Abstract
Electronic health records (EHRs) were implemented to improve quality of care and patient outcomes. This study assessed the relationship between EHR-adoption and patient outcomes.
We performed an observational study using State Inpatient Databases linked to American Hospital Association survey, 2011. Surgical and medical patients from 6 large, diverse states were included. We performed univariate analyses and developed hierarchical regression models relating level of EHR utilization and mortality, readmission rates, and complications. We evaluated the effect of EHR adoption on outcomes in a difference-in-differences analysis, 2008 to 2011.
Medical and surgical patients sought care at hospitals reporting no EHR (3.5%), partial EHR (55.2%), and full EHR systems (41.3%). In univariate analyses, patients at hospitals with full EHR had the lowest rates of inpatient mortality, readmissions, and Patient Safety Indicators followed by patients at hospitals with partial EHR and then patients at hospitals with no EHR (P < 0.05). However, these associations were not robust when accounting for other patient and hospital factors, and adoption of an EHR system was not associated with improved patient outcomes (P > 0.05).
These results indicate that patients receiving medical and surgical care at hospitals with no EHR system have similar outcomes compared to patients seeking care at hospitals with a full EHR system, after controlling for important confounders.
To date, we have not yet seen the promised benefits of EHR systems on patient outcomes in the inpatient setting. EHRs may play a smaller role than expected in patient outcomes and overall quality of care.
INTRODUCTION
It is thought that health information technology, particularly electronic health records (EHR), will improve quality and efficiency of healthcare organizations, from small practices to large groups.1 Given these potential benefits, the federal government encouraged EHR adoption under the Health Information Technology for Economic and Clinical Health (HITECH) Act. In response, many hospitals are striving to adopt these systems and demonstrate meaningful use. In 2013, 59% of US hospitals had some type of EHR system.2 The federal incentive program defined 3 stages for timely adoption of EHR use: stage 1 is EHR adoption, stage 2 is EHR data exchange, and stage 3 is using EHRs to improve patient outcomes.3 However, despite the widespread adoption of EHR systems, only about 6% of hospitals met all criteria of stage 2 meaningful use.2–4 Thus, implementing and developing meaningful use for EHRs is still an ongoing process in the American healthcare system.
Electronic health records were originally built for billing purposes, not for research and quality improvement efforts.5 Accordingly, the impact of EHRs on quality healthcare delivery has focused on physician performance and billing precision.6 EHR studies often concentrate on process quality metrics, analyzing physician-level variability, and guideline compliance, rather than overall quality improvement or patient outcomes.7–11 Some have suggested that EHRs have the potential to decrease medical errors by providing improved access to necessary information, better communication and integration of care between different providers and visits, and more efficient documentation and monitoring.12 Many have used EHRs to decrease prescribing errors by providing real time clinical decision support.13–16 Other recent studies have begun to use EHRs to track and monitor adverse patient outcomes such as catheter-associated urinary tract infections, deep vein thrombosis, or pulmonary embolism, providing critical data to improve patient safety outcomes.17,18
Therefore, while several studies have looked at changes in quality attributed to electronic healthcare systems, overall improvements in patient outcomes associated with EHR implementation are still not yet well documented. In particular, the effect of the implementation of an EHR system on inpatient adverse events, inpatient mortality and 30-day all cause readmission for specific surgical, and medical conditions has yet to be explored. We thus sought to determine the association of hospital level-EHR systems with important patient outcomes.
The objective of this study was to determine whether hospitals with fully implemented EHR systems had better patient outcomes compared to hospitals with partial or no implemented EHR system after controlling for other important patient and hospital characteristics. Our study provides new information about the relationship between the implementation of an EHR system and the quality of healthcare delivered in the inpatient setting.
METHODS
Data Source
We utilized discharge data from the 2011 State Inpatient Databases (SID), Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality from Arkansas, California, Florida, Massachusetts, Mississippi, and New York.19 SID is an all-capture state database that allows linkage of patients overtime and contains information on patient characteristics, primary and secondary diagnoses, and procedures received. The SID database was linked to the 2011 American Hospital Association (AHA) annual survey database, which contains information on EHR utilization in different hospitals along with other important hospital characteristics.20
Patient safety indicators (PSI) are based on ICD-9-CM codes and Medicare severity diagnosis-related groups (DRGs), with specific inclusion and exclusion criteria determined by the Agency for Healthcare Research and Quality (AHRQ).21 Using the PSI software (version 4.5),22 we identified these adverse events in our dataset. Each PSI includes a unique denominator, numerator, and set of risk adjustors.23,24
Study Population
Both surgical and medical patients from several diagnostic categories were included in the study. Specifically, surgical patients undergoing pulmonary lobectomy, open abdominal aortic aneurysm repair, endovascular abdominal aortic aneurysm repair, or colectomy were included. Medical patients receiving care for acute myocardial infarction, congestive heart failure, or pneumonia were included. These categories were chosen based on their frequency, contribution to patient comorbidities, and prevalence in the medical literature.
Outcome of Interest
Our main outcomes of interest were inpatient mortality, 30-day all cause readmission rates, PSIs, and length of stay.
Statistical Analysis
We utilized univariate regression analysis to develop descriptive statistics. A hierarchical regression model relating level of EHR utilization and quality of care was developed. The independent variables were level of EHR utilization (no EHR, partial EHR, or full EHR), patient demographics, comorbidities, and medical or surgical group. The dependent variables were mortality, readmissions, and complications (measured by PSIs). Relative-risk difference in differences analyses (DiD) were used to determine the effect of implementing an EHR system on quality of care.25 The difference-in-differences analyses combined pre–post and treatment–control comparisons to eliminate some types of potential confounding. To do so, the hospitals lacking EHR systems in 2008 were selected and were then split into 3 groups: those that gained full EHRs by 2011 (treatment 1), those that gained only partial EHRs by 2011 (treatment 2), and those that still had no EHRs in 2011 (control). Direct comparison of these groups might be biased by confounders: there must be reasons why some of the hospitals adopted EHRs while others did not, and those reasons might also impact the outcomes of interest, both before and after adoption. Therefore, each hospital's event rates in 2008 are compared with the same hospital's rates in 2011, and the changes in those rates are then used to compare each treatment (i.e., EHR adoption level) with control (no EHR adoption). This analysis assumes that, in the absence of the intervention, the groups would have parallel trends and common external shocks. The use of a modified-Poisson model in these analyses enables estimation of risk ratios rather than odds ratios.26 All statistical analyses were performed using STATA version 13.0, except for the difference-in-differences analyses, which were performed using both STATA and SAS version 9.3.27
RESULTS
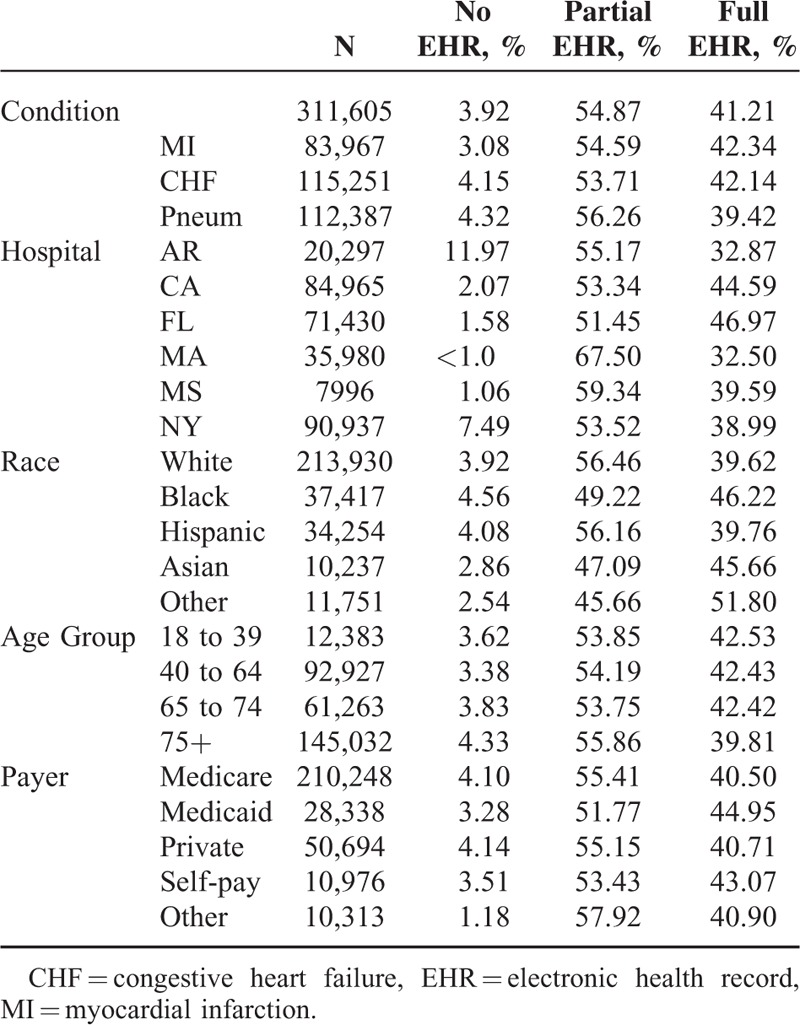
Patient characteristics are described in Tables 1 and 2. A total of 137,162 surgical patients and 311,605 medical patients were included. Medical and surgical patients sought care at hospitals reporting no EHR (3.5%), partial EHR (55.2%), and full EHR (41.3%). Of the surgical patients, 2.7% were treated in a hospital with no EHR, 55.9% were treated in a hospital with partial EHR, and 41.4% were treated in a hospital with full EHR. Of the medical patients, 3.9% were treated in a hospital with no EHR, 55.0% of patients were treated in a hospital with partial EHR, and 41.2% were treated in hospitals with full EHR.
TABLE 1.
Surgical Patient Demographics by EHR Status, 2011
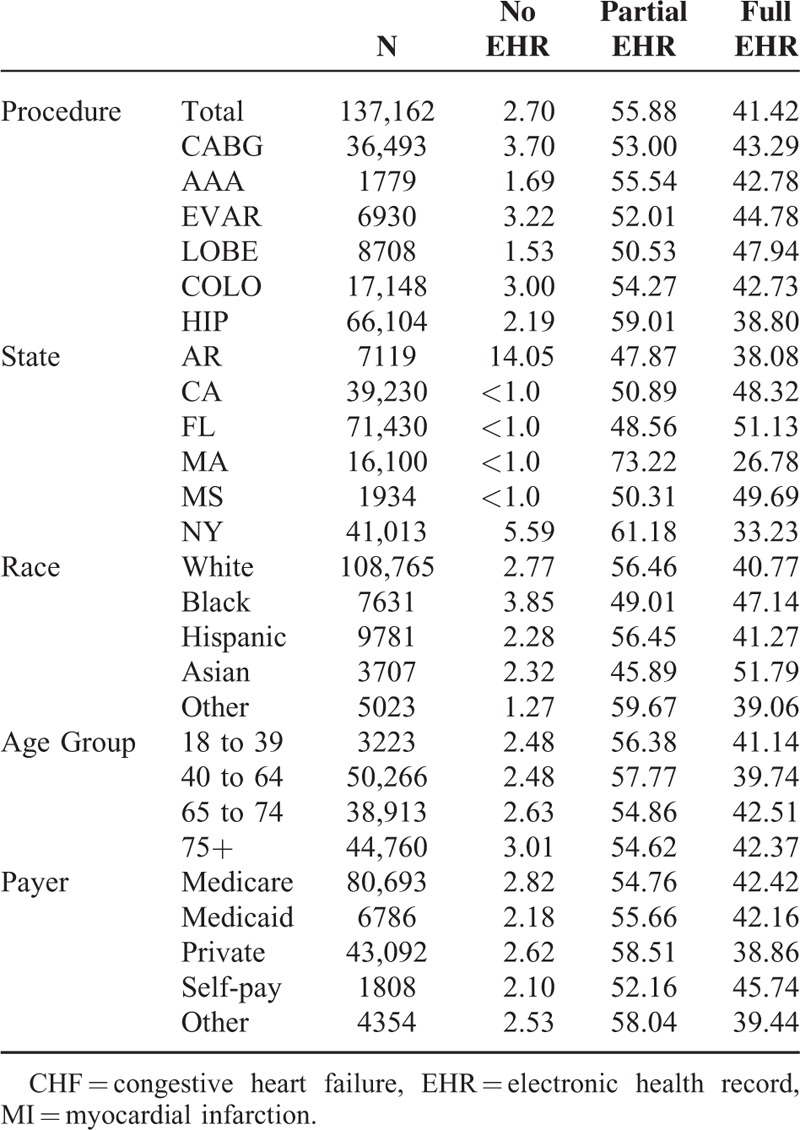
TABLE 2.
Medical Patient Demographics by EHR Status, 2011
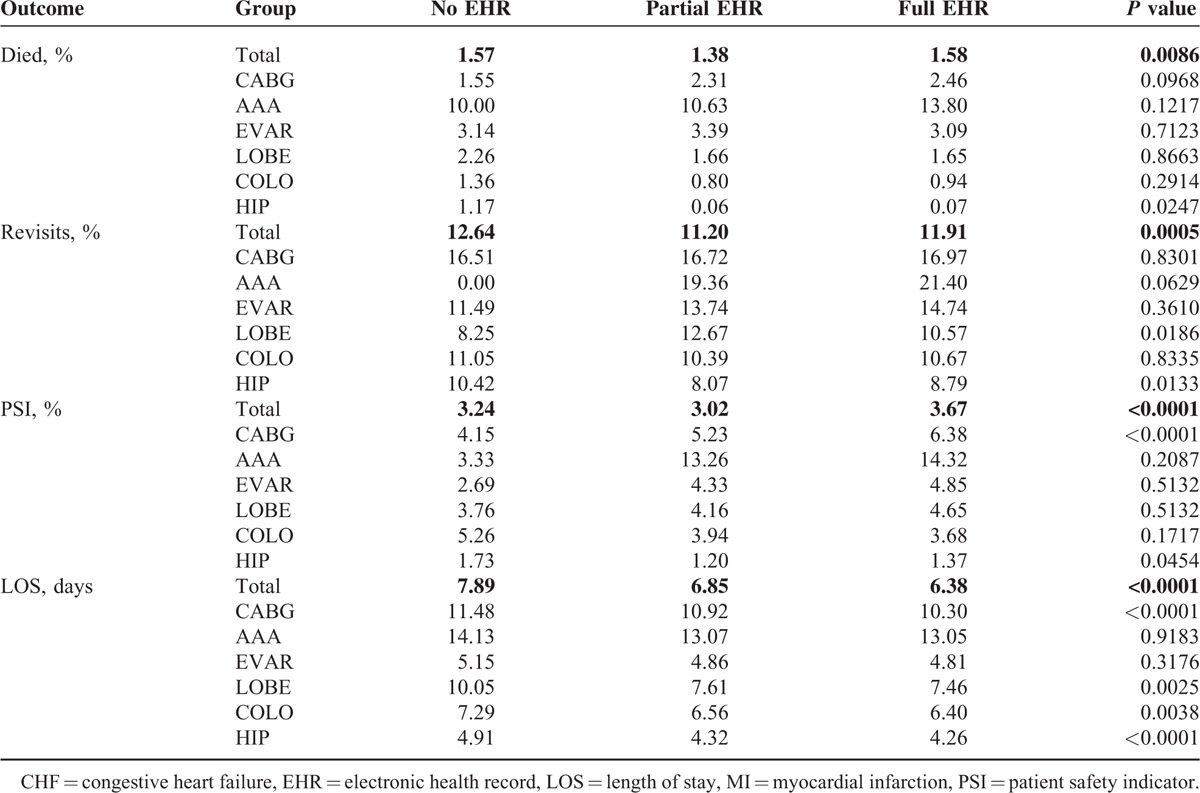
In the cross-sectional analyses, surgical patients treated at hospitals with full EHR had higher mortality rates (1.6%) than patients treated at hospitals with partial EHR (1.4%) or at hospitals with no EHR (1.6%) (P = 0.0086). Surgical patients treated at hospitals with full EHR had higher readmission rates (11.9%) than patients treated at hospitals with partial EHR (11.2%) but lower readmission rates than patients treated at hospitals with no EHR (12.6%) (P = 0.0005). Surgical patients treated at hospitals with full EHR had higher rates of complications measured by PSIs (3.7%) than patients treated at hospitals with partial EHR (3.0%) or no EHR (3.2%) (P < 0.0001). Surgical patients treated at hospitals with full EHR had a shorter length of stay (LOS), measured in days (6.38) than patients treated at hospitals with partial EHR (6.85) or no EHR (7.89) (P < 0.0001) (Table 3).
TABLE 3.
Cross-Sectional Univariate Analysis Surgical Patient Outcomes by EHR Status, 2011
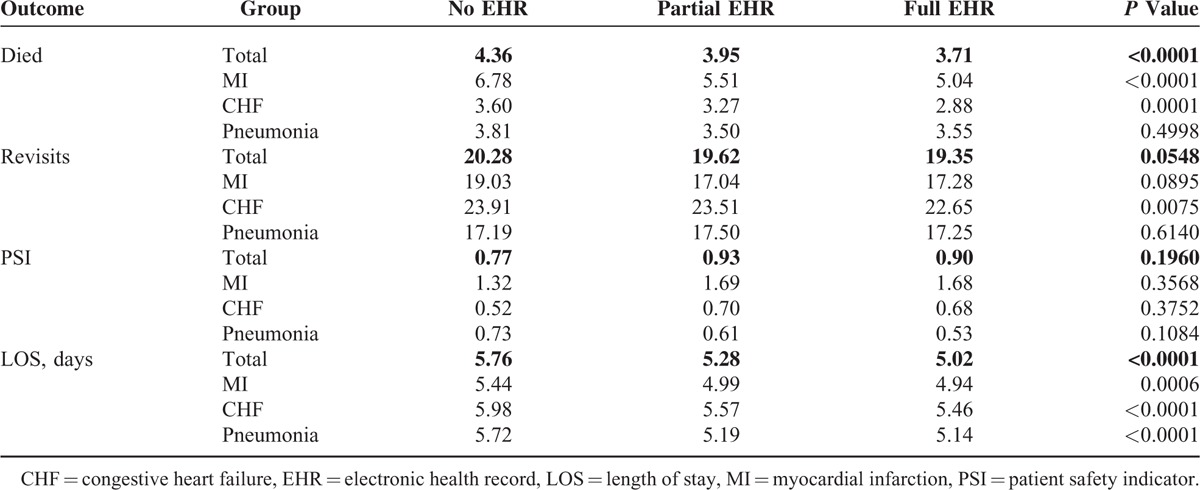
Medical patients treated at hospitals with full EHR had a lower mortality rate (3.7%) than patients treated at hospitals with partial EHR (4.0%) or no EHR (4.4%) (P < 0.0001). Medical patients treated at hospitals with full EHR did not have a statistically significant different readmission rate (19.4%) compared to patients treated at hospitals with partial EHR (19.6%) or no EHR (20.3%) (P = 0.0548). Medical patients treated at hospitals with full EHR did not have a statistically significant difference in complications measured by PSIs (0.9%) compared to patients treated at hospitals with partial EHR (0.9%) or no EHR (0.8%) (P = 0.196). Patients treated at hospitals with full EHR had a shorter length of stay (5.02) than patients treated at hospitals with partial EHR (5.28) or no EHR (5.76) (P < 0.0001) (Table 4).
TABLE 4.
Cross-Sectional Univariate Analysis Medical Patient Outcomes by EHR Status, 2011
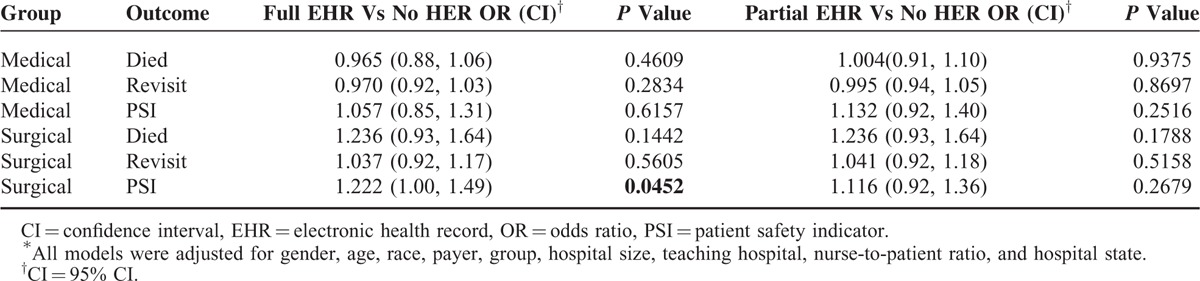
In the multiple regression analysis, there was no statistically significant difference in mortality rate among surgical patients treated at hospitals with full versus no EHR (odds ratio [OR] 1.24, P = 0.1442) or partial versus no EHR (OR 1.24, P = 0.1788) after controlling for important patient and hospital characteristics. There was no statistically significant difference in readmission rates among surgical patients treated at hospitals with full versus no EHR (OR 1.04, P = 0.5605) or partial versus no EHR (OR 1.04, P = 0.5158). There was a significant difference between rates of any complication measured by PSIs among surgical patients treated at hospitals with full versus no EHR (OR 1.22, P = 0.0452) but not between patients treated at hospitals with partial versus no EHR (OR 1.12, P = 0.2679).
There was no statistically significant difference between mortality rates among medical patients treated at hospitals with full EHR versus no EHR (OR 0.97, P = 0.4609) or partial versus no EHR (OR 1.01, P = 0.9375). There was no statistically significant difference between readmission rates among medical patients treated at hospitals with full versus no EHR (OR 0.97, P = 0.2834) or partial versus no EHR (OR 1.00, P = 0.8697). There was no statistically significant difference in complications measured by PSIs among medical patients treated at hospitals with full versus no EHR (OR 1.06, P = 0.6157) or partial versus no EHR (OR 1.13, P = 0.2516) (Table 5).
TABLE 5.
Association Between Patient Outcomes and EHR Implementation Status∗
The difference-in-differences analysis allowed us to estimate the effect of implementing an EHR system on patient outcomes, assuming that the parallel trends and common shocks assumptions are correct. These analyses found statistically significant evidence of an effect in only three cases (Table 6).
TABLE 6.
The Relative Risk∗ of EHR-Adoption on Patient Outcomes, 2008 and 2011
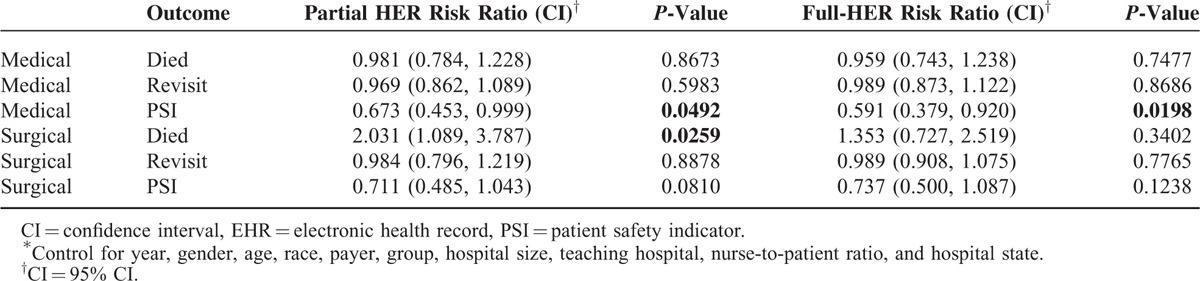
There was evidence of reduced risk of PSIs for medical patients in hospitals that had partially implemented EHRs by 2011 compared to those that still lacked EHRs in 2011 (risk ratio 0.673, 95% confidence intervals [CI] [0.45, 1.00], P-value 0.0492). There was also evidence of reduced risk of PSIs for medical patients in hospitals with fully implemented EHRs by 2011 compared with hospitals with no EHRs in 2011 (risk ratio 0.591, CI [0.38, 0.92], P-value 0.0198. Finally there was evidence of reduce risk of inpatient mortality for surgical patients in hospitals with partially implemented EHRs compared with no EHRs (risk ratio 2.031, CI [1.09, 3.79], P-value 0.0259) (Table 6).
DISCUSSION
This study tested the association between level of EHR implementation in inpatient settings and patient outcomes across 6 large, diverse states for both medical and surgical care. These results provided a preliminary glimpse at EHR meaningful use. Cross-sectional analysis found significant differences in rates of mortality, readmission, and complications between patients at hospitals with full EHR or partial EHR compared to hospitals with no EHR. However, these differences did not hold when adjusted for patient and hospital factors. Furthermore, the effect of EHR adoption was not associated with improved patient outcomes (specifically inpatient mortality, readmissions, and complications). Although EHR systems are thought to improve quality of care, this study suggests that in their current form, EHRs have not begun to reach meaningful use targets and may have a smaller impact than expected on patient outcomes.
This study builds on multiple studies highlighting the limitations of EHR systems on improving quality of care. Although EHRs have been extremely helpful for billing and physician compliance measurements, direct improvement of important patient outcomes have yet to be seen. A possible reason for this is that EHRs thus far have largely served as a recording mechanism after a patient care intervention rather than as an effective checking mechanism during the actual execution phase of patient care interventions. It has also been shown that while basic EHRs are associated with gains in quality measures, less benefit is associated with implementing advanced EHRs, suggesting that initial adoption of EHRs may actually be counterproductive by adding additional complexity into clinical settings.28 Additionally, such improvements have yet to be translated to improvements in mortality.29 Lack of improvement in other patient outcome measures has also been demonstrated. For example, 1 study demonstrated that although EHRs were associated with better rates of cholesterol testing, this did not translate to improvements in patients’ actual cholesterol levels.9 In another study of ambulatory diabetes care in clinics with and without EHRs, patients at EHR enabled clinics actually did worse in rates of meeting 2 year hemoglobin A1c, cholesterol, and blood pressure goals.30 Furthermore, data suggest that EHR implementation may actually increase the amount of time spent by patients during clinic visits.31 These studies suggest that EHRs, with their increased documentation requirements, can have unintended consequences, including clinic inefficacy. All of these studies highlight the complexity of quality of care. Accurate documentation and billing is easily obtainable with EHRs but improving recognition of clinical problems and changing provider practice is much more challenging.
Our study does have some limitations. This study relied on administrative data derived from billing claims data, which has limited information on patients’ treatment courses that can affect outcomes. Additionally, this study uses hospital survey data to identify the level or EHR adoption, which is prone to reporting errors. Furthermore, changes in quality of care after the implementation of EHRs may be attributable in part to non-EHR factors, which cannot be fully accounted for in our analysis.
This population-based study builds on existing literature to demonstrate that EHRs are not yet associated with gains in measures of inpatient mortality, readmissions, and PSIs. Results here suggest that differences in outcomes at hospitals with different levels of EHR utilization may be attributable to other patient and hospital factors rather than EHR utilization itself. As federal incentives encourage EHR adoption and hospitals strive for meaningful use, it will be important to further characterize the benefits received from EHRs.
Acknowledgements
The authors thank National Cancer Institute of the National Institutes of Health under Award Number R01CA183962 and Agency for Healthcare Research and Quality (grant number R01HS024096) for the support. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health and Agency for Healthcare Research and Quality.
Footnotes
Abbreviations: AHA = american hospital association, CI = confidence interval, DiD = difference-in-differences, DRG = diagnosis-related group, EHR = electronic health record, HCUP = health care utilization project, LOS = length of stay, OR = odds ratio, PSI = patient safety indicator, SID = state inpatient database.
THB conceived and designed the study, supervised and contributed to the data analysis, interpreted results, and made substantial revisions to the paper; DM contributed to the study design, conducted the data analysis, and contributed to revisions of the paper; SY drafted the paper and contributed to the interpretation of the data analysis; KM contributed to the interpretation of the data analysis and revisions of the paper; and CC contributed to the interpretation of the data analysis and revisions of the paper.
Preliminary findings from this paper were presented at the Academy Health Research Meeting, San Diego, June 8–10, 2014 and at AMIA Annual Symposium, San Francisco, November 14–18, 2015.
Funding Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Number R01CA183962. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This project was supported by grant number R01HS024096 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Buntin MB, Burke MF, Hoaglin MC, et al. The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Aff (Millwood) 2011; 30:464–471. [DOI] [PubMed] [Google Scholar]
- 2.Adler-Milstein J, DesRoches CM, Furukawa MF, et al. More than half of US hospitals have at least a basic EHR, but stage 2 criteria remain challenging for most. Health Aff (Millwood) 2014; 33:1664–1671. [DOI] [PubMed] [Google Scholar]
- 3.Blumenthal D. Launching HITECH. N Engl J Med 2010; 362:382–385. [DOI] [PubMed] [Google Scholar]
- 4.D’Amore JD, Mandel JC, Kreda DA, et al. Are Meaningful Use Stage 2 certified EHRs ready for interoperability? Findings from the SMART C-CDA Collaborative. J Am Med Inform Assoc 2014; 21:1060–1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hersh WR, Weiner MG, Embi PJ, et al. Caveats for the use of operational electronic health record data in comparative effectiveness research. Med Care 2013; 51 (8 Suppl 3):S30–S37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lynn J, McKethan A, Jha AK. Value-based payments require valuing what matters to patients. JAMA 2015; 314:1445–1446. [DOI] [PubMed] [Google Scholar]
- 7.Harkema H, Chapman WW, Saul M, et al. Developing a natural language processing application for measuring the quality of colonoscopy procedures. J Am Med Inform Assoc 2011; 18 Suppl 1:i150–i156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mehrotra A, Dellon ES, Schoen RE, et al. Applying a natural language processing tool to electronic health records to assess performance on colonoscopy quality measures. Gastrointest Endosc 2012; 75:1233–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ancker JS, Kern LM, Edwards A, et al. Associations between healthcare quality and use of electronic health record functions in ambulatory care. J Am Med Inform Assoc 2015; 22:864–871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ancker JS, Kern LM, Edwards A, et al. How is the electronic health record being used? Use of EHR data to assess physician-level variability in technology use. J Am Med Inform Assoc 2014; 21:1001–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Allen JI. Quality measures for colonoscopy: where should we be in 2015? Curr Gastroenterol Rep 2015; 17:10. [DOI] [PubMed] [Google Scholar]
- 12.Schiff GD, Bates DW. Can electronic clinical documentation help prevent diagnostic errors? N Engl J Med 2010; 362:1066–1069. [DOI] [PubMed] [Google Scholar]
- 13.Bates DW, Gawande AA. Improving safety with information technology. N Engl J Med 2003; 348:2526–2534. [DOI] [PubMed] [Google Scholar]
- 14.Kaushal R, Kern LM, Barron Y, et al. Electronic prescribing improves medication safety in community-based office practices. J Gen Intern Med 2010; 25:530–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Devine EB, Hollingworth W, Hansen RN, et al. Electronic prescribing at the point of care: a time-motion study in the primary care setting. Health Serv Res 2010; 45:152–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abramson E, Kaushal R, Vest J. Improving immunization data management: an editorial on the potential of Electronic Health Records. Expert Rev Vaccines 2014; 13:189–191. [DOI] [PubMed] [Google Scholar]
- 17.Shepard J, Hadhazy E, Frederick J, et al. Using electronic medical records to increase the efficiency of catheter-associated urinary tract infection surveillance for National Health and Safety Network reporting. Am J Infect Control 2014; 42:e33–e36. [DOI] [PubMed] [Google Scholar]
- 18.Rochefort CM, Verma AD, Eguale T, et al. A novel method of adverse event detection can accurately identify venous thromboembolisms (VTEs) from narrative electronic health record data. J Am Med Inform Assoc 2015; 22:155–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Agency for Healthcare Research and Quality. HCUP Databases. In: Human and Health Services, ed. Rockvelle, MD: Agency for Healthcare Research and Quality, 2013. [Google Scholar]
- 20.American Hospital Association. The AHA annual survey database. Chicago, IL: American Hospital Association, 2008. [Google Scholar]
- 21.McDonald KM, Romano PS, Geppert J, et al. Measures of Patient Safety Based on Hospital Administrative Data – The Patient Safety Indicators. Rockville, MD: Agency for Healthcare Research; 2002. [PubMed] [Google Scholar]
- 22.PSI SAS Syntax software [program]. 4.1a version. [Google Scholar]
- 23.AT Agency for Healthcare Research and Quality. AHRQ Quality Indicator: Comparative Data for the PSI based on the 2008 Nationwide Inpatient Sample (NIS). In: Human and Health Services, ed. Rockville, MD: Agency for Healthcare Research and Quality, 2010. [Google Scholar]
- 24.Agency for Healthcare Research and Quality JT AHRQ Quality Indicator: Risk Adjustment Coefficients for the PSI 4 1a ed Rockville, MD: Agency for Healthcare Research and Quality D, 2011 [Google Scholar]
- 25.Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA 2014; 312:2401–2402. [DOI] [PubMed] [Google Scholar]
- 26.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004; 159:702–706. [DOI] [PubMed] [Google Scholar]
- 27.Stata [program]. College Station, TX, 2009. [Google Scholar]
- 28.Jones SS, Adams JL, Schneider EC, et al. Electronic health record adoption and quality improvement in US hospitals. Am J Manag Care 2010; 16 (12 Suppl HIT):S64–S71. [PubMed] [Google Scholar]
- 29.Campanella P, Lovato E, Marone C, et al. The impact of electronic health records on healthcare quality: a systematic review and meta-analysis. Eur J Public Health 2016; 26:60–64.doi: 10.1093/eurpub/ckv122. [DOI] [PubMed] [Google Scholar]
- 30.Crosson JC, Ohman-Strickland PA, Cohen DJ, et al. Typical electronic health record use in primary care practices and the quality of diabetes care. Ann Fam Med 2012; 10:221–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Samaan ZM, Klein MD, Mansour ME, et al. The impact of the electronic health record on an academic pediatric primary care center. J Ambul Care Manage 2009; 32:180–187. [DOI] [PubMed] [Google Scholar]


