Supplemental Digital Content is available in the text
Abstract
This study used a system evaluation method to summarize China's experience on improving the coverage of hepatitis B vaccine, especially the strategies employed to improve the uptake of timely birth dosage. Identifying successful methods and strategies will provide strong evidence for policy makers and health workers in other countries with high hepatitis B prevalence.
We conducted a literature review included English or Chinese literature carried out in mainland China, using PubMed, the Cochrane databases, Web of Knowledge, China National Knowledge Infrastructure, Wanfang data, and other relevant databases.
Nineteen articles about the effectiveness and impact of interventions on improving the coverage of hepatitis B vaccine were included. Strong or moderate evidence showed that reinforcing health education, training and supervision, providing subsidies for facility birth, strengthening the coordination among health care providers, and using out-of-cold-chain storage for vaccines were all important to improving vaccination coverage.
We found evidence that community education was the most commonly used intervention, and out-reach programs such as out-of-cold chain strategy were more effective in increasing the coverage of vaccination in remote areas where the facility birth rate was respectively low. The essential impact factors were found to be strong government commitment and the cooperation of the different government departments.
Public interventions relying on basic health care systems combined with outreach care services were critical elements in improving the hepatitis B vaccination rate in China. This success could not have occurred without exceptional national commitment.
INTRODUCTION
Hepatitis B is a viral infection, spread through blood and bodily fluids, which infects the liver. According to the World Health Organization (WHO) approximately 2 billion people currently are infected by hepatitis B virus (HBV), and an estimated 240 million people are chronic HBV carriers.1 More than 780,000 people die every year due to the consequences of HBV such as hepatic failure, cirrhosis of the liver, and liver cancer.2 Hepatitis B is especially a serious problem in developing countries due to the high infection rate. In China, the National Sero Epidemiological Survey of Hepatitis B in 2006 indicated that the HBV carrier rate was 7.8% in the national population,3 and in 2012, the prevalence was as high as 80.7 per 100,000,4 making China a high endemic area. In the last few years, more and more data have been produced in developing countries where the most common route of infection is still vertical transmission from mother to child.5 About 80% to 90% of infants infected during the 1st year of life and 30% to 50% of children infected before the age of 6 years develop chronic infection. Since 15% to 25% of adults who become chronically infected during childhood die from hepatitis B-related liver cancer or cirrhosis,2 prevention of mother-to-child disease transmission has been crucial to reducing prevalence.
Safe and effective vaccines exist to prevent infection with HBV, and the WHO recommends all infants receive a first vaccine dose within 24 hours of birth to protect against HBV infection.6 By the end of 2013, although global coverage with 3 doses of hepatitis B vaccine was estimated at 81% and as high as 92% in the Western Pacific, global coverage with a birth dose for hepatitis B vaccine was estimated at 38%, only 11% in the African Region.7
China has made great progress with universal vaccination for hepatitis B; the latest data from WHO suggests over 95% of newborns receive a timely birth dose (TBD) of hepatitis B vaccine.8 The vaccine was introduced in 1987, and in 1992 the Chinese government established the National Hepatitis B Immunization Plan,9 which recommended timely first dose within 24 hours of birth and subsequent doses at ages 1 and 6 months.10 However, user fees charged to parents by local health departments for vaccine purchase and administration were serious barriers to uptake at this time.11 In 2002, the Global Alliance on Vaccine and Immunization (GAVI) partnered with the Government of China to provide hepatitis B vaccine for free and cap user fees to ensure affordability.12 By 2005, hepatitis B vaccination of infants was fully integrated into the routine immunization programme and provided completely free of charge nationally.13 As a result of these policies, the 3 dose vaccine coverage tripled from 30.0% for children born in 1992 to 99.7% for children born in 2012, and receipt of a TBD increased from 22.2% to 95.7% for children born during this interval. Most importantly, the carrier rate in Chinese children less than 5 years of age fell to 0.96% in 2006, and further to 0.32% in 2014 (from 10% in the 1990s);14 this reduction of 90% meets the targets set by the WHO.15 Many women of childbearing age in China today were born before hepatitis B vaccine was fully integrated into the routine immunization policy, so the Government has acted to try to sustain reductions in prevalence of hepatitis B infection. In 2010 the Ministry of Health (MoH) recommended screening of all pregnant women for hepatitis B surface antigen and vaccination and hepatitis B immunoglobulin administration within 24 hours of birth for all infants born to hepatitis B surface antigen positive mothers.12
Since the introduction of the first national policy on Hepatitis B vaccination, the government of China has employed many strategies to improve coverage of the timely first dose and subsequent doses for infants. For example, increasing the percentage of births that occur in hospitals, improving vaccine availability in health facilities, building collaboration between different departments, increasing the awareness of the importance of TBD administration, and providing subsidies to village doctors to provide vaccines.
There may be important lessons from China for other countries where coverage of hepatitis B vaccination lags behind and targets remain unmet. We conducted a systematic review of the literature on China's experience in improving the coverage of hepatitis B vaccine, especially strategies to improve the uptake of TBD. We sought to address 3 main questions: what interventions or strategies have been used in China to increase hepatitis B vaccination coverage?; is there any evidence of impact of strategies or interventions on vaccination coverage?; and what can we learn about factors influencing successful implementation of interventions in China?
METHODS
Selection Criteria
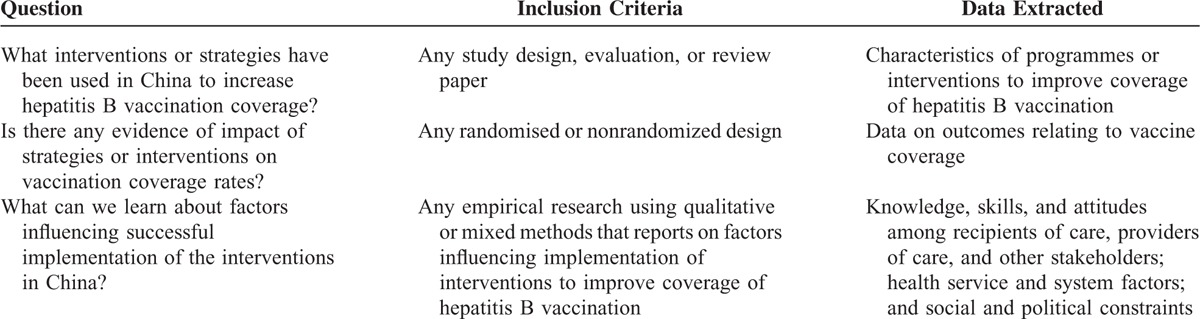
This systematic review only included English or Chinese studies and reports carried out in mainland China. For our objective relating to the strategies used in China, we included any study design including program evaluations and review papers. For our objective relating to the impact of interventions, we included original research, using any randomized or nonrandomized design that assessed outcomes relating to vaccine coverage (number of children fully immunized with 3 doses, or number of infants receiving TBD of vaccine). To address our objective about implementation experiences, we included research or descriptions of the facilitators or barriers to implementing strategies or interventions to increase vaccination coverage or uptake. Studies that involved multiple vaccines were also accepted, as long as one of the vaccines was for hepatitis B (see Table 1).
TABLE 1.
Inclusion Criteria and Data Extracted
Studies were excluded if: 1) the study was restricted to efficacy of the vaccine or other treatment to mothers or the neonates, without analysis of impact factors on vaccine coverage; 2) there was no clear source(s) of evidence or a research method; 3) full-text version was not accessible.
Search Strategy
We searched PubMed, EMBASE, the Cochrane Database of Systematic Reviews, Web of Knowledge, China National Knowledge Infrastructure, and Wanfang data for all relevant studies published in English or Chinese from post-1992 when the first national plan was implemented up to December 24th, 2014. Keywords used were “HBV” OR “hepatitis B,” “vaccination” OR “immunization,” “coverage,” “mother to child” OR “mother to infant” OR “vertical” OR “prenatal transmission” OR infant OR “new-born,” and “China” OR “Chinese” (see Supplementary Table S1 Supplemental Content, which showed an example search strategy used to search PubMed). The strategy was adjusted as necessary for other electronic databases. We also examined reference lists of relevant studies and reviews to identify additional relevant papers.
The first author screened titles and abstracts generated from the initial search to exclude those studies not directly meeting the inclusion criteria. Following this, 2 authors independently screened the full texts in order to select studies relevant to our objectives. Uncertainties and disagreements during all the process were resolved through discussion with coauthors.
Quality Assessment of Included Studies
Each study included in the review that provided data on impact (n = 19) was appraised using quality-assessment tool developed by the Effective Public Health Practice Project in Canada.16 The Effective Public Health Practice Project is a widely used tool used to evaluate a variety of study designs including randomized controlled trials, before-and-after and case–control studies. The tool assesses 6 components according to its dictionary: selection bias, study design, confounders, blinding, data collection method, and withdrawals/dropouts.17 Each component is rated as strong (3 points), moderate (2 points), or weak (1 point), and component scores are averaged to provide the total score.16 Studies are assigned a global rating result of weak (1.00–1.50), moderate (1.51–2.50), or strong (2.51–3.00) based on the total score.18
Synthesis
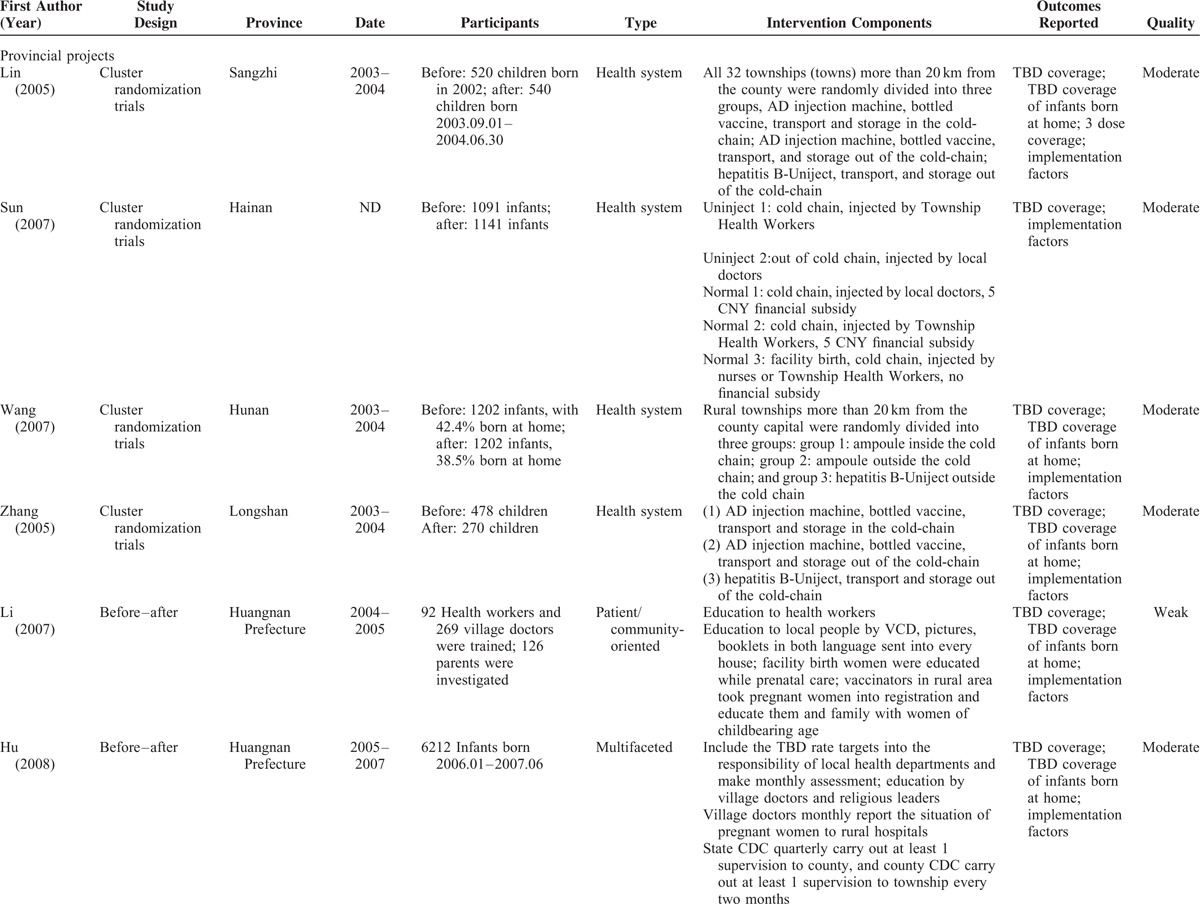
The first author extracted information on the characteristics of each included study, using a standard form, and at the same time categorized the studies into those that reported national programmes and those that described provincial projects. We used a systematic narrative approach to summarize key characteristics of interventions or strategies to increase hepatitis B vaccination coverage, including the study design, participants, type of intervention, intervention components, and outcomes reported (see Table 2 ). We described interventions and categorized them based on the system used by the Cochrane Review of interventions to improve coverage of childhood vaccinations.19 Patient- or community-oriented interventions included public health education targeted toward pregnant women and their families. Provider-oriented interventions included health education, update courses, or training for health care providers to improve their awareness and responsibility for administering timely first dose and subsequent doses as well as more specific interventions targeting provider behavior including payment and incentives/punishment and improved monitoring and supervision. Health system interventions are those designed to improve the quality of vaccine delivery services or access to services via central and local policies, laws, regulations, and guidelines for improving immunization coverage or reducing disease; integration of immunization services with other services; interventions to improve the quality of services; centralized registration; and management system for all pregnant women. We categorized strategies as “multiple levels” if they included any combination of these different levels. As the included studies reported on different strategies or combinations of interventions, used various designs and methods, and reported on different outcomes we used a narrative approach to summarize data on the impact of strategies or interventions on vaccination coverage rates. Data on coverage of TBD, TBD in home births, or 3 doses of vaccine summarized this in a table to show impact of strategies or interventions on vaccination coverage rates (Table 3).
TABLE 2.
Characteristics of Included Studies Grouped by National Programmes and Provincial Projects
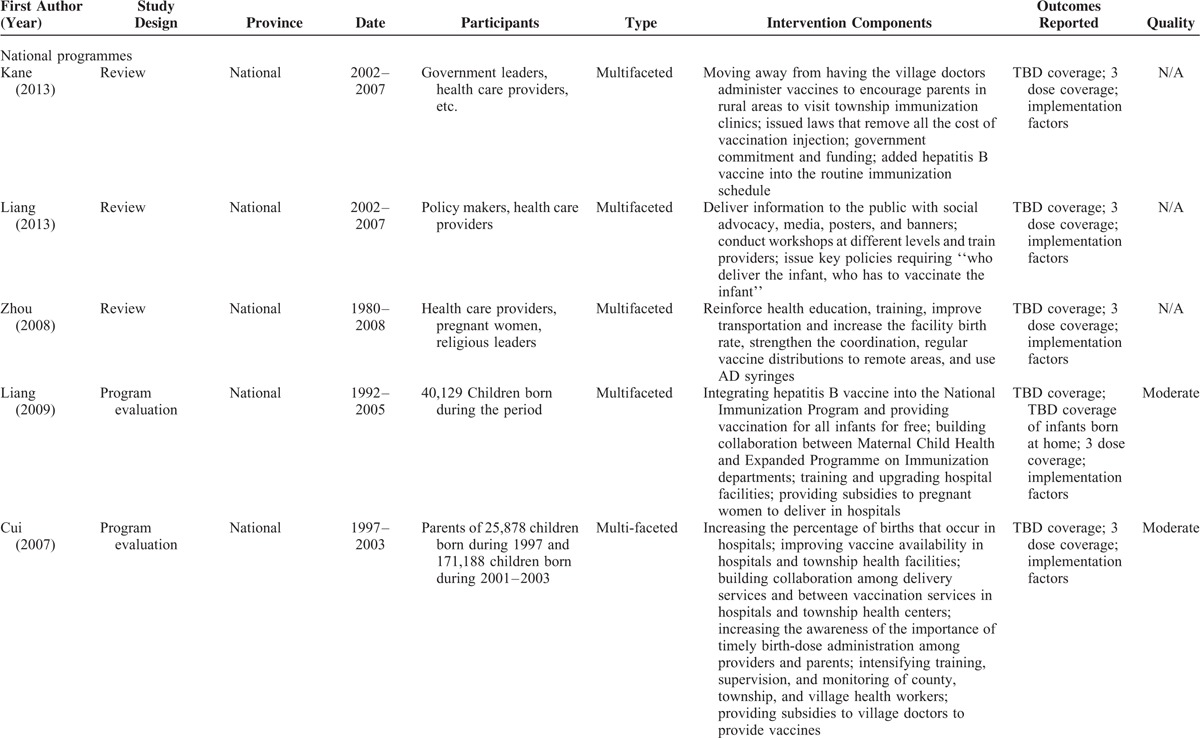
TABLE 2 (Continued).
Characteristics of Included Studies Grouped by National Programmes and Provincial Projects
To help extract relevant information on factors influencing successful implementation we used a proforma adapted from the SURE framework,20 used in other reviews of this nature.21 The framework offers a comprehensive list of possible factors affecting implementation of health system interventions, including knowledge, skills and attitudes among recipients of care, providers of care, and other stakeholders; health service and system factors; and social and political constraints. We extracted findings from the results and discussion sections of included studies into the framework and reviewed these for relevance and consistency. The whole team discussed the content and meaning of emerging themes and decided on final themes to present.
The authors did not access any individual information and had no interactions with the patients involved in this study. So, neither ethics review nor informed consent was required for the current analysis.
RESULTS
We identified 2100 papers from the electronic search and 9 papers from reference lists. A total of 1438 titles and abstracts were considered after duplicate records were removed, and of these, 305 full-text articles were assessed for eligibility. A further 286 were excluded as it was difficult to determine the study design or methods used to assess impact. A total of 19 papers were included in the synthesis. The study selection process is shown in Figure 1.
FIGURE 1.
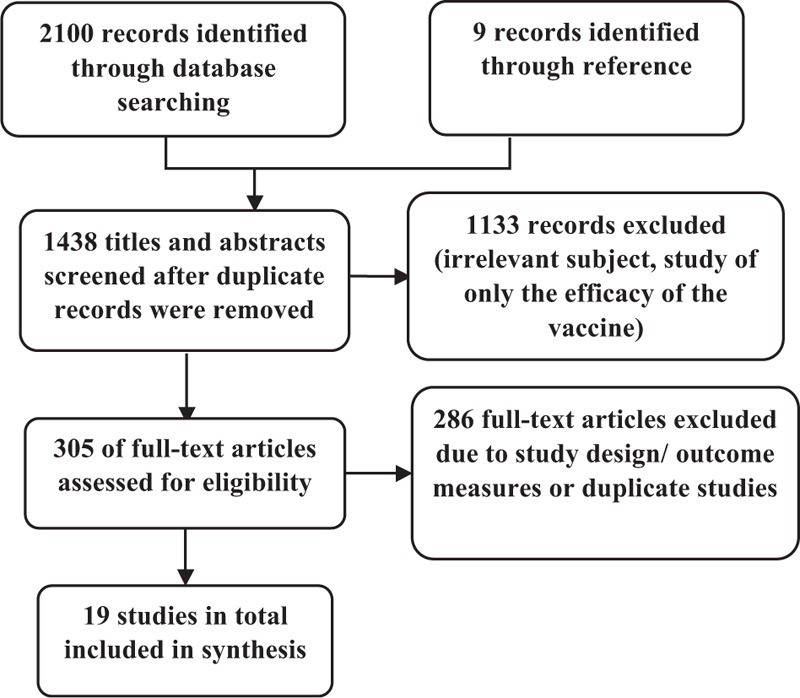
Flow diagram of study search and selection process.
Study designs included before–after studies (n = 7), cluster randomization trials (n = 4), program evaluations (n = 5), and reviews (n = 3). Eight papers were published in English and 11 in Chinese. Of the 19 included studies14,15,22–33 reported on multiple strategies employing a combination of interventions to improve coverage of hepatitis B vaccination; four34–37 reported on health system interventions and only one38 reported patient/community-oriented interventions. All these included studies contain information about implementation factors too. Table 2 shows the characteristics of the included studies.
QUALITY OF INCLUDED STUDIES
No study was rated as “strong,” and most, including all 4 cluster randomization trials, were rated “moderate.” One before-and-after study and 1 programme evaluation were rated “weak.” For both the randomized controlled trials and before-and-after studies, the main limitations were the lack of blinding and no description of methods of randomization. Since most of the data were derived from routine reports, the outcome assessors were usually aware of the intervention status of participants in the projects and since education or other interventions were usually community-based, the study participants were aware of the research objectives.
WHAT INTERVENTIONS HAVE BEEN TRIED IN CHINA?
National Programmes
Among the 19 included studies, 5 including 3 reviews and 2 program evaluations described programmes implemented at national level.14,15,23,29,33 The all programmes used multiple interventions or strategies to achieve the targets. Kane et al14 and Liang et al29 both described the GAVI funded project, while Kane focused more on the political and social context and the inception of the project on the health system level and Liang described mainly the exact strategies involved in the project. The GAVI programme was designed to increase the coverage of hepatitis B vaccination in poor rural areas through health education to increase the awareness of the parents, training for health providers and health workers, improving the number of women giving birth in hospital, and key government policies requiring “who deliver the infant, who has to vaccinate the infant.” Most important of all, the government invested equal funding with GAVI to remove the cost of vaccination and added hepatitis B vaccine into the routine immunization schedule. Zhou et al33 reviewed hepatitis B vaccine used in China and the impact of the vaccination implementation from 1980 to 2008. The strategies mentioned in the review included reinforcing health education, training, improving transportation to increase the facility birth rate, strengthening the coordination between different groups, regular vaccine distributions to remote areas, and using of auto-disposable (AD) syringes.33 Liang et al15 described the results of the National Sero Epidemiological Survey of Hepatitis B in 2006 and evaluated the impact of integrating hepatitis B vaccine into the National Immunization Program and providing vaccination for all infants for free. Cui et al23 reported China's progress in increasing coverage among infants with universal infant hepatitis B vaccination, which emphasized the training of county, township, and village health workers at different levels and the importance of the integration of hepatitis B vaccination into the government immunization plan.
Provincial Projects
System-Oriented Interventions
Among the 14 studies focusing on provincial projects, 4 reported health system interventions and specifically effect of out-of-cold chain strategies. Lin et al,34 Wang et al,36 and Zhang et al37 divided the target population into 3 groups randomly. In the control group, hepatitis B vaccine was provided in ampoules, stored in cold chain, and administered with AD syringes to infants in facilities. In the ampoule outside the cold chain group, vaccine was stored out of the cold chain and administered by the help of village-based health workers to infants born at home. In the hepatitis B-Uniject outside the cold chain group, vaccine was packaged in a prefilled injection device and other strategy was the same as the trial group.36 Sun et al35 used similar strategy but divided the participants into 5 groups, including: Uninject group used cold chain for the hepatitis B vaccine which was delivered by township health workers; Uninject group 2 delivered the vaccine by local doctors out of the cold chain; control groups all delivered the vaccine with cold chain while in group 1 vaccine was injected by local doctors with 5 CNY financial subsidy, in group 2 vaccine was injected by township health workers with 5 CNY financial subsidy, and in group 3 vaccine was delivered by nurses or township health workers in hospitals without financial subsidy.
Patient/Community-Oriented Interventions
One study evaluated a patient/community-oriented intervention. Li et al38 analyzed the effect of health education on improving the TBD coverage of hepatitis B in rural and pasturing areas in Qinghai Province. Interventions included distribution of multilanguage posters, pictures, booklets and leaflets in the community, broadcast of educational films during traditional religious congregation, and health education in the clinics or at home on the immunization schedule for those registered pregnant women.
Multiple Levels
The other 9 provincial level studies (6 before-and-after studies and 3 program evaluations) reported on multiple strategies to improve coverage of HBV vaccination. Usually system-oriented interventions were combined with provider-oriented strategies since health system would always affect the way heath care was delivered. In some projects, all the 3 levels of strategies were combined together.
Among the 9 studies, 6 mentioned patient-oriented strategies while 5 mentioned system-oriented strategies. Community education was the most common intervention in the included studies, usually combined with other interventions as a basic strategy. Chen et al,22 Gao et al,24 Gou and Qi,25 Guan et al,26 Han et al,27 and Qi et al30 all mentioned strategies to raise public awareness. For example, using rural radio stations to publicize knowledge, creating simple and appealing educational literature, posters, and interactive materials.
For families living in remote and rural areas, the TBD rate was quite low because of the difficulty in accessing health care facilities for hospital birth. Chen et al22 developed a centralized registration and management system for pregnant women, while Han et al,27 Hu et al,28 Qi et al,30 and Yvan et al31 mentioned outreach programmes in which vaccinators in rural areas actively vaccinate the infants. Usually village doctors collaborated with the outreach vaccinators to take registered of the pregnant women and reported the probable place and timing of the delivery to rural hospitals to help organizing for early notification of the delivery. At the time of birth, vaccinators were identified to fetch the vaccine stored locally and immediately administer it at home births. In that way, the local clinics can manage the information of the pregnant women and vaccinate the infant either in the facility or at home with the help of village doctors. These interventions were most successfully implemented in prefectures with highest proportion of home births but received less attention where hospital births were more common.31
To assure full and sustainable access of the recommended hepatitis B vaccination, the MoH issued a number of regulations to improve the management of the vaccination service, especially in the institutions that deliver new-borns. Yvan reported the regulation requiring “who delivers the infant, who has to vaccinate the infant” to assure have designated persons to provide TBD.31
Among the 9 provincial level studies, 5 involved provider-oriented interventions. Training was used to improve health care providers’ knowledge and awareness of vaccination; various types of training were used.31,32 Chen et al22 and Gou and Qi25 also trained government officials and community leaders as well as healthcare providers. To fully mobilize health care workers, some programs provided subsidies to village doctors, midwives, and vaccinators to encourage them to implement vaccines at home births.27,31 The China MoH provided incentives to pregnant women to give birth in hospital according to the policy issued in 2009, and there were 2 studies specifically mentioned this policy. Yvan et al31 mentioned that the increase in the proportion of hospital deliveries was a key determinant of the improvement of TBD coverage, and Han et al27 described the subsidy provided to the pregnant women for facility birth by implementing New Cooperative Medical policies.
IMPACT OF THE INTERVENTIONS
Here, we provide a summary of the available data on impact of the interventions on vaccine coverage. Because of the variability in the type of studies, interventions and outcome measures reported in the included studies, the impact data were also presented by the type of intervention (see Table 3).
Health System Interventions
Among the 4 studies focusing on the out-of-cold chain strategy, three35–37 only reported the increase of the TBD rate of hepatitis B vaccination as an outcome, while Lin et al34 reported the coverage of the 3 doses as well as the TBD rate. After the implementation of the intervention, coverage of the birth dose of hepatitis B vaccine administered on time increased in all groups while the hepatitis B-Uniject outside the cold chain group showed the highest TBD coverage increase. Coverage rate was much higher in the out-of-cold chain group than the normal group with P < 0.05 for differences between each of the groups, especially among infants born at home.36 All the 4 studies affirmed the effect of the out-of-cold chain strategy and emphasized that the additional use of hepatitis B-Uniject device could further improve the coverage of vaccination out of cold chain.
Patient/Community-Oriented Interventions
In Qinghai Province, after the 1 year education project from 2004 to 2005, the TBD rate of hepatitis B vaccination increased by 32% from 42.61% to 75.02% after the program, among which the TBD rate of infants born at home increased from 19.58% to 59.56% while the awareness of the importance of TBD among the parents also increased by about 40% than the base investment.38 The result showed the positive correlation between the knowledge level of the community and the implementation of the vaccination.
Multiple Levels
Since most of the included studies used more than 1 type of intervention, we summarized the overall result of the projects.
Two studies described the impact of the China GAVI project implemented since 2002.14,29 Through the project, the 85% hepatitis B3 coverage goal was reached in 98% of GAVI China project counties, the 75% TBD coverage goal was reached in 80% of GAVI project counties, and AD syringes were introduced into 100% of GAVI-supported areas.29 This project also impacted the national policy decisions as the MoH issued a number of key policies and regulations that assured full and sustainable access to the recommended hepatitis B vaccine series for all infants upon initial implementation and during the GAVI project.
Three studies evaluated the progress of national projects during different time periods.15,23,33 Cui et al (2007) compared the 2 national vaccination coverage surveys. The result indicated that estimated 3-dose hepatitis B coverage increased substantially overall, from 70.7% among children born in 1997 to 89.8% among children born in 2003, while timely hepatitis B birth-dose coverage also increased by more than 46% (29.1% in 1997 to 75.8% in 2003).23 Liang et al15 described the result of the national serosurvey and concluded that hepatitis B vaccine coverage (3 doses) increased by 63.4% (from 30.0% for children born in 1992 to 93.4% for children born in 2005) while receipt of a TBD increased from 22.2% to 82.6% for children born during this interval. Zhou et al33 reviewed the implementation of mass vaccination of hepatitis B vaccine from 1980 to 2008 and stated that the overall coverage of hepatitis B vaccine in infants has increased steadily and reached more than 95.0% in urban and 97.0% in rural areas.
The all last 9 studies used a series of strategies including at least 2 levels of intervention. All the projects reported significant increases in the coverage of hepatitis B vaccination. The TBD coverage reached a level ranging from 67% to over 95% from the baseline level ranging from 44% to 75%. Seven studies also reported the increase of the TBD coverage among infants born at home. The result indicated that although in most studies the TBD coverage reached a level of 60% to 80%, there was still challenge for this kind of population since in some rural areas the TBD coverage only increased from 9% to 14% to about 29%.26,31
FACTORS INFLUENCING THE IMPLEMENTATION OF HEPATITIS B VACCINATION
Among the included studies, the 3 reviews14,29,33 and 5 program evaluations15,22,23,31,32 described the factors influencing the success of the vaccination implementation directly, while in cluster randomization trials34–37 or before-and-after studies24–28,30,38 we collected the impact factors mainly from the result and discussion sections. We categorized factors into those related to the recipients of care, health systems constraints, and the influence of the social and political context in China.
Recipients of Care
We identified several factors related to how communities, parents, and family members perceive policies and interventions to promote hepatitis B vaccination, including awareness and knowledge about the disease and accessibility of health services and facilities (see Table 4).
TABLE 2 (Continued).
Characteristics of Included Studies Grouped by National Programmes and Provincial Projects
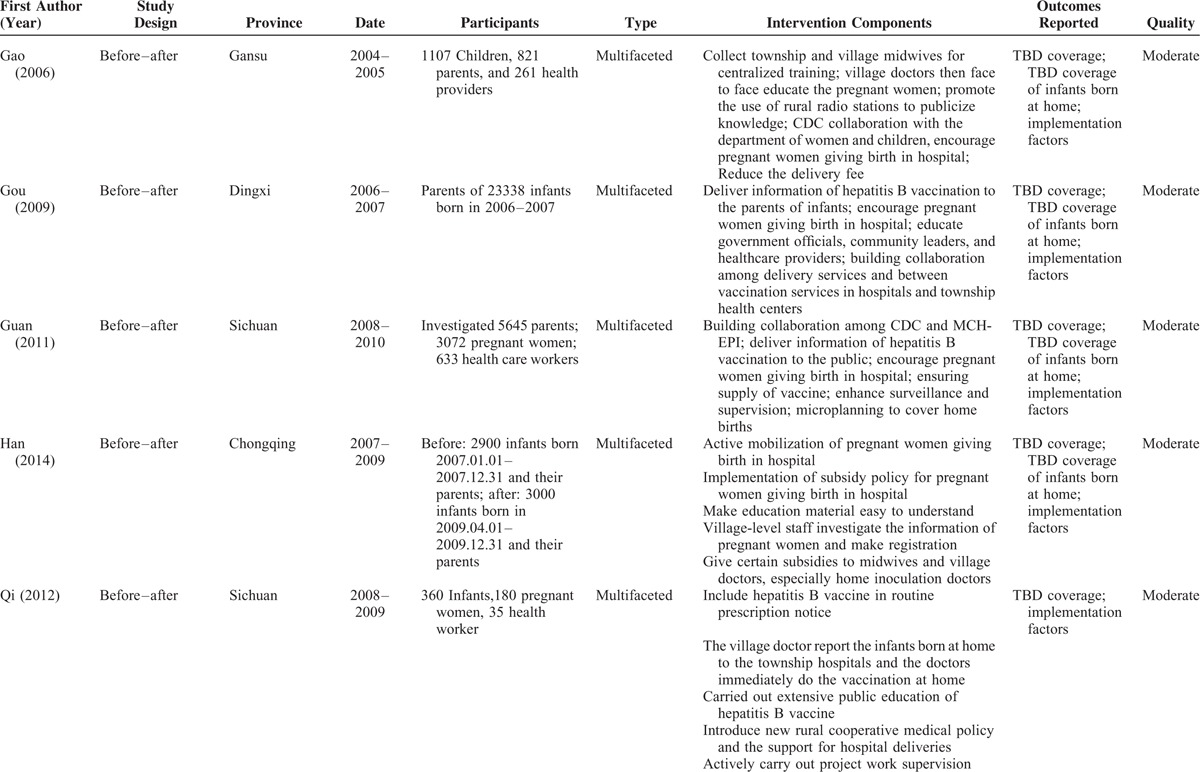
TABLE 4.
Recipients of Care: Factors Affecting the Implementation of Interventions
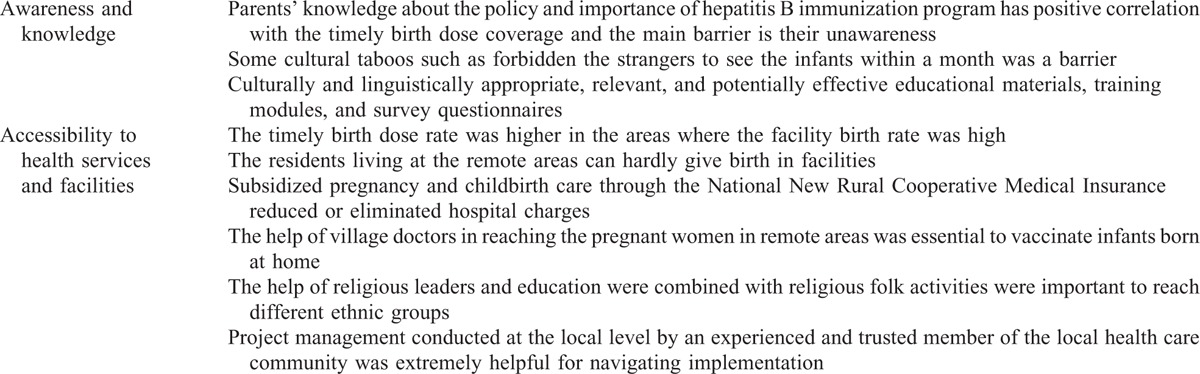
The knowledge of communities, especially parents, about the transmission of hepatitis B virus, the importance of hepatitis B vaccine, immunization procedures, and related supporting policies was an important impact factor to promote the vaccination among the infants. Many studies24–27,30–32,37,38 indicated that besides financial barriers to vaccination, a lack of awareness about hepatitis B and prevention through vaccination was the main barrier to improving coverage. Several papers advocated for community-based information, education, and communication activities to facilitate the implementation of the hepatitis B vaccination in line with the government policy.24,25,27,28,30,32 During community education, some studies emphasized that if the language used was too complex, marginalized populations may be missed so culturally and linguistically appropriate, educational materials, training modules, could help improve the impact of community education.22,31,38
It has been reported that increases in TBD rate of hepatitis B vaccination highly corresponded to increased facility birth rate in China.24–27,31,35 The TBD rate was higher in the areas where the facility birth rate was high. For example, the National Epidemiological Serosurvey of Hepatitis B in 2006 indicated that during 2002 to 2005 in 31 provinces, birth dose coverage rates were highest (84%) among children born in county level hospitals and a lower rate was observed in children who were born in township hospitals (78%) while coverage rates among children born at home were only 31.4%.15 However, it is more difficult for poor families in rural areas to access health facilities for childbirth,31,34 which can influence the coverage of timely first dose of hepatitis B vaccine, and demand for routine childhood vaccinations more generally. To address this, the government initiated subsidized pregnancy and childbirth care through the National New Rural Cooperative Medical Insurance, which reduces or eliminates hospital charges.15,24,28,29 Some studies indicate that the coverage of hepatitis B vaccination increased along with the increase of facility birth rate.
The main barriers for neonatal vaccination were difficulty in access to health care service in rural and remote areas where many pregnant women gave birth at home. As a result, to ensure vaccination coverage rate of infants born at home, the health care providers also used out-reach programs to vaccinate neonates at home, in which the village doctors played an important role in reaching the pregnant women in remote areas and help vaccinating infants born at home in time.15,27,28,30,32,34–37 But some studies also highlighted the influence of customs and cultural taboos on parents’ acceptance of the vaccine for their newborns.26,27,30,36 For example, in some areas inhabited by minority ethnic groups (e.g., Zang or Yi), “strangers,” which were people outside of the immediate family were forbidden to see newborn infants within a month; this impacts on community health workers’ ability to conduct home visits for timely vaccination of infants.26 In 1 study conducted in Chengkou County, a remote area in Chongqing City, the long-lasting preference for sons persists made women inferior in social position and pregnant women could rarely get support from their families to give birth in a facility, which limits the opportunity for infants born in this area to receive a timely first dose of hepatitis B vaccine.27 As a result, in some minority areas, the education to the community and the outreach programs were based on the motivation of religious leaders in order to reach different ethnic groups, and education was commonly combined with religious folk activities.28,38 Chen et al22 reported that project management conducted at the local level by an experienced and trusted member of the local health care community was extremely helpful for the implementation of the interventions in Haimen City and its villages.
Health System Constraints
We identified several aspects of the health system that constrain the implementation of strategies to increase hepatitis B vaccination coverage in China. We found factors relating to supply and procurement of vaccines, knowledge and motivations of health care workers, monitoring and supervision of programmes, and effective management and cooperation seemed to increase vaccine coverage (see Table 5).
TABLE 2 (Continued).
Characteristics of Included Studies Grouped by National Programmes and Provincial Projects
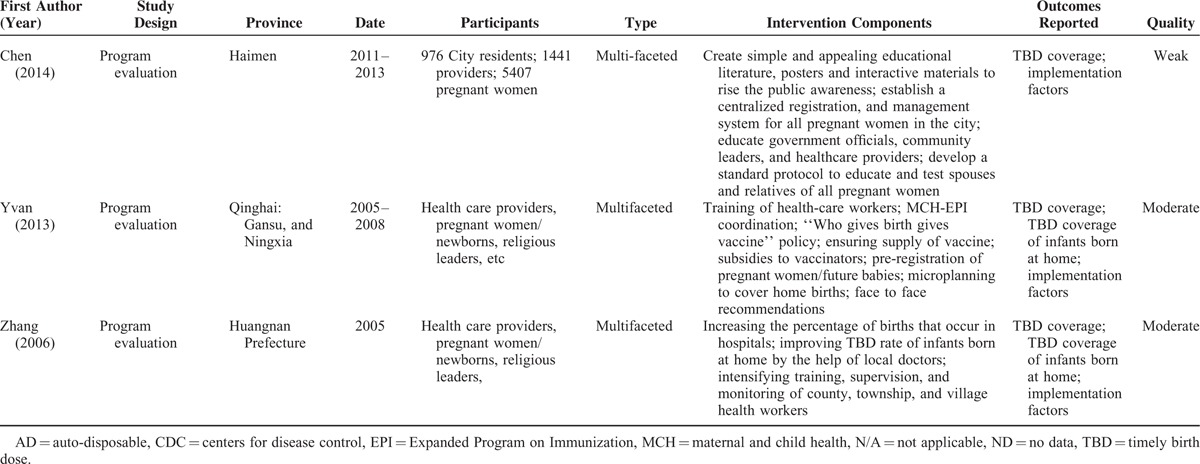
TABLE 5.
Health System Factors Affecting the Implementation of Interventions
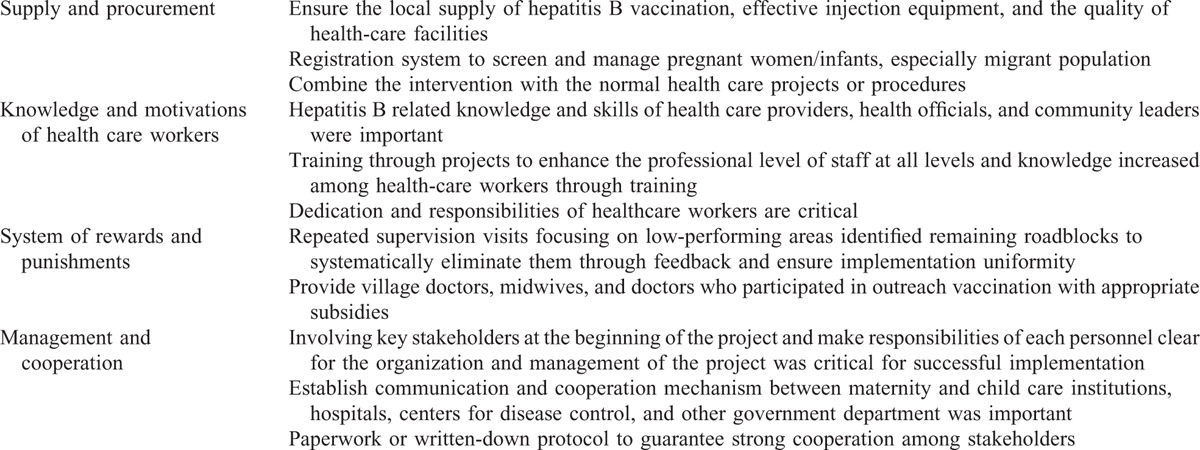
The regular supply of essential vaccine and injection equipment was highlighted in many papers as important for the implementation of hepatitis B vaccination.15,23,26,29,31–35,37 The quality and the price of the vaccine both impact on availability. The evaluation of the GAVI China project showed that domestic procurement of hepatitis B vaccine and AD syringes, which stimulated national vaccine production and ensured a continuous supply and low prices, was central to programme sustainability.29 In some rural areas, poor availability of the vaccine in village clinics was an obstacle to the improvement in coverage rates, especially the TBD at home.31
Combining the intervention with usual health care projects or procedures could help accomplish the program goals. Some studies26,30 indicated that including the vaccination in normal clinical routines can improve the vaccination rate in facilities. Hu et al28 reported the positive impact of combining the promotion of hospital birth with the existing reducing maternal mortality and eliminating neonatal tetanus project. This is especially helpful for governments which aim to introduce a new intervention or project into the areas.
The knowledge and skills of the health care providers can affect the vaccination coverage in facilities. According to Guan et al,26 Qi et al,30 and Wang et al,36 the coverage surveys revealed that because of the lack of knowledge of the vaccine about its indication and contraindication, some health workers were reluctant to give the vaccine birth dose to infants perceived to be sick, weak, or of low birth weight.36 Training to enhance the awareness of staff at all levels could help increase the knowledge among health-care workers and improve the vaccination coverage.25,26,29–32,37 Besides skills and knowledge, Zhou et al33 concluded that dedication of healthcare workers was one of the most critical factors for the achievement China had made in increasing the coverage of hepatitis B vaccination; Han et al27 also described the importance of the motivation of the local vaccinators in the accomplishment of home visits.
A well-defined system of rewards and punishments for performance of health care workers was found to be an essential guarantee of implementation of HBV vaccine. Many studies reported that repeated and regular supervision visits focusing on low-performing areas could identify the remaining roadblocks and systematically eliminate them through feedback so as to ensure implementation.25,28–31,37 In different levels, the frequency and form of supervision could be various. In most cases, the monitoring would follow a top-down procedure in which the upper levels of government health care workers supervise the lower level. The accomplishment of the goals to improve the vaccination coverage would feedback to the upper level and is used as part of assessment of the officials.25,28 Besides, Sun et al35 enhanced the importance of providing village doctors, midwives, and doctors who participated in outreach vaccination with appropriate subsidies. Since the local health care workers mainly work in the low-income areas, economic incentives can greatly improve the motivation of the local doctors in participating in the vaccination programs.23,27,31,35
A communication and cooperation mechanism between maternity and child care institutions, hospitals, centers for disease control (CDC), and other government departments was also important. Some studies indicated that written protocols could encourage better cooperation among project stakeholders.29 Critical to the management of programs and projects to promote hepatitis B vaccination was the involvement of key stakeholders at project inception and being clear about roles and responsibilities of cooperating organizations, services, and personnel.14,22,25,28–30,37 The stakeholder in management could help push the process of the intervention implementation and gain success in reaching out to the targeted population. Maintained communication with the government and public health officials could also facilitate policy changes based on current and forthcoming project data.22 Kane et al14 also noted that the success of GAVI China project was because of the close work between China Expanded Program on Immunization and the vast network of CDC staff at different levels.
Social and Political Context
We identified several factors related to the health system, including political commitment, social context and international cooperation, that influenced hepatitis B vaccination coverage in China (see Table 6).
TABLE 3.
Impact of Strategies or Interventions on Vaccination Coverage Rates
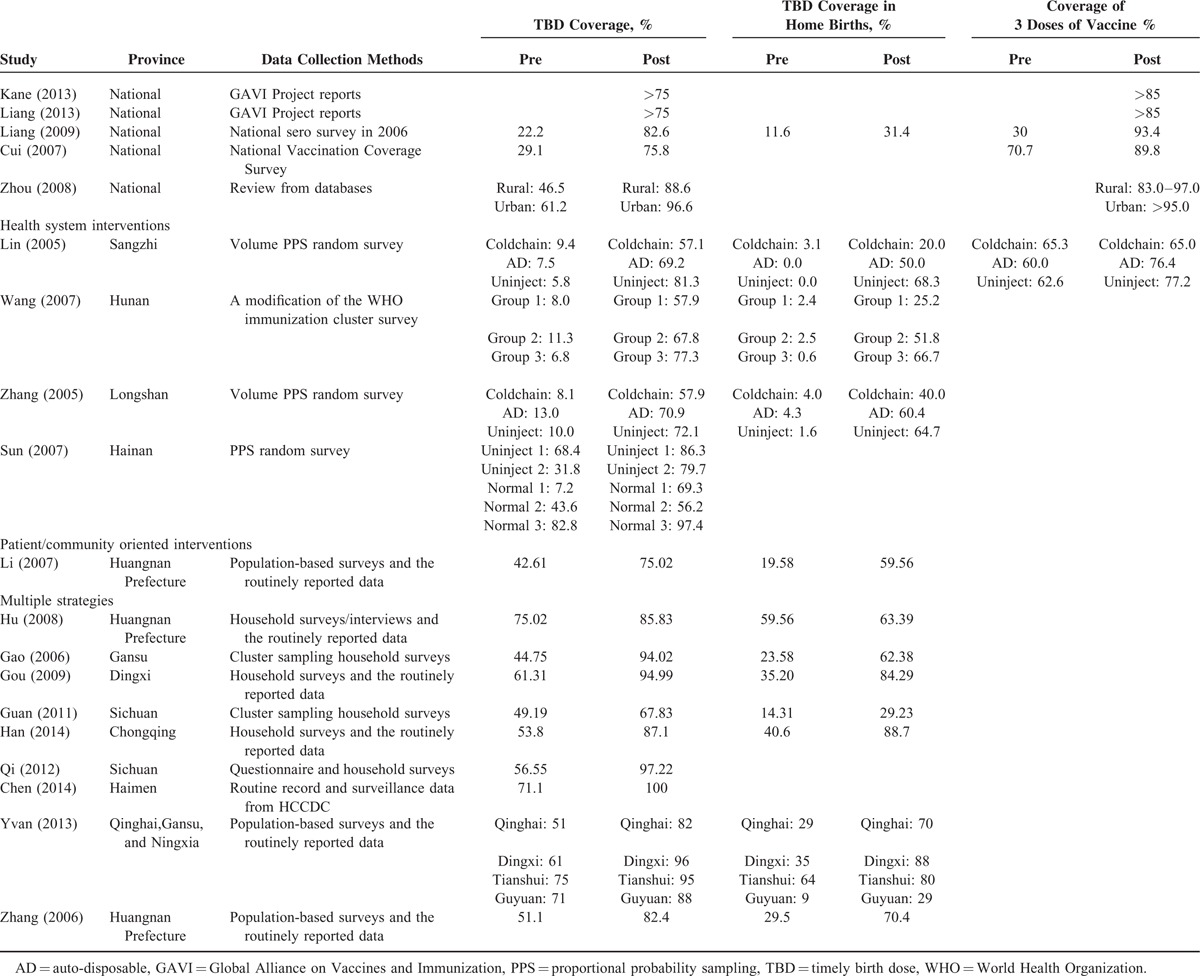
TABLE 6.
Social and Political Factors Affecting the Implementation of Interventions
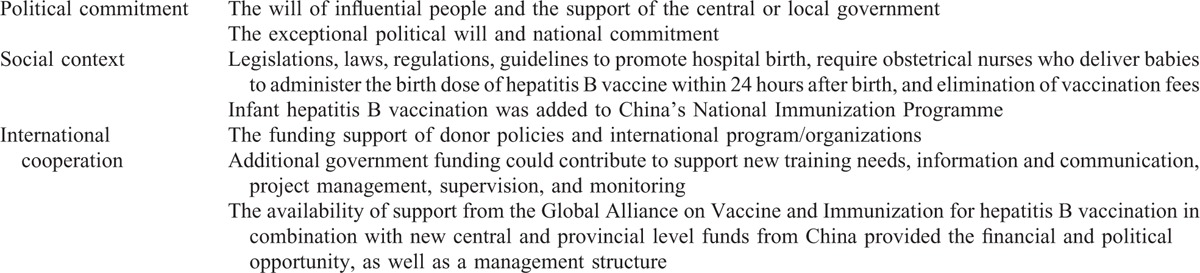
The influence of the central government and exceptional political will that lead to national commitment was the key to the success of universal vaccination in China.14,22,29,31,33 In 1992, the former MoH of China decided to use hepatitis B vaccine routinely for neonates as a part of China's Planned Vaccination Program and issued the Implementation Plan of the National Hepatitis B Vaccination which standardized the implementation of hepatitis B vaccination.33 In 2001, the State Council had approved a statement from the MoH and the Ministry of Finance that hepatitis B vaccine was to be integrated into routine Expanded Program on Immunization throughout the China; this was a milestone for the improvement of universal hepatitis B vaccination rate. Without the influential group of forward thinking leaders from both the China CDC and the MoH advocating the process, however, the hepatitis B would not have been included into the immunization programs in China so readily.29 The success of GAVI China can also be attributed in part to national government commitment and the support of the central and local government departments.14
Some studies also mentioned the importance of policies and laws in providing standardized services.14,15,23,29,31,33 The China government enacted a series of legislations, laws, regulations, and guidelines to promote hospital birth, to require obstetric nurses to administer the birth dose of hepatitis B vaccine within 24 hours after birth, and to eliminate vaccination fees. Both the National Plan of Prevention of Hepatitis B from 2006 to 2010 and the Expanded National Immunization Program Management Plan recommended timely first dose within 24 hours of birth. Those legislations and laws became not only the guideline for the health workers to implement the interventions, but also the legal ground that the end users could rely on for demanding health care information, service, and economic support. These policies greatly helped improve the accessibility to health service and the quality of health care.
Another important factor that facilitated the implementation of hepatitis B vaccination was additional government funding combined with financial support from donors and international program/organizations.14,22,23,29 In 2002, hepatitis B vaccination of infants was fully integrated into the routine immunization programme and the Government of China partnered with the GAVI to provide free vaccine to western and poor areas while provincial financial departments also provided necessary funding to cap user fees to ensure affordability. GAVI offered $76 million budget with an equal amount of Chinese Government to cover the cost of AD syringes and vaccine in remote areas in China.14 That funding support helped the inception and spread of the vaccination at the beginning and the realization of eliminate the vaccination and administration cost. Meanwhile, the sustainability of the project also relied on the ongoing financial input of the government in different levels, which contributed in the ability of Chinese government to take over the responsibility from the international organizations. By 2005, the State Council promulgated the regulations on the administration of vaccine circulation and implementation which stated that the vaccine should be provided completely free of charge nationally. The government additional funding contributed to support new training needs, information and communication, project management, supervision, and monitoring. It also covered the subsidies for local health care workers and greatly enhanced the enthusiasm of grass-roots health care workers. What is more, the availability of support from GAVI for hepatitis B vaccination in combination with new central and provincial government level funds from China provided not only the financial and political opportunity but also a management structure.14
DISCUSSION AND CONCLUSION
This review systematically collected and assessed effects of interventions on improving infants’ uptake of hepatitis B vaccination, and focused on summarizing the factors that influenced implementation of the interventions. Overall, we found that although there are many studies assessing the effect of hepatitis B vaccination, number of original studies exploring the reasons for success are limited.
The study designs used to evaluate impact of different interventions to improve coverage of hepatitis B vaccination varied, so meta-analysis was not feasible for the synthesis of the evidence. The interventions used in the included studies were categorized into health system-oriented, provider-oriented, and patients/community-oriented level. All the included studies reported that interventions increased the coverage of hepatitis B vaccination of newborns, especially the birth dose of hepatitis B vaccination which is the most important dose for preventing mother to child transmission of HBV infection. Although studies generally showed that vaccination coverage in the subgroup of infants born at home increased to a greater extent than in the whole population, which indicates that the outreach intervention has bigger influence on the disadvantaged groups.
We found evidence from the included studies that community education was the most frequently used intervention. All studies indicated the importance of increasing the awareness of the public, especially pregnant and women of reproductive age, and their families. Since hospital birth was the most essential factor which determined the coverage of the vaccination in the whole population, public education about knowledge of HBV or hepatitis B vaccination was usually combined with the promotion of hospital birth in rural areas. It also showed evidence from the included studies that it was more effective to put the relevant interventions together with the current maternal health promotion programs.
To improve the accessibility to the health care service, the former MoH issued a circular on further strengthening facility birth services in rural areas which aimed at improving facility birth rate in rural areas and TBDs of hepatitis B vaccination in 2009. Meanwhile, some studies would use out-reach programs to cover the home-birth infants. Out-of-cold chain strategy was more effective in increase the coverage of vaccination in the remote area where the facility birth rate was respectively low. In this kind of programs, the help of local health workers and religious leaders were the most important facilitators in the implementation. In China, hepatitis B vaccination services are usually provided by community-based health workers in both rural and urban areas. So strengthening of the knowledge and skills training, and setting up appropriate accountability and necessary incentives and/or punishments mechanisms can promote the dedication and ensure the active participation of community-based health workers.
Besides all the interventions or vaccination campaigns, the essential impact factors were political and social factors and the system reinforcement. The strong government commitment and the cooperation of the different government departments were the basic of the policy making and the smooth implementation of the programs. So, it was important to involve the key stakeholders in making the legislation and guidelines.
POTENTIAL LIMITATIONS OF THE REVIEW
None of the included studies were strict double-blind randomized trial considering the ethnic principle because there had been enough evidence on the effectiveness of infant immunization. Since all the programs used more than 1 intervention and were influenced by factors in different levels, it is difficult to access which interventions worked best and which were the most effective. It was also difficult to tell which factors played the most important role in the implementation of the program. In other systematic reviews which tried to summarize the effectiveness of health promotion interventions, the same kind of problems also occurred.39 It was believed that no single magic bullet intervention exists and significant changes were made because of all interventional programs were integrated in nature.
We did not locate any qualitative research reporting in detail why different interventions might or might not have improved the coverage of the hepatitis B vaccination. Although we tried to find some description in the result or discussion part of the included studies, few studies mentioned the detailed implementation process and the obstacles or facilitators during the process.
IMPLICATIONS FOR POLICY AND FUTURE RESEARCH
The most important lesson from China's experience in increasing TBD of the hepatitis B vaccine is the integration of hepatitis B vaccine into the national planning and the strong implementation ability, which relies on the top-down health system. Strategies included establishing maternal registration system, especially strengthening tracking of migrant population, out-reach interview in remote areas, mobilization of facility birth, and facility birth incentives for poor areas. This could be an important component of vaccination programmes in low and middle income countries, integrating important and urgent health measures into the government agenda can facilitate large-scale interventions.
Necessary policy and regulation with additional government funding could contribute to support procurement of the vaccine, and ensuring equipment and subsidies to grass-root health care workers. This strategy is essential to improve vaccination coverage among the poor, especially the migrant population. Meanwhile, free services are an important measure to address the accessibility of hepatitis B vaccination and can enhance the health care receivers’ approval and acceptance, which helps achieve the policy goals.
Appropriate service delivery is the key to China's hepatitis B vaccination. Raising facility birth rate was one of the key measures for the improvement of vaccination coverage. In remote areas, however, where faced with difficulties in facility birth, the door-to-door vaccination service became an effective support measure. Invest in out-of-cold chain storage and transportation equipment should also be taken into consideration. Better health information systems can be managed by village doctors so that vaccine can be delivered at home to increase the TBD rate of infants born at home. The economic conditions and health infrastructure varies largely in low and middle income countries, so services should be adapted to local contexts. Also, with challenges of health human resource in developing countries, government should focus more on the promotion of grass-roots health human resource capacity and enthusiasm.
Supplementary Material
Acknowledgments
The authors thank China-UK Global Health Support Programme (Grant No. GHSP-CS-OP1–02) for the support. The authors also thank the help and comments from Professor Mary Story from Community and Family Medicine and Global Health, Duke Global Health institute, Duke University.
Footnotes
Abbreviations: AD = auto-disposable, CDC = centers for disease control, GAVI = Global Alliance on Vaccine and Immunization, HBV = hepatitis B virus, MoH = Ministry of Health, TBD = timely birth dose, WHO = World Health Organization.
This study was supported by the China-UK Global Health Support Programme (Grant No. GHSP-CS-OP1-02).
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
REFERENCES
- 1.World Health Organization. Improving the Health of Patients with Viral Hepatitis: Report by the Secretariat. SIXTY-SEVENTH WORLD HEALTH ASSEMBLY. http://apps.who.int/gb/e/e_wha67.html Published 28 March 2014. [Google Scholar]
- 2.WHO. World Health Organization Media Centre. Hepatitis B.2014; http://www.who.int/mediacentre/factsheets/fs204/en/#. Updated July 2014. [Google Scholar]
- 3.Li J, Zhuang H. Progress in epidemiology of viral hepatitis. Chin Hepatol 2012; 2–5. [Google Scholar]
- 4.National Health and Family Planning Commission of the PRC. Chinese Health Statistics Yearbook 2013(Chinese).2014; http://www.nhfpc.gov.cn/htmlfiles/zwgkzt/ptjnj/year2013/index2013.html Updated April 2014. [Google Scholar]
- 5.Franco E, Hepatitis B. Epidemiology and prevention in developing countries. World J Hepatol 2012; 4:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO. WHO Position Paper On Hepatitis B Vaccines. Weekly epidemiological record.2009; 84, 405-420. http://www.who.int/wer/2009/wer8440.pdf?ua=1. [Google Scholar]
- 7.WHO. Global Immunization Data.2014; http://apps.who.int/immunization_monitoring/Global_Immunization_Data_v2.pdf?ua=1 Updated July 2014. [Google Scholar]
- 8.WHO and UNICEF. Estimates of National Immunization Coverage: China 2014 revision. http://apps.who.int/immunization_monitoring/globalsummary/wucoveragecountrylist.html#C. Data as of July 7, 2015. [Google Scholar]
- 9.Zhang C, Zhong Y, Guo L. Strategies to prevent hepatitis B virus infection in China: Immunization, screening, and standard medical practices. Biosci Trends 2013; 7:7–12. [PubMed] [Google Scholar]
- 10.Cui FQ, Wang XJ, Cao L, et al. Progress in hepatitis B prevention through universal infant vaccination—China, 1997–2006. JAMA 2007; 298:506. [Google Scholar]
- 11.Progress in preventing hepatitis B through universal infant vaccination: China, 1997–2006. Wkly Epidemiol Rec 2007; 82:209–216. [PubMed] [Google Scholar]
- 12.Cui F, Luo H, Wang F, et al. Evaluation of policies and practices to prevent mother to child transmission of hepatitis B virus in China: results from China GAVI project final evaluation. Vaccine 2013; (31 Suppl 9):J36–J42. [DOI] [PubMed] [Google Scholar]
- 13.Jia J. Hepatitis B in China: from guideline to practice. Virol Sin 2008; 23:152–155. [Google Scholar]
- 14.Kane MA, Hadler SC, Lee L, et al. The inception, achievements, and implications of the China GAVI Alliance Project on Hepatitis B Immunization. Vaccine 2013; (31 Suppl 9):J15–J20. [DOI] [PubMed] [Google Scholar]
- 15.Liang X, Bi S, Yang W, et al. Evaluation of the impact of hepatitis B vaccination among children born during 1992–2005 in China. J Infect Dis 2009; 200:39–47. [DOI] [PubMed] [Google Scholar]
- 16.H T. Quality Assessment Tool for Quantitative Studies 2010; http://www.ephpp.ca/PDF/Quality%20Assessment%20Tool_2010_2.pdf. [Google Scholar]
- 17.H T. Quality Assessment Tool for Quantitative Studies Dictionary 2009; Toronto: McMaster University. http://www.ephpp.ca/PDF/QADictionary_dec2009.pdf. [Google Scholar]
- 18.Armijo-Olivo S, Stiles CR, Hagen NA, et al. Assessment of study quality for systematic reviews: a comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: methodological research. J Eval Clin Pract 2012; 18:12–18. [DOI] [PubMed] [Google Scholar]
- 19.Machingaidze S, Rehfuess E, von Kries R, et al. Understanding interventions for improving routine immunization coverage in children in low- and middle-income countries. Syst Rev 2013; 2:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The SURE Collaboration. SURE Guides for Preparing and Using Evidence-Based Policy Briefs: 5. Identifying and Addressing Barriers to Implementing Policy Options. Version 2.1.2011; http://global.evipnet.org/SURE-Guides/. [Google Scholar]
- 21.Smith HJ, Colvin CJ, Richards E, et al. Programmes for advance distribution of misoprostol to prevent post-partum haemorrhage: a rapid literature review of factors affecting implementation. Health Policy Plan 2016; 31:102–113. [DOI] [PubMed] [Google Scholar]
- 22.Chen G, Block JM, Evans AA, et al. Gateway to care campaign: a public health initiative to reduce the burden of hepatitis B in Haimen City, China. BMC Public Health 2014; 14:754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cui F, Wang X, Cao L, et al. Progress in hepatitis B prevention through universal infant vaccination – China, 1997–2006. MMWR Morb Mortal Wkly Rep 2007; 56:441–445. [PubMed] [Google Scholar]
- 24.Gao L, Li H, Meng L, et al. Analysis on intervention effect of the first dose coverage rate timely for hepatitis B vaccine in rural areas in Gansu province (Chinese). Chin J Public Health 2006; 22:1255–1256. [Google Scholar]
- 25.Gou Q, Qi K. Study on the executive strategy of the pilot project of improving the first dose coverage rate timely for hepatitis B vaccine in poor areas (Chinese). Chin Primary Health Care 2009; 23:51–53. [Google Scholar]
- 26.Guan X, Qi Q, Yang C, et al. Analysis of the project effect on MOH/GAVI increasing the coverage rate of timely—birth dose hepatitis B vaccine in the remote minority areas in Sichuan Province (Chinese). Chin J Vaccines Immun 2011; 540–544. [Google Scholar]
- 27.Han Z, Wang Q, Wang Y, et al. Study on the collaborated project of strategies to improve the vaccination coverage rate of timely first dose of hepatitis B vaccine of newborns in remote poverty mountain areas (Chinese). Modern Prev Med 2014; 2022–2024. [Google Scholar]
- 28.Hu Y, Zhang Y, Wan M, et al. Evaluation of sustainability of the project of improving timely birth dose of hepatitis B vaccine in Tibetan autonomous prefecture of Huangnan (Chinese). Chin J Vaccines Immun 2008; 14:147–149. [Google Scholar]
- 29.Liang X, Cui F, Hadler S, et al. Origins, design and implementation of the China GAVI project. Vaccine 2013; 31 Suppl 9:J8–J14. [DOI] [PubMed] [Google Scholar]
- 30.Qi Q, Qing-lian L, Yun-xia C, et al. Intervention on first dose injection of hepatitis B vaccine in rural areas and remote mountainous areas of Sichuan Province (Chinese). J Occup Health Damage 2012; 27:216–219. [Google Scholar]
- 31.Yvan H, Hennessey K, Cairns L, et al. Improving hepatitis B vaccine timely birth dose coverage: lessons from five demonstration projects in China, 2005–2009. Vaccine 2013; 319:J49–J55. [DOI] [PubMed] [Google Scholar]
- 32.Zhang Y, Zhang X, Hu Y, et al. Report of the Project to Improve First Dose Coverage of Hepatitis B Vaccine in Huangnan Prefecture, Qinghai Province (Chinese). Paper presented at: National Hepatitis Vaccine Research and Experience Changing Conference; November 1, 2006; Chengdu: 155-161. [Google Scholar]
- 33.Zhou YH, Wu C, Zhuang H. Vaccination against hepatitis B: the Chinese experience. Chin Med J (Engl) 2009; 122:98–102. [PubMed] [Google Scholar]
- 34.Lin Q, Wang Z, Chen C, et al. Study on strategy of enhancing the vaccination coverage rate of timely first dose of hepatitis B vaccine in Zhangjiajie City (Chinese). Pract Prev Med 2005; 12:540–542. [Google Scholar]
- 35.Sun L, Zeng Z, Fu Z, et al. Study on results of immunization service model of improving the timeliness coverage of the first dose of hepatitis B vaccine among newborns in the poor area (Chinese). China Trop Med 2007; 7:1740–1742. [Google Scholar]
- 36.Wang LX, Li JH, Chen HP, et al. Hepatitis B vaccination of newborn infants in rural China: evaluation of a village-based, out-of-cold-chain delivery strategy. B World Health Organ 2007; 85:688–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang J, Zou G, Dong J, et al. Research on strategy of improving the first hepatitis B vaccine inoculation rate of children living in village regions in Longshan County (Chinese). Chin J Vaccines Immun 2005; 11:96–99. [Google Scholar]
- 38.Li X, Wan M, Li Q, et al. Analysis on health education on improving the timely-birth dose coverage of hepatitis B in rural and pasturing areas in Qinghai Province (Chinese). Chin J Vaccines Immun 2007; 43–45. [Google Scholar]
- 39.Nyamtema AS, Urassa DP, van Roosmalen J. Maternal health interventions in resource limited countries: a systematic review of packages, impacts and factors for change. BMC Pregnancy Childbirth 2011; 11:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


