weakness lies in inadequate sample sizes and a lack of adequate hypotheses. Evaluating the criterion validity, most studies chose the direct observation as the gold criterion. However, 12 studies were considered poor in criterion validity because of inadequate sample sizes. Among the 20 studies reporting responsiveness, 1 study had good quality, 7 studies had fair quality, and 16 studies had poor quality.
Studies on patient-reported measures
Among the 32 studies analyzing the measurement properties of patient-reported measures, internal consistency, reliability, and hypothesis testing were the measurement properties reported most frequently (reported in 21, 20, and 21 studies, respectively), whereas no study reported on the measurement error of the patient-reported measures. Cross-cultural validity and criterion validity were also only reported in 6 studies and 2 studies, respectively. Content validity and cross-cultural validity were more so evaluated in the development of the scales rather than in the final version.
The qualities of the studies analyzing the internal consistency of patients-reported measures were as follows: 1 excellent, 3 good, 4 fair, and 13 poor. Studies were deemed poor mostly because of the fact that unidimensionality was not properly checked. The quality of the studies analyzing the reliability was 1 excellent, 5 good, 9 fair, and 5 poor. Inadequate sample size was the decisive factor of lesser quality. The quality of the studies analyzing the hypothesis testing was 4 good and 17 fair. The quality of most studies stopped at fair because of that they did not formulate any hypotheses in their studies. Studies reporting responsiveness did not have high quality because of inadequate sample sizes or to the fact that inappropriate methods were used. Structural validity was analyzed in 8 studies and the qualities were mostly determined by the sample size.111,113–115,119,124–126
Quality of Psychometric Properties for Outcome Measures
A summary of best-evidence synthesis is provided in Table 6 . The summary was driven from the results of study qualities and the quality of psychometric properties for outcome measures (see table, Supplemental Digital Content 3, which describes quality of psychometric properties for outcome measures) using the criteria displayed in Table 3.
TABLE 4 (Continued).
Results of Quality of Design, Methods, and Reporting for Included Studies on Performance-Based Measures
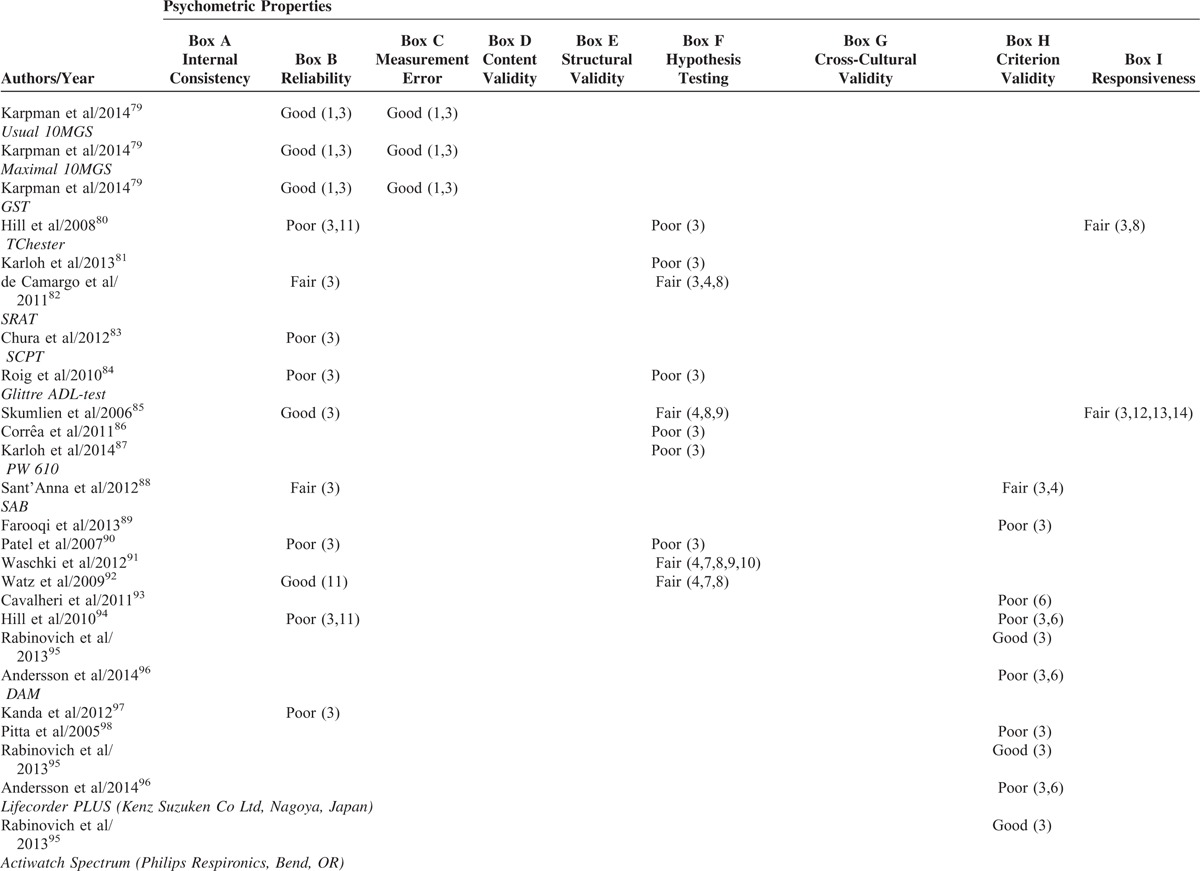
TABLE 6.
A Summary of Best-Evidence Synthesis
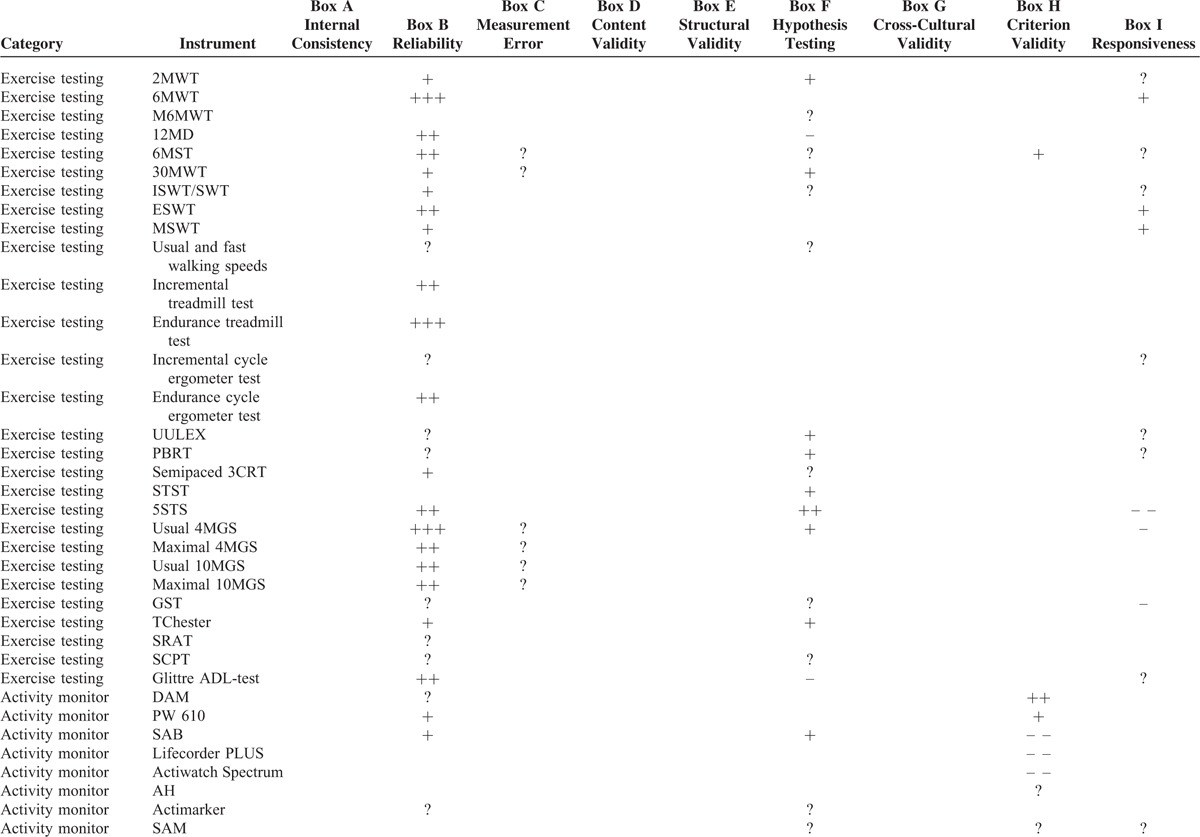
TABLE 6 (Continued).
A Summary of Best-Evidence Synthesis
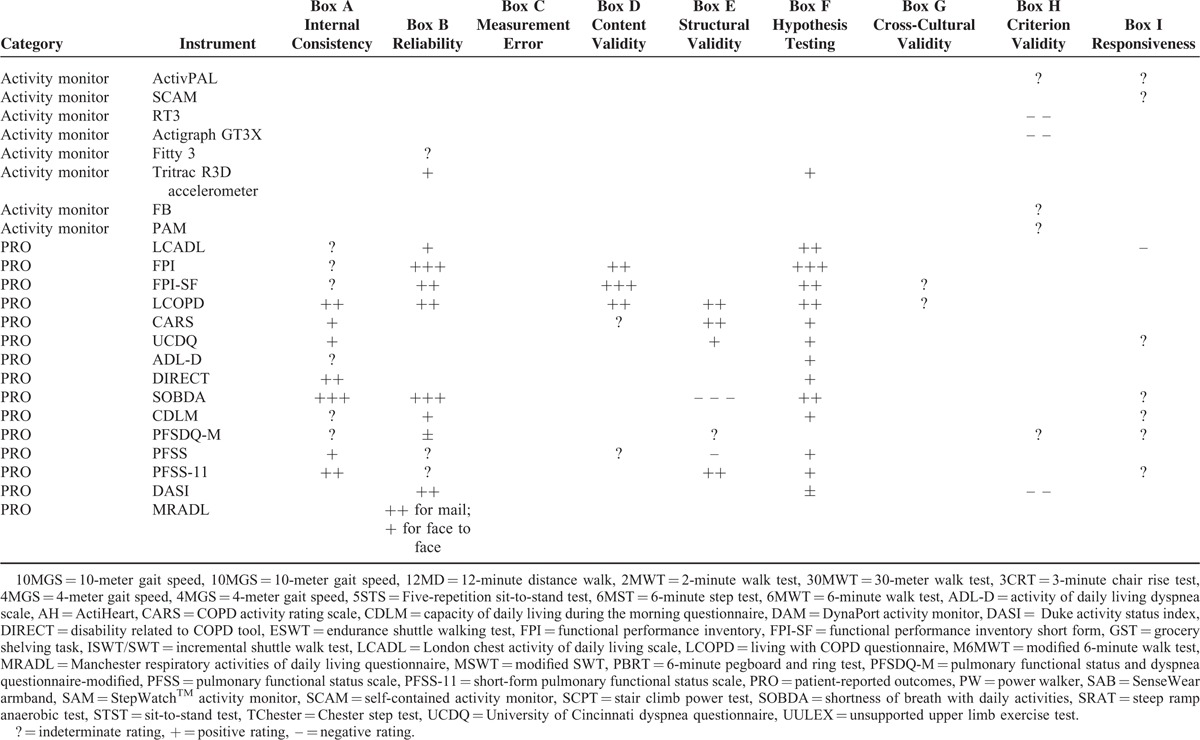
Patient-reported measures performed better than performance-based measures. All positive evidence of patient-reported measures were evenly distributed in both reliability and validity. Most of the positive evidence of performance-based measures was confined to exercise testing and reliability measurement property.
Best rated instruments with a “+++” in one measurement property or “+”/“++” in at least three measurement properties among performance-based measures are 6-minute walk test (6MWT), endurance treadmill test, and usual 4-meter gait speed (usual 4MGS). The best rated patients-reported measures were functional performance inventory (FPI), functional performance inventory short form (FPI-SF), living with COPD questionnaire (LCOPD), COPD activity rating scale (CARS), University of Cincinnati dyspnea questionnaire (UCDQ), shortness of breath with daily activities (SOBDA), and short-form pulmonary functional status scale (PFSS-11).
DISCUSSION
The present review provides the first evidence on comparing all candidate instruments measuring functional status in COPD patients according to the COSMIN criteria. It highlighted some areas worthy of future researched, including the lack of adequate positive evidence on measurement properties of performance-based measures compared with patient-reported measures, the weakness limiting the quality of the existing studies, and the important measurement properties neglected by existing studies. Although none of the instruments was tested for all measurement properties, the existing evidence still confirms that some instruments performed better in terms of some measurement properties or some survey types. For clinical practice, this review recommends 10 out or 57 instruments assessing functional status of COPD patients. More importantly, it demonstrates how to choose suitable measures according to both the studies on elevating these measures and the requirements of clinical practice.
Comparing Performance-Based Measures with Patient-Reported Measures
According to the summary of best-evidence synthesis, performance-based measures did not have as much positive evidence on measurement property in comparison to patient-reported measures. The lack of adequate positive evidence contradicts their present importance in measuring functional status in COPD patients. Performance-based measures objectively measure what patients actually do by assessing indicators like timing, counting, and distance.137 It was believed to be more likely to fully characterize a change in functional status than patient-reported measures alone.138 Some of these performance-based measures have been widely approved and used for many years to evaluate treatment effect, to assess health status, and to explore etiology. For example, 6MWT is a widely used walking test in clinical practice, and it was often used as a standard for other instruments.139–142 However, its positive evidence confined to reliability, which is also a common situation in all performance-based measures. Activity monitors capture the patients’ activities of daily living. They are an essential supplement to laboratory tests. Although there are numerous studies (27 studies), the qualities of these studies were poor (16 poor studies), leading to a weaker positive rating in evidence synthesis. More good quality studies need to be conducted in order to assess the measurement properties of these performance-based measures.
Weakness Limiting the Quality and Neglected Measurement Properties in the Existing Studies on Performance-Based Measures and Patient-Reported Measures
The methodological qualities of the studies included in this review ranged from poor to excellent. Good and excellent quality studies only took up ∼20% of all studies. In terms of performance-based measures, inadequate sample size was one major drawback, probably because performance-based measurements are more difficult to conduct. Some studies on performance-based measures had a sample size <10.37,47,66,71,90,105 The sample size should be enlarged in future similar studies according to COSMIN criterion, which is ≥100 for excellent, 50–99 for good, 30–49 for fair, and <30 for poor. However, one thing to note is that the COSMIN checklist was originally developed to assess studies focusing on patient-reported measures. Considering the differences in instrument characteristics and study designs between studies on performance-based measures and studies on patient-reported measures, the sample size criteria may need some adjustment. Methodology on performance-based measures should be discussed in the future. Another obvious drawback affecting studies on performance-based measures was that methods did not meet the COSMIN criteria. For example, some studies measuring reliability tend to not calculate the ICC or Pearson or Spearman correlations, no correlation was calculated with other comparative instruments, whereas only P values were used when testing responsiveness, and no adequate hypotheses were formulated a priori. Qualities of studies on patient-reported measures were better than studies on performance-based measures (Table 5 ). However, checking for unidimensionality, enlarging sample sizes, and formulating hypotheses a priori may further improve all study quality.
According to the results, the included studies and positive evidence were confined to several measurement properties. Some important measurement properties, including content validity and responsiveness, were neglected or poorly reported. Content validity examines the extent to which the concepts of interest are comprehensively represented by the items of the questionnaire,24,143 so it is especially important for studies on patient-reported measures. To measure content validity, a clear concept model is to be developed.144 However, present PROs that aim to measure physical activity in chronic respiratory disease patients or similar populations (chronic heart disease patients or the elderly) are rarely based on a conceptual framework.145 Additionally, a standard method to assess content validity should be applied. According to COSMIN, an appropriate method is to have experts and the target population to assess the relevance and comprehensiveness of the instrument (s) based on criteria set by COSMIN. The two studies on content validity measurement were determined to be poor because they did not meet the above-mentioned criterion. Responsiveness is another key issue for future studies on both performance-based measures and patient-reported measures. An important role of functional status measurement is the evaluation of the effect of rehabilitation or treatment. Therefore, it is important for measurement instruments to respond to change. In the present studies measuring responsiveness, the rating of poor was given because of inadequate sample size. Also, most fair studies used P values instead of showing correlation with comparative instruments or with AUC values. Further studies exploring the responsiveness of functional status instruments should be conducted by applying appropriate methods.
Choosing Measures According to the Present Evidence
Valid and systematical measures of COPD patients’ health status are the base of the accurate quantification of the therapy effects. Facing an impressive and increasing number of measures assessing functional status of COPD patients, clinicians might be confused and feel difficult to find one measure satisfying all of their demands. Another source of confusion is the inconsistent conclusions of reports which employed various measures to evaluate the effect of therapy. It is difficult for clinicians to choose best care for patients by comparing and combining results of these clinical trials.
According to the results, none of measures has been tested for all measurement properties. However, the existing evidence demonstrates that some instruments perform better: 6MWT, endurance treadmill test, and usual 4MGS; and FPI, FPI-SF, LCOPD, CARS, UCDQ, SOBDA, and PFSS-11. These instruments should be preferred in future studies and clinical practice (Table 7). 6MWT was proven to predict the survival in COPD patients well.146–148 Usual 4MGS needs much shorter course than 6MWT, making it useful for frail patients and applicable in most healthcare settings (including home). MCID was reported to be 0.11 m/s.77 It is worth to be considered as an instrument for health management of COPD patients. Endurance treadmill test can clearer reflect the physiological limitations.67 FPI, FPI-SF, LCOPD, CARS, UCDQ, SOBDA, and PFSS-11 are different in terms of their measurement focus and the length of scales. In other words, each measure has its own advantage and most suitable domain. Thus, researchers and clinicians should employ those measures whose measurement properties alignment to their purposes. For example, if the instruments were to be used to measure the therapeutic effect of pulmonary rehabilitation or a respiratory medicine, then the responsiveness of the measurement instruments should be preferred. Finally, functional status measurement of COPD patients is complex, as it contains multidimensional constructs. Different types of instruments have their own strength. It was suggested that both types of measures—performance-based measures and patient-reported measures—are complementary rather than competing when assessing functional status of COPD patients.149 Finding an optimal combination of measures from both types is worth for further research.
TABLE 4 (Continued).
Results of Quality of Design, Methods, and Reporting for Included Studies on Performance-Based Measures
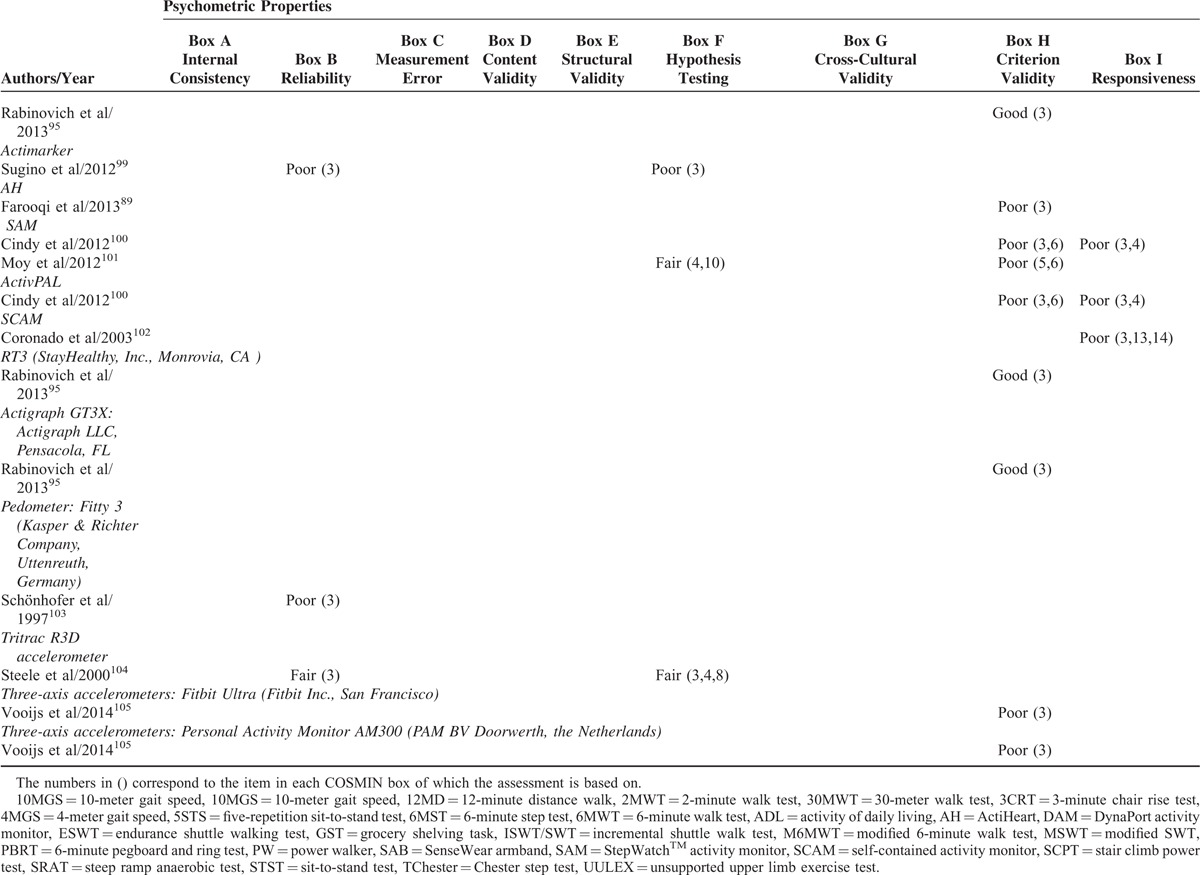
TABLE 7.
Characteristics of Recommended Instruments
LIMITATIONS
This study has several limitations. First, some comprehensive HRQOL instruments, including dimensions measuring functional status were excluded in our study. The reason is that their reliability and validity were calculated for the whole instrument rather than the dimension of interest, functional status. Second, some studies focusing on evaluating the therapy effect were excluded because they failed to provide enough information on measurement properties. Admittedly, reviewing measurement properties for a certain type of therapy is interesting and valuable for clinical practice, which should be implemented in the future.
In summary, further research is needed to evaluate the measurement properties of performance-based measures because there is a lack of available information and present studies lack in quality. Content validity and responsiveness should be fully assessed in all instruments, and sample size needs to be enlarged. As for choosing measurement tools for functional status in COPD patients, we recommend FPI, FPI-SF, LCOPD, CARS, UCDQ, SOBDA, PFSS-11, 6MWT, endurance treadmill test, and usual 4MGS. These instruments are different in their measurement content or administer requirement, which may tailor to different usage in clinical practice. We also recommend selecting instruments that perform well in certain measurement properties required for certain assessment purposes and combining instruments from both measurement types.
Supplementary Material
Acknowledgments
The authors thank Terwee CB for providing us permission to use the COSMIN checklist and instruction to do the systematic review using COSMIN. We also thank Weldam, S.W.M., for responding to their consultation about quality criteria for measurement properties in his article. We thank Nan Jiang for her kind help with correcting English of the manuscript.
Footnotes
Abbreviations: 10MGS = maximal 10-meter gait speed, 10MGS = usual 10-meter gait speed, 12MD = 12-minute distance walk, 2MWT = 2-minute walk test, 30MWT = 30-meter walk test, 3CRT = 3-minute chair rise test, 4MGS = 4-meter gait speed, 4MGS = 4-meter gait speed, 5STS = five-repetition sit-to-stand test, 6MST = 6-minute step test, 6MWT = 6-minute walk test, ADL-D = activity of daily living dyspnea scale, ADLs = activities of daily living, AH = actiheart, AUC = area under the curve, CARS = COPD activity rating scale, CAT = COPD assessment test, CDLM = capacity of daily living during the morning questionnaire, COPD = chronic obstructive pulmonary disease, COSMIN = consensus-based standards for the selection of health measurement instruments, DAM = DynaPort activity monitor, DASI = Duke activity status index, DIF = differential item functioning, DIRECT = DIsability RElated to COPD Tool, ESWT = endurance shuttle walking test, FPI = functional performance inventory, FPI-SF = functional performance inventory short form, GST = grocery shelving task, HRQOL = health-related quality of life, ICC = intraclass correlation coefficient, ISWT/SWT = incremental shuttle walk test, LCADL = London chest activity of daily living scale, LCOPD = living with COPD questionnaire, LoA = limits of agreement, M6MWT = modified 6-minute walk test, MIC = minimal important change, MRADL = Manchester respiratory activities of daily living questionnaire, MSWT = modified SWT, PBRT = 6-minute pegboard and ring test, PFSDQ-M = pulmonary functional status and dyspnea questionnaire-modified, PFSS = pulmonary functional status scale, PFSS-11 = short-form pulmonary functional status scale, PRO = patient-reported outcomes, PW = power walker 610, SAB = SenseWear armband, SAM = StepWatch activity monitor, SCAM = self-contained activity monitor, SCPT = stair climb power test, SDC = smallest detectable change, SOBDA = shortness of breath with daily activities, SRAT = steep ramp anaerobic test, STST = sit-to-stand test, TChester = Chester step test, UCDQ = University of Cincinnati dyspnea questionnaire, UULEX = unsupported upper limb exercise test.
This study was supported by Natural Science Foundation of China (NSFC) (fund number: 71573032).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.From the Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2016. Available from: http://goldcopd.org/ Accessed March 10, 2016. [Google Scholar]
- 2.Fan VS, Ramsey SD, Make BJ, et al. Physiologic variables and functional status independently predict COPD hospitalizations and emergency department visits in patients with severe COPD. COPD 2007; 4:29–39. [DOI] [PubMed] [Google Scholar]
- 3.Pitta F, Troosters T, Probst VS, et al. Physical activity and hospitalization for exacerbation of COPD. Chest 2006; 129:536–544. [DOI] [PubMed] [Google Scholar]
- 4.Wang KY, Sung PY, Yang ST, et al. Influence of family caregiver caring behavior on COPD patients’ self-care behavior in Taiwan. Respir Care 2012; 57:263–272. [DOI] [PubMed] [Google Scholar]
- 5.Celli BR, MacNee W. ATS/ERS Task Force. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J 2004; 23:932–946. [DOI] [PubMed] [Google Scholar]
- 6.National Clinical Guideline Centre (UK). Chronic Obstructive Pulmonary Disease: Management of Chronic Obstructive Pulmonary Disease in Adults in Primary and Secondary Care [Internet]. London: Royal College of Physicians (UK); 2010 Jun. (NICE Clinical Guidelines, No. 101.) Available from: http://www.ncbi.nlm.nih.gov/books/NBK65039/ Accessed August 25, 2015. [PubMed] [Google Scholar]
- 7.Yohannes AM, Connolly MJ. Pulmonary rehabilitation programmes in the UK: a national representative survey. Clin Rehabil 2004; 18:444–449. [DOI] [PubMed] [Google Scholar]
- 8.Brooks D, Sottana R, Bell B, et al. Characterization of pulmonary rehabilitation programs in Canada in 2005. Can Respir J 2007; 14:87–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leidy NK. Functional performance in people with chronic obstructive pulmonary disease. Image J Nurs Sch 1995; 27:23–34. [DOI] [PubMed] [Google Scholar]
- 10.Larson JL. Functional performance and physical activity in chronic obstructive pulmonary disease: theoretical perspectives. COPD 2007; 4:237–242. [DOI] [PubMed] [Google Scholar]
- 11.Reardon JZ, Lareau SC, ZuWallack R. Functional status and quality of life in chronic obstructive pulmonary disease. Am J Med 2006; 119 (10 Suppl 1):32–37. [DOI] [PubMed] [Google Scholar]
- 12.Leidy NK. Functional status and the forward progress of merry-go-rounds: toward a coherent analytical framework. Nurs Res 1994; 43:196–202. [PubMed] [Google Scholar]
- 13.Leidy NK. Subjective measurement of activity in chronic obstructive pulmonary disease. COPD 2007; 4:243–249. [DOI] [PubMed] [Google Scholar]
- 14.Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA 1995; 273:59–65. [PubMed] [Google Scholar]
- 15.Ferrans CE, Zerwic JJ, Wilbur JE, et al. Conceptual model of health-related quality of life. J Nurs Scholarsh 2005; 37:336–342. [DOI] [PubMed] [Google Scholar]
- 16.Kocks JW, Asijee GM, Tsiligianni IG, et al. Functional status measurement in COPD: a review of available methods and their feasibility in primary care. Prim Care Respir J 2011; 20:269–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fotheringham I, Meakin G, Punekar YS, et al. Comparison of laboratory- and field-based exercise tests for COPD: a systematic review. Int J Chron Obstruct Pulmon Dis 2015; 10:625–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Janaudis-Ferreira T, Beauchamp MK, Robles PG, et al. Measurement of activities of daily living in patients with COPD: a systematic review. Chest 2014; 145:253–271. [DOI] [PubMed] [Google Scholar]
- 19.Stull DE, Leidy NK, Jones PW, et al. Measuring functional performance in patients with COPD: a discussion of patient-reported outcome measures. Curr Med Res Opin 2007; 23:2655–2665. [DOI] [PubMed] [Google Scholar]
- 20.Mokkink LB, Terwee CB, Knol DL, et al. The COSMIN checklist for evaluating the methodological quality of studies on measurement properties: a clarification of its content. BMC Med Res Methodol 2010; 10:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mokkink LB, Terwee CB, Patrick DL, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol 2010; 63:737–745. [DOI] [PubMed] [Google Scholar]
- 22.Mokkink LB, Terwee CB, Knol DL, et al. Protocol of the COSMIN study: consensus-based standards for the selection of health measurement Instruments. BMC Medical Res Methodol 2006; 6:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Terwee CB, Bot SD, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007; 60:34–42. [DOI] [PubMed] [Google Scholar]
- 24.Kroman SL, Roos EM, Bennell KL, et al. Measurement properties of performance-based outcome measures to assess physical function in young and middle-aged people known to be at high risk of hip and/or knee osteoarthritis: a systematic review. Osteoarthritis Cartilage 2014; 22:26–39. [DOI] [PubMed] [Google Scholar]
- 25.Mijnarends DM, Meijers JM, Halfens RJ, et al. Validity and reliability of tools to measure muscle mass, strength, and physical performance in community-dwelling older people: a systematic review. J Am Med Dir Assoc 2013; 14:170–178. [DOI] [PubMed] [Google Scholar]
- 26.Granger CL, McDonald CF, Parry SM, et al. Functional capacity, physical activity and muscle strength assessment of individuals with non-small cell lung cancer: a systematic review of instruments and their measurement properties. BMC Cancer 2013; 13:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pike S, Lannin NA, Cusick A, et al. A systematic review protocol to evaluate the psychometric properties of measures of function within adult neuro-rehabilitation. Syst Rev 2015; 4:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gupta N, Pinto LM, Morogan A, et al. The COPD assessment test: a systematic review. Eur Respir J 2014; 44:873–884. [DOI] [PubMed] [Google Scholar]
- 29.Weldam SW, Schuurmans MJ, Liu R, et al. Evaluation of quality of life instruments for use in COPD care and research: a systematic review. Int J Nurs Stud 2013; 50:688–707. [DOI] [PubMed] [Google Scholar]
- 30.Janaudis-Ferreira T, Beauchamp MK, Goldstein RS, et al. How should we measure arm exercise capacity in patients with COPD? CHEST 2012; 141:111–120. [DOI] [PubMed] [Google Scholar]
- 31.Terwee CB, Jansma EP, Riphagen II, et al. Development of methodological PubMed search filter for finding studies on measurement properties of measurement instruments. Qual Life Res 2009; 18:1115–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Terwee CB, Mokkink LB, Knol DL, et al. Rating the methodological quality in systematic reviews of studies on measurement properties: a scoring system for the COSMIN checklist. Qual Life Res 2012; 21:651–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Furlan AD, Pennick V, Bombardier C, et al. Editorial Board, Cochrane Back Review Group. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine 2009; 34:1929–1941. [DOI] [PubMed] [Google Scholar]
- 34.van Tulder M, Furlan A, Bombardier C, et al. Editorial Board of the Cochrane Collaboration Back Review Group. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine 2003; 28:1290–1299. [DOI] [PubMed] [Google Scholar]
- 35.Butland RJ, Pang J, Gross ER, et al. Two-, six-, and 12-minute walking tests in respiratory disease. Brit Med J (Clin Res Ed) 1982; 284:1607–1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eiser N, Willsher D, Doré CJ. Reliability, repeatability and sensitivity to change of externally and self-paced walking tests in COPD patients. Respir Med 2003; 97:407–414. [DOI] [PubMed] [Google Scholar]
- 37.Leung AS, Chan KK, Sykes K, et al. Reliability, validity, and responsiveness of a 2-min walk test to assess exercise capacity of COPD patients. Chest 2006; 130:119–125. [DOI] [PubMed] [Google Scholar]
- 38.Casanova C, Cote CG, Marin JM, et al. The 6-min walking distance: long-term follow up in patients with COPD. Eur Respir J 2007; 29:535–540. [DOI] [PubMed] [Google Scholar]
- 39.Brown CD, Benditt JO, Sciurba FC, et al. National emphysema Treatment Trial Research Group. Exercise testing in severe emphysema: association with quality of life and lung function. COPD 2008; 5:117–124. [DOI] [PubMed] [Google Scholar]
- 40.Spencer LM, Alison JA, McKeough ZJ. Six-minute walk test as an outcome measure: are two six-minute walk tests necessary immediately after pulmonary rehabilitation and at three-month follow-up? Am J Phys Med Rehabil 2008; 87:224–228. [DOI] [PubMed] [Google Scholar]
- 41.Jenkins S, Cecins NM. Six-minute walk test in pulmonary rehabilitation: do all patients need a practice test? Respirology 2010; 15:1192–1196. [DOI] [PubMed] [Google Scholar]
- 42.Chatterjee AB, Rissmiller RW, Meade K, et al. Reproducibility of the 6-minute walk test for ambulatory oxygen prescription. Respiration 2010; 79:121–127. [DOI] [PubMed] [Google Scholar]
- 43.Andersson M, Moberg L, Svantesson U, et al. Measuring walking speed in COPD: test–retest reliability of the 30-metre walk test and comparison with the 6-minute walk test. Prim Care Respir 2011; 20:434–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hernandes NA, Wouters EF, Meijer K, et al. Reproducibility of 6-minute walking test in patients with COPD. Eur Respir J 2011; 38:261–267. [DOI] [PubMed] [Google Scholar]
- 45.Puhan MA, Chandra D, Mosenifar Z, et al. National Emphysema Treatment Trial (NETT) Research Group. The minimal important difference of exercise tests in severe COPD. Eur Respir J 2011; 37:784–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chandra D, Wise RA, Kulkarni HS, et al. Sciurba FC; NETT Research Group. Optimizing the 6-min walk test as a measure of exercise capacity in COPD. Chest 2012; 142:1545–1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Burioka N, Imada A, Kiyohiro A, et al. Modified six-minute walk test: number of steps per second. Yonago Acta Med 2014; 57:61–63. [PMC free article] [PubMed] [Google Scholar]
- 48.Mungall IP, Hainsworth R. Assessment of respiratory function in patients with chronic obstructive airways disease. Thorax 1979; 34:254–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Larson JL, Covey MK, Vitalo CA, et al. Reliability and validity of the 12-minute distance walk in patients with chronic obstructive pulmonary disease. Nurs Res 1996; 45:203–210. [DOI] [PubMed] [Google Scholar]
- 50.Borel B, Fabre C, Saison S, et al. An original field evaluation test for chronic obstructive pulmonary disease population: the six-minute stepper test. Clin Rehabil 2010; 24:82–93. [DOI] [PubMed] [Google Scholar]
- 51.Marrara KT, Marino DM, Jamami M, et al. Responsiveness of the six-minute step test to a physical training program in patients with COPD. J Bras Pneumol 2012; 38:579–587. [DOI] [PubMed] [Google Scholar]
- 52.da Costa JN, Arcuri JF, Goncalves IL, et al. Reproducibility of cadence-free 6-minute step test in subjects with COPD. Respir Care 2014; 59:538–542. [DOI] [PubMed] [Google Scholar]
- 53.Pessoa BV, Arcuri JF, Labadessa IG, et al. Validity of the six-minute step test of free cadence in patients with chronic obstructive pulmonary disease. Braz J Phys Ther 2014; 18:228–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Coquart JB, Lemaître F, Castres I, et al. Reproducibility and sensitivity of the 6-minute stepper test in patients with COPD. COPD 2015; 12:533–538. [DOI] [PubMed] [Google Scholar]
- 55.Singh SJ, Morgan MD, Scott S, et al. Development of a shuttle walking test of disability in patients with chronic airways obstruction. Thorax 1992; 47:1019–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Singh SJ, Morgan MD, Hardman AE, et al. Comparison of oxygen uptake during a conventional treadmill test and the shuttle walking test in chronic airflow limitation. Eur Respir J 1994; 7:2016–2020. [PubMed] [Google Scholar]
- 57.Rosa FW, Camelier A, Mayer A, et al. Evaluating physical capacity in patients with chronic obstructive pulmonary disease: comparing the shuttle walk test with the encouraged 6-minute walk test. J Bras Pneumol 2006; 32:106–113. [DOI] [PubMed] [Google Scholar]
- 58.Perrault H, Baril J, Henophy S, et al. Paced-walk and step tests to assess exertional dyspnea in COPD. COPD 2009; 6:330–339. [DOI] [PubMed] [Google Scholar]
- 59.McKeough ZJ, Leung RW, Alison JA. Shuttle walk tests as outcome measures: are two incremental shuttle walk tests and two endurance shuttle walk tests necessary? Am J Phys Med Rehabil 2011; 90:35–39. [DOI] [PubMed] [Google Scholar]
- 60.Revill SM, Morgan MD, Singh SJ, et al. The endurance shuttle walk: a new field test for the assessment of endurance capacity in chronic obstructive pulmonary disease. Thorax 1999; 54:213–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Brouillard C, Pepin V, Milot J, et al. Endurance shuttle walking test: responsiveness to salmeterol in COPD. Eur Respir J 2008; 31:579–584. [DOI] [PubMed] [Google Scholar]
- 62.Revill SM, Williams J, Sewell L, et al. Within-day repeatability of the endurance shuttle walk test. Physiotherapy 2009; 95:140–143. [DOI] [PubMed] [Google Scholar]
- 63.Borel B, Pepin V, Mahler DA, et al. Prospective validation of the endurance shuttle walking test in the context of bronchodilation in COPD. Eur Respir J 2014; 44:1166–1176. [DOI] [PubMed] [Google Scholar]
- 64.Campo LA, Chilingaryan G, Berg K, et al. Validity and reliability of the modified shuttle walk test in patients with chronic obstructive pulmonary disease. Arch Phys Med Rehabil 2006; 87:918–922. [DOI] [PubMed] [Google Scholar]
- 65.Rozenberg D, Dolmage TE, Evans RA, et al. Repeatability of usual and fast walking speeds in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil Prev 2014; 34:348–354. [DOI] [PubMed] [Google Scholar]
- 66.Mathur RS, Revill SM, Vara DD, et al. Comparison of peak oxygen consumption during cycle and treadmill exercise in severe chronic obstructive pulmonary disease. Thorax 1995; 50:829–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cooper CB, Abrazado M, Legg D, et al. Development and implementation of treadmill exercise testing protocols in COPD. Int J Chron Obstruct Pulmon Dis 2010; 5:375–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Covey MK, Larson JL, Alex CG, et al. Test–retest reliability of symptom-limited cycle ergometer tests in patients with chronic obstructive pulmonary disease. Nurs Res 1999; 48:9–19. [DOI] [PubMed] [Google Scholar]
- 69.Cox NJ, Hendriks JC, Binkhorst RA, et al. Reproducibility of incremental maximal cycle ergometer tests in patients with mild to moderate obstructive lung diseases. Lung 1989; 167:129–133. [DOI] [PubMed] [Google Scholar]
- 70.van’t Hul A, Gosselink R, Kwakkel G. Constant-load cycle endurance performance test-retest reliability and validity in patients with COPD. J Cardiopulm Rehabil 2010; 23:143–150. [DOI] [PubMed] [Google Scholar]
- 71.Takahashi T, Jenkins SC, Strauss GR, et al. A new unsupported upper limb exercise test for patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil 2003; 23:430–437. [DOI] [PubMed] [Google Scholar]
- 72.Janaudis-Ferreira T, Hill K, Goldstein RS, et al. Relationship and responsiveness of three upper-limb tests in patients with chronic obstructive pulmonary disease. Physiother Can 2013; 65:40–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhan S, Cerny FJ, Gibbons WJ, et al. Development of an unsupported arm exercise test in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil 2006; 26:180–187.discussion 188–190. [DOI] [PubMed] [Google Scholar]
- 74.Aguilaniu B, Roth H, Gonzalez-Bermejo J, et al. A simple semipaced 3-minute chair rise test for routine exercise tolerance testing in COPD. Int J Chron Obstruct Pulmon Dis 2014; 9:1009–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ozalevli S, Ozden A, Itil O, et al. Comparison of the sit-to-stand test with 6 min walk test in patients with chronic obstructive pulmonary disease. Respir Med 2007; 101:286–293. [DOI] [PubMed] [Google Scholar]
- 76.Jones SE, Kon SS, Canavan JL, et al. The five-repetition sit-to-stand test as a functional outcome measure in COPD. Thorax 2013; 68:1015–1020. [DOI] [PubMed] [Google Scholar]
- 77.Kon SS, Canavan JL, Nolan CM, et al. The 4-metre gait speed in COPD: responsiveness and minimal clinically important difference. Eur Respir J 2014; 43:1298–1305. [DOI] [PubMed] [Google Scholar]
- 78.Kon SS, Patel MS, Canavan JL, et al. Reliability and validity of 4-metre gait speed in COPD. Eur Respir J 2013; 42:333–340. [DOI] [PubMed] [Google Scholar]
- 79.Karpman C, Lebrasseur NK, Depew ZS, et al. Measuring gait speed in the out-patient clinic: methodology and feasibility. Respir Care 2014; 59:531–537. [DOI] [PubMed] [Google Scholar]
- 80.Hill CJ, Denehy L, Holland AE, et al. Measurement of functional activity in chronic obstructive pulmonary disease: the grocery shelving task. J Cardiopulm Rehabil Prev 2008; 28:402–409. [DOI] [PubMed] [Google Scholar]
- 81.Karloh M, Corrêa KS, Martins LQ, et al. Chester step test: assessment of functional capacity and magnitude of cardiorespiratory response in patients with COPD and healthy subjects. Braz J Phys Ther 2013; 17:227–235. [DOI] [PubMed] [Google Scholar]
- 82.de Camargo AA, Justino T, de Andrade CH, et al. Chester step test in patients with COPD: reliability and correlation with pulmonary function test results. Respir Care 2011; 56:995–1001. [DOI] [PubMed] [Google Scholar]
- 83.Chura RL, Marciniuk DD, Clemens R, et al. Test-retest reliability and physiological responses associated with the steep ramp anaerobic test in patients with COPD. Pulm Med 2012; 2012:653831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Roig M, Eng JJ, MacIntyre DL, et al. Associations of the stair climb power test with muscle strength and functional performance in people with chronic obstructive pulmonary disease: a cross-sectional study. Phys Ther 2010; 90:1774–1782. [DOI] [PubMed] [Google Scholar]
- 85.Skumlien S, Hagelund T, Bj⊘rtuft O, et al. A field test of functional status as performance of activities of daily living in COPD patients. Resp Med 2006; 100:316–323. [DOI] [PubMed] [Google Scholar]
- 86.Corrêa KS, Karloh M, Martins LQ, et al. Can the Glittre ADL test differentiate the functional capacity of COPD patients from that of healthy subjects? Rev Bras Fisioter 2011; 15:467–473. [DOI] [PubMed] [Google Scholar]
- 87.Karloh M, Karsten M, Pissaia FV, et al. Physiological responses to the Glittre-ADL test in patients with chronic obstructive pulmonary disease. J Rehabil Med 2014; 46:88–94. [DOI] [PubMed] [Google Scholar]
- 88.Sant’Anna T, Escobar VC, Fontana AD, et al. Evaluation of a new motion sensor in patients with chronic obstructive pulmonary disease. Arch Phys Med Rehabil 2012; 93:2319–2325. [DOI] [PubMed] [Google Scholar]
- 89.Farooqi N, Slinde F, Håglin L, et al. Validation of SenseWear Armband and ActiHeart monitors for assessments of daily energy expenditure in free-living women with chronic obstructive pulmonary disease. Physiol Rep 2013; 1:e00150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Patel SA, Benzo RP, Slivka WA, et al. Activity monitoring and energy expenditure in COPD patients: a validation study. COPD 2007; 4:107–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Waschki B, Spruit MA, Watz H, et al. Physical activity monitoring in COPD: compliance and associations with clinical characteristics in a multicenter study. Resp Med 2012; 106:522–530. [DOI] [PubMed] [Google Scholar]
- 92.Watz H, Waschki B, Meyer T, et al. Physical activity in patients with COPD. Eur Respir J 2009; 33:62–272. [DOI] [PubMed] [Google Scholar]
- 93.Cavalheri V, Donária L, Ferreira T, et al. Energy expenditure during daily activities as measured by two motion sensors in patients with COPD. Resp Med 2011; 105:922–929. [DOI] [PubMed] [Google Scholar]
- 94.Hill K, Dolmage TE, Woon L, et al. Measurement properties of the SenseWear armband in adults with chronic obstructive pulmonary disease. Thorax 2010; 65:486–491. [DOI] [PubMed] [Google Scholar]
- 95.Rabinovich RA, Louvaris Z, Raste Y, et al. Validity of physical activity monitors during daily life in patients with COPD. Eur Respir J 2013; 42:1205–1215. [DOI] [PubMed] [Google Scholar]
- 96.Andersson M, Janson C, Emtner M. Accuracy of three activity monitors in patients with chronic obstructive pulmonary disease: a comparison with video recordings. COPD 2014; 11:560–567. [DOI] [PubMed] [Google Scholar]
- 97.Kanda M, Minakata Y, Matsunaga K, et al. Validation of the triaxial accelerometer for the evaluation of physical activity in Japanese patients with COPD. Internal Med 2012; 51:369–375. [DOI] [PubMed] [Google Scholar]
- 98.Pitta F, Troosters T, Spruit MA, et al. Activity monitoring for assessment of physical activities in daily life in patients with chronic obstructive pulmonary disease. Arch Phys Med Rehab 2005; 86:1979–1985. [DOI] [PubMed] [Google Scholar]
- 99.Sugino A, Minakata Y, Kanda M, et al. Validation of a compact motion sensor for the measurement of physical activity in patients with chronic obstructive pulmonary disease. Respiration 2012; 83:300–307. [DOI] [PubMed] [Google Scholar]
- 100.Cindy Ng LW, Jenkins S, Hill K. Accuracy and responsiveness of the stepwatch activity monitor and ActivPAL in patients with COPD when walking with and without a rollator. Disabil Rehabil 2012; 34:1317–1322. [DOI] [PubMed] [Google Scholar]
- 101.Moy ML, Danilack VA, Weston NA, et al. Daily step counts in a US cohort with COPD. Respir Med 2012; 106:962–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Coronado M, Janssens JP, de Muralt B, et al. Walking activity measured by accelerometry during respiratory rehabilitation. J Cardiopulm Rehabil 2003; 23:357–364. [DOI] [PubMed] [Google Scholar]
- 103.Schönhofer B, Ardes P, Geibel M, et al. Evaluation of a movement detector to measure daily activity in patients with chronic lung disease. Eur Respir J 1997; 10:2814–2819. [DOI] [PubMed] [Google Scholar]
- 104.Steele BG, Holt L, Belza B, et al. Quantitating physical activity in COPD using a triaxial accelerometer. Chest 2000; 117:1359–1367. [DOI] [PubMed] [Google Scholar]
- 105.Vooijs M, Alpay LL, Snoeck-Stroband JB, et al. Validity and usability of low-cost accelerometers for internet-based self-monitoring of physical activity in patients with chronic obstructive pulmonary disease. Interact J Med Res 2014; 3:e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Garrod R, Bestall JC, Paul EA, et al. Development and validation of a standardized measure of activity of daily living in patients with severe COPD: the London Chest Activity of Daily Living scale (LCADL). Resp Med 2000; 94:589–596. [DOI] [PubMed] [Google Scholar]
- 107.Garrod R, Paul EA, Wedzicha JA. An evaluation of the reliability and sensitivity of the London Chest Activity of Daily Living Scale (LCADL). Resp Med 2002; 96:725–730. [DOI] [PubMed] [Google Scholar]
- 108.Carpes MF, Mayer AF, Simon KM, et al. The Brazilian Portuguese version of the London Chest Activity of Daily Living scale for use in patients with chronic obstructive pulmonary disease. J Bras Pneumol 2008; 34:143–151. [DOI] [PubMed] [Google Scholar]
- 109.Kovelis D, Zabatiero J, Oldemberg N, et al. Responsiveness of three instruments to assess self-reported functional status in patients with COPD. COPD 2011; 8:334–339. [DOI] [PubMed] [Google Scholar]
- 110.Larson JL, Kapella MC, Wirtz S, et al. Reliability and validity of the functional performance inventory in patients with moderate to severe chronic obstructive pulmonary disease. J Nurs Meas 1998; 6:55–73. [PubMed] [Google Scholar]
- 111.Leidy NK. Psychometric properties of the functional performance inventory in patients with chronic obstructive pulmonary disease. Nurs Res 1999; 48:20–28. [DOI] [PubMed] [Google Scholar]
- 112.Weldam SW, Lammers JJ, de Bruin-Veelers MC, et al. The Dutch functional performance inventory: validity and reliability in patients with chronic obstructive lung disease. Nurs Res 2015; 64:44–52. [DOI] [PubMed] [Google Scholar]
- 113.Ozkan S, Gemicioglu B, Durna Z, et al. Turkish version of the functional performance inventory used on patients with chronic obstructive pulmonary disease. Saudi Med J 2009; 30:1098–1100. [PubMed] [Google Scholar]
- 114.Leidy NK, Knebel A. In search of parsimony: reliability and validity of the Functional Performance Inventory-Short Form. Int J Chron Obstruct Pulmon Dis 2010; 5:415–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Guo AM, Han JN, Leidy NK, et al. Validation of the Chinese version of the functional performance inventory short form in patients with chronic obstructive pulmonary disease. J Clin Nurs 2011; 20:1613–1622. [DOI] [PubMed] [Google Scholar]
- 116.Leidy NK, Hamilton A, Becker K. Assessing patient report of function: content validity of the functional performance inventory-short form (FPI-SF) in patients with chronic obstructive pulmonary disease (COPD). Int J Chron Obstruct Pulmon Dis 2012; 7:543–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Wall MP. Predictors of functional performance in community-dwelling people with COPD. J Nurs Scholarsh 2007; 39:222–228. [DOI] [PubMed] [Google Scholar]
- 118.McKenna SP, Meads DM, Doward LC, et al. Development and validation of the living with chronic obstructive pulmonary disease questionnaire. Qual Life Res 2011; 20:1043–1052. [DOI] [PubMed] [Google Scholar]
- 119.McKenna SP, Twiss J, Crawford SR, et al. The living with chronic obstructive pulmonary disease scale was successfully adapted for use in Southern European (Italian and Spanish) and Eastern European (Russian) cultures. J Clin Epidemiol 2012; 65:906–914. [DOI] [PubMed] [Google Scholar]
- 120.Morimoto M, Takai K, Nakajima K, et al. Development of the chronic obstructive pulmonary disease activity rating scale: reliability, validity and factorial structure. Nurs Health Sci 2003; 5:23–30. [DOI] [PubMed] [Google Scholar]
- 121.Lee L, Friesen M, Lambert IR, et al. Evaluation of dyspnea during physical and speech activities in patients with pulmonary diseases. Chest 1998; 113:625–632. [DOI] [PubMed] [Google Scholar]
- 122.Hodgev V, Kostianev S, Marinov B. University of cincinnati dyspnea questionnaire for evaluation of dyspnoea during physical and speech activities in patients with chronic obstructive pulmonary disease: a validation analysis. Clin Physiol Funct Imaging 2003; 23:269–274. [DOI] [PubMed] [Google Scholar]
- 123.Binazzi B, Lanini B, Romagnoli I, et al. Dyspnea during speech in chronic obstructive pulmonary disease patients: effects of pulmonary rehabilitation. Respiration 2011; 81:379–385. [DOI] [PubMed] [Google Scholar]
- 124.Yoza Y, Ariyoshi K, Honda S, et al. Development of an activity of daily living scale for patients with COPD: the activity of daily living dyspnoea scale. Respirology 2009; 14:429–435. [DOI] [PubMed] [Google Scholar]
- 125.Aguilaniu B, Gonzalez-Bermejo J, Regnault A, et al. Disability related to COPD tool (DIRECT): towards an assessment of COPD-related disability in routine practice. Int J Chron Obstruct Pulmon Dis 2011; 6:387–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Wilcox TK, Chen WH, Howard KA, et al. Item selection, reliability and validity of the Shortness of Breath with Daily Activities (SOBDA) questionnaire: a new outcome measure for evaluating dyspnea in chronic obstructive pulmonary disease. Health Qual Life Outcomes 2013; 11:196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Watkins ML, Wilcox TK, Tabberer M, et al. Shortness of breath with daily activities questionnaire: validation and responder thresholds in patients with chronic obstructive pulmonary disease. BMJ Open 2013; 3:e003048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Partridge MR, Miravitlles M, Ståhl E, et al. Development and validation of the capacity of daily living during the morning questionnaire and the global chest symptoms questionnaire in COPD. Eur Respir J 2010; 36:96–104. [DOI] [PubMed] [Google Scholar]
- 129.Wingårdh A, Engström CP, Claesson L. Test-retest of a Swedish version of the pulmonary functional status and dyspnea questionnaire-modified. Scand J Occup Ther 2007; 14:183–191. [DOI] [PubMed] [Google Scholar]
- 130.Kovelis D, Segretti NO, Probst VS, et al. Validation of the modified pulmonary functional status and dyspnea questionnaire and the Medical Research Council scale for use in Brazilian patients with chronic obstructive pulmonary disease. J Bras Pneumol 2008; 34:1008–1018. [DOI] [PubMed] [Google Scholar]
- 131.Lareau SC, Meek PM, Roos PJ. Development and testing of the modified version of the Pulmonary Functional Status and Dyspnea Questionnaire (PFSDQ-M). Heart Lung 1998; 27:159–168. [DOI] [PubMed] [Google Scholar]
- 132.Weaver TE, Narsavage GL, Guilfoyle MJ. The development and psychometric evaluation of the pulmonary functional status scale: an instrument to assess functional status in plumonary disease. J Cardiopulm Rehabil 1998; 18:105–111. [DOI] [PubMed] [Google Scholar]
- 133.Chen YJ, Narsavage GL, Culp SL, et al. The development and psychometric analysis of the short-form pulmonary functional status scale (PFSS-11). Res Nurs Health 2010; 33:477–485. [DOI] [PubMed] [Google Scholar]
- 134.Tavares Ldos A, Barreto Neto J, Jardim JR, et al. Cross-cultural adaptation and assessment of reproducibility of the Duke Activity Status Index for COPD patients in Brazil. J Bras Pneumol 2012; 38:684–691. [DOI] [PubMed] [Google Scholar]
- 135.Carter R, Holiday DB, Grothues C, et al. Criterion validity of the Duke Activity Status Index for assessing functional capacity in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil 2002; 22:298–308. [DOI] [PubMed] [Google Scholar]
- 136.Yohannes AM, Greenwood YA, Connolly MJ. Reliability of the Manchester Respiratory Activities of Daily Living Questionnaire as a postal questionnaire. Age Ageing 2002; 31:355–358. [DOI] [PubMed] [Google Scholar]
- 137.Dobson F, Hinman RS, Hall M, et al. Measurement properties of performance-based measures to assess physical function in hip and knee osteoarthritis: a systematic review. Osteoarthritis Cartilage 2012; 20:1548–1562. [DOI] [PubMed] [Google Scholar]
- 138.Boer LM, Asijee GM, van Schayck OC, et al. How do dyspnoea scales compare with measurement of functional capacity in patients with COPD and at risk of COPD. Prim Care Respir J 2012; 21:202–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Marquis N, Larivée P, Dubois MF, et al. Are improvements maintained after in-home pulmonary telerehabilitation for patients with chronic obstructive pulmonary disease? Int J Telerehabil 2015; 6:21–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Coyle ME, Shergis JL, Huang ET, et al. Acupuncture therapies for chronic obstructive pulmonary disease: a systematic review of randomized, controlled trials. Altern Ther Health Med 2014; 20:10–23. [PubMed] [Google Scholar]
- 141.Divo M, Pinto-Plata V. Role of exercise in testing and in therapy of COPD. Med Clin North Am 2012; 96:753–766. [DOI] [PubMed] [Google Scholar]
- 142.Deepak TH, Mohapatra PR, Janmeja AK, et al. Outcome of pulmonary rehabilitation in patients after acute exacerbation of chronic obstructive pulmonary disease. Indian J Chest Dis Allied Sci 2014; 56:7–12. [PubMed] [Google Scholar]
- 143.Guyatt GH, Feeny DH, Patrick DL. Measuring health related quality of life. Ann Intern Med 1993; 118:622–629. [DOI] [PubMed] [Google Scholar]
- 144.Aaronson N, Alonso J, Burnam A, et al. Assessing health status and quality-of-life instruments: attributes and review criteria. Qual Life Res 2002; 11:193–205. [DOI] [PubMed] [Google Scholar]
- 145.Gimeno-Santos E, Frei A, Dobbels F, et al. Validity of instruments to measure physical activity may be questionable due to a lack of conceptual frameworks: a systematic review. Health Qual Life Outcomes 2011; 9:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Pinto-Plata VM, Cote C, Cabral H, et al. The 6-min walk distance: change over time and value as a predictor of survival in severe COPD. Eur Respir J 2004; 23:28–33. [DOI] [PubMed] [Google Scholar]
- 147.Bowen JB, Votto JJ, Thrall RS, et al. Functional status and survival following pulmonary rehabilitation. Chest 2000; 118:697–703. [DOI] [PubMed] [Google Scholar]
- 148.Meriem M, Cherif J, Toujani S, et al. Sit-to-stand test and 6-min walking test correlation in patients with chronic obstructive pulmonary disease. Ann Thorac Med 2015; 10:269–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Downs CA. Functional assessment of chronic obstructive pulmonary disease. J Am Acad Nurse Pract 2011; 23:161–167. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


