Abstract
Background
US guidelines now recommend that all HIV-infected persons receive antiretroviral therapy). HIV prevention is increasingly focused on ensuring that infected persons are diagnosed soon after HIV acquisition and quickly link to care and initiate antiretroviral therapy. We examined trends in time from HIV diagnosis to viral load suppression in King County, WA, to gauge improvement in our HIV care continuum over time.
Methods
We used HIV surveillance data and Cox proportional hazards to evaluate how the time from diagnosis to viral suppression changed among persons newly diagnosed as having HIV in King County, WA, between 2007 and 2013.
Results
A total of 1490 (84%) of 1766 newly diagnosed persons achieved viral suppression in a median time of 213 days (95% confidence interval, 203–229). Thirty-six percent of all persons diagnosed in 2007 and 77% in 2013 were virally suppressed within 12 months of HIV diagnosis (P < 0.0001). Differences in time to suppression by calendar year persisted when stratifying by CD4 count at diagnosis. Race was not significantly associated with time to viral suppression.
Conclusions
Time from HIV diagnosis to viral suppression dramatically declined between 2007 and 2013, and more than three quarters of recently HIV-diagnosed individuals in King County, WA, now achieve viral suppression within a year of diagnosis. This improvement was evident among all persons newly diagnosed as having HIV, regardless of race/ethnicity or CD4 count at time of diagnosis.
In 2012, US Health Resources and Service Administration recommended that all persons with human immunodeficiency virus (HIV) infection receive antiretroviral treatment (ART), regardless of their CD4 lymphocyte count (Table 1).5 That change in treatment guidelines was adopted in the face of new evidence that early ART improves patients’ health and has the potential to diminish HIV transmission.6,7 The emphasis on early treatment codified in the guidelines is also evident in the US National HIV/AIDS Strategy, and the more recent HIV Care Continuum Initiative.8 All of these documents focus on the HIV care continuum—the sequential steps from HIV diagnosis, to linkage and retention in care, ART initiation, and viral suppression9–12—and all emphasize the importance of identifying persons with HIV infection shortly after HIV acquisition and rapidly achieving the goal of viral suppression.
TABLE 1.
| 2006 | After CD4 count <350/mm3 and before 200/mm3 |
| 2008 | Before CD4 count <350/mm3 with individualized initiation decisions >350/mm3 |
| 2009 | CD4 count ≤500/mm3 |
| 2012 | ART to all patients regardless of CD4 count |
We previously published data on the HIV care continuum in King County, WA, demonstrating that 67% to 75% of all diagnosed persons with HIV infection are virally suppressed.13,14 This cross-sectional evaluation is a measure of the success of the HIV prevention and care system in King County, but provides relatively little insight into the system’s success in meeting the needs of persons with recently diagnosed HIV infection, and accelerating progress along the HIV care continuum. Here we present data on trends in the time from diagnosis to viral suppression among persons diagnosed as having HIV infection in King County, WA, from 2007 to 2013, demonstrating that our local care system has rapidly responded to new scientific evidence, treatment guidelines, and public health initiatives that emphasize early linkage to care and initiation of ART.
MATERIALS AND METHODS
We examined the time from HIV diagnosis to viral suppression among persons diagnosed as having HIV infection in King County, WA, from 2007 to 2013. The work was conducted at the Public Health–Seattle & King County HIV/AIDS Epidemiology section and included the period after all CD4 and viral loads became legally reportable (mid-2006). Participants included all HIV-infected individuals older than 14 years diagnosed between 2007 and 2013 who resided in King County at the time of diagnosis and were reported to Public Health–Seattle & King County as of June 4, 2015. Individuals known to be enrolled in research studies were not included in this analysis because WA State law excludes research studies from HIV laboratory reporting requirements. Study status is ascertained through provider and patient contact either during surveillance and partner services investigations undertaken when cases are first reported or, if the individual has not had a laboratory in a 12-month period, through an investigation undertaken of persons thought to be out of care. Public Health does not collect data on the period of study involvement, so we excluded individuals enrolled in a study at any point.
This study is a secondary data analysis of data collected through public health HIV surveillance, including HIV Incidence and Core HIV Surveillance data sources. HIV Incidence and Core HIV Surveillance comprise the Washington State HIV data system called eHARS. HIV Incidence collects testing data, whereas Core contains demographic and transmission characteristics and laboratory tests. Both sources contain data from medical record abstractions, provider reports, and patient interviews. HIV core surveillance and partner services investigations are substantially integrated in King County, and Public Health attempts to interview all persons with newly diagnosed HIV infection. We defined first HIV diagnosis as the earliest positive HIV diagnostic test result or date of self-reported HIV diagnosis. In the event that these differed by more than 40 days, Public Health staff investigated cases to establish which date was likely to be the more accurate. The date of initial viral suppression was defined as the date of first reported plasma quantitative real-time HIV-1 RNA polymerase chain reaction test result showing an HIV viral load of 200 copies/mL or less. This assay is consistently used for viral load quantification in King County. The following variables were assessed for associations with time to viral suppression: age group at time of diagnosis (15–24, 25–34, 35–44, 45–54, 55+ years), sex, race/ethnicity (non-Hispanic white, foreign-born black, non-Hispanic US born black, Hispanic, and other), HIV exposure category (men who have sex with men [MSM], injection drug user [IDU], MSM-IDU, unknown exposure, or heterosexual exposure as indicated by the National HIV Surveillance System), CD4 lymphocyte count within the first 6 months of diagnosis (defined in groups <350, 350–500, >500 per mm3), and year of diagnosis (2007 through 2013). CD4 counts more than 6 months after diagnosis were changed to missing due to concern that such values might not be representative of CD4 counts at time of diagnosis.
We calculated estimates of time taken for 50% and 75% of the population to reach viral suppression and created Kaplan-Meier survival plots to visually present time from HIV diagnosis to viral suppression. Individuals contributed time from their date of HIV diagnosis to the date of initial viral suppression (event). Persons with no laboratory results demonstrating HIV viral suppression who were not known to have left the area or died were censored on the date the analytic dataset was created (June 5, 2015). Persons who died were censored on the date of their death. Patient deaths are updated in eHARS from the Washington state and King County death certificates, the National Death Index, and the Social Security Death Master File. Persons who migrated out of WA State were censored on the date of their last laboratory test result reported to Public Heath HIV surveillance. We have previously reported our procedures for identifying persons who migrate out of the area.15 We used log rank testing and Cox proportional hazard regression to evaluate the association of independent variables with time to viral suppression. We decide a priori to include age, sex, exposure category, race/ethnicity, CD4 count at diagnosis, and year of diagnosis in the multivariable model of the association of independent variables with time to viral suppression. To address the lack of laboratory completeness validation 2007–2009, we repeated analysis for the 3 years with greater than 90% laboratory completeness (2011–2013). We also conducted a secondary multivariable analysis excluding elite controllers (viral loads <50 copies/mL) to examine whether they were skewing results. People missing a CD4 count or with CD4 counts more than 6 month after diagnosis were removed from multivariable models. A secondary multivariable analysis and Kaplan-Meier plots were done for those without CD4 counts within 6 months of diagnosis and for alternative groupings of CD4 counts (0–200, 200–350, 350, 500, >500 per mm3).
RESULTS
Between 2007 and 2013, 1841 persons were newly diagnosed as having HIV infection in King County, WA. We excluded 56 persons who were enrolled in research studies and 19 persons younger than 14 years from further analysis, leaving a study population of 1766 persons (96% of persons newly diagnosed as having HIV during the study period). A total of 140 (8%) people did not have a CD4 lymphocyte count reported to Public Health in the first 6 months after HIV diagnoses; these persons were excluded from analyses that included CD4 count as an independent variable.
The population was predominantly non-Hispanic white (59%), 25 to 44 years of age (59%), and composed of MSM (76% including 8% MSM-IDU; Table 2). Of those with CD4 lymphocyte counts done within 6 months of diagnosis, 45% had less than 350 cells/mm3. Although some demographic, clinical, and risk characteristics varied year-to-year, we did not observe significant changes in trends of the characteristics of the newly HIV-diagnosed population.
TABLE 2.
Demographic and Transmission Characteristics Among Those Newly Diagnosed With HIV in King County, WA (2007–2013)
| No. (%)
|
Total No. (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | ||
| Risk | ||||||||
| MSM | 181 (64.9) | 172 (62.6) | 170 (68.3) | 205 (73.0) | 156 (69.6) | 156 (63.9) | 147 (68.7) | 1187 (67.2) |
| MSM/IDU | 27 (9.7) | 16 (5.8) | 19 (7.6) | 20 (7.1) | 26 (11.6) | 24 (9.8) | 17 (7.9) | 149 (8.4) |
| IDU | 7 (2.5) | 8 (2.9) | 11 (4.4) | 12 (4.3) | 8 (3.6) | 10 (4.1) | 4 (1.9) | 60 (3.4) |
| Heterosexual | 30 (10.8) | 35 (12.7) | 21 (8.4) | 23 (8.2) | 9 (4.0) | 16 (6.6) | 15 (7.0) | 149 (8.4) |
| Unknown | 34 (12.2) | 44 (16.0) | 28 (11.2) | 21 (7.5) | 25 (11.2) | 38 (15.6) | 31 (14.5) | 221 (12.5) |
| Race/ethnicity | ||||||||
| Foreign-born black | 22 (7.9) | 26 (9.5) | 14 (5.6) | 7 (2.5) | 16 (7.1) | 18 (7.4) | 17 (7.9) | 120 (6.8) |
| US-born black | 32 (11.5) | 28 (10.2) | 25 (10.0) | 19 (6.8) | 24 (10.7) | 25 (10.3) | 22 (10.3) | 175 (9.9) |
| Non-Hispanic white | 157 (56.3) | 150 (54.6) | 152 (61.0) | 181 (64.4) | 135 (60.3) | 147 (60.3) | 116 (54.2) | 1038 (58.8) |
| Hispanic | 47 (16.9) | 40 (14.6) | 40 (16.1) | 46 (16.4) | 34 (15.2) | 28 (11.5) | 35 (16.4) | 270 (15.3) |
| Other | 21 (7.5) | 31 (11.3) | 18 (7.2) | 28 (10.0) | 15 (6.7) | 26 (10.7) | 24 (11.2) | 163 (9.2) |
| Age at diagnosis, y | ||||||||
| 15–24 | 41 (14.7) | 42 (15.3) | 36 (14.5) | 44 (15.7) | 38 (17.0) | 34 (13.9) | 31 (14.5) | 266 (15.1) |
| 25–34 | 81 (29.0) | 88 (32.0) | 78 (31.3) | 94 (33.5) | 70 (31.2) | 86 (35.3) | 65 (30.4) | 562 (31.8) |
| 35–44 | 81 (29.0) | 75 (27.3) | 64 (25.7) | 76 (27.1) | 53 (23.7) | 69 (28.3) | 63 (29.4) | 481 (27.2) |
| 45–54 | 46 (16.5) | 45 (16.4) | 52 (20.9) | 53 (18.9) | 40 (17.9) | 38 (15.6) | 41 (19.2) | 315 (17.8) |
| 55+ | 30 (10.6) | 25 (9.1) | 19 (7.6) | 14 (5.0) | 23 (10.3) | 17 (7.0) | 14 (6.5) | 142 (8.0) |
| Sex | ||||||||
| Female | 33 (11.8) | 35 (12.7) | 24 (9.6) | 29 (10.3) | 21 (9.4) | 33 (13.5) | 26 (12.2) | 201 (11.4) |
| Male | 246 (88.2) | 240 (87.3) | 225 (90.4) | 252 (89.7) | 203 (90.6) | 211 (86.5) | 188 (87.9) | 1565 (88.6) |
| CD4, cells/mm3* | ||||||||
| < 350 | 106 (44.7) | 121 (48.8) | 117 (51.5) | 110 (41.4) | 98 (47.6) | 91 (38.1) | 84 (41.4) | 727 (44.7) |
| 350–500 | 50 (21.1) | 54 (21.8) | 37 (16.3) | 61 (22.9) | 53 (25.7) | 60 (25.1) | 49 (24.1) | 364 (22.4) |
| >500 | 81 (34.2) | 73 (29.4) | 73 (32.2) | 95 (35.7) | 55 (26.7) | 88 (36.8) | 70 (34.5) | 535 (32.9) |
| Viral load, copies/mL† | ||||||||
| <50 | 4 (1.6) | 4 (1.6) | 2 (0.9) | 2 (0.8) | 4 (1.9) | 1 (0.4) | 2 (1.0) | 19 |
| 50–1000 | 23 (9.2) | 19 (7.6) | 22 (9.6) | 17 (6.4) | 11 (5.3) | 16 (6.8) | 13 (6.4) | 121 |
| >1000 | 224 (89.2) | 228 (90.8) | 205 (89.5) | 247 (92.9) | 194 (92.8) | 220 (92.8) | 187 (92.6) | 1505 |
| Total | 279 (100) | 275 (100) | 249 (100) | 281 (100) | 224 (100) | 244 (100) | 214 (100) | 1766 |
CD4 counts done later than 6 months after initial diagnosis have been removed (140 missing).
Viral loads done later than 6 months after initial diagnosis have been removed (121 missing).
The 1766 newly diagnosed persons included in the study population achieved viral suppression or were censored in a median time of 258 days (0–3063 days) with an average of 3 viral loads per year before suppression. Of the 276 (16%) who were censored without achieving viral suppression, 36 (13%) died, 86 (31%) moved out of the state, 56 (20%) were still in care with laboratory results reported to surveillance in the final year of study observation (June 2014 or later), and 98 (36%) had no laboratory test results reported in surveillance in the final year of study observation and were not known to have moved out of state or died. This indicates roughly 9% (154 persons) of our initial population never achieved viral suppression, including those who seemed to be out of care as of June 2015 (i.e., no laboratory results reported in the 12 months before the end of observation).
A total of 1490 (84%) persons achieved viral suppression in a median time of 213 days (95% confidence interval [CI], 203–229) after HIV diagnosis. In 2007, half of newly diagnosed persons had achieved viral suppression by 685 days after diagnosis. In contrast, by 2013, half of all newly diagnosed persons were virally suppressed 142 days after diagnosis. In 2007, 36% of all persons diagnosed were virally suppressed within the first 12 months after HIV diagnosis, whereas in 2013, 77% were suppressed 12 months after HIV diagnosis (P < 0.0001).
Trends in time from HIV diagnosis to viral suppression varied by initial CD4 lymphocyte count, although all groups did see a significant decrease in time to suppression over this period (Fig. 1A–C [also see Figure, Supplemental Digital Content 1, http://links.lww.com/OLQ/A120, trends for those with CD4 count 200–350 cells/mm3]). A similar pattern persisted when looking at those without CD4 counts within 6 months, although significance was lost due to small number size (see Figure, Supplemental Digital Content 2, http://links.lww.com/OLQ/A121, trends for those without CD4 counts). Persons with initial CD4 counts less than 350 cells/mm3 rapidly achieved viral suppression throughout the period of observation (median, 157 days; 95% CI, 151–167). Among persons with CD4 counts greater than 500, the time from diagnosis to when 50% of persons were virally suppressed decreased 87%, from 1112 days in 2007 to 142 days in 2013. This decrease was only slightly smaller (83%) among persons with initial CD4 lymphocyte counts of 350 to 500 cells/mm3 (717 days in 2007 vs. 120 days in 2013).
FIGURE 1.
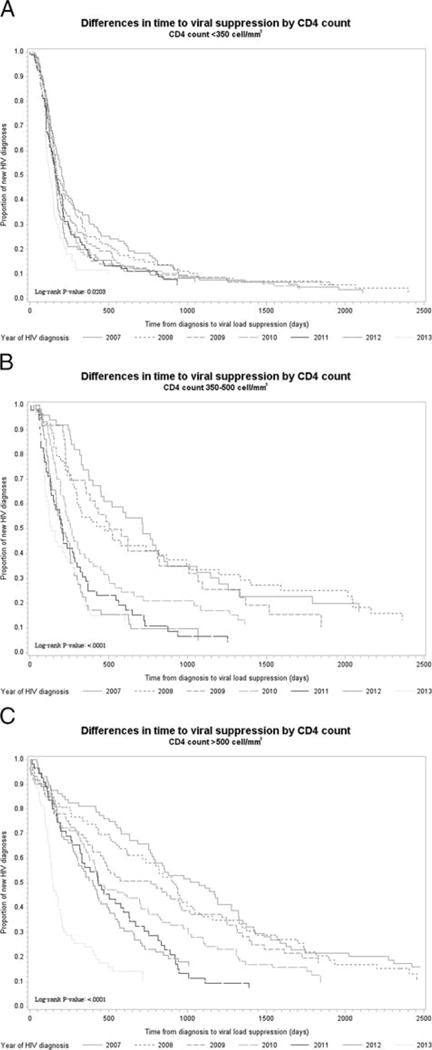
A–C, Kaplan-Meier curves depicting time to viral load suppression by diagnosis year, among those with CD4 counts less than 350 cells/mm3, 350–500 cells/mm3, and greater than 500 cells/mm3 in King County, WA (2007–2013).
On univariate analysis, more rapid viral suppression was significantly associated with unknown HIV risk, IDU, or heterosexual transmission categories, female sex, CD4 lymphocyte count less than 500 cells/mm3, older age, being a foreign-born black, and later year of HIV diagnosis (Table 3 and Fig. 2). On multivariable analysis, lower CD4 count, older age, female sex, and more recent year of diagnosis were all significantly associated with more rapid viral suppression (Table 4 [also see Table, Supplemental Digital Content 3, http://links.lww.com/OLQ/A122, multivariable analysis with alternative CD4 groupings]). Similar associations were seen when restricting the analysis to those without CD4 counts at diagnosis (see Table, Supplemental Digital Content 4, http://links.lww.com/OLQ/A123, multivariate analysis for those without CD4 counts). Multivariable analysis restricted to 2011, 2012, and 2013 showed minimal differences in variables associated with time to viral suppression (see Table, Supplemental Digital Content 5, http://links.lww.com/OLQ/A124, multivariable analysis restricted to 2011–2013). An analysis excluding 19 elite controllers with viral loads less than 50 copies/mL did not significantly change the multivariable adjusted hazard ratio (HRadj) findings (data not shown).
TABLE 3.
Univariate Proportional Cox Analysis of Variables Associated With Viral Suppression After HIV Diagnosis in King County, WA (2007–2013)
| Time for 50% of Persons to Be Suppressed, d | Time for 75% of Persons to Be Suppressed, d | HR | 95% CI | P | |
|---|---|---|---|---|---|
| Race/ethnicity | |||||
| Foreign-born black | 155 | 406 | 1.52 | 1.24–1.86 | <0.0001 |
| US-born black | 322 | 2358 | 0.87 | 0.72–1.04 | 0.13 |
| Hispanic | 269 | 980 | 1.06 | 0.91–1.22 | 0.45 |
| Other | 286 | 842 | 1.15 | 0.97–1.38 | 0.11 |
| Non-Hispanic white | 322 | 1004 | Reference | ||
| CD4, cells/mm3 | |||||
| <350 | 169 | 358 | 2.14 | 1.89–2.42 | <0.0001 |
| 350–500 | 300 | 868 | 1.27 | 1.10–1.47 | <0.01 |
| >500 | 524 | 1350 | Reference | ||
| Sex | |||||
| Female | 176 | 620 | 1.36 | 1.16–1.60 | <0.001 |
| Male | 308 | 1034 | Reference | ||
| Age at diagnosis, y | |||||
| 15–24 | 413 | 1192 | 0.68 | 0.54–0.85 | <0.001 |
| 25–34 | 364 | 1223 | 0.72 | 0.59–0.88 | <0.01 |
| 35–44 | 281 | 995 | 0.84 | 0.69–1.04 | 0.11 |
| 45–54 | 198 | 621 | 0.98 | 0.79–1.21 | 0.82 |
| 55+ | 204 | 855 | Reference | ||
| Risk | |||||
| Unknown | 188 | 980 | 0.94 | 0.75–1.17 | 0.56 |
| IDU | 279 | 962 | 0.75 | 0.54–1.05 | 0.09 |
| MSM | 317 | 952 | 0.72 | 0.60–0.87 | <0.001 |
| MSM/IDU | 610 | — | 0.51 | 0.40–0.66 | <0.0001 |
| Heterosexual | 189 | 482 | Reference | ||
| Year of diagnosis | |||||
| 2007 | 685 | 1502 | 0.37 | 0.31–0.46 | <0.0001 |
| 2008 | 433 | 1739 | 0.42 | 0.34–0.51 | <0.0001 |
| 2009 | 363 | 1325 | 0.47 | 0.38–0.58 | <0.0001 |
| 2010 | 291 | 894 | 0.56 | 0.46–0.68 | <0.0001 |
| 2011 | 230 | 630 | 0.68 | 0.55–0.83 | <0.001 |
| 2012 | 211 | 543 | 0.71 | 0.58–0.87 | <0.001 |
| 2013 | 142 | 327 | Reference |
FIGURES 2.
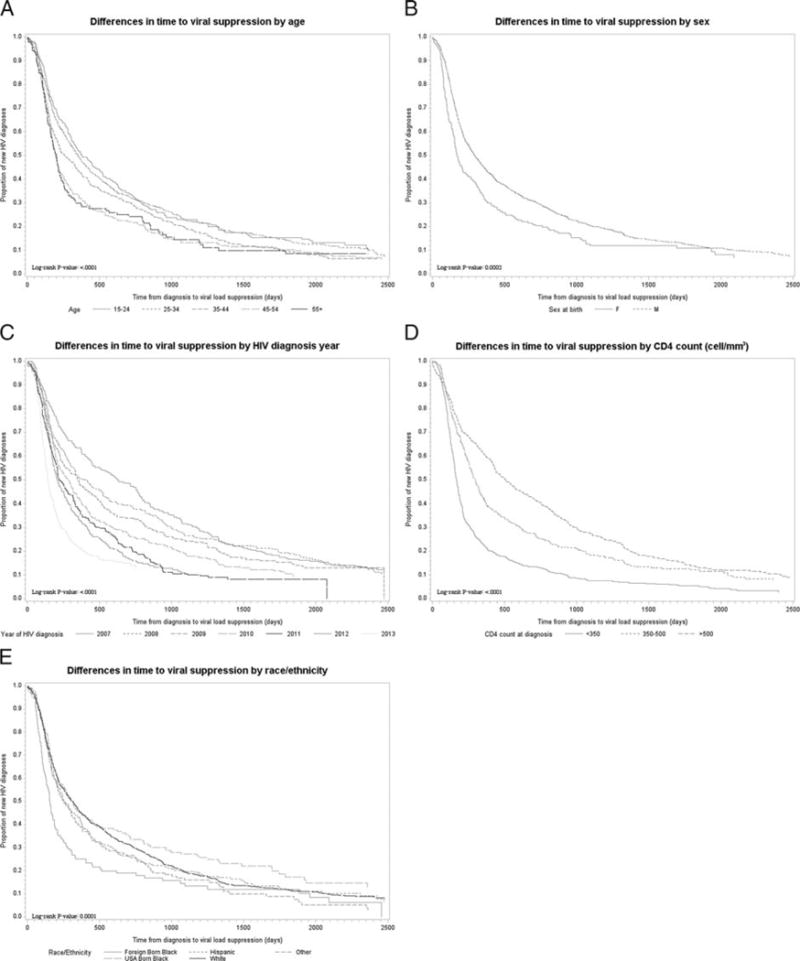
A–F, Kaplan-Meier curves depicting time to viral load suppression among newly diagnosed cases by age, sex, year of diagnosis, CD4 count, race/ethnicity, and transmission category in King County, WA (2007–2013). HETERO indicates heterosexuals.
TABLE 4.
Multivariable Proportional Cox Analysis of Variables Associated With Viral Suppression After HIV Diagnosis in King County, WA (2007–2013)
| HRadj | 95% CI | P | |
|---|---|---|---|
| Race/ethnicity | |||
| Foreign-born black | 1.05 | 0.82–1.33 | 0.72 |
| US-born black | 0.87 | 0.72–1.06 | 0.17 |
| Hispanic | 0.96 | 0.82–1.12 | 0.60 |
| Other | 0.97 | 0.81–1.17 | 0.77 |
| Non-Hispanic white | Reference | ||
| CD4, cells/mm3 | |||
| <350 | 2.07 | 1.82–2.35 | <0.0001 |
| 350–500 | 1.27 | 1.10–1.47 | <0.01 |
| >500 | Reference | ||
| Sex | |||
| Female | 1.31 | 1.02–1.69 | 0.04 |
| Male | Reference | ||
| Age at diagnosis, y | |||
| 15–24 | 0.80 | 0.63–1.01 | 0.06 |
| 25–34 | 0.79 | 0.64–0.98 | 0.03 |
| 35–44 | 0.93 | 0.75–1.15 | 0.48 |
| 45–54 | 1.09 | 0.87–1.36 | 0.48 |
| 55+ | Reference | ||
| Risk | |||
| Unknown | 1.05 | 0.80–1.37 | 0.73 |
| IDU | 0.75 | 0.53–1.08 | 0.12 |
| MSM | 1.03 | 0.78–1.36 | 0.81 |
| MSM/IDU | 0.72 | 0.52–1.01 | 0.06 |
| Heterosexual | Reference | ||
| Year of diagnosis | |||
| 2007 | 0.39 | 0.32–0.48 | <0.0001 |
| 2008 | 0.43 | 0.35–0.52 | <0.0001 |
| 2009 | 0.49 | 0.39–0.60 | <0.0001 |
| 2010 | 0.58 | 0.47–0.70 | <0.0001 |
| 2011 | 0.71 | 0.58–0.87 | <0.01 |
| 2012 | 0.70 | 0.57–0.86 | <0.001 |
| 2013 | Reference |
DISCUSSION
Evaluating King County, WA, HIV surveillance data, we found that the median time from diagnosis to viral load suppression declined 79% for individuals diagnosed between 2007 and 2013, and the decline was most pronounced among persons diagnosed as having higher CD4 counts. We observed no significant indication of racial disparities in time to suppression. These findings highlight the success of one US urban area in instituting early initiation of ART. Further studies are needed to elucidate whether provider prescribing practices or other local implementation factors (funding, political climate, patient awareness, access to medication and the health care system, etc) are primarily responsible for early ART initiation. Our findings have favorable implications related to the clinical outcomes among persons living with HIV/AIDS and HIV transmission.16
Although much of the change in time to viral suppression is likely a consequence of changes in clinical practice prompted by changes in US national ART guidelines, our findings suggest that guideline changes alone do not entirely explain the dramatic increase in how quickly patients became virally suppressed. Stratifying by CD4 count, we found that the time to viral suppression among persons with the highest CD4 counts clearly declined before the 2012 change in HIV treatment guidelines recommending that all persons with HIV receive ART. This finding demonstrates that clinical practice favoring earlier initiation of ART, at least in King County, WA, changed well in advance of national treatment guidelines.
Prior studies from San Francisco and New York City (NYC) evaluated trends in time from diagnosis to viral load suppression. Investigators in San Francisco found that the median time to virologic suppression decreased roughly 69% between 2004 and 2009, from 32 months (~960 days) to 10 months (~300 days).17 In NYC, persons suppressed (defined as viral load <400 copies/mL) 12 months after diagnoses increased from 36% in 2006 to 45% in 2009, with the most rapid viral suppression occurring among persons with the lowest CD4 lymphocyte counts (0–199 cells/mm3).18 The pattern of viral suppression in King County in 2009 was very similar to that reported in NYC and San Francisco; in 2009, the median time to viral suppression in King County was 363 days, and 50% of persons suppressed within the first 12 months after diagnosis. Our more recent data demonstrate that viral suppression now occurs much more quickly after HIV diagnosis. That older data from King County are so similar to findings in other cities suggests that our more recent data may be reflective of patterns of viral suppression occurring in at least some other US cities.
After adjusting for calendar year and CD4 count at time of HIV diagnosis, the only factor significantly associated with a lower likelihood of viral suppression was younger age. This finding highlights the need to focus particular attention on young persons with HIV, but also demonstrates our area’s success in avoiding significant racial or ethnic disparities in ensuring that persons with HIV receive the care they need after HIV diagnosis. Nationally, blacks are less likely to be virally suppressed than whites, and reducing HIV-related disparities is a critical component of the National HIV/AIDS Strategy.19,20 Our findings are good evidence that such disparities can be mitigated, at least in the initial period after HIV diagnosis.
Our study has several limitations. Laboratory reporting improved over the study period, and more complete ascertainment of viral suppression, rather than a true change in virologic outcomes, may have contributed to our findings. Although this change in surveillance data quality could have affected data from earlier years of observation, we believe that changes in data completeness are unlikely to have affected our more recent data. Viral load reporting completeness increased from 86% in 2010 to 93% in 2011 and has subsequently stayed high.21 Because of an administrative censoring date of June 5, 2015, it is also possible that very recent laboratories were missed, although this impact should be small due to high levels of suppression before this date. Surveillance data could also be limited by missing or inaccurate dates of HIV diagnosis. However, all new HIV diagnoses in King County are investigated through medical record reviews and, when possible, interviews with patients conducted as part of HIV partner services, and date of HIV diagnosis reflects the results of these comprehensive efforts. We may also be unaware of individuals enrolled in studies, although through initial interviews and follow-up with providers when laboratories are missing, missing study information should be minimized. Our team would not have ascertained viral suppression among persons who left WA State after HIV diagnosis. When looking at the total population of persons living with HIV/AIDS, migration leads to substantial underestimates of population-level viral suppression.11 This limitation is likely less important when evaluating outcomes in the period immediately after HIV diagnosis, but could have led to an underestimate of viral suppression in our data. We defined time to viral suppression using the date of first HIV RNA test demonstrating viral suppression. The true time to viral suppression is clearly somewhat shorter than this date. Thus, our findings are conservative. Finally, because it was not possible to include specific drug regimen used as an independent variable in our analysis, we cannot assess the extent to which more rapid viral suppression may have been a consequence of use of drug regimens that more quickly achieve viral suppression.
In summary, we found that the time from HIV diagnosis to viral suppression dramatically declined between 2007 and 2013; that the median time from diagnosis to documented viral suppression in King County, WA, in 2013 was 142 days; and that 77% persons in the area in 2013 were virally suppressed within 1 year of HIV diagnosis. Although additional efforts to further shorten this period between diagnosis and effective treatment may be worthwhile, our findings demonstrate that most persons with HIV in our area rapidly achieve the goals of HIV treatment after initial diagnosis. In areas like ours, efforts to minimize the morbidity associated with HIV and diminish transmission should focus on ensuring that HIV diagnoses occur as quickly as possible after infection and promoting the effective treatment for the minority of persons who fail to achieve viral suppression.
Supplementary Material
Acknowledgments
Sources of Funding: Research reported in this publication was supported, in part, by Co-operative Agreement with the Centers for Disease Control and Prevention (CDC) for the National HIV Surveillance System (CDC-RFA-PS13-130202) and National Institute of Allergy and Infectious Disease, National Cancer Institute, National Institute of Mental Health, National Institute on Drug Abuse, National Institute of Child Health and Human Development, National Heart, Lung, and Blood Institute, National Institute on Aging, National Institute of General Medical Sciences, and National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under award number P30AI027757. The content is solely the responsibility of the authors and does not necessarily represent the official views of the CDC or National Institutes of Health.
Footnotes
Conflict of Interest: There are no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (http://www.stdjournal.com).
References
- 1.Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents. Department of Health and Human Services; May 4, 2006. p. 8. Available at: https://aidsinfo.nih.gov/contentfiles/adultandadolescentgl05042006050.pdf. Accessed June 22, 2015. [Google Scholar]
- 2.Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in HIV-1–Infected Adults and Adolescents. Department of Health and Human Services; Jan 29, 2008. p. 12. Available at: https://aidsinfo.nih.gov/contentfiles/adultandadolescentgl000988.pdf. Accessed June 22, 2015. [Google Scholar]
- 3.Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in HIV-1–Infected Adults and Adolescents. Department of Health and Human Services; Dec 1, 2009. p. 22. Available at: https://aidsinfo.nih.gov/contentfiles/adultandadolescentgl001419.pdf. Accessed June 22, 2015. [Google Scholar]
- 4.Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents. Department of Health and Human Services; Mar 27, 2012. p. E-1. Available at: https://aidsinfo.nih.gov/contentfiles/adultandadolescentgl003093.pdf. Accessed June 22, 2015. [Google Scholar]
- 5.Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1–infected adults and adolescents. Department of Health and Human Services; Available at: http://aidsinfo.nih.gov/contentfiles/lvguidelines/AdultandAdolescentGL.pdf. Accessed May 10, 2014. [Google Scholar]
- 6.Kitahata MM, Gange SJ, Abraham AG, et al. Effect of early versus deferred antiretroviral therapy for HIV on survival. N Engl J Med. 2009;360:1815–1826. doi: 10.1056/NEJMoa0807252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Executive Order—HIV Care Continuum Initiative. 2013 Available at: http://www.whitehouse.gov/the-press-office/2013/07/15/executive-order-hiv-care-continuum-initiative. Accessed Apr 20, 2014.
- 9.Gardner EM, McLees MP, Steiner JF, et al. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52:793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nosyk B, Montaner JS, Colley G, et al. The cascade of HIV care in British Columbia, Canada, 1996–2011: A population-based retrospective cohort study. Lancet Infect Dis. 2014;14:40–49. doi: 10.1016/S1473-3099(13)70254-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McNairy ML, El-Sadr WM. Antiretroviral therapy for the prevention of HIV transmission: What will it take? Clin Infect Dis. 2014;58:1003–1011. doi: 10.1093/cid/ciu018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hall H, Frazier E, Rhodes P, et al. Continuum of HIV care: differences in care and treatment by sex and race/ethnicity in the United States. Program and abstracts of the XIX International AIDS Conference; July 22–27; Washington, DC. 2012. Abstract FRLBX05. [Google Scholar]
- 13.Dombrowski JC, Buskin SE, Bennett A, et al. Use of multiple data sources and individual case investigation to refine surveillance-based estimates of the HIV care continuum. J Acquir Immune Defic Syndr. 2014;67:323–330. doi: 10.1097/QAI.0000000000000302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.HIV/AIDS Epidemiology Unit, Public Health–Seattle & King County and the Infectious Disease Assessment Unit, Washington State Department of Health. HIV/AIDS Epidemiology report, First Half. 2013;82 Available at: www.kingcounty.gov/healthservices/health/communicable/hiv/epi.aspx. Accessed August 21, 2014. [Google Scholar]
- 15.Buskin SE, Kent JB, Dombrowski JC, et al. Migration distorts surveillance estimates of engagement in care: Results of public health investigations of persons who appear to be out of HIV care. Sex Transm Dis. 2014;41:35–40. doi: 10.1097/OLQ.0000000000000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Institute of Allergy and Infectious Disease. Questions and Answers The START HIV Treatment Study. 2015 May 27; Available at: http://www.niaid.nih.gov/news/QA/Pages/STARTqa.aspx. Accessed June 22, 2015.
- 17.Moupali D. Reducing Community Viral Load to Achieve HIV Prevention. Available at: http://www.iapac.org/AdherenceConference/presentations/ADH7_Invited_Das.pdf. Accessed May 10, 2014.
- 18.Torian LV, Xia Q. Achievement and maintenance of viral suppression in persons newly diagnosed with HIV, New York City, 2006–2009: Using population surveillance data to measure the treatment part of “test and treat”. J Acquir Immune Defic Syndr. 2013;63:379–386. doi: 10.1097/QAI.0b013e3182926b02. [DOI] [PubMed] [Google Scholar]
- 19.U.S Department of Health and Human Services. Goals for the National HIV/AIDS Strategy. Available at: http://aids.gov/federal-resources/national-hiv-aids-strategy/overview/. Accessed May 1, 2014.
- 20.Hall HI, Tang T, Westfall AO, et al. HIV care visits and time to viral suppression, 19 U.S. jurisdictions, and implications for treatment, prevention and the national HIV/AIDS strategy. PLoS One. 2013;8:e84318. doi: 10.1371/journal.pone.0084318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.HIV/AIDS Epidemiology Unit, Public Health–Seattle & King County and the Infectious Disease Assessment Unit, Washington State Department of Health. HIV/AIDS Epidemiology report. 83 Available at: www.kingcounty.gov/healthservices/health/communicable/hiv/epi.aspx. Accessed August 21, 2014. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


